Академический Документы
Профессиональный Документы
Культура Документы
Periodontal Infection
Загружено:
AmelyahАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Periodontal Infection
Загружено:
AmelyahАвторское право:
Доступные форматы
Epidemiology/Health Services Research
O R I G I N A L A R T I C L E
Periodontal Infection, Systemic
Inammation, and Insulin Resistance
Results from the continuous National Health and Nutrition
Examination Survey (NHANES) 19992004
RYAN T. DEMMER, PHD1 WILLIAM T. FRIEDEWALD, MD1,4 as a potential risk factor for insulin resis-
ANTHONY SQUILLARO, MPH1 DAVID R. JACOBS JR., PHD5,6 tance and T2DM development. This notion
2
PANOS N. PAPAPANOU, DDS, PHD MOSE DESVARIEUX, MD, PHD1,7 is bolstered by previous research suggest-
MICHAEL ROSENBAUM, MD3 ing a bidirectional relationship between-
periodontal disease and glycemic control
among individuals with diabetes (2,3).
OBJECTIVEdAdverse microbial exposures might contribute to diabetogenesis. We hypoth-
esized that clinical periodontal disease (a manifestation of microbial exposures in dysbiotic
However, research exploring periodontal
biolms) would be related to insulin resistance among diabetes-free participants. The roles of infection as a diabetes risk factor among
inammatory mediation and effect modication were also studied. diabetes-free adults has only been initiated
recently.
RESEARCH DESIGN AND METHODSdThe continuous National Health and Nutrition Two previous publications reported
Examination Survey 19992004 enrolled 3,616 participants (51% women) who received a peri- that the presence of periodontal disease
odontal examination and fasting blood draw. Participants were mean age (6 SD) 43 6 17 years and predicted 1) a twofold increase in incident
28% Hispanic, 52% Caucasian, 17% African American, and 3% other. Log-transformed values of the
homeostasis model assessment of insulin resistance (HOMA-IR) or HOMA-IR $3.30 (75th percen- T2DM during 20 years of follow-up in a
tile) were regressed across full-mouth periodontal probing depth (PD) levels using linear and logistic nationally representative sample of
models. White blood cell (WBC) count and C-reactive protein (CRP) were considered as either ;9,000 initially diabetes-free men and
mediators or effect modiers in separate analyses. Risk ratios (RRs) stem from marginal predictions women (4); and 2) an approximately
derived from the logistic model. Results were adjusted for multiple periodontal disease and insulin vefold increase in the progression of A1C
resistance risk factors. among 2,700 diabetes-free participants aris-
RESULTSdIn linear regression, geometric mean HOMA-IR levels increased by 1.04 for every
ing from a randomly selected population-
1-mm PD increase (P = 0.007). WBC mediated 6% of the association (P , 0.05). Among par- based sample (5). The latter publication also
ticipants with WBC #6.4 3 109, PD was unrelated to HOMA-IR $3.30. Fourth-quartile PD was reported that the infection-associated risk
associated with HOMA-IR $3.30 among participants with WBC .7.9 3 109; RR 2.60 (1.36 related to A1C progression was stronger
4.97) (P for interaction = 0.05). Findings were similar among participants with CRP .3.0 mg/L among participants with evidence of ele-
(P for interaction = 0.04). vated C-reactive protein (CRP) (5). These
studies were unable to specically examine
CONCLUSIONSdPeriodontal infection was associated with insulin resistance in a nationally
representative U.S. sample of diabetes-free adults. These data support the role of inammation as the association between periodontal disease
both mediator and effect modier of the association. and insulin resistance.
The potential for periodontal infec-
Diabetes Care 35:22352242, 2012 tions to contribute to insulin resistance
and overt T2DM is biologically plausible
T
ype 2 diabetes mellitus (T2DM) is a fasting plasma glucose secondary to insulin (2,6,7), and one specic causal pathway
prominent public health problem resistance and impaired pancreatic b-cell linking infections and T2DM risk is
(1) currently affecting at least 17.7 function. Adverse microbial exposures, chronically elevated systemic inamma-
million individuals in the U.S. The hall- such as those observed in dysbiotic peri- tion. Systemic inammation is known to
mark of T2DM is chronically elevated odontal biolms, have been suggested be elevated among participants with peri-
odontal infections and has also been
shown to predict the progression of insu-
c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c
lin resistance (8) as well as the develop-
From the 1Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, ment of T2DM (9,10).
New York; the 2Division of Periodontics, Section of Oral and Diagnostic Sciences, College of Dental
Medicine, Columbia University, New York, New York; the 3Division of Molecular Genetics, Departments of
In this study, we explored the associ-
Pediatrics and Medicine, Columbia University, New York, New York; the 4College of Physicians and ation between clinically assessed periodon-
Surgeons, Columbia University, New York, New York; the 5Division of Epidemiology and Community tal disease (a clinical manifestation of
Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota; the 6Department of adverse microbial exposures in dysbiotic
Nutrition, University of Oslo, Oslo, Norway; and 7INSERM, U738, Paris, France.
Corresponding author: Ryan T. Demmer, rtd2106@columbia.edu.
biolms) and insulin resistance in the
Received 11 January 2012 and accepted 12 May 2012. continuous National Health and Nutrition
DOI: 10.2337/dc12-0072 Examination Survey (NHANES). We also
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10 studied whether or not there was evidence
.2337/dc12-0072/-/DC1.
2012 by the American Diabetes Association. Readers may use this article as long as the work is properly
that systemic inammation either mediated
cited, the use is educational and not for prot, and the work is not altered. See http://creativecommons.org/ or modied the association between peri-
licenses/by-nc-nd/3.0/ for details. odontal disease and insulin resistance.
care.diabetesjournals.org DIABETES CARE, VOLUME 35, NOVEMBER 2012 2235
Periodontal infection and insulin resistance
RESEARCH DESIGN AND assessment of insulin resistance and natural logtransformed values were
METHODSdThe continuous NHANES (HOMA-IR) as previously described considered (no meaningful differences
began in 1999 and consists of six unique (15). In brief, HOMA-IR is dened as (in- were noted). Both arithmetic- and geo-
data sets that have been generated in 2-year sulin in mU/mL 3 glucose in mmol/L)/ metric-adjusted mean values of insulin
cycles (i.e., 19992000, 20012002, 2003 22.5. and HOMA-IR are presented in the re-
2004, 20052006, 20072008, and 2009 sults. All P values presented for linear
2010). The survey examines a nationally Risk factor assessments trend were based on models using a con-
representative sample of ;5,000 people A comprehensive set of questionnaires to tinuous periodontal exposure variable.
each year and collects a variety of health-re- assess risk factors relevant to both peri- Multivariable models were adjusted for
lated data via questionnaire, physical exam- odontal disease and insulin resistance was confounding by the following variables:
ination, and laboratory assessments. The administered. The demographic variables continuous age, poverty-to-income ratio,
current analysis uses the NHANES age, race/ethnicity, sex, education, and caloric intake, BMI, blood pressure, tri-
19992000, 20012002, and 2003 poverty-to-income ratio (calculated by glycerides, total cholesterol-to-HDL cho-
2004 cross-sections and includes n = dividing family income by the poverty lesterol ratio, and inammatory
3,616 diabetes-free men and women guidelines, specic to family size, as well biomarkers as well as race/ethnicity (His-
aged 2085 years who received a clinical as the appropriate year and state accord- panic, non-Hispanic white, non-Hispanic
periodontal examination and fasting glu- ing to Department of Health and Human black, or other), sex, education (,high
cose and insulin assessments. The Services guidelines) were collected. Be- school, high-school graduate, or .high
NHANES protocol was approved by the havioral risk factor assessments included school), smoking status (never, former,
National Center for Health Statistics insti- physical activity level, cigarette smoking or current in addition to pack-years),
tutional review board, and written in- duration and intensity, alcohol consump- physical activity level in the past 30 days
formed consent was obtained from all tion, and caloric intake. Waist, weight, (none, moderate, or vigorous), and alco-
participants. height, and blood pressure measurements hol consumption (drinks/day). Mediation
were performed by trained research assis- analyses were performed to estimate
Oral examination tants according to standardized pro- whether or not the association between
The NHANES oral health examination tocols. Triglycerides, total and HDL periodontal infection and insulin resis-
(OHE) has been previously described cholesterol, CRP, and white blood cell tance was mediated by inammatory bio-
(11,12). Trained dentists performed a (WBC) count were measured from fasting markers (i.e., WBC or CRP) (Table 1)
full-mouth tooth count as well as a peri- blood samples. (18). Interactions between either WBC
odontal examination according to a ran- or CRP and periodontal infection were
dom half-mouth method (excluding third Statistical analysis also examined. Categories of systemic in-
molars). Periodontal probing depth (PD) Survey procedures in SAS version 9.2 and ammation were based on either quartiles
and clinical attachment loss (AL) SAS-callable SUDAAN version 10 were of WBC or alternatively on CRP dened
measurements were performed at two used for all analyses. by the CDC/American Heart Association
sites per tooth (mid- and mesio-facial) in Periodontal disease was dened ac- (AHA) statement on inammatory mark-
the 19992000 cross-section (i.e., up to cording to quartiles of either mean full- ers in cardiovascular disease (19).
28 possible sites per participant). In the mouth PD or AL values to obtain a
20012002 and 20032004 periodon- balanced categorization of the periodon-
tal examinations, a third distal surface tal exposure and to enable the assessment RESULTS
(disto-facial) measurement was added. of dose responsiveness. The Centers
OHE 19992002 used National Institute for Disease Control and Prevention/ General characteristics
for Dental Research periodontal probes, American Academy of Periodontology Supplementary Table 1 presents general
and the 20032004 OHE used a techni- (CDC/AAP) working group denition characteristics of study participants both
cally similar Hu-Friedy PCP2 probe (12). was also considered (16). The outcomes weighted and unweighted to the U.S.
Both instruments were color banded with analyzed were fasting glucose, insulin, population. Before applying NHANES
PD graduations at 2, 4, 6, 8, 10, and 12 and HOMA-IR. The probability of weights, participants included in this
mm. When the examiner was equivocal as HOMA-IR $3.30 (the population- analysis were aged 44 6 17 years (age 6
to the best value to assign, measurements specic 75th percentile of HOMA-IR) SD) and 51% were women. Whites, His-
were rounded to the next lowest band. was regressed on quartiles of periodontal panics, and blacks represent 52, 28, and
Interexaminer reproducibility ranged disease in logistic regression models using 17% of the sample (3% reported other
from good to very good with k scores SAS PROC SURVEYLOGISTIC. PROC race/ethnicity). Participants had 28 teeth
ranging from 0.64 to 0.82 (11,12). RLOGIST in SUDAAN was used to obtain on average (including third molars), and
multivariable-adjusted risk ratios (RRs) the mean PD and mean AL values were
Fasting glucose and insulin from tted logistic regression models by 1.2 6 0.5 and 0.8 6 0.9 mm, respectively.
assessments obtaining point estimates of model- The cumulative prevalence estimates of
Fasting glucose and insulin were mea- adjusted RRs as functions of average mar- moderate or severe periodontitis were 11
sured at the same central laboratory. ginal predictions (17). Linear regression and 1%, respectively.
Glucose was determined according to a (SAS PROC SURVEYREG) modeled ei- Higher levels of PD were associated
hexokinase enzymatic method (13) and ther the mean values of continuous glu- with several demographic, SES, and life-
insulin according to a radioimmunoassay cose, insulin, or HOMA-IR across style variables as summarized in Supple-
(14). Glucose and insulin were used to quartiles of periodontal disease. For insu- mentary Table 1, and although many of
calculate the homeostasis model lin and HOMA-IR, both untransformed these associations were statistically
2236 DIABETES CARE, VOLUME 35, NOVEMBER 2012 care.diabetesjournals.org
Demmer and Associates
Table 1dInammatory mediation of the association between periodontal infection and insulin resistance
White blood cell count
Effect Estimate SE T value P value Lower 95% CL Upper 95% CL
a (exposuremediator) 0.21006 0.08121 2.59 0.01 0.05089 0.36923
b (mediatoroutcome) 0.02894 0.00594 4.87 ,0.0001 0.01730 0.04059
c (total effect) 0.09527 0.03110 3.06 0.0037 0.03431 0.15622
c9 (direct effect) 0.08919 0.03090 2.88 0.0061 0.02862 0.14975
ab (mediated effect) 0.00608 0.00266 NA ,0.05 0.00087 0.01129
ab/c (WBC proportion mediated) = 6.4%
CRP
Effect Estimate SE T value P value Lower 95% CL Upper 95% CL
a (exposuremediator) 20.02976 0.02881 21.03 0.3073 20.08624 0.02672
b (mediatoroutcome) 0.01606 0.01795 0.89 0.3758 20.01912 0.05124
c (total effect) 0.09527 0.03111 3.06 0.0037 0.03430 0.15623
c9 (direct effect) 0.09574 0.03100 3.09 0.0035 0.03498 0.15651
ab (mediated effect) 20.00048 0.00071 NA NS 20.00187 0.00091
ab/c (CRP proportion mediated) = 20.5%
Men and women (n = 3,616) aged 2085 years enrolled in the continuous NHANES 19992004. Estimates are derived from linear regression analyses modeling mean
periodontal PD as the exposure, WBC or CPR as the mediator, and HOMA-IR as the outcome. a, b, c, c9, and ab as described in MacKinnon (18). a is the regression
coefcient summarizing the association between exposure and mediator; b is the regression coefcient summarizing the association between mediator and outcome,
adjusted for exposure; c is the unadjusted regression coefcient summarizing the association between exposure and outcome (i.e., the total effect); c9 is the regression
coefcient summarizing the association between exposure and outcome adjusted for mediator; and ab is the cross product of a and b and represents the amount of the
association between exposure and outcome that goes through the mediator.
signicant in this large sample, trends PD increase (P = 0.007), and this nding 0.791.96), 1.34 (0.752.38), and 1.39
across PD quartiles were generally weak was similar when restricting the analysis (0.802.42). Similarly, ndings were con-
in comparison with trends across quar- to nonobese participants (regression co- sistent among nonobese participants as
tiles of AL. Mean age varied from 44 to efcient = 1.05; P = 0.006). well as never smokers; the respective RRs
45 years across PD quartiles (P for trend = Mean AL was not associated with comparing participants in the fourth versus
0.08), whereas mean age varied from 34 glucose, insulin, or insulin resistance. rst PD quartile were 1.21 (0.772.31)
to 56 years across AL quartiles (P , 0.01). Mean HOMA-IR values across quartiles (among nonobese participants) and 1.32
Similarly, mean pack-years in the rst ver- of AL were 2.00 6 0.06, 2.03 6 0.06, (0.881.99) (among never smokers).
sus fourth AL quartile varied from 2 to 12, 1.94 6 0.06, and 1.90 6 0.07 (P for linear
respectively (P , 0.0001), an increase trend = 0.53); glucose and insulin data are Inammatory mediation
threefold greater than observed for PD not shown. In linear regression analyses, there was
quartiles as described in Supplementary In fully adjusted logistic regression evidence that the association between PD
Table 1. models, a 1-mm increase in continuous and HOMA-IR was mediated by WBC.
The arithmetic mean 6 SD fasting PD was associated with an increased risk Mean PD was positively associated with
plasma glucose, insulin, and HOMA- of HOMA-IR $75th percentile: RR 1.24 both WBC and HOMA-IR. Further, WBC
IR values were 95 6 10 mg/dL and (95% CI 1.031.48); P for trend = 0.03. was positively associated with HOMA-IR
66 6 48 and 2.6 6 2.1 pmol/L. Geomet- Findings were consistent when consider- after adjustment for PD (Table 1). It was
ric mean values of insulin and HOMA-IR ing risk for HOMA-IR $75th percentile estimated that 6% of the total association
were 54 and 2.1 pmol/L, respectively. across quartiles of PD (Table 2). Mean AL between mean PD and HOMA-IR was
was not associated with elevated HOMA- mediated by WBC (P , 0.05) (Table 1).
Association between periodontal IR risk (Table 2). There was no evidence that CRP mediated
disease, glucose, insulin, and Relative to participants with no/mild the association between mean PD and
insulin resistance periodontitis, HOMA-IR risk was not in- HOMA-IR (Table 1).
Values of mean fasting glucose (mg/dL) 6 creased among participants with moderate
SE across quartiles of mean PD were periodontitis but was increased among Inammatory interaction
95.3 6 0.4, 94.8 6 0.4, 95.1 6 0.4, participants with severe periodontitis: RRs (effect modication)
and 95.3 6 0.4 (P for trend = NS). Geo- for moderate and severe periodontitis 0.85 PD was only associated with HOMA-IR in
metric mean values of insulin and (0.611.19) and 2.30 (1.274.15). the presence of elevated systemic inam-
HOMA-IR varied across PD quartiles Results were consistent among age- mation. For example, participants with
in a dose-responsive fashion (Fig. 1). In subgroups; the RRs for fourth versus rst both fourth-quartile PD and WBC values
multivariable linear regression analy- quartile of PD among participants aged (vs. rst-quartile PD and WBC) realized a
sis, geometric mean HOMA-IR levels in- 2039 (n = 1,732), 4059 (n = 1106), or 160% increase in the risk of HOMA-IR
creased by 1.04 for every 1 mm of mean $60 (n = 778) years were 1.25 (95% CI $75th percentile: RR 2.60 (95%
care.diabetesjournals.org DIABETES CARE, VOLUME 35, NOVEMBER 2012 2237
Periodontal infection and insulin resistance
associated with increased risk of ele-
vated fasting insulin and insulin resis-
tance in a dose-responsive fashion. In
the full sample, the risk of elevated
HOMA-IR increased by ;30% across
PD quartiles. There was only weak evi-
dence for mediation by systemic inam-
mation but much stronger support for the
hypothesis of a synergistic interaction be-
tween elevated systemic inammation
and periodontal status, such that peri-
odontal status was only associated with
insulin resistance among participants
with WBC $6.5 3 109 cells/L or CRP
$1.0 mg/L. All ndings remained after
comprehensive adjustment for demo-
graphics, health-related behaviors, sys-
temic inammation, smoking status, and
adiposity.
The current data support recently
published ndings that periodontal in-
fection might be a risk factor for the
development of T2DM. Previously pub-
lished prospective data from the Study of
Health in Pomerania (SHIP) demon-
strated that baseline periodontal status
predicted 5-year progression of A1C (5).
These SHIP data extended a previous
cross-sectional report of elevated A1C
levels among participants with periodon-
titis (20) as well as an earlier publication
from NHANES I reporting increased lev-
els of baseline periodontal disease to pre-
dict incident diabetes during two decades
of follow-up (4). Although a recent study
had equivocal ndings for incident dia-
betes in a Japanese population (21), the
mean follow-up time was only 6 years,
which limited the number of incident ca-
ses and minimized power to detect the
association observed. Collectively, these
earlier studies were limited by an inability
to address the potential role of insulin re-
sistance as a mechanistic explanation of
the aforementioned A1C change and in-
Figure 1dThe association between PD quartiles and geometric mean insulin (A) and geometric cident diabetes ndings.
mean HOMA-IR (B) values. Adjusted for age, sex, race/ethnicity, education level, smoking status, Chronic inammation is a plausible
activity level, BMI, total caloric intake, systolic blood pressure, total cholesterol-to-HDL cho- biological mechanism linking infections
lesterol ratio, and triglycerides. Men and women (n = 3,616) 2085 years of age enrolled in the and insulin resistance. Animal models
continuous NHANES 19992004. (A high-quality color representation of this gure is available have shown that inammatory cytokines,
in the online issue.) such as tumor necrosis factor-a (TNF-a),
can induce a state of insulin resistance
(22), possibly as a consequence of TNF-as
CI 1.364.97); P for interaction = 0.05 both mean PD values $50th percentile ability to interrupt serine phosphorylation
(Fig. 2). Similarly, the RR comparing par- and a CRP value .3.0 mg/L, correspond- of insulin receptor substrate-1 (23), and
ticipants with fourth-quartile PD and CRP ing to 20,519,829 diabetes-free adults. epidemiological data in humans have re-
.3.0 mg/L versus rst-quartile PD and Similarly, 24% (31,278,079) of U.S. peatedly shown inammation to be an
CRP ,1.0 mg/L was 2.22 (1.343.68); adults had both PD $50th and WBC independent risk factor for both insulin
P for interaction = 0.04 (Fig. 2). These nd- $50th percentile. resistance (8) and T2DM (9,10,24).
ings are generalizable to a sizable propor- There are many potential exogenous in-
tion of U.S. adults; after applying NHANES CONCLUSIONSdWe have found ammatory stimuli that might trigger in-
sampling weights, 16% of participants had periodontal PD, but not AL, to be positively ammatory responses, some of which also
2238 DIABETES CARE, VOLUME 35, NOVEMBER 2012 care.diabetesjournals.org
Demmer and Associates
Table 2dCumulative prevalence RRs (95% CI) for HOMA-IR 75th percentile by mean periodontal PD and AL categories
Periodontal disease Periodontal disease Periodontal disease Periodontal disease
Q1 Q2 Q3 Q4
Quartiles of mean PD
Model 19% (166/879)* 23% (212/929)* 26% (238/904)* 28% (254/904)* P for trend**
1 Ref 1.21 (0.951.54) 1.40 (1.051.88) 1.56 (1.182.07) 0.002
2 Ref 1.10 (0.841.44) 1.22 (0.891.68) 1.34 (0.981.83) 0.02
2b Ref 1.03 (0.771.38) 1.26 (0.921.73) 1.38 (0.981.92) 0.02
3 Ref 1.00 (0.771.30) 1.12 (0.821.53) 1.26 (0.941.68) 0.03
4 Ref 1.00 (0.771.30) 1.10 (0.811.51) 1.24 (0.921.65) 0.05
Quartiles of mean AL
21% (200/935)* 26% (257/974)* 25% (243/961)* 27% (255/953)*
1 Ref 1.24 (1.001.55) 1.25 (0.951.64) 1.25 (0.991.59) 0.10
2 Ref 1.17 (0.891.54) 1.20 (0.861.67) 1.09 (0.771.54) 0.51
2b Ref 1.16 (0.901.49) 1.28 (0.901.82) 1.20 (0.841.72) 0.28
3 Ref 1.11 (0.841.46) 1.19 (0.841.68) 1.05 (0.741.49) 0.73
4 Ref 1.10 (0.841.44) 1.20 (0.851.69) 1.03 (0.731.45) 0.91
Men and women (n = 3,616) aged 2085 years enrolled in the continuous NHANES 19992004. Model 1, crude; model 2, age, sex, race/ethnicity, education level,
smoking status, physical activity level, total energy intake, and BMI; model 2b, model 2 + poverty income ratio and pack-years of smoking (n = 478 missing poverty
and pack-years data); model 3, model 2 + systolic blood pressure, total cholesterol-to-HDL cholesterol ratio, and triglycerides; model 4, model 3 + WBC and high-
sensitivity CRP. *Crude cumulative prevalence of HOMA-IR $75th percentile. **P for linear trend derived from models using the continuous mean PD or AL
variables.
have been linked to insulin resistance and inammatory markers (WBC and CRP) pathogenic periodontal microbiota
diabetes development, such as air pollu- are simply surrogates of an underlying (32,33), might be more precise for out-
tion (25) and organic pollutants (26). Ac- genetic susceptibility to infection-induced comes that are acute and/or reversible
cordingly, periodontal infection has been insulin resistance. Unfortunately, more (34). The strong association between se-
repeatedly demonstrated to be associated advanced methods that could address vere periodontitis (dened according to
with elevated levels of systemic inamma- both mediation and interaction concur- recommendations from the CDC/AAP
tion (27), and periodontal therapy has rently (i.e., exposure-mediator interac- working group) (16) and insulin resis-
been shown to result in changes in sys- tions) in a complex sampling design tance is consistent with this line of think-
temic monocytic gene expression (28) as such as NHANES are not readily avail- ing because it not only requires clinical
well as decreases in systemic inammation able. Nevertheless, as these data are evidence of historical infection (i.e., peri-
(29,30) and insulin resistance (31). There- cross-sectional, results from such analy- odontal sites with high AL) but the de-
fore, it is plausible that insulin resistance ses are unlikely to add meaningful value nition also incorporates a measure of
might be reduced via appropriate anti-in- from the standpoint of causal inference. current disease (i.e., periodontal sites
fective/anti-inammatory periodontal Longitudinal studies that can more pre- with deep PD). In contrast, moderate pe-
therapy. cisely investigate the interplay between riodontitis, which does not require clini-
Despite strong biological plausibility, microbial exposures, inammatory re- cal signs of current disease, was unrelated
our current ndings provide only weak sponse, and insulin resistance are neces- to insulin resistance. The low prevalence
support for inammatory mediation. This sary. of severe periodontitis in these data pre-
might be due to the fact that our inam- The fact that PD, and not AL, was cluded exploration of inammatory in-
matory construct was limited in this associated with HOMA-IR is notable be- teractions.
analysis and importantly did not include cause it suggests that clinical indicators of The specicity of insulin resistance
TNF-a, which likely mischaracterizes any current infection and/or inammation are ndings to PD measures (as opposed to
true causal inammatory intermediates. more relevant when studying cross-sectional AL) is also notable because it minimizes
Alternatively, these data do strongly sup- associations between periodontal infection potential confounding. Factors such as
port the possibility of synergy between and insulin resistance. As previously dis- age and smoking are generally stronger
periodontal infection and systemic in- cussed, evidence of irreversible, historical risk factors for AL and radiographic bone
ammation, and this is unlikely to be a oral infection (e.g., AL) might be more loss but weaker risk factors for PD (35),
chance nding, as the results are statisti- informative when studying insidious and/ and the current data support this notion
cally signicant and based on a priori hy- or irreversible outcomes presumed to be (see RESULTS). Nevertheless, in these data,
potheses generated from previously partly caused by chronic infectious expo- even crude associations between AL and
published data (5). Although the biologi- sure. Alternatively, ephemeral measures, insulin resistance were weak and not dose
cal mechanisms that might underpin the such as PD, which are closely associated responsive.
observed interaction are not immediately with the presence of current periodontal The nding that increased levels of
obvious, it is possible that our crude inammation in response to potentially periodontal disease are associated with
care.diabetesjournals.org DIABETES CARE, VOLUME 35, NOVEMBER 2012 2239
Periodontal infection and insulin resistance
microbial exposures in dysbiotic peri-
odontal biolms. Previous studies have
included direct assessments of oral (39)
or gut (40) microbial exposures to study
either cardiovascular or obesity risk;
similar approaches can provide more
precise characterizations of infection
insulin resistance associations in future
studies. Consequently, our current nd-
ings may be attenuated due to a lack of
comprehensive information on micro-
bial exposures, both oral and otherwise.
The fact that these data are cross-sectional
is also a limitation, as we cannot infer
temporality.
We have found clinical measures of
periodontal infection to be associated
with elevated insulin resistance in a na-
tionally representative, population-based
sample of diabetes-free adult men and
women. The ndings remained after
comprehensive multivariable adjustment
and strongly suggest a synergistic inter-
action between oral infection and inam-
matory response. Future research that can
incorporate direct assessments of expo-
sure to periodontal bacterial species and
more comprehensive assessments of in-
ammation during longitudinal follow-
up is necessary for more direct causal
inference.
AcknowledgmentsdThis research was sup-
ported by National Institutes of Health grants
R00-DE-018739 (to R.T.D.) and R01-DE-
13094 (to M.D.). Additional funding support
was provided by a Calderone Research Award
from the Mailman School of Public Health,
Columbia University (to R.T.D.); a Pilot and
Feasibility Award to R.T.D. from the Diabetes
and Endocrinology Research Center, College
of Physicians and Surgeons, Columbia Uni-
versity (DK-63608); a Chair in Chronic Dis-
ease, cole des Hautes tudes en Sant
Publique, Paris, France (to M.D.); and a Mayo
Chair Endowment, School of Public Health,
University of Minnesota (to D.R.J.).
Figure 2dCumulative prevalence RRs (95% CI) for HOMA-IR $75th percentile across in- No potential conicts of interest relevant to
creasing levels of periodontal PD and either WBC count dened in quartiles (A) or CRP dened this article were reported.
via AHA categories (B) (19). Adjusted for age, sex, race/ethnicity, education level, smoking status, R.T.D. obtained and analyzed the data
activity level, BMI, systolic blood pressure, total cholesterol-to-HDL cholesterol ratio, and tri- and wrote the manuscript. A.S. analyzed the
glycerides. Men and women (n = 3,616) aged 2085 years enrolled in the continuous NHANES data and wrote the manuscript. P.N.P., M.R.,
19992000. W.T.F., and M.D. wrote, reviewed, and edited
the manuscript. D.R.J. analyzed the data and
wrote, reviewed, and edited the manuscript.
increased fasting insulin resistance is epidemiological studies for subjects of R.T.D. is the guarantor of this work and, as
such, had full access to all the data in the
meaningful for the prediction of future various ethnicities and a wide range of study and takes responsibility for the in-
T2DM development. Elevations in insu- glucose tolerance (38). tegrity of the data and the accuracy of the data
lin resistance have been repeatedly shown Our exposure was based on clini- analysis.
to be strong predictors of incident di- cally assessed measures of periodontal The authors thank Dr. Sharon Schwartz
abetes (36,37), and the HOMA-IR disease because these measures are man- (Columbia University) for her thoughtful re-
method has been validated for large ifestations of host response to adverse view of the manuscript.
2240 DIABETES CARE, VOLUME 35, NOVEMBER 2012 care.diabetesjournals.org
Demmer and Associates
References 14. Centers for Disease Control and Pre- type 2 diabetes: results from the SALIA
1. Wild S, Roglic G, Green A, Sicree R, King vention National Center for Health Sta- cohort study. Environ Health Perspect
H. Global prevalence of diabetes: esti- tistics. National Health and Nutrition 2010;118:12731279
mates for the year 2000 and projections Examination Survey 19992001 [Inter- 26. Lee DH, Lee IK, Jin SH, Steffes M, Jacobs DR
for 2030. Diabetes Care 2004;27:10471053 net]. Available from http://www.cdc.gov/ Jr. Association between serum concentrations
2. Taylor GW. Bidirectional interrelation- nchs/data/nhanes/nhanes_99_00/lab10am_ of persistent organic pollutants and insulin
ships between diabetes and periodontal met_insulin.pdf. Accessed 10 December resistance among nondiabetic adults: results
diseases: an epidemiologic perspective. 2011. from the National Health and Nutrition
15. Matthews DR, Hosker JP, Rudenski AS, Examination Survey 1999-2002. Diabetes
Ann Periodontol 2001;6:99112
Naylor BA, Treacher DF, Turner RC. Ho- Care 2007;30:622628
3. Lalla E, Papapanou PN. Diabetes mellitus
meostasis model assessment: insulin re- 27. Slade GD, Ghezzi EM, Heiss G, Beck
and periodontitis: a tale of two common
sistance and beta-cell function from JD, Riche E, Offenbacher S. Relation-
interrelated diseases. Nat Rev Endocrinol
fasting plasma glucose and insulin con- ship between periodontal disease and
2011;7:738748
centrations in man. Diabetologia 1985;28: C-reactive protein among adults in the
4. Demmer RT, Jacobs DR Jr, Desvarieux
412419 Atherosclerosis Risk in Communities
M. Periodontal disease and incident type
16. Page RC, Eke PI. Case denitions for use study. Arch Intern Med 2003;163:1172
2 diabetes: results from the First Na-
in population-based surveillance of peri- 1179
tional Health and Nutrition Examination
odontitis. J Periodontol 2007;78(Suppl.): 28. Papapanou PN, Sedaghatfar MH, Demmer
Survey and its epidemiologic follow-up
13871399 RT, et al. Periodontal therapy alters gene
study. Diabetes Care 2008;31:1373 17. Bieler GS, Brown GG, Williams RL, expression of peripheral blood mono-
1379 Brogan DJ. Estimating model-adjusted cytes. J Clin Periodontol 2007;34:736
5. Demmer RT, Desvarieux M, Holtfreter B, risks, risk differences, and risk ratios from 747
et al. Periodontal status and A1C change: complex survey data. Am J Epidemiol 29. DAiuto F, Parkar M, Andreou G, et al.
longitudinal results from the Study of 2010;171:618623 Periodontitis and systemic inammation:
Health in Pomerania (SHIP). Diabetes 18. MacKinnon DP. Introduction to Statistical control of the local infection is associated
Care 2010;33:10371043 Mediation Analysis. New York, Lawrence with a reduction in serum inammatory
6. Yki-Jrvinen H, Sammalkorpi K, Koivisto Erlbaum Associates, 2008. markers. J Dent Res 2004;83:156160
VA, Nikkil EA. Severity, duration, and 19. Pearson TA, Mensah GA, Alexander RW, 30. Tonetti MS, DAiuto F, Nibali L, et al.
mechanisms of insulin resistance during et al.; Centers for Disease Control and Treatment of periodontitis and endothe-
acute infections. J Clin Endocrinol Metab Prevention; American Heart Association. lial function. N Engl J Med 2007;356:
1989;69:317323 Markers of inammation and cardiovas- 911920
7. Genco RJ, Grossi SG, Ho A, Nishimura F, cular disease: application to clinical and 31. Sun WL, Chen LL, Zhang SZ, Wu YM, Ren
Murayama Y. A proposed model linking public health practice: a statement for YZ, Qin GM. Inammatory cytokines, adi-
inammation to obesity, diabetes, and healthcare professionals from the Centers ponectin, insulin resistance and metabolic
periodontal infections. J Periodontol for Disease Control and Prevention and control after periodontal intervention in
2005;76(Suppl.):20752084 the American Heart Association. Circula- patients with type 2 diabetes and chronic
8. Park K, Steffes M, Lee DH, Himes JH, tion 2003;107:499511 periodontitis. Intern Med 2011;50:1569
Jacobs DR Jr. Association of inammation 20. Wolff RE, Wolff LF, Michalowicz BS. A 1574
with worsening HOMA-insulin resistance. pilot study of glycosylated hemoglobin 32. Demmer RT, Papapanou PN, Jacobs DR
Diabetologia 2009;52:23372344 levels in periodontitis cases and healthy Jr, Desvarieux M. Bleeding on probing
9. Pradhan AD, Manson JE, Rifai N, Buring controls. J Periodontol 2009;80:1057 differentially relates to bacterial proles:
JE, Ridker PM. C-reactive protein, inter- 1061 the Oral Infections and Vascular Disease
leukin 6, and risk of developing type 2 21. Ide R, Hoshuyama T, Wilson D, Epidemiology Study. J Clin Periodontol
diabetes mellitus. JAMA 2001;286:327 Takahashi K, Higashi T. Periodontal dis- 2008;35:479486
334 ease and incident diabetes: a seven-year 33. Demmer RT, Papapanou PN, Jacobs DR
10. Hu FB, Meigs JB, Li TY, Rifai N, Manson study. J Dent Res 2011;90:4146 Jr, Desvarieux M. Evaluating clinical
JE. Inammatory markers and risk of de- 22. Ling PR, Bistrian BR, Mendez B, Istfan periodontal measures as surrogates for
veloping type 2 diabetes in women. Di- NW. Effects of systemic infusions of bacterial exposure: the Oral Infections
abetes 2004;53:693700 endotoxin, tumor necrosis factor, and and Vascular Disease Epidemiology Study
11. Dye BA, Barker LK, Selwitz RH, et al. interleukin-1 on glucose metabolism (INVEST). BMC Med Res Methodol 2010;
Overview and quality assurance for the in the rat: relationship to endogenous 10:2
National Health and Nutrition Examina- glucose production and peripheral tis- 34. Demmer RT, Kocher T, Schwahn C,
tion Survey (NHANES) oral health com- sue glucose uptake. Metabolism 1994; Vlzke H, Jacobs DR Jr, Desvarieux M.
ponent, 1999-2002. Community Dent 43:279284 Rening exposure denitions for
Oral Epidemiol 2007;35:140151 23. Hotamisligil GS, Peraldi P, Budavari A, studies of periodontal disease and sys-
12. Dye BA, Nowjack-Raymer R, Barker LK, Ellis R, White MF, Spiegelman BM. IRS- temic disease associations. Community
et al. Overview and quality assurance for 1-mediated inhibition of insulin receptor Dent Oral Epidemiol 2008;36:493
the oral health component of the National tyrosine kinase activity in TNF-alpha- and 502
Health and Nutrition Examination Survey obesity-induced insulin resistance. Sci- 35. Grossi SG, Zambon JJ, Ho AW, et al. As-
(NHANES), 2003-04. J Public Health ence 1996;271:665668 sessment of risk for periodontal disease. I.
Dent 2008;68:218226 24. Pradhan AD, Cook NR, Buring JE, Risk indicators for attachment loss. J Peri-
13. Centers for Disease Control and Prevention Manson JE, Ridker PM. C-reactive protein odontol 1994;65:260267
National Center for Health Statistics. Na- is independently associated with fasting 36. Hanley AJ, Williams K, Gonzalez C, et al.;
tional Health and Nutrition Examination insulin in nondiabetic women. Arte- San Antonio Heart Study; Mexico City
Survey 19992001 [Internet]. Available rioscler Thromb Vasc Biol 2003;23:650 Diabetes Study; Insulin Resistance Ath-
from http://www.cdc.gov/nchs/data/nhanes/ 655 erosclerosis Study. Prediction of type 2
nhanes_99_00/lab10am_met_plasma_ 25. Krmer U, Herder C, Sugiri D, et al. diabetes using simple measures of insulin
glucose.pdf. Accessed 10 December 2011. Trafc-related air pollution and incident resistance: combined results from the San
care.diabetesjournals.org DIABETES CARE, VOLUME 35, NOVEMBER 2012 2241
Periodontal infection and insulin resistance
Antonio Heart Study, the Mexico City a multiethnic population: the Insulin Re- the oral infections and vascular disease
Diabetes Study, and the Insulin Re- sistance Atherosclerosis Study. Diabetes epidemiology study (INVEST). J Hypertens
sistance Atherosclerosis Study. Diabetes Care 2010;33:6772 2010;28:14131421
2003;52:463469 38. Wallace TM, Levy JC, Matthews DR. Use 40. Turnbaugh PJ, Ley RE, Mahowald MA,
37. Lorenzo C, Wagenknecht LE, DAgostino and abuse of HOMA modeling. Diabetes Magrini V, Mardis ER, Gordon JI. An
RB Jr, Rewers MJ, Karter AJ, Haffner SM. Care 2004;27:14871495 obesity-associated gut microbiome with
Insulin resistance, beta-cell dysfunction, 39. Desvarieux M, Demmer RT, Jacobs DR Jr, increased capacity for energy harvest.
and conversion to type 2 diabetes in et al. Periodontal bacteria and hypertension: Nature 2006;444:10271031
2242 DIABETES CARE, VOLUME 35, NOVEMBER 2012 care.diabetesjournals.org
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Rorschach Inkblot TestДокумент19 страницRorschach Inkblot Testiqra urooj100% (6)
- Short Essay On ObesityДокумент6 страницShort Essay On ObesityLisa Wong100% (1)
- What Is FOCUS CHARTINGДокумент38 страницWhat Is FOCUS CHARTINGSwen Digdigan-Ege100% (2)
- 2022 Mart YÖKDİL YÖKDİL - Fen BilimleriДокумент17 страниц2022 Mart YÖKDİL YÖKDİL - Fen BilimleriErdal Bozkurt100% (2)
- DLL - Mapeh 6 - Q4 - W6Документ4 страницыDLL - Mapeh 6 - Q4 - W6Bernard Martin100% (1)
- Med Tech LawsДокумент78 страницMed Tech LawsMarie LlanesОценок пока нет
- Summary Report On Health and HygieneДокумент4 страницыSummary Report On Health and HygieneVisal ShresthaОценок пока нет
- Forensic MedicineДокумент157 страницForensic MedicineKОценок пока нет
- Todentj 9 250 PDFДокумент7 страницTodentj 9 250 PDFRSU DUTA MULYAОценок пока нет
- Development and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersДокумент17 страницDevelopment and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersShyamlaОценок пока нет
- 1053-Article Text-2175-1-10-20230227Документ8 страниц1053-Article Text-2175-1-10-20230227inОценок пока нет
- As 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksДокумент9 страницAs 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksSAI Global - APACОценок пока нет
- Knee Pain and The Internal Arts: Correct Alignment (Standing)Документ7 страницKnee Pain and The Internal Arts: Correct Alignment (Standing)Gabriel PedrozaОценок пока нет
- Normal GFR in ChildДокумент8 страницNormal GFR in ChildbobbypambudimdОценок пока нет
- Redfern Mianscum LetterДокумент6 страницRedfern Mianscum LettermediaindigenaОценок пока нет
- Nursing Process Patients With DiabetesДокумент14 страницNursing Process Patients With DiabetesJelly Jia100% (2)
- Standards For Accreditation-Schools - 2010Документ43 страницыStandards For Accreditation-Schools - 2010Nayda Jiménez Pérez100% (1)
- Project ProposalДокумент3 страницыProject ProposalSkrrtt SkrrttОценок пока нет
- Internet Addiction Kids and The South Korean Govt Boot CampsДокумент5 страницInternet Addiction Kids and The South Korean Govt Boot Campslgheorma0Оценок пока нет
- Ufgs 01 57 19.01 20Документ63 страницыUfgs 01 57 19.01 20jackcan501Оценок пока нет
- Secondary P.E. 10 Q3Документ9 страницSecondary P.E. 10 Q3Jayzi VicenteОценок пока нет
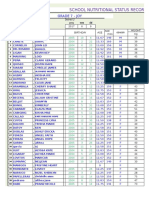
- School Nutritional Status Record: Grade 7 - JoyДокумент4 страницыSchool Nutritional Status Record: Grade 7 - JoySidОценок пока нет
- DSM 5Документ33 страницыDSM 5Grace Marie100% (2)
- Prehension, Mastication, and DeglutitionДокумент3 страницыPrehension, Mastication, and DeglutitionAnjelica Louise MartinОценок пока нет
- CCL-81 Product Sheet - VeroДокумент5 страницCCL-81 Product Sheet - VeroKrishnan KrishnanОценок пока нет
- Raynaud Syndrome Brochure-1 1Документ2 страницыRaynaud Syndrome Brochure-1 1api-340995574Оценок пока нет
- Dunkin DonutsДокумент2 страницыDunkin DonutszerpthederpОценок пока нет
- Derma GITДокумент48 страницDerma GITapi-3843372Оценок пока нет
- 16 MSDS NaHSO3Документ6 страниц16 MSDS NaHSO3Furqan SiddiquiОценок пока нет
- A Study To Assess The Effectiveness of Selected Teaching Strategies Knowledge Regarding Drug Calculation Among B.Sc. N Students in Selected College at ChennaiДокумент3 страницыA Study To Assess The Effectiveness of Selected Teaching Strategies Knowledge Regarding Drug Calculation Among B.Sc. N Students in Selected College at ChennaiEditor IJTSRDОценок пока нет