Академический Документы
Профессиональный Документы
Культура Документы
CHF Oral Board Sheet
Загружено:
Kaitlyn Probasco0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров2 страницыCHF Oral Board Sheet
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документCHF Oral Board Sheet
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
26 просмотров2 страницыCHF Oral Board Sheet
Загружено:
Kaitlyn ProbascoCHF Oral Board Sheet
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 2
Congestive Heart Failure
Definition: Abnormality in heart structure or function resulting in (3) Cardiovascular
the inability to adequately perfuse metabolic tissues: (a) Myocardial hypertrophy with valvular
- Heart failure can be systolic or diastolic in origin regurgitation (preload) and HTN
(systolic dysfunction = failure of muscular pumping of ii) Eventual failure of compensatory mechanisms leads to
systole) decreased stroke volume and worsening of
(diastolic dysfunction = failure of relaxation and filling symptomatology
of the heart) 4) Signs
a) General:
1) Epidemiology i) Oliguria
a) 5 million people in the U.S. ii) Tachycardia
b) Incidence is increasing iii) HOTN
c) Prevalence increases with age iv) Decreased peripheral pulses
i) 75% are 65 yrs v) Narrow pulse pressure
d) Gender: men > women vi) Severe: cachexia, cyanotic, clubbing
e) Race: more prevalent in minorities b) Skin:
f) Risk factors i) Pallor
i) CAD: mc cause of HF ii) Cold/clammy extremities
ii) HTN iii) Diaphoresis
iii) DM c) Heart:
iv) Obesity i) Parasternal lift
v) Family hx ii) Enlarged apical impulse
iii) Diminished S1, S3 gallop
2) Etiology d) L:
a) Systolic dysfunction i) Crackles/rales at lung base
i) Ischemic damage: MI, cardiogenic shock ii) Pleural effusion
ii) Chronic pressure overload: HTN iii) S4
iii) Non ischemic - dilated cardiomyopathy e) R:
b) Diastolic dysfunction i) JVD
i) MC cause is systolic dysfunction ii) Abn V waves
ii) Myocardial hypertrophy secondary to HTN iii) Tender or NT hepatic congestion/enlargement
iii) Ischemic fibrosis, deposition Dz iv) Ascites
iv) Restrictive cardiomyopathy v) Pitting edema
c) Mechanical issues: valvular disease, congenital abs
d) arrhythmia 5) Symptoms
e) Pulmonary heart disease a) Left-sided HF
f) High output states (thyrotoxicosis, severe anemia) i) Fatigue
ii) SOB
3) Pathophysiology iii) Syncope
a) Systolic dysfunction from the above leads to impaired iv) Dyspnea at rest, DOE, exercise intolerance
myocardial contractility v) PND (paroxysmal nocturnal dyspnea)
i) EF falls to <40 left-sided HF vi) Orthopnea
b) Diastolic dysfunction from the above leads to increased vii) Chronic non-productive cough
ventricular stiffness or impaired myocardial relaxation viii) Nocturia
i) Preserved ejection fraction c right-sided HF
c) These changes stimulate compensatory responses: b) Right-sided HF possibly all of above sx PLUS
i) Frank-Starling Mechanism Compensatory i) Nausea, anorexia
mechanism leading to increase in preload ii) Peripheral edema (swollen ankles/feet) wt gain
(1) Neurohormonal
6) Diagnosis
(a) Epi /N-epi vasoconstriction
a) Labs
(b) plasma N-epi activates the SNS, causing i) CBC: anemia or hemochromatosis
renal hypoperfusion ii) Electrolytes: hyponatremia, hyperkalemia (unless on
(2) Renal thiazide diuretics, then hypokalemia)
(a) RAAS activation Na and H2O retention iii) LFTs: elevated liver enzymes
BP & vasoconstriction iv) TFTs: may have thyrotoxicosis
(b) Kidney baroreceptors that maintain CV v) RFTs to rule out kidney failure & get a baseline
vi) BNP: inc when ventricular pressures are high
homeostasis become desensitized
vii) Blood glucose and lipid panel
b) EKG: nonspecific findings
i) Arrhythmia, new or old MI, LVH
c) Imaging (3) If sx continue with ACE-I/ARB and BB
i) CXR (a) Digoxin 0.25mg/d PO
(1) Cardiomegaly
(2) B/L or right-sided pleural effusions e) Surgery
(3) Perivascular/interstitial edema (Kerley B lines) i) ICD (internal cardiodefibrillator) if LVEF < 30%
(4) Cephalization (vascular dilation) more than 40 days post-MI
(5) Alveolar fluid ii) If conduction abnormalities - resynchronization with
ii) Echo with doppler: to assess LV function (EF biventricular pacing abnormal
<40%) iii) If CAD - revascularization
iii) Stress imaging, angiography, or cardiac catheter to iv) Cardiac transplant if end stage disease plus:
assess cause or severity (1) < 70 years
(2) No evidence of:
7) Treatment (a) Permanent end organ dysfunction
a) Correct underlying causes (b) Cancer
b) Recording daily weight (>2 lbs in a day, >5 lbs above (c) Severe pulmonary hypertension
baseline call Dr.) (3) Have good social support and are compliant
c) Non-pharma - diet & exercise, wt. loss, stop smoking
d) Pharmacologic 8) Complications
i) Initial therapy for ALL: diuretic + ACE a) Organ failure kidney, liver
(1) Diuretics b) Ascites
(a) Thiazide diuretic - Hydrochlorothiazide 25- c) Pulmonary edema
100mg/d PO d) Arrhythmias
(b) If GFR < 30: Loop diuretic - Furosemide e) MI
20-320 mg/d PO f) Death 5 yr mortality is 50%
(2) ACE-I: LV remodeling and mortality 20%
(a) Lisinopril 10-40 mg/d PO
ii) Add-ons NYHA Classification
(1) If cough switch ACE-I for ARB I No limitation
(a) Losartan PO 25-100 mg/d II Slight limitation (sxs c moderate activity)
(2) If CAD/HTN/A-fib beta blocker III Marked limitation (sxs c mild activity)
(a) Metoprolol 25mg/d PO IV sxs at rest
Вам также может понравиться
- 3 - Important Topics For The AMC Part 1 MCQ CAT ExaminationДокумент23 страницы3 - Important Topics For The AMC Part 1 MCQ CAT ExaminationMohd FaizhakimОценок пока нет
- CardiologyДокумент4 страницыCardiologyES AbedОценок пока нет
- Review QuizДокумент107 страницReview QuizAhmad JalladОценок пока нет
- AMC Part 1 CAT MCQ Examination Important TopicsДокумент23 страницыAMC Part 1 CAT MCQ Examination Important TopicsSOMANATHAN UMAHSUTHANОценок пока нет
- Cardiology PDFДокумент27 страницCardiology PDFNada AKОценок пока нет
- 6 - Pericarditis & MyocarditisДокумент6 страниц6 - Pericarditis & MyocarditisAhmed AdelОценок пока нет
- SHOCKДокумент5 страницSHOCKSamridhi SrivastavaОценок пока нет
- Definition of Stroke: Risk FactorsДокумент12 страницDefinition of Stroke: Risk FactorsNik Fatnin YusoffОценок пока нет
- TCM3 Long Quiz 1-1Документ3 страницыTCM3 Long Quiz 1-1PARA SYTEОценок пока нет
- Express GI Notes 2012Документ31 страницаExpress GI Notes 2012Zul Azim AnuarОценок пока нет
- Pulmonary Valve Stenosis & RegurgitationДокумент5 страницPulmonary Valve Stenosis & Regurgitationwika.s1243Оценок пока нет
- MCQ Int - MedДокумент166 страницMCQ Int - MedOmar Ahmed100% (1)
- Recovery and ComplicationsДокумент36 страницRecovery and ComplicationsWalid KahinОценок пока нет
- MCQ IM DepДокумент183 страницыMCQ IM DepHesham A100% (3)
- Shock: DefinitionДокумент18 страницShock: DefinitionGaurav ChauhanОценок пока нет
- Theoretical Revision in 25 Days 2019Документ131 страницаTheoretical Revision in 25 Days 2019Sleman M BashirОценок пока нет
- Surgery II: Congenital Heart DiseaseДокумент10 страницSurgery II: Congenital Heart DiseaseRea Dominique CabanillaОценок пока нет
- 20-Feb-2023 at 2 - 11 - 12 PMДокумент37 страниц20-Feb-2023 at 2 - 11 - 12 PMmihikaОценок пока нет
- Management of Patientswith Complications From Heart DiseaseДокумент8 страницManagement of Patientswith Complications From Heart Diseasekristine keen buanОценок пока нет
- Shock, Acid-Base Balance and Fluid Therapy: Shock Stages of ShockДокумент4 страницыShock, Acid-Base Balance and Fluid Therapy: Shock Stages of ShockLonely WolfОценок пока нет
- TH Year Past Q InternalДокумент220 страницTH Year Past Q Internalibrahim 12Оценок пока нет
- Blood & HaematologyДокумент12 страницBlood & HaematologySagor DeyОценок пока нет
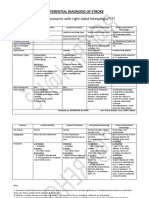
- Differential Diagnosis of StrokeДокумент2 страницыDifferential Diagnosis of StrokeAnonymous 7dsX2F8nОценок пока нет
- Echo Heart FailureДокумент82 страницыEcho Heart FailureJing CruzОценок пока нет
- General ExaminationДокумент2 страницыGeneral ExaminationYara WaelОценок пока нет
- Mphil Mid Term 1 With KeyДокумент3 страницыMphil Mid Term 1 With Keyasfandyar roghaniОценок пока нет
- Cardiovascular Pathology - 025) Valvular Heart Diseases Overview (Notes)Документ18 страницCardiovascular Pathology - 025) Valvular Heart Diseases Overview (Notes)Geraldine HernandezОценок пока нет
- CMSE 2019 Paper 1Документ26 страницCMSE 2019 Paper 1Sandip GaraiОценок пока нет
- Cardiology Revision DR - Ahmed MowafyДокумент35 страницCardiology Revision DR - Ahmed MowafyMohamed AlsaabОценок пока нет
- Cardiovascular NotesДокумент69 страницCardiovascular NotesAnnissaLarnardОценок пока нет
- NOTES - Heart FailureДокумент5 страницNOTES - Heart Failureeva halimОценок пока нет
- Aortic Valve RegurgitationДокумент3 страницыAortic Valve Regurgitationprakash ramОценок пока нет
- Cvspa07 Cardiac FailureДокумент6 страницCvspa07 Cardiac FailureRobert So JrОценок пока нет
- Heart FailureДокумент4 страницыHeart FailurersheedmahdiiОценок пока нет
- MCQ 1. Heart Sound Heart Sound S1 S2Документ7 страницMCQ 1. Heart Sound Heart Sound S1 S2Atirah AaОценок пока нет
- 200 Special Topics For 42 BCSДокумент187 страниц200 Special Topics For 42 BCSRezaul RazibОценок пока нет
- 2 Year 2 Term: PathophysiologyДокумент21 страница2 Year 2 Term: PathophysiologyMasyithah ZerlinaОценок пока нет
- Hings To Do: Tuesday, 28 October 2014 2:44 AmДокумент45 страницHings To Do: Tuesday, 28 October 2014 2:44 AmMital BhaktaОценок пока нет
- Chronic Liver DiseaseДокумент3 страницыChronic Liver DiseaseNikey LimОценок пока нет
- TH ND TH NDДокумент3 страницыTH ND TH NDSoumabho ParuiОценок пока нет
- 140 - Neurology Pathology) Seizures - Etiology, Pathophysiology, Clinical Features, Treatment, ComplicationsДокумент10 страниц140 - Neurology Pathology) Seizures - Etiology, Pathophysiology, Clinical Features, Treatment, ComplicationsUssama MDОценок пока нет
- Heart FailureДокумент1 страницаHeart FailureDarell M. BookОценок пока нет
- Triad of DeathДокумент4 страницыTriad of DeathHayudhiaОценок пока нет
- FCPS SurgeryДокумент106 страницFCPS Surgeryrehan hayderОценок пока нет
- Cvs Assesment 1 OrigkeyДокумент5 страницCvs Assesment 1 OrigkeydrashtisataОценок пока нет
- Atrial Fibrillation AtfДокумент11 страницAtrial Fibrillation AtfChristine MagnoОценок пока нет
- Aortic StenosisДокумент16 страницAortic StenosisAbdur RaqibОценок пока нет
- Hemodynamic DisorderДокумент7 страницHemodynamic DisorderYana MilyushinaОценок пока нет
- 150 Must Read Topics To Pass AMC MCQ CATДокумент4 страницы150 Must Read Topics To Pass AMC MCQ CATNomar Casiven NonatoОценок пока нет
- Cardiology DR - Ahmed MowafyДокумент150 страницCardiology DR - Ahmed MowafyMohamed AlsaabОценок пока нет
- 345 - Hematology Physiology) PolycythemiasДокумент3 страницы345 - Hematology Physiology) PolycythemiasAro DanaОценок пока нет
- Hemodynamic DisordersДокумент6 страницHemodynamic DisordersPradeep100% (1)
- Afmg Medicine Test+ 2023 1Документ6 страницAfmg Medicine Test+ 2023 1manishОценок пока нет
- MS Faculty Mock Test 1 Question PaperДокумент16 страницMS Faculty Mock Test 1 Question Paperbikalbelar123Оценок пока нет
- Pathophysiology CVA (Final2)Документ10 страницPathophysiology CVA (Final2)Jayselle Costes FelipeОценок пока нет
- Nigel Fong's MRCP NotesДокумент66 страницNigel Fong's MRCP Noteslucas0% (1)
- 10 CardiomyopathyДокумент71 страница10 CardiomyopathyAnonymous vUEDx8100% (5)
- THROMBOSISДокумент11 страницTHROMBOSISChandan DebbarmaОценок пока нет
- Dentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsДокумент4 страницыDentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsSasa AprilaОценок пока нет
- Serosal Appendicitis: Incidence, Causes and Clinical SignificanceДокумент3 страницыSerosal Appendicitis: Incidence, Causes and Clinical SignificancenaufalrosarОценок пока нет
- Letter Explanation To DoctorДокумент1 страницаLetter Explanation To DoctorDonnaОценок пока нет
- Exploratory Study of Self-Medication Practices Among StudentsДокумент5 страницExploratory Study of Self-Medication Practices Among StudentsN SОценок пока нет
- Carboplatin MonographДокумент9 страницCarboplatin Monographmerkuri100% (1)
- Test Bank For Medical Surgical Nursing 7th Edition Donna D IgnataviciusДокумент24 страницыTest Bank For Medical Surgical Nursing 7th Edition Donna D Ignataviciusrobertblackmwjkpnyfrq100% (37)
- Uterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateДокумент48 страницUterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateRuben Orduño RizoОценок пока нет
- Anti InflamasiДокумент27 страницAnti InflamasiAuLia DamayantiОценок пока нет
- Case Report Two Blue Chromhidrosis Patients in Emergency RoomДокумент2 страницыCase Report Two Blue Chromhidrosis Patients in Emergency RoomInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Children Complete QSTДокумент1 страницаChildren Complete QSTHoda AtwaОценок пока нет
- 4D CT With Respiratory GatingДокумент2 страницы4D CT With Respiratory GatingLaura Karina Sanchez ColinОценок пока нет
- OncologyДокумент3 страницыOncologyMichtropolisОценок пока нет
- Ebook Emergency Radiology The Requisites PDF Full Chapter PDFДокумент67 страницEbook Emergency Radiology The Requisites PDF Full Chapter PDFrobert.prinz849100% (22)
- TEACHING PLAN HypertensionДокумент2 страницыTEACHING PLAN Hypertensionpheochromocytoma59% (41)
- Approach To The Adult With Epistaxis - UpToDateДокумент29 страницApproach To The Adult With Epistaxis - UpToDateAntonella Angulo CruzadoОценок пока нет
- Departm Ent of Education: R e P U B Lic of Tlje JH JilippineffДокумент7 страницDepartm Ent of Education: R e P U B Lic of Tlje JH JilippineffJoyce CarilloОценок пока нет
- Hypertency Emergency Acute PDFДокумент12 страницHypertency Emergency Acute PDFmasdika09Оценок пока нет
- Rishum 1 262421216 2Документ1 страницаRishum 1 262421216 2HellcroZОценок пока нет
- Final Report Sero Survey0409Документ160 страницFinal Report Sero Survey0409BSL-2Оценок пока нет
- Grading Scale 2017 PDFДокумент2 страницыGrading Scale 2017 PDFAlibek ZhumanazarovОценок пока нет
- ATO - Compassionate - Release - of - SuperannuationДокумент5 страницATO - Compassionate - Release - of - SuperannuationBen RamalliОценок пока нет
- Seminar On Shock: IndexДокумент37 страницSeminar On Shock: IndexGayathri R100% (1)
- Common Dermatology Multiple Choice Questions and Answers - 6Документ3 страницыCommon Dermatology Multiple Choice Questions and Answers - 6Atul Kumar Mishra100% (1)
- Revisiting Structural Family TherapyДокумент2 страницыRevisiting Structural Family TherapyKim ScottОценок пока нет
- Clark 2004Документ18 страницClark 2004Joo XanderОценок пока нет
- GBS Source 1Документ4 страницыGBS Source 1PJHG50% (2)
- 30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFДокумент10 страниц30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFRicovially DavyaОценок пока нет
- M SДокумент162 страницыM SAnn Claudette SyОценок пока нет
- Subacute Bacterial Endocarditis and Antimicrobial ProphylaxisДокумент42 страницыSubacute Bacterial Endocarditis and Antimicrobial Prophylaxisalex-pham-2258Оценок пока нет
- Geriatric Medicine and Gerontology: Prevention of Frailty in The Elderly Through Physical Activity and NutritionДокумент8 страницGeriatric Medicine and Gerontology: Prevention of Frailty in The Elderly Through Physical Activity and NutritionSARAH AZIZAH 2015Оценок пока нет