Академический Документы
Профессиональный Документы
Культура Документы
Lung 1
Загружено:
Technos_IncОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Lung 1
Загружено:
Technos_IncАвторское право:
Доступные форматы
Assessment of Operative Risk in Patients
Undergoing Lung Resection*
Importance of Predicted Pulmonary Function
David]. Kearney, M.D.; Thomas H. Lee, M.D.; John]. Reilly, M.D.,
F.C.C.A. ; Malcolm M. DeCamp, M.D.; and David]. Sugarbaker, M.D.,
F.C.P.P.
Objective: To evaluate the ability of preoperative FEV 1 Hypercarbia (~ 45 mm Hg) on preoperative
variables to identify patients at increased risk for arterial glood gas analysis, desaturation on exercise
complications after lung resection and the usefulness oximetry(~ 90 percent), and a preoperative FEV 1 less
of predicted postoperative FEV 1 as a marker of risk than 1 L were not predictive of complications. When
for adverse outcomes. the effect of these variables was controlled for in a
Design: Prospective analysis of a cohort of patients multivariate analysis, a low predicted postoperative
undergoing pulmonary resection. Complication rates FEV 1 remained the only significant independent pre-
were analyzed according to preoperative pulmonary dictor of complications. For each 0.2 L decrease in
variables, demographic variables, procedure per- predicted FEV 1, the odds ratio for complications was
formed, and predicted postoperative FEV 1 Predicted 1.46 (95 percent confidence interval [CI] 1.2 to 1.8).
postoperative FEV 1 was calculated using a formula Conclusions: A low predicted postoperative FEV 1
estimating the decline in preoperative FEV 1 based on appears to be the best indicator of patients at high
the number of bronchopulmonary segments removed risk for complications, and it was the only significant
during surgery. correlate of complications when the effect of other
Setting: A major teaching hospital and tertiary refer- potential risk factors was controlled for in a multivari-
ral center. ate analysis. Pulmonary resection should not be de-
Patients: A consecutive series of patients undergoing nied on the basis of traditionally cited preoperative
pulmonary resection. pulmonary variables, and a prediction of postopera-
Measurements and main results: Medical complica- tive pulmonary function by a technique of simple
tions were recorded as part of an ongoing clinical calculation may be useful to identify patients at
database. The overall complication rate was low (17 increased risk for medical complications.
percent rate of any complication, 1 percent death (Chest 1994; 105: 153-59)
rate). Univariate predictors of complications included ABG =arterial blood gas; MVV =maximum voluntary
age ~ 60, male sex, history of smoking, a pneumon- ventilation; PPOFEV 1 =predicted postoperative FEV 1
ectomy procedure, and a low predicted postoperative
~ng cancer is the most common cause of cancer associated with atherosclerotic vascular disease, mak-
death in the United States. 1 An estimated 168,000 ing these conditions prevalent in patients with lung
new cases will occur this year, 2 and the majority will carcinoma. Thus, the clinician is often faced with the
die within the first year after diagnosis.3 For patients problem of considering lung resection as the only
with non-small-cell carcinoma presenting as localized curative treatment in a patient with significant comorbid
disease and ventilatory impairment.
For editorial comment see page 654 A wide range of tests has been evaluated to aid the
identification of patients at high risk for developing
disease, surgical resection remains the only potentially complications after lung resection. These tests have
curative option 4 The high rate of coexistent medical included spirometry, arterial blood gas measurement
conditions in lung cancer patients complicates referral (ABC), exercise testing, and radionuclide lung scan-
of such patients to surgery. Smoking is highly associ- ning. Previously reported studies have sought to de-
ated with the development of lung carcinoma;5 the fine values for each of these modalities that would
incidence increases further in smokers with COPD.B-9 identify patients at prohibitive risk. 10- 15 Demographic
Additionally, smoking and chronic lung disease are variables such as male sex, advanced age, and smoking
status have been shown to identify groups at increased
*From the Respiratory Division( Dr. Reilly) , Division of Tho-
racic Surgery (Drs. DeCamp and Sugarbaker), Department of risk. 6 814161i Reported complication rates after lung
Medicine (Dr. Lee) , Brigham & Women's Hospital, and De- resection have ranged from a 40 percent rate of death
partme nt of Medicine (Dr. Kearney) , Beth Israel Hospital ,
Boston. or severe disability in the 1950s and 1960s to mortality
Manuscript received March 24, 1993; revision accepted July 23. rates of9 to 27 percent in the 1970s} 2 18' 20 Advances in
Reprint requests: Dr. Srfgarbaker, Division of Thoracic Surgenj,
Briglwmand Wom en's Hospital, Boston 02115. operative technique and postoperative care have led
CHEST I 105 I 3 I MARCH, 1994 753
to a further decline in postoperative complication Table 1 - Baeline Characteri.tic of 331 Patient
rates, with mortality rates of 2 to 11 percent reported Undergoing Lung Reection
in recent studies.15 21 "26
No. of
This decline in risk for patients undergoing lung Characteristic Patients %
resection has led to a reappraisal of many of the
Sex
criteria that previously would have rendered a patient
Male 185 56
inoperable. The present study examines the relevance Female 146 44
of many of these traditionally cited risk factors in the Age
modem hospital setting and evaluates the use of a Mean SD 58 13.0
simple calculation of predicted postoperative pulmo- Range 17-82
Type of Operation
nary function as a predictor of postoperative complica- 1-3 wedge resection(s) 127 38
tions. <!: 4 wedge resections 9 3
Lobectomy 145 44
METHODS Bilobectomies 4 1
Pneumonectomy 46 14
Patients Smoking history
The patient population consists of 331 patients who underwent Past or present 243 73
single or multiple pulmonary wedge resections, lobectomies, or Still smoking 67 20
pneumonectomies. Subjects who underwent exploratory or staging Never smoked 88 27
thoracotomy procedures without resection of lung parenchyma Grade of dyspnea
were excluded from the study. This study population represents 86 preoperatively (n = 274)
percent (331) of 385 patients undergoing the above procedures Dyspnea with severe exertion only 153 56
during 24 months from August 1989, to August 1991, at the Dyspnea on hills or stairs 79 29
Brigham and Women's Hospital, Boston. The 54 patients (14 Can walk indefinitely on level ground 29 11
percent) meeting the above criteria not included in the analysis Dyspnea at 100 yds 10 4
were omitted because they were inadvertently not entered pro- Dyspnea with minimal activity 3 1
spectively in the clinical database. This occurred on a random basis Kamofsky score (n = 279)
without apparent selection bias. MeanSD 9.1 1.1
After surgery, all patients were cared for in a specialized Range 4-10
intermediate care unit by the thoracic surgery service. The purpose Pathology final diagnosis
of this unit is to provide specialized nursing care, respiratory Benign 65 20
therapy, pain control, and medical care to patients immediately Malignant 266 80
after thoracic surgery. Emphasis is placed on aggressive pulmonary
care, early ambulation, and pain control to minimize postoperative
pulmonary complications.
number of bronchopulmonary segments removed was recorded for
Data Collection each patient. Assuming that each of the 19 bronchopulmonary
All clinical data were recorded prospectively as part of an segments in the normal lung contributes equally to ventilatory
ongoing clinical database. Preoperative assessment included the function, each segment accounts for 5.26 percent of total lung
documentation of historic information (symptoms, coexistent medical function. The predicted postoperative FEY1 was then estimated by
conditions, and tobacco use) as well as functional status (Kamofsky the following formula: 17 predicted postoperative FEY1 = preoperative
score). Preoperative pulmonary evaluation included ABC analysis FEY1 x [1- (S x 5.26)/100), (S =number of bronchopulmonary
(recorded in 95 percent of patients) and spirometry (recorded in 98 segments removed).
percent of patients). Patients also underwent measurement of A right pneumonectomy was considered to cause a 55 percent
room air oxygen saturation by oximetry at rest and with ambulation decrement in preoperative FEY1 and a left pneumonectomy to
(recorded in 79 percent of patients). The ambulatory measure- cause a 45 percent decrement. In patients undergoing wedge
ments involved a 6 -min walk on a level surface followed by two resections, each wedge resection was assumed to account for one
flights of stairs. The lowest percent saturation during this course bronchopulmonary segment. The right and left lower lobes were
was examined for this study. considered to have five bronchopulmonary segments, the right
All patients were followed up prospectively after surgery and middle lobe to have two bronchopulmonary segments, the right
complications occurring during the patient's hospitalization that upper lobe to have three bronchopulmonary segments, and the left
were identified in physician progress notes were recorded. For this upper lobe to have four bronchopulmonary segments.
study, "complications" were defined to include respiratory compli-
cations (pneumonia, atelectasis, mechanical ventilation for longer Statistics
than 2 days, and respiratory failure), cardiac complications (myo- The relationships between potential predictors and postoperative
cardial infarction, supraventricular arrhythmias, ventricular complications were assessed in univariate and multivariate analyses.
arrhythmias), renal failure, and postoperative death. All statistical tests were two-tailed, with a significance level of 0.05.
Categoric variables (sex, smoking status, preoperative Pco2 45 mm
Predicted Postoperative FEV1 Hg, complications, and FEY1 > 1 L) were evaluated using a chi-
Calculation of the forced expiratory volume in Ls (FEY1) was square test or Fisher's exact test when the expected cell counts
performed using preoperative pulmonary function testing data and were less than five. Continuous variables (age, FEY 1 value) were
information on the number of bronchopulmonary segments re- evaluated using the Student's t test and a Wilcoxon rank sum test.
moved (which usually can be predicted on the basis of preoperative A multivariate logistic regression analysis was performed to identify
radiologic studies). All operative notes were reviewed, and the the independent correlates of complications.
754 Operative Risk In Patients Undergoing Lung Resection (Kearney eta/)
Table 2 -Complications Occurring in 331 Patienn Patients older than 60 years had a significantly higher
After Lung Resection rate of any complication. Thirty-seven (22 percent) of
167 patients aged 60 or older had complications vs 18
No. of
Complication Type Patients % (11 percent) of 159 patients less than 60 years of age
(p < 0.05). Male patients had a significantly higher
Any complication 56 17
overall complication rate. Complications occurred in
Respiratory
Pneumonia 8 2 40 (22 percent) male patients vs 16 (11 percent)
Atelectasis (~2 bronchoscopies req) 13 4 female patients (p < 0.05).
Atelectasis (>2 bronchoscopies req) 1 0.3 Smoking status also was evaluated in patients un-
Respiratory failure 6 2 dergoing surgery. Two hundred forty-three patients
Mechanical ventilation required for >2 days 4 1
had a history of cigarette use, and 67 patients were still
postoperatively
Cardiac smoking at the time of surgery (Table 3). Eighty-eight
Supraventricular tachycardia 37 11 patients denied any history of tobacco use. The num-
Ventricular arrhythmia 4 1 ber of adverse postoperative events was not signifi-
Arrhythmia req cardoiversion 1 0.3 cantly higher in patients still smoking at the time of
My?Cardial infarction 2 0.6
surgery. Complications occurred in 12 (18 percent) of
Renal failure 4 1
Postoperative death 3 0.9 67 patients still smoking vs 44 (17 percent) of 264
patients not using tobacco at the time of admission (p
value not significant). When patients with any history
RESULTS of tobacco use (current or at any point in the past)
were examined, a significantly higher rate of postop-
Study Population erative complications was found. Forty-eight (20 per-
The clinical characteristics of the 331 patients (mean cent) of 243 patients with any history of tobacco use
age 58; 56 percent men) who underwent wedge
Table 3 -Clinical Correlates of Poltoperatiofl
resections, lobectomies, or pneumonectomies are sum- Complications
marized in Table 1. The most common operation, a
lobectomy, was performed in 145 cases, while 46 No. No. (%)With Any
patients underwent pneumonectomy. Two hundred Parameter Patients Complication p Value
forty-three patients had a history of tobacco use. Only Age* <0.05
13 of the patients had dyspnea after walking 100 yards ~ 167 37 (22)
<60 159 18 (11)
or less before surgery, and the mean Karnofsky score
Sex <0.05
was 9.1. Two hundred sixty-six patients had malignant Male 185 40 (22)
neoplasms as their final diagnosis. Female 146 16 (11)
Smoker
Complication Rate Current NSf
Yes 67 12 (18)
Complications occurring postoperatively are dis- No 264 44 (17)
played in Table 2. Eight of 331 patients developed Ever smoked
pneumonia, and 14 patients developed atelectasis, one Yes 243 48 (20) <0.05
No 88 8 (9)
of whom required more than two bronchoscopies Preoperative FEV1 NS
postoperatively. Four patients required mechanical :2:1 L 307 51 (17)
ventilation for more than 2 days after surgery, and <lL 17 3 (18)
respiratory failure developed in six patients. Cardiac Preoperative Pco2 NS
:2:45 mm Hg 30 4 (13)
complications included supraventricular arrhythmias <45 mm Hg 285 50 (17)
that occurred in 37 patients and ventricular arrhythmias Exercise %Sa02 NS
that occurred in 4 patients. One patient required :2:90 185 28 (15)
cardioversion, and two patients developed postopera- <90 77 12 (16)
Procedure
tive myocardial infarctions. Renal failure occurred in Pneumonectomy <0.001
four patients, and three patients died during hospital- Yes 46 18 (39)
ization. No 285 38 (13)
Lobectomy NS
Predictors of Postoperative Complications Yes 145 28 (19)
No 186 28 (15)
Variables often considered predictors of postopera- 1-3 Wedge resections <0.001
tive complications are displayed in Table 3. These Yes 127 8 (6)
include advanced age, male sex, smoking status, pro- No 204 48 (24)
cedure performed, and preoperative pulmonary vari- *Data missing on 5 patients.
ables (FEV" Pco2 data, and exercise pulse oximetry). t NS =not significant.
CHEST I 105 I 3 I MARCH, 1994 755
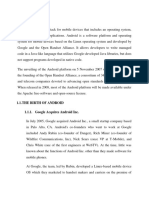
40
...
Predicted postoperative FEV1 :
z (')
< 1.0 l n=47
0
t= 0 1.01 .4L n=56
c 30
0 > 1.4 L n=221
0
::; p < 0.001 p < 0.05
a. C\1
:::E
0 20 "'
0 II)
%
1-
i 10
0~
0
2 3
An y Cardiac Respiratory
TYPE OF COMPLICATION
FI<: l! HE I. Postoperati\e complication rate according to predicted postope ratiq FE\' ntlue.
1
had a postoperative complication vs 8 (9 percent) of 88 had a significantly lower rate of any complication.
patients without any history (p < 0.05). Eight (6 percent) of 12i patients having a wedge
Patients with a preoperative FEV 1 of less than 1 L resection had a complication vs 48 (24 percent) of
did not have an increased overall complication rate. 204 patients having a more extensive procedure
Complications occurred in 3 (18 percent) of li (p < 0.001). Patients who underwent lobectomies or
patients with a FEV 1 less than 1 L vs .51 ( 1i percent) four or more wedge resections did not have signifi-
of 30i patients with a preoperative FEV 1 greater cantly different complication rates when compared
than 1 L (p value not significant). Complication with patients not having these procedures.
rates also were evaluated according to preoperative
Pco., data on ABC analysis. No significant differ- Complication Rate by Predicted Postoperative
ence in the overall complication rate was noted for FEV 1 Values
patients with a Pco 2 greater than or equal to 4.5 mm Figure 1 shows the postoperative complication
Hg preoperatively. Four ( 13 percent) of 30 patients rate stratified according to predicted postoperative
with hypercarbia had complications vs 50 (li per- FEV 1 value. Complication rates were assessed for
cent) of 285 patients without hypercarbia (p value other complications , cardiac complications, and res-
not significant). Preoperative exercise pulse oximetry piratory complications . Forty-seven patients had a
data also was assessed (as evaluated by recording predicted postoperative FEV 1 less than 1 L, and 16
the lowest percent saturation during a 6-min walk of these (34 percent) had other complications, 9 ( 19
on a level surface followed by two flights of stairs) . percent) had a cardiac complication, and i ( 15
This was not associated with an increased occur- percent ) had a respiratory complication. Fifty-six
rence of complications. Twelve ( 16 percent) of ii patients had predicted postoperative FEV 1 of 1.01
patients with desaturation on exercise pulse oximetry to 1.40 L, and 14 (25 percent) of these had other
had complications vs 28 ( 1.5 percent) of 18.5 patients complications, 12 (21 percent) had a cardiac com-
without desaturation (p value not significant). plication, and .5 (9 percent) had a respiratory com-
Patients were classified according to the extent of plication. Two hundred twenty-one patients had a
lung resection performed, and differences in com- predicted postoperative FEV 1 of greater than 1.4 L,
plication rates were examined (Table 3). Patients and 24 ( 11 percent) of these had other complica-
undergoing a pneumonectomy had a significantly tions , 20 (9 percent) had cardiac complications, and
higher rate of complications . All deaths occurred in 6 (3 percent) had respiratory complications. As the
the group undergoing pneumonectomies. Eighteen predicted postoperative FEV 1 declined , a signifi-
(39 percent) of 46 patients undergoing a pneumon- cant association \Vas found for an increased occur-
ectomy had a complication vs 38 (13 percent) of 28.5 rence of other complications (p < 0.001), cardiac
patients not having this procedure (p < 0.001) . Pa- complications (p < 0.0.5), and respiratory complica-
tients undergoinig one to three wedge resections tions (p < 0.001) .
756 Operative Risk in Patients Undergoing Lung Resection (Kearney et a/)
Multivariate Analysis modalities (chest physiotherapy, incentive broncho-
In a multivariate logistic-regression analysis adjust- spirometry, adequate anesthesia, and early ambulation)
ing for age, sex, preoperative Pco 2 greater than or may also have led to a decreased occurrence of
equal to 45 mm Hg, exercise pulse oximetry saturation respiratory complications. Furthermore, this study
of less than 90 percent, history of tobacco use, history was performed in a tertiary referral center with sur-
of coronary artery disease, and history of hyperten- geons experienced in performing large numbers of
sion, postoperative FEV1 was a significant indepen- lung resections. Also, the patient population operated
dent predictor of complications. For each 0.2 L de- on appears to have been relatively healthy. The small
crease in predicted FEV 1, the odds ratio for number of patients in this study with preoperative
complications was 1.46 (95 percent CI 1.2 to 1.8). FEV1 values less than 1 L (17 patients) suggests that
Only the predicted postoperative FEV1 subgroup re- selection of a patient population without severe venti-
mained associated significantly with an increased rate latory impairment is likely to have contributed to a low
of other complications postoperatively when the effect complication rate, and the relatively intact grades of
of the other variables was controlled for in the model. preoperative dyspnea and Kamofsky scores support
this hypothesis. Also, patients undergoing exploratory
DISCUSSIO:-; procedures without resection of lung parenchyma
This study examined the postoperative course of a were excluded from the analysis. This may have
large cohort of patients undergoing lung resections contributed to the low complication rate as well, with
and evaluated the significance of a number of the exclusion of patients with more advanced non-
preoperative variables as indicators of postoperative resectable disease who may be more likely to have a
risk. The postoperative complication rate was quite complicated course.
low, and the best indicators of patients at high risk for Previous studies have yielded conflicting results
the development of complications were a low pre- regarding the use of preoperative pulmonary function
dicted postoperative FEV1 or a pneumonectomy as tests as predictors of postoperative complications. The
the procedure performed. The predicted postopera- original work by Gaensler et al in 1955, 18 was based on
tive FEV 1 remained the only significant predictor of the outcome of patients undergoing surgery for tuber-
complications when the effect of other traditionally culosis. He found that patients with a preoperative
cited markers of increased risk was controlled in a FEV1 less than 70 percent predicted or with a maxi-
multivariate analysis. Alow preoperative FEV 1did not mum voluntary ventilation ( MW) less than 50 percent
correlate with complications (although the small num- predicted had a 40 percent mortality rate. Subsequent
ber of patients [17] with an FEV1 less than 1 L limits investigators noted in the 1960s and 1970s that pa-
the power to detect a significant difference). An tients with an MW less than 50 percent or a depressed
elevated Pco2 also did not correlate with a complicated FEV 1 ( < 1.2 L or < 2 L and age > 60) had a high
postoperative course in this study. These results sug- mortality rate when undergoing surgery for lung can-
gest that lung resection usually is tolerated well even cer.1119.21 Other investigators found no significant dif-
in patients with significant ventilatory impairment and ference in FEV1 between survivors or nonsurvivors in
that estimation of the predicted postoperative FEV1 patients undergoing pneumonectomy or lobectomy. 2028
by a simple calculation may be useful in identifying Olsen et al 29 identified patients considered at high risk
patients at high risk for a complicated course. (FEV1 <2 Lor MW <50 percent predicted) and found
The postoperative complication rate (less than 1 that these patients could undergo resection with ac-
percent mortality rate and 17 percent rate of any ceptable mortality rates if they did not have pulmo-
medical complication) is somewhat lower than that nary hypertension or hypoxia on pulmonary occlusion
reported in previous studies. Large studies in the studies, or had a predicted postoperative FEV1 of
1980s have reported mortality rates after lung resec- greater than 800 ml by quantitative perfusion scan-
tion as low as 2 to 5 percent with somewhat higher ning.29 Interestingly, they note in this study that the
mortality rates in older patients and in series examin- predicted postoperative FEV 1 value of 800 ml as a
ing pneumonectomies alone. 15 21 ' 26 2~ The low occur- cutoff point was not derived through studies of pa-
rence of adverse outcomes in this series may be due to tients undergoing lung resection but through observa-
several factors . The method of recording complica- tion of the degree of ventilatory impairment usually
tions by reviewing physician progress notes rather tolerated by patients with severe obstructive lung
than by examining objective measures of disease (ie, disease. A postoperative FEV1value of less than 800 to
reviewing chest x-ray films for evidence of pneumo- 1,000 ml has been cited widely as a prohibitive level of
nia) is likely to have contributed to the low rate of pulmonary function since that time. One study since
postoperative complications. Treating patients after has shown that patients with marked impairment of
surgery in a specialized intermediate care unit, with pulmonary function (preoperative FEV1< 1Lor MW
emphasis on aggressive , preventive respiratory <35-40 percent predicted) tolerated limited resec-
CHEST I 105 I 3 I MARCH, 1994 757
tions well. 30 The present study appears to confirm monary function. Previous studies also have shown
these findings . Limited resections (single or multiple that low predicted postoperative FEV 1 values (using
wedge resections) were performed in 12 of the 17 quantitative perfusion lung scanning) correlate with
patients with a preoperative FEV1ofless than 1 L, and complications. 1521 Markos et aP 5 examined the out-
the remaining 5 patients underwent lobectomies. These come of 55 patients undergoing lung resections, and
patients with markedly impaired preoperative pulmo- they found a significantly increased mortality rate
nary function did not have an increased incidence of among patients with predicted FEV1 less than 40
complications. percent predicted. In a larger study, Wahi and col-
A predicted postoperative FEV1of less than 1 L was leagues21 analyzed 197 patients undergoing pneumon-
the best predictor of postoperative complications in ectomies, and they found a significantly elevated
this study (p < 0.001), whereas a preoperative FEV1of mortality rate among patients whose predicted post-
less than 1 L was not predictive of complications. operative FEV1 was less than 1.65 L. Another study
While this appears to confirm the criteria of Olsen et (involving only 22 patients) has shown no significant
al29 that patients with a low predicted postoperative correlation between predicted postoperative pulmo-
FEV1 are at an increased risk of complications, the nary function values and complications rates.3 1 The
degree of risk does not appear to be prohibitive. Only present study is the first to our knowledge to examine
two deaths occurred in this group (4.3 percent of the the use of estimating the predicted postoperative
47 patients), and two thirds of the patients had an FEV1 by the technique of simple calculation alone.
uncomplicated postoperative course. These results Our study indicates that with modem surgical tech-
also suggest that the magnitude of change in pulmo- niques and improved postoperative care, the level of
nary function may be an important indicator of risk for prohibitive pulmonary function as defined by calcula-
postoperative complications. The group with a pre- tion of predicted postoperative FEV 1 may be signifi-
dicted postoperative FEV1ofless than 1 L necessarily cantly lower than indicated by previous studies using
includes all patients with a preoperative FEV1 of less this method. Although the rate of complications sig-
than 1 L, and this low preoperative FEV1 value alone nificantly was higher in our study among patients with
did not confer increased risk. When patients with a a predicted postoperative FEV1 less than 1 L, the
preoperative FEV1 of greater than 1 L and a postop- magnitude of risk did not appear to be prohibitive.
erative FEV1ofless than 1 L, however, are analyzed as The level of prohibitive risk may lie lower than 1 L,
a group including the patients with both preoperative possibly in the 60 to 800 ml range.
and postoperative FEV1 values less than 1 L, a pre- Patients with hypercarbia on preoperative ABC
dicted postoperative FEV1 less than 1 L is the most measurement have been classified traditionally as
significant predictor of complications. This suggests being at very high risk for postoperative respiratory
that patients with preoperative FEV1 values greater complications (as noted in a recent position paper by
than 1 L who have a predicted decline in FEV1 to less the American College of Physicians on pulmonary
than 1 L after surgery are at higher risk for complica- function testing). 32 The categorization of these pa-
tions. The higher rate of complications among patients tients as very high risk candidates for pulmonary
undergoing pneumonectomies supports this possibil- resection is based on anecdotal reports in the litera-
ity that a large decline in ventilatory function rather ture and has never been studied formally in a large
than a low preoperative FEV1 value alone may be an group of patients. The 30 patients in this study with a
important marker of increased risk. preoperative Pco2 greater than or equal to 45 mm Hg
The use of the technique of estimating predicted did not have an increased occurrence of postoperative
postoperative pulmonary function by simple calcula- complications, and it appears that this should not be
tion is supported by previous studies comparing quan- considered a contraindication to surgery. Previous
titative nuclear medicine scans, simple calculation, investigators also have cited desaturation on pulse
and actual measured postoperative spirometric val- oximetry as indicating a high risk population for lung
ues. 152731 These studies have shown simple calculation resection, 15 but in this study desaturation to less than
to be as accurate as quantitative perfusion scans for 90 percent did not correlate with postoperative com-
this purpose. Estimation of predicted postoperative plications. Patients still smoking until the time of
pulmonary function by simple calculation, however, is surgery did not have significantly more complications
based on the assumption that each bronchopulmonary compared with those not still smoking. Prior studies of
segment contributes equally to ventilatory function, patients undergoing elective coronary artery bypass
and patients with severe atelectasis, hilar disease, or grafting have indicated that patients who choose to
endobronchial involvement may have significantly stop smoking at least 2 months before surgery have a
unequal ventilation or perfusion. In cases where this is lower incidence of complications compared with pa-
suspected, quantitative ventilation/perfusion scanning tients who stop smoking closer to their date of sur-
may be more useful in predicting postoperative pul- gery.33 Unfortunately, it is not clear whether it is
758 Operative Risk in Patients Undergoing Lung Resection (Kesmey et sl)
appropriate to extrapolate these data to patients un- Thorac Surg 1987; 44:344-49
14 Smith TP, Kinasewitz GT, Tucker WY, Spillers WP, George
dergoing lung resection, and the time interval from RB. Exercise capacity as a predictor of post-thoracotomy
smoking cessation to surgery is not recorded in our morbidity. Am Rev Respir Dis 1984; 129:730-34
database. Patients without any smoking history had 15 Markos J, Mullan BP, Hillman DR, Musk AW, Centico VF,
significantly fewer overall complications. Lovegrove FT. Preoperative assessment as a predictor of
mortality and morbidity after lung resection. Am Rev Respir
These data suggest that lung resection can be Dis 1989; 139:902-10
performed in patients with significant ventilatory im- 16 Warner MA, Offord KP, Warner ME, Lennon RL, Conover
pairment with a low rate of morbidity and mortality MA, Jansson-Schumacher U. Role of preoperative cessation of
and that surgery should not be denied on the basis of smoking and other factors in postoperative pulmonary compli-
cations: a blinded prospective study of coronary artery bypass
preoperative variables such as a low FEV" hypercarbia patients. Mayo Clin Proc 1989; 64:609-16
on blood gas analysis, or exercise desaturation on pulse 17 Garibaldi RA, Britt MR, Coleman ML, Reading JC, Pace NL.
oximetry. Additionally, patients undergoing pneumon- Risk factors for postoperative pneumonia. Am J Med 1981;
ectomies or with a low predicted postoperative FEV 1 70:677-80
18 Gaensler EA, Cugell DW, Lindgren I, Verstraeten JM, Smith
as estimated by simple calculation appear to be at SS, Strieder JW. The role of pulmonary insufficiency in mortal-
increased risk for complications, but they may still ity and invalidism following surgery for pulmonary tuberculo-
undergo surgery with acceptable mortality rates. sis. J Thorac Surg 1955; 29:163-85
19 Mittman C. Assessment of operative risk in thoracic surgery.
ACKNOWLEDGMENT: The authors thank Mary Sullivan Visciano Am Rev Respir Dis 1961; 84:197-207
for her editorial assistance. 20 Didolkar MS, Moore RH, Takita H. Evaluation of the risk in
pulmonary resection for bronchogenic carcinoma. Am J Surg
1974; 127:700-03
REFERENCES
21 Wahi R, McMurtrey MJ, DeCaro LF, Mountain CF, Ali MK,
Centers for Disease Control. Trends in lung cancer incidence Smith TL. Determinants of perioperative morbidity and mor-
and mortality-United States,1980-1987. MMWR 1990; 39:875- tality after pneumonectomy. Ann Thorac Surg 1989; 48:33-7
81 22 Ginsberg RJ, Hill LD, Eagan RT, Thomas P. Mountain CF.
2 Boring CC, Squires TS, Tong T. Cancer statistics, 1992. CA Deslauriers J. Modem thirty-day operative mortality for surgi-
1992; 42:19-43 cal resections in lung cancer. J Thorac Cardiovasc Surg 1983;
3 American Cancer Society. Cancer Manual. 8th ed. Boston: 86:654-58
23 Krowka MJ, Pairolero PC, Trastek VF, Payne WS, Bematz PE.
American Cancer Society. 1990
Cardiac dysrhythmia following pneumonectomy: clinical corre-
4 Flehinger BJ. Kimmel M, Melamad MR. The effect of surgical
lates and prognostic significance. Chest 1987; 91 :490-95
treatment on survival in early lung cancer: implications for
24 Kohman LJ, Meyer JA, Ikins PM, Oates RP. Random versus
screening. Chest 1992; 101:1013-18 predictable risks of mortality after thoracotomy for lung cancer.
5 US Department of Health and Human Services. Reducing the J Thorac Cardiovasc Surg 1986; 91:551-54
health consequences of smoking: 25 years of progress-a report 25 Keagy BA, Lores ME, Starek PJK, Murray GF, Lucas CL,
of the Surgeon General. Rockville, Md: US Department of Wilcox BR. Elective pulmonary lobectomy: factors associated
Health and Human Services, Centers for Disease Control, with morbidity and operative mortality. Ann Thorac Surg 1985;
Center for Chronic Disease Prevention and Health Promotion, 40:349-52
Office on Smoking and Health, Public Health Service, DHHS 26 Nagasaki F, Flehinger BJ, Martini N. Complications of surgery
publication No. (CDC) 89-8411, 1989:43-169 in the treatment of carcinoma of the lung. Chest 1982; 82:25-
6 Nomura A, Stemmermann GN. Chyou P, Marcus GB, Buist AS. 9
Prospective study of pulmonary function and lung cancer. Am 27 Juhl B, Frost N. Acomparison between measured and calcu-
Rev Respir Dis 1991; 144:307-11 lated changes in the lung function after operation for pulmo-
7 Large P, Nyboe J. Appleyard M, Jensen G, Schnohr P. Ventila- nary cancer. Acta Anaesth Scand 1975; 57 (suppl):39-45
tory function and chronic mucus hypersecretion as predictors 28 Keagy BA, Schorlemmer GR, Murray GF, Starek PJK, Wilcox
of death from lung cancer. Am Rev Respir Dis 1990; 141:613- BR. Correlation of preoperative pulmonary function testing
16 with clinical course in patients after pneumonectomy. Ann
8 Skillrud DM, Offord KP, Miller RD. Higher risk oflung cancer Thorac Surg 1983; 36:253-57
in chronic obstructive pulmonary disease. Ann Intern Med 29 Olsen GN, Block AJ, Swenson EW, Castle JR, Wynne JW.
1986; 10.5:503-7 Pulmonary function evaluation of the lung resection candidate:
9 Tockman MS. Anthonisen NR. Wright EC, Donithan MG. a prospective study. Am Rev Respir Dis 1975; 111:379-87
Ainvay obstruction and the risk oflung cancer. Ann Intern Med 30 Miller JI, Hatcher CR. Limited resection of bronchogenic
1987; 106:512-8 carcinoma in the patient with marked impairment of pulmo-
10 Zibrak JD, O'Donnell CR. Marton K. Indications for pulmo- nary function . Ann Thorac Surg 1987; 44:340-43
nary function testing. Ann Intern Med 1990; 112:763-71 31 Wemly JA, DeMeester TR, Kirchner PT. Myerowitz PD,
11 Boushy SF, Billing DM, North LB, Helgason AH. Clinical Oxford DE, Golomb HM. Clinical value of quantitative venti-
course related to preoperative and postoperative pulmonary lation-perfusion scans in the surgical management of
function in patients with bronchogenic carcinoma. Chest 1971; bronchogenic carcinoma. J Thorac Cardiovasc Surg 1980;
59:383-91 80:535-43
12 Boysen PC, Block AJ, Moulder PV. Relationship between 32 American College of Physicians. Preoperative pulmonary func-
preoperative pulmonary function tests and complications after tion testing. Ann Intern Med 1990; 112:793-94
thoracotomy. Surg Gynecol Obstet 1981; 152:813-15 33 Warner MA, Divertie MB, Tinker JH. Preoperative cessation of
13 Bechard D, Wetstein L. Assessment of exercise oxygen con- smoking and pulmonary complications in coronary artery by-
sumption as preoperative criterion for lung resection. Ann pass patients. Anesthesiology 1984; 60:380-83
CHEST I 105 I 3 I MARCH, 1994 759
Вам также может понравиться
- Wind Turbine ArchitectureДокумент1 страницаWind Turbine ArchitectureTechnos_IncОценок пока нет
- An Efficient E2E Verifiable E-Voting System Without Setup AssumptionsДокумент9 страницAn Efficient E2E Verifiable E-Voting System Without Setup AssumptionsTechnos_IncОценок пока нет
- WSN and RoutingДокумент20 страницWSN and RoutingTechnos_IncОценок пока нет
- A Human Hand Gesture Based TV Fan Control System Using Open CVДокумент99 страницA Human Hand Gesture Based TV Fan Control System Using Open CVTechnos_IncОценок пока нет
- Smartphone-Based Door Locking SystemДокумент4 страницыSmartphone-Based Door Locking SystemTechnos_IncОценок пока нет
- Banking Robot MissingДокумент18 страницBanking Robot MissingTechnos_IncОценок пока нет
- Android Best Titles 2018Документ2 страницыAndroid Best Titles 2018Technos_IncОценок пока нет
- Bigdata Medical1 PDFДокумент5 страницBigdata Medical1 PDFTechnos_IncОценок пока нет
- Android IntroДокумент7 страницAndroid IntroTechnos_IncОценок пока нет
- Form 1Документ5 страницForm 1rammohanОценок пока нет
- Robot LiteratureДокумент58 страницRobot LiteratureTechnos_IncОценок пока нет
- IEEE ConferenceДокумент9 страницIEEE ConferenceTechnos_IncОценок пока нет
- Economical Study and TestingДокумент16 страницEconomical Study and TestingTechnos_IncОценок пока нет
- Driver Drowsiness ProjectДокумент67 страницDriver Drowsiness ProjectTechnos_IncОценок пока нет
- Buffer ReportДокумент58 страницBuffer ReportTechnos_IncОценок пока нет
- Energy Efficient Scheduling of Real-Time Tasks in Cloud EnvironmentДокумент8 страницEnergy Efficient Scheduling of Real-Time Tasks in Cloud EnvironmentTechnos_IncОценок пока нет
- Skin Cancer ReportДокумент85 страницSkin Cancer ReportTechnos_IncОценок пока нет
- Install Guide Ja JPДокумент124 страницыInstall Guide Ja JPAtlantislandОценок пока нет
- Thermal and Structural Analysis of Vented and Normal Disc Brake RotorsДокумент9 страницThermal and Structural Analysis of Vented and Normal Disc Brake RotorsTechnos_IncОценок пока нет
- ESP8266 WiFi Module Quick Start GuideДокумент15 страницESP8266 WiFi Module Quick Start GuideMitesh Khadgi100% (1)
- Object DetectionДокумент20 страницObject DetectionTechnos_Inc100% (1)
- Android Theft Tracking ReportДокумент56 страницAndroid Theft Tracking ReportTechnos_IncОценок пока нет
- Hand GestureДокумент18 страницHand GestureTechnos_IncОценок пока нет
- AddersДокумент11 страницAddersFikris RamadhaniОценок пока нет
- MEMS and Microsystems OverviewДокумент11 страницMEMS and Microsystems OverviewSenthilkumaar JSОценок пока нет
- Io DesignДокумент14 страницIo DesignTechnos_IncОценок пока нет
- Image Fusion ReportДокумент79 страницImage Fusion ReportTechnos_IncОценок пока нет
- Embedded C LanguageДокумент34 страницыEmbedded C LanguageTechnos_Inc100% (1)
- Target TrackinДокумент39 страницTarget TrackinTechnos_IncОценок пока нет
- Online Review ModulesДокумент2 страницыOnline Review ModulesTechnos_IncОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Columbia-Presbyterian Patient Safety StudyДокумент9 страницColumbia-Presbyterian Patient Safety StudyKathleen Beatty100% (1)
- Be Your Own Boss - Steps To Self-EmploymentДокумент4 страницыBe Your Own Boss - Steps To Self-EmploymentfroseboomОценок пока нет
- Camp Hearne POW Brochure TexasДокумент2 страницыCamp Hearne POW Brochure TexaspcojediОценок пока нет
- Lauren Bradley ResumeДокумент1 страницаLauren Bradley Resumeapi-403271636Оценок пока нет
- NCLEX Test FlashcardsДокумент6 страницNCLEX Test FlashcardsMa Vina Clata100% (1)
- How To Survive Hospital StayДокумент38 страницHow To Survive Hospital StayLaurentiu M.Оценок пока нет
- Lec9 - Intra Oral Radiographic TechniquesДокумент13 страницLec9 - Intra Oral Radiographic TechniquesSawsan Z. JwaiedОценок пока нет
- Masimo Radical 7 Monitor TrainingДокумент35 страницMasimo Radical 7 Monitor TrainingDanniel SchaafОценок пока нет
- An Investigation of The Share of Elements of The Marketing Mix For Selling ICP-Monitoring Devices in Medical Centers of Fars, IranДокумент3 страницыAn Investigation of The Share of Elements of The Marketing Mix For Selling ICP-Monitoring Devices in Medical Centers of Fars, IranardalaneyniОценок пока нет
- Study Objective:: M Sunil KumarДокумент2 страницыStudy Objective:: M Sunil KumarSunil MeesalaОценок пока нет
- Peritonitis Clinical Pathway PDFДокумент4 страницыPeritonitis Clinical Pathway PDFIndah95Оценок пока нет
- 1 Snake BiteДокумент8 страниц1 Snake BiteMatthew Wei Hua CaiОценок пока нет
- Stephanie Merlino ResumeДокумент1 страницаStephanie Merlino Resumeapi-314674970Оценок пока нет
- Principles, Contents, and Steps: Clinical InstructorДокумент25 страницPrinciples, Contents, and Steps: Clinical InstructorWillie KitsОценок пока нет
- Lecture 4 ExerciseДокумент1 страницаLecture 4 ExerciseJobelle Fernandez-SantosОценок пока нет
- Best Practices For The Prevention and Treatment of Pressure UlcersДокумент15 страницBest Practices For The Prevention and Treatment of Pressure UlcersViroj รักเมืองไทยОценок пока нет
- Ross Judice, Acadian Ambulance - The-Katrina-DiariesДокумент113 страницRoss Judice, Acadian Ambulance - The-Katrina-DiariesM. Darryl Woods100% (1)
- 19-06-2017-10-15-0416257 - PD - VMO - Cardiology - Ryde HospitalДокумент8 страниц19-06-2017-10-15-0416257 - PD - VMO - Cardiology - Ryde HospitalHassamОценок пока нет
- DMC Class of 1985 Digital Magazine July 2013Документ41 страницаDMC Class of 1985 Digital Magazine July 2013skhananiОценок пока нет
- Patricia Benner PP Nurs 324Документ31 страницаPatricia Benner PP Nurs 324api-251662522Оценок пока нет
- Process RecordingДокумент10 страницProcess Recordingmichaelsulivan616450% (2)
- Quality in Healthcare SystemsДокумент95 страницQuality in Healthcare Systemslaxman Bhatt0% (1)
- Transcultural NursingДокумент32 страницыTranscultural Nursingnovi100% (2)
- Infection Control Guidance For EMS ProvidersДокумент41 страницаInfection Control Guidance For EMS ProvidersNicholaiCabadduОценок пока нет
- Significance of The StudyДокумент3 страницыSignificance of The StudyFrecious ConcepcionОценок пока нет
- Unit 9 - Lesson 1Документ17 страницUnit 9 - Lesson 1mahammed mahdyОценок пока нет
- Choose The Correct Answer by Crossing (X) A, B, C or D!Документ9 страницChoose The Correct Answer by Crossing (X) A, B, C or D!Yogi WibowoОценок пока нет
- Economics of Canadian Health CareДокумент300 страницEconomics of Canadian Health CareChowdhury Golam Kibria100% (1)
- Abstak Neurointervention EditДокумент2 страницыAbstak Neurointervention Editzefri suhendarОценок пока нет
- Pathology Quality ManualДокумент83 страницыPathology Quality Manualrose_almonteОценок пока нет