Академический Документы
Профессиональный Документы
Культура Документы
Counseling
Загружено:
Irene Demegillo Salonga100%(2)100% нашли этот документ полезным (2 голоса)
763 просмотров5 страницCounseling
Авторское право
© © All Rights Reserved
Доступные форматы
DOC, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документCounseling
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
100%(2)100% нашли этот документ полезным (2 голоса)
763 просмотров5 страницCounseling
Загружено:
Irene Demegillo SalongaCounseling
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOC, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
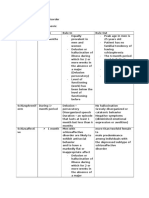
COUNSELING Interpretation
Dr. Agnes Segunda Gerasmo Confrontation
Information Giving
Counseling Summarizing
To give advise or opinion on what to Goal setting
do.
Dr. Rakel Family Practice emphasizes CIA- Client Centered
knowledge in such areas as Family Counseling
psychodynamics, interpersonal Catharsis- Ventilation Stage
relationship, counseling and Insight
supportive psychotherapy. Action
Dr. Engel- Biosphychosocial Model Based on Carl Rogers
Also called Client-centered
2 Types of Counseling counseling or patient-centered
couseling.
1. CIA- (Catharsis, Insight, Action)
Individual counselling, with Carl Rogers Basic Premise
psychosocial issues based on Carl Rogers Human Beings are essentially
rational, constructive, positive,
2. CEA- (Catharsis, Education, Action) independent, realistic, cooperative,
Individual or group counseling usually trustworthy, accepting, forward-
done on clinical consult moving and full of potential.
2 things necessary in counselling When there is a discrepancy between
actual self (described above), and the
1. Characteristic of a good counselor: perceived self- creates Misperception
Empathy Tension, Internal Confusion---ill
Unconditional Positive Regard Health.
Genuineness
The 3 main conditions can promote
Characteristic of Good Counselor: growth towards actual self and
improve communication.
a) Genuineness-
transparency, absence of Active Listening Skills
pretense. Skills used by the doctor-counselor to
b) Unconditional Positive regard- understand how the patient sees the
we can care for and accept the world and how he perceives the
confusion, fear, anger, loneliness, problematic reality for which he is
resentments of our client. consulting.
c) Empathy
ability to put oneself in the Active listening skills (Opening
situation of another. skills)
Attending Skills
2. Active Listening Skills Bracketing
Opening skill Leading
Attending Skills Reflecting
Bracketing Focusing
Leading Probing
Reflecting Summarizing
Focusing
Probing 1. Attending skills- paying attention,
Summarizing maintaining eye contact, nonverbals or the
verbals like saying yes or go on indicating
Closing skill that you are listening to the patient.
articulate into words patients emotions.
2. Bracketing -not so much a verbal or non- Giving name to feelings makes pt. more
verbal skill as it is a mental skill. aware of emotions.
Feelings not articulated and
3. Reflecting Skill- mirror reflecting back acknowledge have a way of taking
the image of the person gazing at it. A control of behavior.
patient who is emotionally burdened is also When feelings accurately reflected
unable to see himself clearly. back,
Example Reflecting skills: patient feels understood, rapport
(45/M walks in the office, sits down, improves.
stands up again and looks out the door Example:
to where his wife is sitting. He shuts Reflecting feeling: You seemed so anxious
the door and sits down again.) about your sore throat?
Patient: Doctor, a month ago, I had
this sore throat, so I went to a doctor C. Reflecting Experience
and he gave me penicillin for it. So I pointing out the non-verbals in order
took it for 7 days and it went away. for the patient to become aware of how he is
But a week later, I had sore throat behaving.
again. Example:
Reflecting Experience: I noticed that a
(patient shifts in his seats and looks while ago you looked out at the door at your
down at the floor.) wife and you shut it? Could you tell me
The doctor gave me amoxicillin this behind the action?
time and I took it and the sore throat
went away. But a few days ago
( patient takes his handkerchief and Leading
crumples it and pulls at it repeatedly)
The sore throat came back. 2 Kinds of Leading:
(Voice becomes softer; patient shakes 1. Indirect Lead- open invitation. Choice of
what to talk about depends on the patient.
his head).
Indirect leads take the form of words or
I just cant understand what is
phrases such as: Yes, Go on, And then?
happening.
2. Direct Lead- requires that the doctor-
counselor make a judgment call to where the
A. Reflecting content
patient should go.
verbal content is repackages or
rephrased to become clearer.:
Example:
a. Paraphrasing- putting to clearer
P: You see, we have been married for 5 yrs
words and
and we were okay most of the time but
summarizing what the patient is saying.
several months ago, I noticed she had been
b. Perception Check- use same words
less talkative and irritable and I got a hard
with that of the patient but putting is that it
time because she keeps on cutting me off.
at the end to confirm the counselors
D: Tell me more about how she cuts you off?
perception.
Example:
Focusing
Paraphrase: This is the 3rd time you
Asking the patient to prioritize his emotions
have had a sore throat within a month or identify which one is heavier or
and you dont understand why it keeps troublesome for him.
on coming back. Example:
Perception check: This is the 3rd D: You have financial difficulties, your wife is
time you have had a sore throat within nagging you, your daughter is rebellious, and
a month and you dont understand your son had an accident. But of this 4 which
why it keeps on coming back. Is that one gives you the most pressure.
it?
Probing
B. Reflecting Feeling
Probes are questions asked to elicit more P: I dont like selfish people.
information. D:Because?
They must be open-ended. You can P: Selfish people arent so popular
probe by beginning the questions with D: (I.Q.): So popularity is important to you;
What, Where, and when and how and if you are self-centered, people wont
Probe for the feeling rather than like you. Is that getting close to where you
content. are now?
Probe where the emotional content is
greatest, and watch out what the patient Interpretation as Fantasy or metaphor
decides to mention last or when patient Another form of interpretative
often repeats it. statements using fantasy or metaphor.
Example:
Active Listening skills (Closing Metaphor: I perceive you are like a puppet
with strings who conforms to what ever you
Skills)
are told to do.
Interpretation
Confrontation
2. Confrontation
Information Giving
This skill enables the doctor-counselor to
Summarizing challenge, discrepancies, distortions that the
Goal setting patient is using knowingly or unknowingly.
a. Challenging Discrepancies
b. Challenging Distortions.
1. Interpretation a. Challenging Discrepancies
An active process of explaining the Confrontation can be 0 in on
meaning of events that happened in discrepancies between what the patients
the patients life from the Doctor- thinks or feels and what he says and
counselor Frame of Reference. between what he says and what he does,
Interpretative Statements between his perception of himself and the
Interpretative questions perception of others regarding who he is,
Metaphor between what he is and what he dreams to
be between his expressed values and actual
A. Interpretative statements. behavior.
It involves sharing your hunches
with the patient in declarative form Example:
Jenny says she feels happy and is contented
Example: with her current job and yet expresses that it
P: I hate the way I am being treated in this would be a lot better if she gets paid more
hosp. Just because I dont have enough and her boss would cut her some slack. She
money everyone feel they can bother me occasionally complains of the long hours.
anytime and insert all these needles. (She has this tired and faraway look and a
Sometimes I just feel like yelling at them all forced smile.)
to get lost. Challenge: Jen you say you are happy and
D: You feel very angry of the way you are content with your work yet I have listened a
being treated with less respect simply lot of your complaints about it. Also when
because you cannot pay. you say your happy your eyes still have this
tired and sad look. Im not truly certain if you
B. Interpretative questions are contented and happy.
The counselor who wants to confirm his
hunch uses questions. b. Challenging Distortions
Some patients find reality as harsh and very
Example: hard to face so they distort it in various
D: When are you going to be concerned ways.
about yourself too?
P: Thats selfish attitude. 3. Information Giving
D: So whats wrong with that? A. Advice Giving
Giving suggestions and Opinions based on Active listening skills used in clinical
experience. Useful in crisis situations when practice.
several people must cooperate to prepare Correcting of emotionally critical
patient for major readjustment. misperception, and medical misperceptions.
B. Informing 2 reasons for consult
Giving valid information based on 1. Physical illness
expertise. Biomedical aspect
Advise must be clear and relevant. 2. Impact of illness or consequence of
impact of illness or psychosocial aspect
4. Summarizing of illness.
Tying together into several statements
ideas and feelings to close the discussion. 3 Reasons why we have to deal with
Summaries are good way to close a Impact of illness:
session. 1. Biopsychosocial Approach
It is useful to the doctor to check if he has -gives importance to the unity of body,
grasped the full spectrum of the patients mind and social context.
message. Holistic Approach- addressing
Example: both the illness and impact of illness.
D: Youve been discussing about your Conventional method-
ideal jobs and what things you have liked pathophysiology and pharmacology.
and disliked about your work; Youve also 2. We cannot be cerebral when we are
talked about your plans of getting more emotional.
training. Are you ready to take a look at When our patients are anxious they find
some options in planning for a new it hard to listen to us.
career? 3. Emotions have their roots in the
D: Try to put it together briefly. Lets take a patients perception.
look at what we have accomplished so
far. How does that appear to you? Perceptions of patient incongruent
with the reality as the physician
5. Goal Setting perceives it is a misperception.
As a result of earlier processes both
doctor and patient has a clearer view of ECM- Emotionally Critical
what is happening and possible solutions Misperception- are
to the problem. This is a vital part of the misperceptions that are most-
counseling process since it enables the anxiety provoking.
patient to explore new behaviors to cope
and deal with the circumstances.
CEA
Specific and measurable Catharsis- purgation ventilation of and
Realistic emotions.
Hierarchical Education
Desired by the person and tailored to Action
him.
Frequently evaluated. CEA Principles:
George Engel Biopsychosocial
___________________________________________ model
Motivation for consult may be due to
CEA physical illness or the impact of that
Dr. Agnes Segunda Gerasmo illness.
So we must address both the physical
Catharsis and emotional impact of that illness.
Education Sir William Osler The good
Action physician cures sometimes, palliates
often, but comforts always.
2. What feelings came out when did thoughts
1. The doctor plays as a doctor counselor. came to your mind?
2. The doctor detects or identifies 3. What consequences of your illness makes
misperception on the diagnosis, disease you feel this way most?
process, treatment or prognosis. What is the worst thing that your illness
3. The doctor gives name or reflects back to can do to you?
the patient, what the patient feels for What is the result or outcome your illness
him/her to be aware. that you dread most? ( Emotionally Critical
Misperception)
Goal of CEA 4. Summarize the ECM and the emotions
Not to make patient fear the disease associated with it.
process, but rather for them to understand
and make clear the disease process. Education
He will have articulated and ventilated
When to use it: his emotions
If you perceive the patient to be anxious He has now enough space in his mind
or with medical misperceptions. to be able to listen.
Address the ECM or medical
Characteristic of Good Counselor: misperceptions.
1. Genuineness- Explain and discuss to allay emotions.
transparency, absence of pretense. Make comparison to make things
2. Unconditional Positive regard- clearer for the patient.
we can care for and accept the
confusion, fear, anger, loneliness, Tips in Educating:
resentments of our client. 1. Speak the language of the patient.
3. Empathy 2. Use the power of analogy.
ability to put oneself in the situation of 3. Use of anecdotes and personal
another. testimonies.
4. Misperceptions hidden under emotions
Active Listening Skills should be explored and corrected.
Skills used by the doctor-counselor to 5. Allaying of anxiety.
understand how the patient sees the world
and how he perceives the problematic reality Action
for which he is consulting.
Therapeutic Plans
1. Attending skills- paying attention,
Pharmacologic and non-pharmacologic
maintaining eye contact, nonverbals
Schedule date and other plans.
Catharsis
Feedback
1. Medical Knowledge- as a doctor
Ask how the patient feels.
a. Explore the patients health
understanding.
b. Identify medical misperception if
TEAM FIEL AND CO.
present (on diagnosis,treatment or
disease process.)
c. Identify Health Framework.
2. Emotional/Psychological aspect
Ventilation- as a counselor
a. Probing the patients feelings.
b. Identify the Emotionally Critical
Misperception
Steps in Catharsis
1. What came into your mind when you
started feeling your symptoms?
Вам также может понравиться
- ASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study GuideОт EverandASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study GuideОценок пока нет
- The Beginning Counselor's Survival Guide: The New Counselor's Guide to Success from Practicum to LicensureОт EverandThe Beginning Counselor's Survival Guide: The New Counselor's Guide to Success from Practicum to LicensureОценок пока нет
- Rights and Responsibilities in Behavioral Healthcare: For Clinical Social Workers, Consumers, and Third PartiesОт EverandRights and Responsibilities in Behavioral Healthcare: For Clinical Social Workers, Consumers, and Third PartiesОценок пока нет
- Handouts for Psychotherapy: Tools for helping people changeОт EverandHandouts for Psychotherapy: Tools for helping people changeРейтинг: 1 из 5 звезд1/5 (1)
- LMSW Exam Prep Pocket Study Guide: Intervention Methods and TheoriesОт EverandLMSW Exam Prep Pocket Study Guide: Intervention Methods and TheoriesОценок пока нет
- Problem-Solving Group Therapy: A Group Leader's Guide for Developing and Implementing Group Treatment PlansОт EverandProblem-Solving Group Therapy: A Group Leader's Guide for Developing and Implementing Group Treatment PlansРейтинг: 4.5 из 5 звезд4.5/5 (2)
- How to Make Group Psychotherapy Work: New Perspectives on Group TherapyОт EverandHow to Make Group Psychotherapy Work: New Perspectives on Group TherapyОценок пока нет
- How to Start a Private Practice in Mental Health CounselingОт EverandHow to Start a Private Practice in Mental Health CounselingРейтинг: 5 из 5 звезд5/5 (1)
- Counseling Issues: A Handbook for Counselors and PsychotherapistsОт EverandCounseling Issues: A Handbook for Counselors and PsychotherapistsРейтинг: 5 из 5 звезд5/5 (1)
- Cognitive Behavioral Therapy (CBT) for Depression, Anxiety, Phobias and Panic AttacksОт EverandCognitive Behavioral Therapy (CBT) for Depression, Anxiety, Phobias and Panic AttacksОценок пока нет
- The Therapist Writer: Helping Mental Health Professionals Get PublishedОт EverandThe Therapist Writer: Helping Mental Health Professionals Get PublishedОценок пока нет
- Psychotherapy with Adolescents and Their Families: Essential Treatment StrategiesОт EverandPsychotherapy with Adolescents and Their Families: Essential Treatment StrategiesОценок пока нет
- Annual Review of Addictions and Offender Counseling: Best PracticesОт EverandAnnual Review of Addictions and Offender Counseling: Best PracticesОценок пока нет
- Therapy and Beyond: Counselling Psychology Contributions to Therapeutic and Social IssuesОт EverandTherapy and Beyond: Counselling Psychology Contributions to Therapeutic and Social IssuesMartin MiltonОценок пока нет
- NATIONAL COUNSELOR EXAMINATION (NCE): Passbooks Study GuideОт EverandNATIONAL COUNSELOR EXAMINATION (NCE): Passbooks Study GuideРейтинг: 5 из 5 звезд5/5 (1)
- ASWB EXAMINATION IN SOCIAL WORK – INTERMEDIATE/MASTERS (ASWB/II): Passbooks Study GuideОт EverandASWB EXAMINATION IN SOCIAL WORK – INTERMEDIATE/MASTERS (ASWB/II): Passbooks Study GuideРейтинг: 2 из 5 звезд2/5 (1)
- Basic Counseling Techniques: A Beginning Therapist’S Toolkit (Third Edition)От EverandBasic Counseling Techniques: A Beginning Therapist’S Toolkit (Third Edition)Рейтинг: 3 из 5 звезд3/5 (1)
- Basic Counseling SkillsДокумент25 страницBasic Counseling SkillsAnkit_4668Оценок пока нет
- Therapist's Guide to Clinical Intervention: The 1-2-3's of Treatment PlanningОт EverandTherapist's Guide to Clinical Intervention: The 1-2-3's of Treatment PlanningРейтинг: 3.5 из 5 звезд3.5/5 (2)
- NCE Exam Prep 2019-2020: A Study Guide with 300+ Test Questions and Answers for the National Counselor ExamОт EverandNCE Exam Prep 2019-2020: A Study Guide with 300+ Test Questions and Answers for the National Counselor ExamРейтинг: 5 из 5 звезд5/5 (1)
- Therapy Interruptus and Clinical Practice, Building Client Investment from First Contact through the First SessionОт EverandTherapy Interruptus and Clinical Practice, Building Client Investment from First Contact through the First SessionОценок пока нет
- A Counseling Skills Primer: 3 Minute Microskills Videos for the Visual LearnerОт EverandA Counseling Skills Primer: 3 Minute Microskills Videos for the Visual LearnerРейтинг: 5 из 5 звезд5/5 (1)
- Social Work Supervision in Practice: The Commonwealth and International Library: Social Work DivisionОт EverandSocial Work Supervision in Practice: The Commonwealth and International Library: Social Work DivisionОценок пока нет
- The “Family Interactive Rating Scale” a Therapy Tool for Working with Families: A Practice-Oriented Manual for Mental Health ProvidersОт EverandThe “Family Interactive Rating Scale” a Therapy Tool for Working with Families: A Practice-Oriented Manual for Mental Health ProvidersОценок пока нет
- Cognitive Behavioral Therapy: 10 Simple Guide To CBT For Overcoming Depression,Anxiety & Destructive ThoughtsОт EverandCognitive Behavioral Therapy: 10 Simple Guide To CBT For Overcoming Depression,Anxiety & Destructive ThoughtsОценок пока нет
- Certified Mental Health Counselor: Passbooks Study GuideОт EverandCertified Mental Health Counselor: Passbooks Study GuideОценок пока нет
- Psycho Therapy: Therapy Practices for the Mind, Body and EmotionsОт EverandPsycho Therapy: Therapy Practices for the Mind, Body and EmotionsОценок пока нет
- Therapist's Guide to Posttraumatic Stress Disorder InterventionОт EverandTherapist's Guide to Posttraumatic Stress Disorder InterventionОценок пока нет
- Group CounselingДокумент17 страницGroup CounselingnajarardnusОценок пока нет
- C6436 Individual Counseling Theory and Practices SUMMARYДокумент138 страницC6436 Individual Counseling Theory and Practices SUMMARYstarmania83167% (3)
- Counseling Session Summary Progress SOAPNotesДокумент2 страницыCounseling Session Summary Progress SOAPNotesmohd hafeez100% (1)
- Corey Powerpoints Theories (Outline Form)Документ36 страницCorey Powerpoints Theories (Outline Form)Terron Abner100% (14)
- Adlerian TherapyДокумент1 страницаAdlerian TherapyTinoRepaso100% (2)
- Counseling Theories ApproachesДокумент4 страницыCounseling Theories ApproachesCindy TanОценок пока нет
- Clinical Assessment Inteview, Steps To Psychological Assessment & Expression TechniquesДокумент3 страницыClinical Assessment Inteview, Steps To Psychological Assessment & Expression TechniquesAnthony Pangan100% (2)
- Summary of MedicationsДокумент1 страницаSummary of MedicationsIrene Demegillo SalongaОценок пока нет
- Review of Related LiteratureДокумент1 страницаReview of Related LiteratureIrene Demegillo SalongaОценок пока нет
- Cpm9th UtiДокумент29 страницCpm9th UtiIrene Demegillo SalongaОценок пока нет
- PRC Board Exam Schedule 2018Документ6 страницPRC Board Exam Schedule 2018TheSummitExpress0% (1)
- Pathophysiology of PneumoniaДокумент2 страницыPathophysiology of PneumoniaIrene Demegillo SalongaОценок пока нет
- After 2017Документ2 страницыAfter 2017NonoyTaclino100% (1)
- Digging Up The Bones - MicrobiologyДокумент31 страницаDigging Up The Bones - MicrobiologyMossa Di Base100% (1)
- Hiv 101Документ3 страницыHiv 101Irene Demegillo SalongaОценок пока нет
- Anemia Testing Algorithm PDFДокумент1 страницаAnemia Testing Algorithm PDFIrene Demegillo SalongaОценок пока нет
- Brief Psychotic Disorder DDДокумент3 страницыBrief Psychotic Disorder DDIrene Demegillo SalongaОценок пока нет
- Survival GuideДокумент69 страницSurvival GuideCharlene FernándezОценок пока нет
- Febrile Seizures PDFДокумент9 страницFebrile Seizures PDFIrene Demegillo SalongaОценок пока нет
- Physiology ReviewДокумент14 страницPhysiology ReviewIrene Demegillo SalongaОценок пока нет
- Cerebral PalsyДокумент3 страницыCerebral PalsyIrene Demegillo SalongaОценок пока нет
- Gender SensitivityДокумент4 страницыGender SensitivityIrene Demegillo SalongaОценок пока нет
- 12Lec-Pneumonia LocalДокумент21 страница12Lec-Pneumonia LocalIrene Demegillo SalongaОценок пока нет
- SGOP 2008 (Guidelines On Management)Документ87 страницSGOP 2008 (Guidelines On Management)Via Alip100% (1)
- A.H. CaseДокумент11 страницA.H. CaseIrene Demegillo SalongaОценок пока нет
- Hiv 101Документ3 страницыHiv 101Irene Demegillo SalongaОценок пока нет
- PTSD in DSM-5 Understanding The ChangesДокумент3 страницыPTSD in DSM-5 Understanding The ChangesIrene Demegillo SalongaОценок пока нет
- Menetrier DiseaseДокумент2 страницыMenetrier DiseaseIrene Demegillo SalongaОценок пока нет
- OB Case PreДокумент9 страницOB Case PreIrene Demegillo SalongaОценок пока нет
- Schizophrenia Psy Beh ActivityДокумент4 страницыSchizophrenia Psy Beh ActivityClancy Anne Garcia NavalОценок пока нет
- Brief Psychotic Disorder DDДокумент3 страницыBrief Psychotic Disorder DDIrene Demegillo SalongaОценок пока нет
- Case DiscussionДокумент7 страницCase DiscussionIrene Demegillo SalongaОценок пока нет
- Ingres in ReproductionДокумент20 страницIngres in ReproductionKarlОценок пока нет
- 20150714rev1 ASPACC 2015Документ22 страницы20150714rev1 ASPACC 2015HERDI SUTANTOОценок пока нет
- Millennium Development GoalsДокумент6 страницMillennium Development GoalsSasha Perera100% (2)
- Photoshoot Plan SheetДокумент1 страницаPhotoshoot Plan Sheetapi-265375120Оценок пока нет
- Marketing Plan Nokia - Advanced MarketingДокумент8 страницMarketing Plan Nokia - Advanced MarketingAnoop KeshariОценок пока нет
- English 8 q3 w1 6 FinalДокумент48 страницEnglish 8 q3 w1 6 FinalJedidiah NavarreteОценок пока нет
- Fractional Differential Equations: Bangti JinДокумент377 страницFractional Differential Equations: Bangti JinOmar GuzmanОценок пока нет
- Characteristics: Our in Vitro IdentityДокумент4 страницыCharacteristics: Our in Vitro IdentityMohammed ArifОценок пока нет
- Protected PCM USB Memory Sticks For Pa3X.Документ1 страницаProtected PCM USB Memory Sticks For Pa3X.mariuspantera100% (2)
- Machine Tools PDFДокумент57 страницMachine Tools PDFnikhil tiwariОценок пока нет
- ZyLAB EDiscovery 3.11 What's New ManualДокумент32 страницыZyLAB EDiscovery 3.11 What's New ManualyawahabОценок пока нет
- List of Practicals Class Xii 2022 23Документ1 страницаList of Practicals Class Xii 2022 23Night FuryОценок пока нет
- State Common Entrance Test Cell: 3001 Jamnalal Bajaj Institute of Management Studies, MumbaiДокумент9 страницState Common Entrance Test Cell: 3001 Jamnalal Bajaj Institute of Management Studies, MumbaiSalman AnwarОценок пока нет
- Video ObservationДокумент8 страницVideo Observationapi-532202065Оценок пока нет
- Market Structure and TrendДокумент10 страницMarket Structure and TrendbillОценок пока нет
- Jurnal Direct and Indirect Pulp CappingДокумент9 страницJurnal Direct and Indirect Pulp Cappingninis anisaОценок пока нет
- Deictics and Stylistic Function in J.P. Clark-Bekederemo's PoetryДокумент11 страницDeictics and Stylistic Function in J.P. Clark-Bekederemo's Poetryym_hОценок пока нет
- D2E133AM4701 Operating Instruction UsДокумент9 страницD2E133AM4701 Operating Instruction UsMohamed AlkharashyОценок пока нет
- Simple Past and Past Perfect TensesДокумент13 страницSimple Past and Past Perfect TensesSincerly RevellameОценок пока нет
- Reflection - Reading and Writing 3Документ3 страницыReflection - Reading and Writing 3Quỳnh HồОценок пока нет
- Boeing SWOT AnalysisДокумент3 страницыBoeing SWOT AnalysisAlexandra ApostolОценок пока нет
- Green ProtectДокумент182 страницыGreen ProtectLuka KosticОценок пока нет
- AJ IntroductionДокумент31 страницаAJ IntroductiontrollergamehuydkОценок пока нет
- F. Moyra Allen: A Life in Nursing, 1921-1996: Meryn Stuart, R.N., PH.DДокумент9 страницF. Moyra Allen: A Life in Nursing, 1921-1996: Meryn Stuart, R.N., PH.DRose Nirwana HandayaniОценок пока нет
- All About History History of Communism - 4th Edition 2022Документ148 страницAll About History History of Communism - 4th Edition 2022Duke100% (1)
- Nodal Analysis Collection 2Документ21 страницаNodal Analysis Collection 2Manoj ManmathanОценок пока нет
- Annotated Bibliography 2Документ3 страницыAnnotated Bibliography 2api-458997989Оценок пока нет
- EQUIP9-Operations-Use Case ChallengeДокумент6 страницEQUIP9-Operations-Use Case ChallengeTushar ChaudhariОценок пока нет
- Feature Glance - How To Differentiate HoVPN and H-VPNДокумент1 страницаFeature Glance - How To Differentiate HoVPN and H-VPNKroco gameОценок пока нет
- Pepsi Mix Max Mox ExperimentДокумент2 страницыPepsi Mix Max Mox Experimentanon_192325873Оценок пока нет
![ASWB EXAMINATION IN SOCIAL WORK [ASWB] (1 VOL.): Passbooks Study Guide](https://imgv2-2-f.scribdassets.com/img/word_document/402068986/149x198/afec08b5ad/1617230405?v=1)