Академический Документы
Профессиональный Документы
Культура Документы
Clinical Pharmaciststandardsofpractice
Загружено:
Wilgab UrlanchАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Clinical Pharmaciststandardsofpractice
Загружено:
Wilgab UrlanchАвторское право:
Доступные форматы
Standards of Practice
for Clinical Pharmacists
American College of Clinical Pharmacy
This document sets forth ACCPs expectations for clini- II. Process of Care
cal pharmacists within the United States and countries
around the world where clinical pharmacy is emerging. Clinical pharmacists work in collaborationa with other
It is also intended to serve as a reference for those de- providers to deliver comprehensive medication man-
signing and assessing clinical pharmacy education and agement that optimizes patient outcomes. Care is coor-
training programs. In addition to articulating the clinical dinated among providers and across systems of care as
pharmacists process of care and documentation, the patients transition in and out of various settings.
eight standards below address the clinical pharmacists
involvement in collaborative, team-based practice and The clinical pharmacists process of care comprises the
privileging; professional development and maintenance following components.
of competence; professionalism and ethics; research
and scholarship; and other professional responsibilities. A. Assessment of the patient
The standards define for the public, health profession- The clinical pharmacist assesses medication-
als, and policy-makers what they can and should expect relatedb needs by:
of clinical pharmacists. Reviewing the medical record using a problem-
oriented framework (e.g., interpreting and ana-
I. Qualifications lyzing subjective and objective information) to
determine the clinical status of the patient;
Clinical pharmacists are practitioners who provide com- Meeting with the patient/caregivers to obtain
prehensive medication management1 and related care and document a complete medication history to
for patients in all health care settings. They are licensed identify all of the patients current medicationsc
pharmacists with specialized advanced education and (including regimens and administration routes),
training who possess the clinical competencies neces-
medication-taking behaviors, adherence, aller-
sary to practice in team-based, direct patient care envi-
gies, and attitudes and experiences with medica-
ronments.2,3 Accredited residency training or equivalent
post-licensure experience is required for entry into di- tion therapyd;
Obtaining, organizing, and interpreting patient
rect patient care practice. Board certification is also re-
quired once the clinical pharmacist meets the eligibility data; and
criteria specified by the Board of Pharmacy Specialties Prioritizing patient problems and medication-related
(BPS).4 needs.
a
Collaboration in the context of this document refers to collaborative and cooperative practice activities performed by the clinical phar-
macist as authorized by 1) state practice acts and 2) formal collaborative drug therapy management agreements with other providers and/
or conferred by local privileging within the relevant practice, health system, organization, or institution.
b
Medication-related applies to issues pertaining to 1) the indication/absence of indication, use and administration, therapeutic goals,
adverse drug events, drug interactions, and monitoring of medications; 2) the patients adherence, attitudes, beliefs, and preferences re-
garding his/her medications; and 3) any allergies or adverse reactions to medications.
c
Medications are defined as any of the following: prescription drugs, non-prescription drugs, vaccines, or complementary and alterna-
tive medications.
d
Some patient conditions and clinical settings (e.g., in an intensive care unit, mental health facility, or emergency department) may render
this activity unfeasible.
Standards of Practice for Clinical Pharmacists 1 American College of Clinical Pharmacy
B. Evaluation of medication therapy meeting with the patient/caregivers to obtain
The clinical pharmacist identifies strategies to an updated medication history to identify, as-
optimize medication therapy by: sess, and document any new medication-related
Assessing, with other members of the health care needs or problems;
team, the appropriateness of current medications Conducting ongoing assessments and refining the
on the basis of health conditions, indication, and the plan of care to optimize medication therapy and
therapeutic goals of each medication; ensure that individual goals are achieved; and
Evaluating the effectiveness, safety, and affordability Monitoring, modifying, documenting, and man-
of each medication; aging the plan of care in collaboration with the
Assessing medication-taking behaviors and adher- patient/caregivers and his/her other health care
ence to each medication; and providers.
Identifying medication-related problems and eval-
uating collaboratively with other members of the III. Documentation
health care team the need for intervention.
Clinical pharmacists document directly in the patients
C. Development and implementation of a plan of care medical record the medication-related assessment and
The clinical pharmacist develops and implements, plan of care to optimize patient outcomes. This docu-
collaboratively with the patient and his/her health care mentation should be compliant with the accepted stan-
providers, a plan for optimizing medication therapy by: dards for documentation (and billing, where applicable)
Reviewing the patients active medical problem list
within the health system, health care facility, outpatient
to inform and guide the development of an individ- practice, or pharmacy in which one works. Where appli-
ualized assessment and plan for optimizing medica- cable, accepted standards must be considered as they
tion therapy; relate to the use of electronic health records (EHRs),
Formulating a comprehensive medication manage-
health information technology and exchange systems,
ment assessment and plane in collaboration with and e-prescribing.
the health care team and implementing this plan to
achieve patient-specific outcomes;
The following components of the encounter are essen-
Educating the patient/caregivers (both verbally and
tial to include in the documentation, which may be com-
in writing) to ensure understanding of the care plan,
municated in the form of a traditional SOAP (subjective
to optimize adherence, and to improve therapeutic
data, objective data, assessment, plan) note or other
outcomes; and
Establishing patient-specific measurable parame-
framework consistent with the standards of documenta-
ters and time frames for monitoringf and follow-up tion within the practice setting.
in collaboration with other members of the health
care team. A. Medication history
A brief summary of the patients past medication
D. Follow-up evaluation and medication monitoring use and related health problems as an introduc-
The clinical pharmacist performs follow-up evaluations tion to the documentation that will follow;
in collaboration with other members of the health care A listing of all current medications that includes
team to continually assess patient outcomes by: information regarding actual use, adherence, and
Coordinating with other providers to ensure that pa- attitudes toward therapy; and
tient follow-up and future encounters are aligned with A listing of medication-related allergies and any
the patients medical and medication-related needs; adverse drug events that may affect prescribing
Revisiting the medical record to obtain updates and monitoring or preclude the future use of a
on the clinical status of the patient and then medication.
e
A comprehensive medication management plan relies on coordinated, team-based collaboration to initiate, modify, monitor, and/or
discontinue medication therapy. Implementation of components of this plan may be delegated to the clinical pharmacist through a col-
laborative drug therapy management agreement or other formalized management protocol.
f
In many settings, the clinical pharmacist will use tools that facilitate his/her monitoring of the patient (e.g., monitoring forms, flow
sheets, and other aids to closely track and organize patient-specific data and/or data sets).
Standards of Practice for Clinical Pharmacists 2 American College of Clinical Pharmacy
B. Active problem list with assessment of each problem B. Consistent participation in continuing professional
A listing of current health conditions and sup- development (CPD) activities that enhance direct
porting data for the status of each condition, em- patient care practice abilities; and
phasizing associated medications and medica-
tion-related problems that may have an impact C. Maintenance of active licensure, including required
on desired goals; and continuing pharmacy education activities, through
A listing of any additional medication-related the appropriate state board(s) of pharmacy.
problems or other medical issues that may be un-
related to current health conditions. Clinical pharmacists also pursue professional and career
development by participating in formal and informal ac-
C. Plan of care to optimize medication therapy and tivities that enhance research and scholarship, teaching,
improve patient outcomes leadership, and/or management.
The specific medication therapy plan that has been
or will be implemented collaboratively by the health VI. Professionalism and Ethics
care team, including drug, dose, route, frequency,
and relevant monitoring parameters; and
Clinical pharmacists have a covenantal, fiducial rela-
The collaborative plan for follow-up evaluation
tionship with their patients. This relationship relies on
and monitoring as well as future visits.
the trust placed in the clinical pharmacist by the patient
and the commitment of the clinical pharmacist to act in
IV. Collaborative, Team-Based Practice and the best interest of individual patients and patient pop-
Privileging ulations, within the context of legal and ethical parame-
ters. Clinical pharmacists exhibit the traits of profession-
Clinical pharmacists work with other health professionals alism: responsibility, commitment to excellence, respect
as members of the health care team to provide high-quali- for others, honesty and integrity, and care and compas-
ty, coordinated, patient-centered care.5 They establish writ- sion.7 They subscribe to the pharmacy professions code
ten collaborative drug therapy management (CDTM) agree- of ethics and adhere to all pharmacist-related legal and
ments with individual physicians, medical groups, or health ethical standards.
systems and/or hold formally granted clinical privileges from
the medical staff or credentialing system of the organization
in which they practice.4 These privileging processes, togeth- VII. Research and Scholarship
er with the applicable state pharmacy practice act, confer
certain authorities, responsibilities, and accountabilities to Clinical pharmacists support and participate in research
the clinical pharmacist as a member of the health care team and scholarship to advance human health and health
and contribute to the enhanced efficiency and effectiveness care by developing research questions; conducting or
of team-based care. participating in clinical, translational, and health servic-
es research; contributing to the evolving literature in ev-
V. Professional Development and idence-based pharmacotherapy; and/or disseminating
and applying research findings that influence the qual-
Maintenance of Competence
ity of patient care.
Clinical pharmacists maintain competence in clinical prob-
lem-solving, judgment, and decision-making; communica- VIII. Other Responsibilities
tion and education; medical information evaluation and
management; management of patient populations; and a Clinical pharmacists serve as direct patient care provid-
broad range of therapeutic knowledge domains.6 Clinical ers, but they may also serve as educators, researchers,
pharmacists maintain competency through: clinical preceptors/mentors, administrators, managers,
policy developers, and consultants. As the clinical phar-
A. Certification and maintenance of certification in macy discipline grows, it must continue to familiarize
the appropriate specialty relevant to their practice, more patients, families, caregivers, other health profes-
including those specialties recognized by the Board sionals, payers/insurers, health care administrators, stu-
of Pharmacy Specialties (BPS) or other nationally dents, and trainees with the full range of clinical phar-
recognized multiprofessional certifications; macists responsibilities.
Standards of Practice for Clinical Pharmacists 3 American College of Clinical Pharmacy
References
1. Patient-Centered Primary Care Collaborative. 6. Burke JM, Miller WA, Spencer AP, Crank CW, Adkins
The patient-centered medical home: integrating L, Bertch KE, et al. Clinical pharmacist competencies.
comprehensive medication management to optimize Pharmacotherapy 2008;28(6):806-15. Available from
patient outcomes resource guide, 2nd edition. http://www.accp.com/docs/positions/whitePapers/
Washington, DC: Patient-Centered Primary Care CliniPharmCompTFfinalDraft.pdf. Accessed March 24,
Collaborative; 2012. Available from http://www.pcpcc. 2014.
org/sites/default/files/media/medmanagement.pdf. 7. Roth MT, Zlatic TD. Development of student
Accessed March 24, 2014. professionalism. Pharmacotherapy 2009;29(6):749-
2. Mitchell P, Wynia M, Golden R, McNellis B, Okun S, 56. Available from http://www.accp.com/docs/
Webb CE, et al. Core principles & values of effective positions/whitePapers/devstuprof.pdf. Accessed
team-based health care. Washington, DC: Institute March 24, 2014.
of Medicine; 2012. Available from http://www.
nationalahec.org/pdfs/VSRT-Team-Based-Care- March 2014
Principles-Values.pdf. Accessed March 24, 2014.
3. American College of Clinical Pharmacy. The definition of Copyright 2014 by the American College of Clinical
clinical pharmacy. Pharmacotherapy 2008;28(6):817-8. Pharmacy.
Available from http://www.accp.com/docs/positions/
commentaries/Clinpharmdefnfinal.pdf. Accessed Cite as:
March 24, 2014.
4. American College of Clinical Pharmacy. Qualifications American College of Clinical Pharmacy. Standards of
of pharmacists who provide direct patient care: Practice for Clinical Pharmacists. Pharmacotherapy
perspectives on the need for residency training and 2014;34(8):794797. Available from http://www.accp.
board certification. Pharmacotherapy 2013;33(8):888- com/docs/positions/guidelines/StndrsPracClinPharm_
91. Available from http://www.accp.com/docs/positions/ Pharmaco8-14.pdf.
commentaries/Commntry_BOR_DPC_phar1285.pdf.
Accessed March 24, 2014.
5. Doherty RB, Crowley RA. Principles supporting dynamic Access this version online at:
clinical care teams: an American College of Physicians accp.com/standards
Position Paper. Ann Intern Med. Published online
17 September 2013 doi:10.7326/0003-4819-159-9-
201311050-00710. Available from http://annals.org/
article.aspx?articleid=1737233. Accessed March 24,
2014.
Standards of Practice for Clinical Pharmacists 4 American College of Clinical Pharmacy
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- SOP 4-1 Source DocumentationДокумент2 страницыSOP 4-1 Source DocumentationDayledaniel SorvetoОценок пока нет
- Medication SafetyДокумент114 страницMedication SafetyRobert Dominic Gonzales100% (2)
- ABC Quality and Patient Saftey Workshop FinalДокумент68 страницABC Quality and Patient Saftey Workshop Finalyousrazeidan1979Оценок пока нет
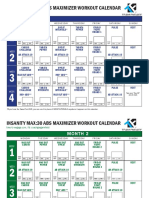
- Insanity Max30 ABS MAXIMIZER Calendar PDFДокумент2 страницыInsanity Max30 ABS MAXIMIZER Calendar PDFWilgab Urlanch67% (3)
- Nicholas E Davies Award of Excellence Organizational)Документ4 страницыNicholas E Davies Award of Excellence Organizational)Lohrhen Lheighh CahreeniyowОценок пока нет
- ISSUES IN INFORMATICS and NURSING INITIATIVESДокумент16 страницISSUES IN INFORMATICS and NURSING INITIATIVESFilamae Jayahr CadayОценок пока нет
- Max30 CalendarДокумент1 страницаMax30 CalendarSamarisyLeilaniОценок пока нет
- KREDENSIAL TENAGA GIZI - SuparmanДокумент39 страницKREDENSIAL TENAGA GIZI - SuparmanIndri TriantikaОценок пока нет
- Articulo 1Документ13 страницArticulo 1Wilgab UrlanchОценок пока нет
- Schedule 3 Black & WhiteДокумент2 страницыSchedule 3 Black & Whiteboris pocusОценок пока нет
- Diseño Racional de VacunasДокумент10 страницDiseño Racional de VacunasWilgab UrlanchОценок пока нет
- Teks Presentasi Maju BeДокумент3 страницыTeks Presentasi Maju BeGita FitrisiaОценок пока нет
- Clinical Audit Is A Process That Has Been Defined As "AДокумент8 страницClinical Audit Is A Process That Has Been Defined As "AAranaya DevОценок пока нет
- EHR Adoption in India: Potential and The ChallengesДокумент7 страницEHR Adoption in India: Potential and The Challengeskanthi056Оценок пока нет
- Critical - WorksheetДокумент3 страницыCritical - WorksheetQonita NahdiyahОценок пока нет
- List of TelemedicineДокумент9 страницList of TelemedicineRutvik ShuklaОценок пока нет
- E PrescribingДокумент6 страницE Prescribingapi-326037307Оценок пока нет
- 3-Article Text-7-123Документ10 страниц3-Article Text-7-123explore mojokertoОценок пока нет
- Evidence-Based Medicine: Tools, Techniques, ResultsДокумент42 страницыEvidence-Based Medicine: Tools, Techniques, ResultsPrimarini RiatiОценок пока нет
- Health Management Information Systems: Computerized Provider Order Entry (CPOE) Lecture BДокумент18 страницHealth Management Information Systems: Computerized Provider Order Entry (CPOE) Lecture BHealth IT Workforce Curriculum - 2012Оценок пока нет
- Prescription PadДокумент1 страницаPrescription Padrbostonvt1652Оценок пока нет
- TelemedicineДокумент12 страницTelemedicineapi-253509573Оценок пока нет
- PrescriptionДокумент55 страницPrescriptionAndrew Yoshihiro WiryaОценок пока нет
- PreskripsiДокумент80 страницPreskripsiIdfy BagusОценок пока нет
- G 3Документ17 страницG 3Bernadette Dangate MalbasОценок пока нет
- Wikipedia Handbook of Biomedical InformaticsДокумент802 страницыWikipedia Handbook of Biomedical InformaticsAndre Garcia100% (1)
- Electronic Health Records A General Overview PDFДокумент4 страницыElectronic Health Records A General Overview PDFDinda Fadhila SariОценок пока нет
- Kailash DCR SeptДокумент248 страницKailash DCR Septanon_146463611Оценок пока нет
- Introduction To Medical InformaticsДокумент24 страницыIntroduction To Medical InformaticscodyОценок пока нет
- PSQCMДокумент9 страницPSQCMapi-372034151Оценок пока нет
- CEBM Levels of Evidence 2.1Документ1 страницаCEBM Levels of Evidence 2.1Béla TóthОценок пока нет
- Definition of TermsДокумент6 страницDefinition of TermspattyreaganОценок пока нет
- Beban Kerja Subyektif Dan Obyektif Tenaga Farmasi PDFДокумент9 страницBeban Kerja Subyektif Dan Obyektif Tenaga Farmasi PDFUpitFlowОценок пока нет
- Nearest Pharmacy Delivery ServiceДокумент8 страницNearest Pharmacy Delivery ServiceRohana HkОценок пока нет
- Minimal Lower Layer ProtocolДокумент4 страницыMinimal Lower Layer Protocolxeon1976Оценок пока нет