Академический Документы
Профессиональный Документы
Культура Документы
04appendix 4 Conc Model
Загружено:
HY Hong YiИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
04appendix 4 Conc Model
Загружено:
HY Hong YiАвторское право:
Доступные форматы
SECTION I
A CONCEPTUAL MODEL OF COMMUNITY HEALTH
The way we define and measure individual and community health is evolving. Over the last
two decades, the definition of health itself has expanded from simply the absence of disease
to a state of complete physical, social, and mental well-being. This latter definition from the
World Health Organization was recast in the 1990s, and it proposed that health is the
degree to which individuals or groups are able to realize aspirations, satisfy needs, and cope
with a changing environment.1 Recognizing this evolution in our understanding of health is
important and suggests that adjustments are required to our methods of improving the
health of our community. Appropriate adjustments begin with acknowledging the many
factors in the physical, social, and individual environments that interact in complex ways to
govern and shape the health of individuals and communities.
Today researchers have developed new indicators of health status beyond standard
morbidity and mortality. Such indicators include the quality of life, burden of disease, years
lived with disability, and developmental delay. These health measures also reflect the
enormous change of disease patterns over the last century, from mostly infectious to mostly
chronic, as well as the migration of interventions upstream toward greater emphasis on
prevention and health promotion. Accordingly, a broad contextual framework or conceptual
model helps to clarify the relationships among a multitude of factors influencing the health
of a population. For agencies, organizations, and policymakers responsible for the health of
citizens and communities, a conceptual model can suggest different ways to leverage
resources and collaboration toward more substantial gains in health status. Such a broad
conceptual model for San Diego County is presented in this section.
MULTI-DETERMINANT MODEL OF HEALTH
Neither the process followed nor the components of the model proposed in this section are
new. In an effort to identify risk factors for disease and a host of social ills, researchers
have for many years investigated a multi-determinant model of community health. This
type of research has led to different adaptations of such models in various communities,
including variations of the personal health and well-being model depicted in Figure 1.
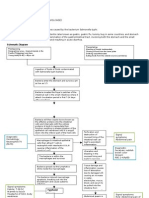
The Determinants of Health and Well-Being model, shown in Figure 1, depicts the various
determinants of health and suggests three ideas for the current discussion:
1. The relative influence of heredity, the environment, lifestyle choices, and health care
(institutional response) on health and well-being is not equal, as implied by the size of
the arrows. Clearly the environment (as defined by culture, socio-economics, prosperity,
employment) is the most significant determinant of health status. Subsequent
determinants might include the myriad of choices that individuals make concerning their
beliefs and behaviors.
2001 Community Health Needs Assessment
2. The two most malleable areas of influence relative to a community health response
include altering personal behaviors/attitudes and improving the institutions of health
care themselves. Although the model presented in this report concentrates on these
two areas, it does not theoretically exclude efforts to address determinants within the
environment.
3. The outer arrows represent the interconnected nature of the determinants. None exist
in isolation, for the relative impact for good or ill of each determinant is shaped by many
influences.
Figure 1. Determinants of Health and Well-Being
Population
Natural Cultural
Resources Systems
Heredity
Health &
Environment Health Care
Well-Being
Physical Prevention
Socio-cultural Treatment
Education Rehabilitation
Employment
Prosperity
Lifestyle
Behaviors
Attitudes
Ecological Human
Balance Satisfactions
Adapted from H.L. Blum, Planning for Health, 1981.
2001 Community Health Needs Assessment
ADAPTING THE MULTI-DETERMINANT MODEL FOR SAN DIEGO COUNTY
The method used to develop the model presented in this section was adapted from the
California Health Report2 published in 2000, and followed a 5-step process outlined below:
(1) (2) (3) (4) (5)
Array Aggregate risk Compare Identify high- Conduct
CHIP factors into critical behavioral/ leverage research
priority pathways according social risk health (HLH) for each
health to: factors by issues overall HLH sub-
issues by Environmental age group and narrow issue
age Behavioral/Social focus for
group Intermediate discussion
Outcomes
Step (1):
Array CHIPs Priority Health Issues by Age Group
The 1998 Needs Assessment made use of an extensive process to identify and prioritize
community health issues and indicators. This process involved: conducting 13 focus groups
with a cross-section of the community; assembling a comprehensive list of health issues;
categorizing health issues by age group (0-14, 15-24, 25-64, 65+); scoring each health
issue according to the size, seriousness, and community concern; and ranking health issues
overall by age group. From this process, 12 major health issues were identified, along with
several key indicators for each issue (See pp. 2-11 in the 1998 Report).
Development of the 2001 Needs Assessment involved a process for validating the priority
health issues by age group. The process included attending community forums and
reviewing their reports; selecting the top four priority health issues for each age group as
well as several overarching issues; surveying CHIP members regarding other possible
emerging health issues; and selecting one or two key indicators for each priority health
issue. Figure 2 lists the priority health issues and indicators reviewed in this report.
2001 Community Health Needs Assessment
Figure 2. Priority Heath Issues: Overarching and by Age Group with Selected Key
Indicators
Overarching
Priority Health Issue Key Indicator
1. Health Insurance Coverage Percent of adults and children with coverage
2. Dental Insurance Coverage Percent of adults and children with coverage
3. Usual Source of Medical Care Percent of adults and children with regular
primary care provider
4. Prenatal Care Percent of women initiating prenatal care in
1st trimester
0-14 Infants and Children
Priority Health Issue Key Indicator
1. Infant Health Low birth weight; infant mortality rate
2. Unintentional Injuries Rate of death due to drowning
3. Violent & Abusive Behaviors Rate of child abuse cases
4. Chronic & Disabling Conditions Rate of hospitalization for asthma; percent of
overweight children
15-24 Adolescents & Young Adults
Priority Health Issue Key Indicator
1. Substance Abuse Percent abusing tobacco, alcohol, drugs
2. Reproductive Health Teenage birth rate; percent having sexual
intercourse
3. Unintentional Injuries Motor vehicle mortality rate
4. Violent & Abusive Behaviors Homicide rate
5. Mental Health Percent attempting suicide
25-64 Adults
Priority Health Issue Key Indicator
1. Mental Health Rate of mental distress (depression/stress)
2. Substance Abuse Rate of drug-related mortality; percent
engaging in binge drinking; smoking
prevalence
3. Healthy Behaviors Percent not physically active; percent obese
4. Violent & Abusive Behaviors Domestic violence report rate
65+ Seniors
Priority Health Issue Key Indicator
1. Cardiovascular Disease Coronary heart disease mortality rate; stroke
mortality rate
2. Chronic & Disabling Conditions Diabetes mortality rate
3. Cancer Cancer mortality rate
4. Mental Health Suicide rate
5. Unintentional Injuries Mortality rates from fall
2001 Community Health Needs Assessment
Step (2):
Aggregate Risk Factors into Critical Pathways by Key Indicator
The framework for presenting the risk factors for each key indicator followed a structure,
process, and outcomes model. Risk factors are categorized and defined accordingly:
Structure = Environmental Risk Factors
Genetics, family history, race/ethnicity, age, gender
Social, cultural, and family functioning
Physical environment
Prosperity (employment, income)
Process = Behavioral + Societal Risk Factors
Personal behaviors/choices
Health status
Educational attainment
Accessibility of health and human services
Appropriateness and quality of health care
Outcomes = Intermediate Outcomes and Final Key Indicator
Morbidity
Prevalence of disease or unhealthy behaviors
For descriptive purposes, each key indicator (with its associated risk factors) was designated
a Critical Pathway a simple and illustrative representation of some of the major risk factors
associated with an outcome indicator. A critical pathway was developed for each key
indicator for the age group priority health issues. Although no critical pathways were
developed for the overarching health issues per se, they do emerge as risk factors within
the key indicators by age group. A general template for a critical pathway is described in
Figure 3, as well as 16 specific examples. Risk factors for each key indicator were obtained
from the scientific literature and publications from national public and private organizations.
Specific critical pathways by age group are presented on the following pages. Some
indicators are combined (e.g., teen use of tobacco, alcohol, marijuana), while some are
categorized as an intermediate outcome because they generally occur in a shorter period
of time than a key indicator event, thus they are termed intermediate.
Figure 3. Critical Pathway Template
Environmental Behavioral + Social Intermediate Final Key
Risk Factors Risk Factors Outcomes Indicator
E1 B1
E2 B2 IO1 I
E3 S1 IO2
E4 S2
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: INFANT HEALTH (Population: 0-14)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race /ethnicity
Maternal substance
Genetics/ family abuse
history
Lack of adequate Drug-exposed
Poverty social supports infants
Exposure to Maternal medical Low birth INFANT
environmental toxins complications weight MORTALITY
(e.g. Lead) RATE
Lack of appropriate Congenital
Young or old prenatal care anomalies
maternal age
Poor nutrition
Lack of adequate Limited maternal
transportation education
Critical Pathway: UNINTENTIONAL INJURIES (Population: 0-14)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Caregiver substance
abuse
Race/ethnicity Lack of adult
supervision
Young age
Lack of perceived
Rural vs. urban risk Near drowning RATE OF
location DROWNINGS
Lack of or
Lack of effective inappropriate use of
barriers to swimming flotation device
pools
Underestimation of
swimming/water
safety skills
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: VIOLENCE & ABUSE (Population: 0-14)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Young parents
Caregiver substance
abuse
Previous births
Unplanned or
unwanted
Poverty/low income pregnancy
Previous CHILD ABUSE/
Disabled children Poor coping skills abuse and NEGLECT CASE
child neglect RATE
Social / family Maternal depression
support network
Stressful life events
Single parents History of violence
Critical Pathway: CHRONIC CONDITIONS (Population: 0-14)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Urban location
Congenital anomalies Exposure to second
hand smoke Early childhood
Age of child (6 wheezing
months 3 years) Mental health
(depression) Low birth
Gender (males in weight
early years) Lack of appropriate (premature ASTHMA
medical care births)
Poverty/low income
Early allergen School
Parental asthma exposure absenteeism
due to asthma
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: SUBSTANCE ABUSE (Population: 15-24)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race/ethnicity Parental substance
abuse
Genetics/ family
history Poor peer role
models
Poverty/low income Life stress events PERCENT OF
HIGH SCHOOL
Mental health STUDENTS
Single parent (states of None identified USING
household depression, poor TOBACCO,
self image) ALCOHOL,
DRUGS
Learning disorders Media promotion
Parenting style
Accessibility of (under/over
substances controlling)
Critical Pathway: REPRODUCTIVE HEALTH (Population: 15-24)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race /ethnicity
Substance abuse
Poverty/low income Sexual abuse Early sexual
activity
Lack of supervision
Single parent Unprotected
household Depression & low intercourse TEENAGE
self esteem BIRTH RATE
Inappropriate media Previous
images pregnancy
Limited education
Negative peer
pressure
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: UNINTENTIONAL INJURIES (Population: 15-24)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Gender (males)
Substance abuse
Age (teens) Unsafe and
inexperienced
Driving Driving under MOTOR
Poor weather/ road the influence VEHICLE
conditions Failure to use RELATED
seatbelts Speeding DEATH RATE
unlawful
Vehicle defects Night time driving driving
Critical Pathway: VIOLENCE & ABUSE (Population: 15-24)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race/ethnicity
Substance abuse
Poverty/low income
Exposure to School
Urban location violence suspension/
expulsion HOMICIDE RATE
Lack of employment History of physical Juvenile arrest
abuse
Poor family
functioning Mental illness
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: MENTAL HEALTH (Population: 25-64)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race/ethnicity
Genetics/ family
history Substance abuse
Mental illness
Lack of appropriate Past suicide
Poverty/low income medical care attempts
Exposure to Depression SUICIDE RATE
Gender (male) violence
Frequent
Lack of employment Stressful events mental distress
Inappropriate
Poor social support medication
network
Critical Pathway: SUBSTANCE ABUSE (Population: 25-64)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Genetics/family
history Negative peer
pressure/poor role
models
Poverty/low income Rates of binge
Depression, poor drinking
self image DRUG-INDUCED
Lack of employment Smoking rates DEATH RATE
Social isolation
Media promotion Rates of illicit
Lack of education drug use
Accessibility of about consequences
substances
Poor family
functioning
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: UNHEALTHY BEHAVIORS (Population: 25-64)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Genetics/ family
history
Poor nutrition and
dietary habits Eating
Poverty/low income disorders PERCENT OF
ADULTS
Sedentary lifestyle Percent of PHYSICALLY
Poor family overweight or ACTIVE
functioning obese children
Media promotion of PERCENT OF
unhealthy foods Percent of OBESE ADULTS
physically
active children
Lack of education
Critical Pathway: VIOLENCE & ABUSE (Population: 25-64)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Poverty/Low Income
Substance Abuse
Gender (females) (alcohol abuse and
drugs)
Age (18-30)
Single, Separated,
Family Isolation Divorced Previous RATE OF
Lack of Social Domestic DOMESTIC
Support Pregnancy Disturbances VIOLENCE
Family History of Poor Self Esteem
Abuse
Lack of Education
Lack of Employment
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: CARDIOVASCULAR DISEASE (Population: 65+)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race /ethnicity Substance abuse
Cardiovascular
Poor nutrition disease
Genetics/ family
history Lack of physical Obesity rates CORONARY
inactivity HEART
Diabetes DISEASE
Poverty/low income Depression DEATH RATE
High blood
Stressful events pressure STROKE
Age (older) circumstances DEATH RATE
High
Lack of appropriate cholesterol
medical care
Critical Pathway: CHRONIC CONDITIONS (Population: 65+)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race /ethnicity Tobacco use
Genetics/ family Lack of physical
history activity
Obesity DIABETES
DEATH RATE
Poverty/low income Poor nutrition Diabetes
Lack of appropriate
Age >45 medical care
2001 Community Health Needs Assessment
Figure 3 (continued)
Critical Pathway: CANCER (Population: 65+)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Race/ethnicity Substance abuse
Genetics/ family Physical inactivity
history
Poor nutrition Lung cancer
Gender Overweight/ obesity Breast cancer CANCER
DEATH RATE
Use of Colon cancer
Older age (75+) contraceptives or
hormones Prostate
cancer
Exposure to Lack of appropriate
environmental toxins medical care
Critical Pathway: UNINTENTIONAL INJURIES (Population: 65+)
Environmental Risk Behavioral + Social Intermediate Key Indicator
Factors Risk Factors Outcomes
Cognitive
Unsafe home impairment
environment
Visual impairment
Older age (85+) Lack of appropriate Previous falls DEATH RATE
equipment within prior DUE TO FALLS
3 months
Neurological
disabilities (lack of
balance and
coordination)
2001 Community Health Needs Assessment
Step (3):
Compare Behavioral/Social Risk Factors by Age Group to Identify Meta-Risk Factors
Because environmental risk factors tend to be less amenable to change, they were not
analyzed in this report. All behavioral/social risk factors were compared to identify those
factors found in multiple critical pathways. Reoccurring behavioral/social risk factors
represent meta-risk factorsrisk factors that influence multiple health outcomes. This
comparative process yielded the following meta-risk factors by age group (Figure 4.).
Figure 4: Meta-Risk Factors by Age (years)
0-14 15-24 25-64 65+
Caregiver Parental Substance abuse Substance
substance abuse substance abuse abuse
Poor mental health
Maternal Poor mental (depression/isolation) Poor nutrition
depression health
(depression and Lack of access to Physical
Lack of self image) appropriate medical care inactivity
appropriate
medical care Poor nutrition Poor mental
including prenatal health
Physicial inactivity
care (sedentary lifestyle) Lack of
access to
appropriate
medical care
Step (4):
Identify High-Leverage Health (HLH) Issues Overall and Narrow Focus for Discussion
Review of the meta-risk factors by age group revealed common meta-risk factors across all
age groups. Because these risk factors appear in multiple pathways, effective intervention
strategies would theoretically impact multiple health outcomes. It is possible, therefore, to
view these meta-risk factors as leverage points targeted areas where improvement efforts
might yield the greatest potential gains to overall health status. Referred to as high-
leverage health (HLH) issues, the four common meta-risk factors can be categorized into
four HLH issues as:
1. Substance abuse
2. Mental health
3. Healthy behaviors
4. Access to appropriate medical care.
2001 Community Health Needs Assessment
It is important to keep in mind that the identification of HLH issues flows directly from a
particular selection of health issues and key indicators. The presentation of this process and
the resulting model are not intended to be authoritative nor scientifically evaluated, but
rather descriptive and informative.
Each HLH issue is too broad for a thorough discussion in this report. Consequently, the
Committee identified sub-issues for each HLH issue for specific review and discussion.
After first identifying common aspects for each HLH issue (e.g., common aspects of
mental health might include mental illness, depression, and poor self-image), the
Committee used the following criteria to select one aspect for in-depth discussion for
each HLH issue:
1. The topic is well researched in the scientific literature.
2. The sub-issue has a major impact on multiple health outcomes.
3. Discussion of the sub-issue could highlight opportunities for improvements for the
San Diego community.
4. There has not already been exhaustive discussion of or investment in the sub-issue.
Selected sub-issues are noted in bold italics in Figure 5.
Figure 5. High-Leverage Health Issues and Selected Sub-issues
Healthy Behaviors
Poor Lack of Adequate Poor stress
Diet/Nutrition Physical Activity Management
Substance Abuse
Tobacco Use Alcohol Abuse Illicit Drug Use
Mental Health
Depression Cognitive Impairment Poor Self Image
& Serious Mental Illness or Isolation
Access to Appropriate Medical Care
Outreach & Preventive Insurance Coverage System Complexity*
Services
* System complexity relates to the difficulty individuals often encounter when utilizing care or navigating various systems of
care.
2001 Community Health Needs Assessment
Step (5):
Conduct Research for Each Targeted HLH Sub-Issue
A summary investigation of each targeted HLH sub-issue is presented in Section II.
Although arguable, there is much evidence to suggest that not only are alcohol abuse,
depression, diet and physical activity, and system complexity important indicators to monitor
in and of themselves, but they are deep-rooted as causative agents within the behavioral
and social dimensions of our community and nation. These issues, both broadly (substance
abuse, mental health, healthy behaviors, and access to care) and particularly (alcohol
abuse, depression, diet & physical activity, system complexity), are among our communitys
most perplexing and persistent problems.
San Diego County is fortunate to have many local experts and organizations invested in
these issues. Although much of this information is known, what may be less understood is
the disproportionate burden these issues place on our community. This discussion is
intended to advance the community dialogue about this impact toward more solutions.
1
Young TK. Population Health, Concepts and Methods. New York: Oxford University Press, 1998.
2
Halfon N, & Ebener P. California Health Report. Santa Monica, CA: RAND Corporation, 2000.
2001 Community Health Needs Assessment
Вам также может понравиться
- Frequencies - ListДокумент171 страницаFrequencies - Listparamatman111199100% (3)
- Modul 7 - Behavioral DiagnosisДокумент19 страницModul 7 - Behavioral DiagnosisKaey Niezam100% (2)
- Emerging Viruses-AIDS & Ebola - Nature, Accident or IntentionalДокумент17 страницEmerging Viruses-AIDS & Ebola - Nature, Accident or IntentionalJamshaidzubairee100% (3)
- Odontogenic Infection & Surgical ManagementДокумент296 страницOdontogenic Infection & Surgical ManagementYazid Eriansyah Pradanta100% (2)
- 1 HEALTH AND ILLNESS HandoutsДокумент5 страниц1 HEALTH AND ILLNESS HandoutsVanessa Mae IlaganОценок пока нет
- Pathophysiology of Typhoid Fever and Acute GastroenteritisДокумент3 страницыPathophysiology of Typhoid Fever and Acute Gastroenteritisteddydeclines14100% (5)
- Concept of Health and Disease PreventionДокумент51 страницаConcept of Health and Disease Preventionimranasif41Оценок пока нет
- Health, Wellness, and IllnessДокумент22 страницыHealth, Wellness, and Illnessjasnate84100% (1)
- Pulmonary Function Test (PFT)Документ24 страницыPulmonary Function Test (PFT)hm3398Оценок пока нет
- 99 Weight Loss Questions Answered 1 PDFДокумент54 страницы99 Weight Loss Questions Answered 1 PDFjasmineОценок пока нет
- Rhodiola RoseaДокумент8 страницRhodiola RoseapnutsterОценок пока нет
- Health and IllnessДокумент71 страницаHealth and IllnessLondho Londho100% (2)
- Module 2 Mental Health Awareness RevisedДокумент10 страницModule 2 Mental Health Awareness RevisedcОценок пока нет
- DermatosДокумент393 страницыDermatosJamish Andrew100% (2)
- NYU CSAAH Testimony Re: Jails PlanДокумент4 страницыNYU CSAAH Testimony Re: Jails PlanS SОценок пока нет
- Unit 1.1Документ40 страницUnit 1.1Sunil RupjeeОценок пока нет
- Concept of Health and DiseaseДокумент42 страницыConcept of Health and DiseaseMayuri PatelОценок пока нет
- CANCER NSG QuestionsДокумент43 страницыCANCER NSG QuestionsAnn Michelle Tarrobago83% (6)
- DKBM IndonesiaДокумент25 страницDKBM IndonesiaBagas Andriyono100% (1)
- Test Taking Strategies For The NCLEXДокумент6 страницTest Taking Strategies For The NCLEXRomel CunetaОценок пока нет
- Determinants of HealthДокумент30 страницDeterminants of HealthRuchi YadavОценок пока нет
- Concept of Health-PushkarДокумент31 страницаConcept of Health-PushkarReenaChauhanОценок пока нет
- Health ConceptДокумент9 страницHealth Conceptmizare29gОценок пока нет
- Epid Profile of HealthДокумент16 страницEpid Profile of HealthBENNY BIN BAKAR (ILKKMKUCHINGKEJURURAWATAN)Оценок пока нет
- Concept of HealthДокумент36 страницConcept of HealthRenuga SureshОценок пока нет
- Health and DiseasesДокумент31 страницаHealth and DiseasesShimmering MoonОценок пока нет
- PHS 2 Models and DeterminantsДокумент52 страницыPHS 2 Models and DeterminantsjОценок пока нет
- PBH101 - Lecture 1 - Concept of Health, Public Health and PHC - 2023 - SKMFДокумент40 страницPBH101 - Lecture 1 - Concept of Health, Public Health and PHC - 2023 - SKMFZahin KhanОценок пока нет
- Prelim Topic 1 IhcsДокумент27 страницPrelim Topic 1 IhcsKim T. EstimoОценок пока нет
- Social Determinants of HealthДокумент44 страницыSocial Determinants of HealthAlaa Abu AishehОценок пока нет
- Life Course Fact SheetДокумент2 страницыLife Course Fact Sheeteriquitomt6361Оценок пока нет
- Epidemiology Course. Lecture (Concepts of Health& Disease)Документ39 страницEpidemiology Course. Lecture (Concepts of Health& Disease)اسامة محمد السيد رمضانОценок пока нет
- Health and Illness: Ronarica B. Diones, RN, RM, ManДокумент78 страницHealth and Illness: Ronarica B. Diones, RN, RM, ManRuffa Mae CalimagОценок пока нет
- Social Pharmacy Chapter 1 Introduction To Social Pharmacy NotesДокумент9 страницSocial Pharmacy Chapter 1 Introduction To Social Pharmacy NotesAbhishek YadavОценок пока нет
- YAR - Konsep Sehat Dan Sakit 2020Документ48 страницYAR - Konsep Sehat Dan Sakit 2020Lala GooseОценок пока нет
- Factors That Influencing HealthДокумент10 страницFactors That Influencing Healthmeryati sinambelaОценок пока нет
- Determinants of HealthДокумент19 страницDeterminants of HealthDan CasuraoОценок пока нет
- Social PharmacyДокумент77 страницSocial Pharmacysanjeev khanalОценок пока нет
- Concept of Health & DiseaseДокумент46 страницConcept of Health & DiseaseAnonymous rNu1uWjweОценок пока нет
- Health Determinants by Rosemary C. AgboДокумент30 страницHealth Determinants by Rosemary C. AgboRosemaryОценок пока нет
- Faculty of Medicine and Surgery Community Medicine An Introduction Lecture OneДокумент56 страницFaculty of Medicine and Surgery Community Medicine An Introduction Lecture OneSAKARIYE MAXAMEDОценок пока нет
- Prof. Saman WimalasunderaДокумент47 страницProf. Saman WimalasunderaAbdus Subhan A TakildarОценок пока нет
- Determinants of Health: DR Amir Akbar Shaikh Asst. Prof (Head of Department) Community DentistryДокумент42 страницыDeterminants of Health: DR Amir Akbar Shaikh Asst. Prof (Head of Department) Community DentistryAriba AsifОценок пока нет
- M1U3 SolutionДокумент25 страницM1U3 SolutionaalaamahmoudОценок пока нет
- SDOHДокумент23 страницыSDOHNezer SorianoОценок пока нет
- C H N 2:levels of Clientele in CHN: IndividualДокумент5 страницC H N 2:levels of Clientele in CHN: IndividualFlorence NightingaleОценок пока нет
- Concept of Health and DiseaseДокумент43 страницыConcept of Health and DiseaseA.JONAH ELISA SHINYОценок пока нет
- Stress and Health InequitiesДокумент47 страницStress and Health InequitiesWala WalkОценок пока нет
- Unit 1 13.04.20Документ46 страницUnit 1 13.04.20Deepak GuptaОценок пока нет
- Modul 6 - Social Diagnosis Assessing Quality of Life ConcernsДокумент19 страницModul 6 - Social Diagnosis Assessing Quality of Life ConcernsKaey NiezamОценок пока нет
- CHN NotesДокумент17 страницCHN NotesporchisОценок пока нет
- Health Social Work - 2Документ89 страницHealth Social Work - 2Muktar AhmedОценок пока нет
- Promoting Mental HealthДокумент17 страницPromoting Mental HealthDavid LyeluОценок пока нет
- The Determinants of Health LanzaДокумент42 страницыThe Determinants of Health Lanzachelsea pasiahОценок пока нет
- Fundamentals of Nursing Practice PDFДокумент8 страницFundamentals of Nursing Practice PDFMing100% (1)
- Lecture 1 - Introduction HandoutsДокумент9 страницLecture 1 - Introduction HandoutsJessica ChowОценок пока нет
- Human Society Lecture 2Документ17 страницHuman Society Lecture 2Eunice KegyedaОценок пока нет
- Health and Safety EducationДокумент34 страницыHealth and Safety Educationakarsh.manjikan35007Оценок пока нет
- Health & WellbeingДокумент29 страницHealth & WellbeingTrinadia Utami100% (1)
- MATERI Keperawatan KomunitasДокумент19 страницMATERI Keperawatan KomunitasYetri MulizaОценок пока нет
- Man, Health, & Illness: InsertДокумент50 страницMan, Health, & Illness: InsertJan Oliver YaresОценок пока нет
- Introduction To Public Health ReviewerДокумент4 страницыIntroduction To Public Health ReviewerVianne TabiqueОценок пока нет
- Community HealthДокумент23 страницыCommunity HealthKakembo NoreenОценок пока нет
- Concepts of Health and IllnessДокумент35 страницConcepts of Health and IllnessDominic SantosОценок пока нет
- TM 9 - ECOLOGICAL - SOCIAL DETERMINANT OF HEALTH - PPTX - AutoRecoveredДокумент14 страницTM 9 - ECOLOGICAL - SOCIAL DETERMINANT OF HEALTH - PPTX - AutoRecoveredgedang gorengОценок пока нет
- Community by Haseeb 1203Документ14 страницCommunity by Haseeb 1203Haseeb MianОценок пока нет
- Askep Agregat Anak & Remaja Dalam KomunitasДокумент36 страницAskep Agregat Anak & Remaja Dalam KomunitasMuhammad Khatami DjabbarОценок пока нет
- Lesson 5 Epidemiology and Public Health For Med Students 2022-2023Документ62 страницыLesson 5 Epidemiology and Public Health For Med Students 2022-2023salemОценок пока нет
- 1.pengantar IKM& Paradigma SehatДокумент19 страниц1.pengantar IKM& Paradigma SehatLucky fazriyaniОценок пока нет
- Psychosocial Dynamic ManojДокумент37 страницPsychosocial Dynamic ManojVivion JacobОценок пока нет
- Palliative Care For Cancer Patients 8 May 2021Документ1 страницаPalliative Care For Cancer Patients 8 May 2021HY Hong YiОценок пока нет
- Ethics and EtiquetteДокумент7 страницEthics and EtiquetteHY Hong YiОценок пока нет
- Resume Standard DocxДокумент2 страницыResume Standard DocxHY Hong YiОценок пока нет
- Soal Respi 2010Документ41 страницаSoal Respi 2010Joseph ThanaОценок пока нет
- 2249 4425 1 SMДокумент15 страниц2249 4425 1 SMHY Hong YiОценок пока нет
- Dosing Interactions Contraindications Precautions: AdultДокумент2 страницыDosing Interactions Contraindications Precautions: AdultHY Hong YiОценок пока нет
- Differential Diagnosis of PULMONARY EDEMAДокумент3 страницыDifferential Diagnosis of PULMONARY EDEMAHY Hong YiОценок пока нет
- Laboratory Manual 1st WeekДокумент11 страницLaboratory Manual 1st WeekHY Hong YiОценок пока нет
- BISOPROLOLДокумент4 страницыBISOPROLOLHY Hong YiОценок пока нет
- Immune Responses To BacteriaДокумент2 страницыImmune Responses To BacteriaSophieStevensОценок пока нет
- Minor Thesis Guidelines Rev 2012Документ27 страницMinor Thesis Guidelines Rev 2012Dini PertiwiОценок пока нет
- Interplay of Market and Demand in MarketДокумент4 страницыInterplay of Market and Demand in MarketHY Hong YiОценок пока нет
- The Information Age in Which You Live Changing The Face of BusinessДокумент38 страницThe Information Age in Which You Live Changing The Face of BusinessHY Hong YiОценок пока нет
- The Information Age in Which You Live Changing The Face of BusinessДокумент38 страницThe Information Age in Which You Live Changing The Face of BusinessHY Hong YiОценок пока нет
- Pathophysiology of LeptospirosisДокумент26 страницPathophysiology of LeptospirosisHY Hong Yi0% (1)
- Garcinia Kola ThesisДокумент36 страницGarcinia Kola ThesisDdn RmaОценок пока нет
- Pediatric RadiographyДокумент31 страницаPediatric RadiographyHakim Abdul Pakaya100% (3)
- Glaucoma, Hyphema: Synonyms and Related Keywords: Hyphema, Microhyphema, Hemorrhage in The AnteriorДокумент22 страницыGlaucoma, Hyphema: Synonyms and Related Keywords: Hyphema, Microhyphema, Hemorrhage in The AnteriorWulandari EmyОценок пока нет
- Summary of Clinical Studies On ImmunocalДокумент20 страницSummary of Clinical Studies On Immunocalimmunotec100% (1)
- Assessment Breast. RleДокумент21 страницаAssessment Breast. RleMa phaz Magnaye0% (1)
- Rebozet Tykerb PDFДокумент33 страницыRebozet Tykerb PDFWinda AgustinaОценок пока нет
- LP Askep Hernia Inguinal DextraДокумент81 страницаLP Askep Hernia Inguinal Dextraicn8Оценок пока нет
- TOEFL Exercises by BarroneeДокумент73 страницыTOEFL Exercises by BarroneeRahmayantiYuliaОценок пока нет
- Nuclear OncologyДокумент33 страницыNuclear OncologyOvguOzenliОценок пока нет
- Anatomy Quiz 1Документ4 страницыAnatomy Quiz 1Jacob BorongОценок пока нет
- Acute Renal Failure-Step23C - 1Документ28 страницAcute Renal Failure-Step23C - 1DEBJIT SARKARОценок пока нет
- MaRS Advisory Services - Regenerative Medicine: Industry Briefing 2009Документ35 страницMaRS Advisory Services - Regenerative Medicine: Industry Briefing 2009HutsDMОценок пока нет
- The Vodka Diet Edit 12.20Документ114 страницThe Vodka Diet Edit 12.20Late Knight GamingОценок пока нет
- Brain Tumor SegmentationДокумент1 страницаBrain Tumor SegmentationHena UmarОценок пока нет
- Anabolic SteroidsДокумент8 страницAnabolic SteroidsSunilОценок пока нет
- Pemberton Sign in Diagnosis of Retrosternal GoiterДокумент3 страницыPemberton Sign in Diagnosis of Retrosternal GoiterRashmeeta ThadhaniОценок пока нет
- Foundation of Health Care and ServicesДокумент21 страницаFoundation of Health Care and ServicesAnnieska Maceda AldeОценок пока нет
- Poet Report: KRAS Testing For Colorectal CancerДокумент9 страницPoet Report: KRAS Testing For Colorectal CancerJohn KentОценок пока нет
- STD Pre TestДокумент2 страницыSTD Pre TestCrystal Ann Monsale TadiamonОценок пока нет
- DAFTAR PUSTAKA AripinДокумент2 страницыDAFTAR PUSTAKA AripinFerdy Ricardo SinagaОценок пока нет