Академический Документы
Профессиональный Документы
Культура Документы
Examen Mental en Demencia Continuum 2016
Загружено:
Marcela Garzon O VelezОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Examen Mental en Demencia Continuum 2016
Загружено:
Marcela Garzon O VelezАвторское право:
Доступные форматы
Review Article
The Mental Status
Address correspondence to
Dr Murray Grossman,
Department of Neurology,
2 Gibson, University of
Examination in Patients Pennsylvania, 3400 Spruce St,
Philadelphia, PA 19104-4283,
mgrossma@upenn.edu.
With Suspected Relationship Disclosure:
Dr Grossman receives personal
compensation for serving as a
Dementia consultant for C2N Diagnostics,
as a lecturer for the Lundbeck
Institute, for serving on the
international scientific advisory
Murray Grossman, MD, FAAN; David J. Irwin, MD board of the Max Planck
Institutes, and for serving as
associate editor of Neurology.
Dr Grossmans institution has
ABSTRACT received grant support from
Purpose of Review: This article describes a comprehensive approach to the mental the National Institutes of
Health (AG017586, AG038490,
status examination and diagnostic workup of patients suspected of having an NS044266, and NS053488),
emerging neurodegenerative dementia. Key strategies for obtaining a history and and Dr Grossman has received
bedside examination techniques are highlighted. research support from the
Arkin Family Foundation, the
Recent Findings: Classic descriptions of behavioral neurology syndromes were Samuel I. Newhouse
largely based on clinicopathologic correlations of strategic lesions in stroke patients. Foundation, Inc, and the
While still very important, advances in neuroimaging have expanded our armamen- Wyncote Foundation.
Dr Irwins institution receives
tarium of cognitive evaluations to include assessments of findings in nonstroke grant support from the National
anatomic distributions of disease. These efforts support comprehensive assessments Institutes of Health and the
of large-scale cerebral networks in cognitive neurology. National Institute of Neurological
Disorders and Stroke
Summary: A thorough and focused mental status examination is essential for the (K23NS088341-01).
evaluation of patients with cognitive symptoms. Selective use of laboratory testing and Unlabeled Use of
neuroimaging can aid in the diagnosis of dementia by excluding non-neurodegenerative Products/Investigational
Use Disclosure:
etiologies. Neurodegenerative diseaseYspecific tests are in development and will Drs Grossman and Irwin
enhance diagnosis and efforts for disease-modifying therapy development. report no disclosures.
* 2016 American Academy
Continuum (Minneap Minn) 2016;22(2):385403. of Neurology.
INTRODUCTION not easily localized to a single ana-
The mental status examination is a key tomic structure. Rather than localizing
component of a complete neurologic an impairment to a specific anatomic
examination. The neurologic exami- locus, our perspective on brain-behavior
nation is structured to assess different relationships is more consistent with
elements of the neuraxis, and the men- an approach focusing on the disruption
tal status examination largely targets the of a large-scale neural network or con-
cerebrum. Like the elemental neurolog- nectome.1Y7 In this approach, each net-
ic examination, the mental status exam- work is composed of multiple gray
ination is organized into subsections to matter nodes that are interconnected
assess each major domain of cognition. by projections within the white mat-
Cognitive processes and behaviors like ter, and these white matter tracts serve
memory, language, visual-perceptual- to integrate the functioning of the gray
spatial functioning, and executive func- matter nodes. From this perspective,
tioning are targeted. These processes disease disrupting some of the nodes
are very complex. Therefore, the cog- or projections of a cerebral network
nitive functions that are interrogated may compromise a complex cogni-
by the mental status examination are tive function. The quality of cognitive
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 385
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h The mental status disruption depends, in part, on the tive impairment of specific components
examination is structured component (or components) of the of the mental status examination, it is
to probe each major network that are disrupted. Indeed, often the overall pattern of cognitive
cognitive domain any gray matter node may contribute performance across multiple compo-
(attention, memory, to multiple networks. While the as- nents that is most informative. For ex-
language, visuospatial sessment of a patient can reveal selec- ample, in Case 1-1 there is a relatively
perception, executive
functioning, and
social comportment).
Case 1-1
h Cognitive function is A 67-year-old woman, who worked as a lawyer, presented for a neurologic
mediated by large-scale evaluation accompanied by her son, who was concerned about slowly
networks or progressive problems with her memory. While she felt that nothing was
connectomes, where wrong, her son stated that she had been misplacing her keys and forgetting
gray matter nodes are the words she wanted to use in a sentence. She also had trouble remembering
interconnected by names of acquaintances. The son also stated that he was concerned that she
white matter tracts. was asking the same questions repeatedly during the course of a day, and she
h Any gray matter node had made some errors at work that had caught the attention of her coworkers.
may contribute to On her screening Mini-Mental State Examination (MMSE), the patient scored 27
multiple cognitive out of 30. Additional screening identified difficulty with a list-learning task,
networks. in which she learned 5 out of 6 words of a 6-word list in three trials, but
subsequently could not recall any words following a 1-minute delay. Presentation
h While the assessment of
of cues and semantic foils found poor recognition, with only 2 out of 6 words
a patient can reveal
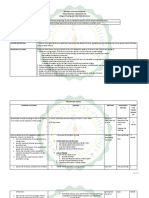
recognized. Similarly, construction of a modified Rey-Osterrieth figure (Figure 1-1)
selective impairment of
showed poor organization with minor spatial displacement and omissions,
specific components
while reproduction of the figure 1 minute later revealed minimal recall. There
of the mental status
was mild difficulty in an oral trials test, and digits recited forward were seven
examination, it is
and backward were five. Her brain MRI showed moderate bilateral hippocampal
often the overall
volume loss. Despite her mild symptoms, her high level of education and
pattern of cognitive
premorbid functioning together with the relative predominance of memory
performance across
impairments raises the question that her diagnosis is suspicious for a mild
multiple components
stage of Alzheimer disease (mild cognitive impairment, amnestic type).
that is most informative.
FIGURE 1-1 Modified Rey-Osterrieth figure. Construction
of a modified Rey-Osterrieth figure by the
patient in Case 1-1 reveals some poor
organization with minor spatial displacement (arrow) and
omissions (asterisks).
Continued on page 387
386 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
Continued from page 386 h A single mental status
Comment. This case vignette illustrates several key points in the cognitive examination obtains only
examination of patients with neurodegenerative disease. First, the importance a cross-sectional
of the mental status history in helping to differentiate benign forgetfulness perspective of a patients
and more clinically worrisome symptoms is noted by the reports of work performance. A history
performance concerns based on memory symptoms. Next, there are relative of slow progression or
imbalances in this patients performance across tasks (ie, relative worse observed longitudinal
episodic memory performance compared to visuospatial and executive decline on serial cognitive
functioning, rather than isolated deficits in one cognitive domain), which is examination testing
a common occurrence. Finally, the patients high level of education may have is required to make
influenced her performance on bedside testing, which illustrates the need a diagnosis of
to account for patient factors in interpretation of cognitive evaluations. a neurodegenerative
dementia.
greater deficit for episodic memory guide cognitive functions that should h The neurologic history is
an important component
compared to other cognitive domains, be ascertained.
to determine the onset,
which suggests the diagnosis of mild It is also important to consider the
tempo, and associated
Alzheimer disease (AD). There are sev- mental status examination in the con- features of the cognitive
eral important caveats to consider when text of other medical and neurologic symptoms. These
administering a mental status examina- features. Attention to elementary neu- factors help direct the
tion. First, the mental status examina- rologic features that are not reflected specific features to focus
tion can be quite lengthy. Like other in the mental status examination will on during examination.
aspects of the neurologic examination, enhance the interpretation of cogni-
it is valuable to tailor the mental status tive findings. It is helpful for cognitive
examination to the most pertinent pos- neurologists to consider involuntary
itive findings and negative features. This movements, for example, in approach-
kind of editing process benefits enor- ing their mental status examination.
mously from a mental status history and Conversely, attention to the mental status
the larger medical history. Indeed, a examination by neurologists treating
single mental status examination ob- neuromuscular or movement disorders,
tains only a cross-sectional perspective such as amyotrophic lateral sclerosis
of a patients performance at a given (ALS) or Parkinson disease (PD), are
period of time, and longitudinal assess- important due to the high frequency of
ment is often very informative. cognitive difficulties in these patients.8,9
A detailed mental status history is Furthermore, the mental status exam-
important to determine onset, time ination may be significantly influenced
course, and progression of symptoms by demographic features of the patient.
that influences the differential diagno- Thus, factors such as education, age,
sis. For example, the pace of disease and cultural background can have an
progression may be characterized as important impact on cognitive and
an acute decline that can be seen fol- behavioral functioning. For example,
lowing a stroke or head injury, or sub- education may influence baseline vo-
acute decline that can be associated cabulary and other cognitive skills, age
with an infectious or neoplastic pro- may influence executive functioning,
cess, or a slow, insidious change that is and ethnicity may influence familiarity
most often associated with a neurode- with specific objects or social norms.
generative condition. Since each of these Consequently, performance expecta-
time courses may be associated with a tions should be adjusted to accom-
particular pattern of cognitive and be- modate individual differences, as
havioral impairment, the history can help illustrated by Case 1-1. In these
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 387
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Each cognitive domain scenarios, formal neuropsychological NEUROLOGIC HISTORY
should be probed during testing using standardized examina- After obtaining a patients chief com-
the history, similar tions with normative scores scaled for plaint, reviewing the history of the in-
to a medical review age and education can be useful and dividuals cognitive and behavioral
of symptoms. compliment observations from bed- symptoms is essential. In addition to
h Differentiating side evaluations. A number of comput- querying the nature of the onset and
age-associated memory erized cognitive test batteries are pace of cognitive change, each major
decline from pathologic available, but these are often limited in domain of cognition and behavior
etiologies is challenging. their scope and testing by computer should be probed, similar to a review
Mental status history often does not replicate the result of of systems. This is critical since an in-
should include details on testing administered by a human. Fi- dividuals chief complaint may not re-
the functional impact nally, it is also important to be mind- flect the true nature of the disorder.
of problems associated ful of an individuals current mental For example, a patients reported
with aging and state. Poor sleep, anxiety/depression, or memory difficulty may indicate prob-
recognition of a problem
side effects of a medication in the in- lems remembering words (ie, word-
by others. finding difficulty) rather than problems
dividuals regimen may interfere with
remembering recent events (ie, epi-
concentration and level of functioning.
sodic memory difficulty). It is also
If there is suspicion of a neurode-
important to review reported cognitive
generative disease upon the conclusion
and behavioral symptoms with a family
of a detailed mental status examination,
member or close friend because there
it is important to judiciously consider is often limited insight in ones own
ancillary laboratory and neuroimaging cognitive functioning.
studies to help support the diagnosis
and exclude non-neurodegenerative Memory
etiologies. Indeed, a range of toxic, Memory difficulties can be probed by
metabolic, inflammatory, neoplastic, asking about problems learning and
paraneoplastic, or infectious etiologies recalling new information, as well as
can mimic neurodegenerative diseases. forgetfulness. Individuals may forget
Diagnosis of these conditions is critical, conversations and repeat questions
as disease-specific treatments may need about recent activities. Forgetting to
to be implemented. Conversely, labora- pay bills or paying bills twice and going
tory and neuroimaging investigations to the store and purchasing the same
can be initially equivocal or normal in food items repeatedly represent worri-
early neurodegenerative disease; thus, some memory difficulties, as in Case 1-1.
a careful mental status examination is By comparison, minor memory prob-
the first line in detecting these condi- lems associated with aging, such as mis-
tions. This is of critical importance as placing keys and difficulty finding a car
earlier diagnosis and implementation of in a parking lot, are less concerning.
supportive care can improve quality of
life, prevent comorbidities, and reduce Language
caregiver distress. As disease-modifying Many patients may report a decline
treatments emerge, patients are likely in language production and may
to benefit from the earliest possible experience word-finding difficulty.
administration of these interventions. Sometimes this can take the form of
This article reviews the mental status trouble retrieving the name of a family
examination with exemplary case vig- member or familiar friend. At other
nettes and discusses the diagnostic times, patients may report difficulty re-
evaluation and emerging biomarkers trieving the names of objects. Some-
for neurodegenerative diseases. times individuals will report substituting
388 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
one word for another or mispronounc- (eg, over the telephone), and reading
ing words. These are lifelong findings and writing difficulties. It is important
that increase in frequency as individuals to ascertain whether these symptoms
age, and, thus, symptoms of this sort are truly a disorder of language, such
are challenging to evaluate and should as spelling difficulty when writing, or
be investigated carefully since they reflect another source of difficulty, such
may represent an exaggeration of as motor weakness interfering with
otherwise healthy aging. Other com- mechanical aspects of writing. It is im-
monly reported symptoms include portant to consider other nonlanguage
effortful speech, as in Case 1-2, difficul- etiologies that contribute to these
ties with comprehension of speech symptoms, including reduced auditory
Case 1-2
A 62-year-old woman who worked as a phone operator reported difficulty
getting her words out. She stated that she worked at a busy switchboard
for a large building complex, and she had become easily overwhelmed
with complex tasks and had stopped working as a result. She stated that
she was aware of the words she would like to use but had difficulty
producing them, which caused her great frustration. Her daughter felt
impatient waiting for her mother to finish a sentence, which caused a
significant depressed mood for the patient, but she had no other behavioral
changes. She noticed that she had made more spelling errors lately.
Mental status examination found a Mini-Mental State Examination
(MMSE) score of 28 out of 30, with two points lost for difficulty spelling
world backward (the patient spelled D-L-O-R-W). She had significant
difficulty with executive functioning including oral alternation between
letter and number sequences and reciting digits backward. She also had
some minor difficulty with an alternating manual manipulation task (ie,
Luria three-step maneuver to pantomime an alternating sequence of hand
gestures), a measure of executive functioning. Her speech was slow and
hesitant. Sentence length was short with simplified grammatical structure
to her speech and rare frank agrammatisms. Verbal comprehension for
simple commands like fold a paper in half and put it on your lap was
preserved, but she had difficulty with the request to point to the ceiling
after you point to the floor due to grammatical comprehension difficulties.
She had preserved single word and object knowledge and could readily
identify and describe line drawings and objects. Reading and writing were
comparable to her oral language. The patient did not exhibit limb apraxia
but she had difficulty pantomiming how to blow out a match or suck
in through a straw, indicating orobuccal apraxia.
She was asked to describe a childrens photo book depicting a scene
where a boys pet frog sneaks out of his bedroom in the middle of the
night. The patients response was as follows: And the dog and the boy
was oo- eh sleeping, on the baw- eh the- the, um, the uh, bed. And uh...
the uh, the- the frog (2.7 second pause) emptied- of the- move the- the
glass, ba- bottom... and go to... uh... uh, w- wo wook goo could do anything.
Comment. This patient was diagnosed with the nonfluent variant of
primary progressive aphasia due to her relatively isolated grammatical
comprehension and expression difficulties with executive limitations and
preserved single word/object comprehension.
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 389
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Visual-perceptual-spatial acuity, visual acuity limitations, or other ning, as in Case 1-3. Individuals may
difficulties may be sensory-motor deficits. describe challenges executing previ-
difficult to elicit through ously familiar multistep activities such
history. Common Visual-Perceptual-Spatial as cooking a meal, organizing a trip, or
examples include Performance maintaining the household. Family
difficulty navigating a Visual-perceptual-spatial symptoms are members may have noticed a change
car, finding objects in often challenging for patients to report in the patients lifestyle, with the indi-
the home, recognizing because of problems articulating day- vidual no longer engaging in activities
faces or objects, or to-day examples. There may be diffi- outside of the home, requiring others
difficulty dressing. culty driving, such as frequent fender to initiate activities or talk the individ-
h Detecting social and benders or difficulty with parallel ual through the steps of the task. Indi-
personality changes parking. An individual may struggle viduals may have difficulty completing
associated with when trying to find an object in a tasks that have been started because
neurodegenerative complex visual scene, such as identify- of easy distractibility. Driving is a dual-
dementia often requires
ing a specific jar in a pantry. Patients tasking environment, and driving
a careful history from a
may have difficulty recognizing faces difficulty may be related to limited
reliable informant who
spends significant time
or objects and may find it necessary executive resources. The patient may
with the patient. to hear a persons voice or an objects exhibit limited attention or fluctuating
associated sound prior to recognition. levels of attention.
Difficulty dressing may reflect a visuo-
spatial symptom, and there may be Social and Personality Changes
difficulty negotiating space around the Family members may note a significant
home, and falls may occur because of change in the patients personality, while
lateralized neglect. It is important to patients with social difficulties often
rule out deficits of coordination or the have limited insight, as in Case 1-3. De-
extrapyramidal system that can influ- tecting social and personality changes
ence these symptoms. necessitates a careful mental status
history from a reliable companion.
Executive Functioning There may be some obvious
Dysexecutive symptoms often reflect changes suggesting disinhibition,
difficulty with organization and plan- which may take the form of frequent
Case 1-3
A 54-year-old man developed slowly progressive behavior and personality
changes. His wife reported that she first noticed a change when he became
less interested in socializing approximately 3 years earlier. He formerly would
be well dressed but had begun to wear the same ripped sweatpants daily.
He approached strangers to tell them his political views, which included racist
and sexist comments that most would find offensive, and his wife claimed
that these were not his previous beliefs. This behavior caused considerable
interpersonal relationship problems both at home and at his employment as a
salesman, although he questioned why his family found his behaviors to be
objectionable. He showed no concern for his brothers recent cancer diagnosis.
After eating large amounts of food, he left his cousins wedding unexpectedly
and was found watching television in his hotel room. On one recent occasion he
sent large sums of money to a stranger over the Internet who claimed to
be a prince from another country. He demonstrated increasing difficulty
performing multistep activities at home, such as making a sandwich for lunch.
Continued on page 391
390 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Continued from page 390
Mental status examination revealed difficulty with attention and poor
social discourse (he interrupted the examiner on several occasions with
tangential comments). He could not perform a complex oral alternating
pattern (continuing an oral sequence that begins with A-1-B-2-C-3I) and
made several perseverative errors throughout testing, indicating poor
set-shifting ability. He inappropriately tapped his fingers on the desk and
whistled a repetitive song during the majority of the examination. A brain
MRI showed atrophy in the orbitofrontal and medial frontal lobe and the
insula on the right with similar but less pronounced change in the homologous
regions of the left hemisphere, consistent with the behavioral variant of
frontotemporal dementia (bvFTD) (Figure 1-2).
FIGURE 1-2 Knife-edge cortical atrophy in the behavioral
variant of frontotemporal dementia.
Parasagittal T1 MRI of the right
hemisphere of the patient in Case 1-3 displaying significant
dorsolateral, orbitofrontal, and perisylvian atrophy in the
frontal lobes and severe anterior and medial temporal
atrophy in the right hemisphere greater than the left
hemisphere (arrows). There is relative preservation of
posterior cortices, resulting in a dramatic knife-edge
appearance of the border between precentral gyri and
postcentral gyri.
Comment. This case illustrates the range of social and behavioral
impairments commonly seen in bvFTD. Furthermore, this patient exhibited
only mild executive impairments, which is common early in the course of
bvFTD as patients can have largely a social disorder with minimal cognitive
deficits. Finally, social cognition is difficult to assess without a reliable
informant due to the reduced insight in patients with bvFTD.
rude or inappropriate comments in- may exhibit hypersexuality in the
volving strangers, or engaging in form of sexual jokes, viewing pornog-
overly familiar behavior or sharing raphy on the Internet, or inappropriate
confidential information. The patient touching of strangers. Episodes of
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 391
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Social comportment is explosive agitation and rage without harmful events for others, as evidenced
difficult to assess in apparent provocation may be seen. An by Case 1<3. There may be limited in-
the mental status individual may become apathetic and sight into the motivations of others,
examination and often have difficulty initiating activities. Flat- which can result in a range of behav-
requires a thorough tening of affect and a loss of the normal iors, such as investing in scams or fail-
history from a variety of emotions may be seen. Al- ing to acknowledge significant events
reliable informant to ternatively, the patient may exhibit ex- in the lives of others, such as the death
be detected. aggerated and childlike emotional of a spouse.
h It is important to inquire expressions. There may be ritualistic These behavioral changes are com-
about activities of daily behavior such as the development of monly associated with the behavioral
living to identify potential unusual and repetitive habits and col- variant of frontotemporal dementia
safety issues that could lections, and the emergence of novel (bvFTD) and forms of primary progres-
result in morbidity religious beliefs or political interests. sive aphasia, but can be also seen in
and mortality from Socially intrusive simple repetitive be- other neurodegenerative conditions.
cognitive impairment.
haviors also can be seen such as clap- Indeed, there is significant overlap of
ping, tapping, and humming. Hoarding frontotemporal dementia (FTD) symp-
of unusual collections of objects may toms with atypical parkinsonian disor-
occur. Hyperoral behavior may become ders (eg, corticobasal degeneration and
evident, such as shoveling food into the progressive supranuclear palsy) and
mouth, continuing to eat even though ALS.10,11 Furthermore, apathy and de-
the individual is sated, or oral explora- creased motivation are not uncommon
tion of nonedible substances. There in AD and PD. Impulse control disor-
may be a strong preference for sweets der seen in PD may also resemble fea-
or carbohydrates, and an individual tures of FTD.12
may gain substantial weight over a
very brief period of time. There may Activities of Daily Living
be shoplifting as the result of hyper- Safe execution of activities of daily living
oral behavior or attraction to shiny is essential for minimizing morbidity
objects. Utilization behavior involves and mortality in patients with cognitive
unavoidably using objects such as a impairment, so it is important to ask
patient picking up a pen on the desk about activities of daily living. Specific
and signing his or her name. Patients activities of daily living should be
may perseverate or exhibit echolalic or probed, including bathing, toileting,
echopractic behavior that mirrors the eating, and dressing, as difficulties could
behaviors of others. Frequently, the lead to falls, aspiration, or infection. It
patient may have limited insight into is also important to note if patients
these changes in behavior and may be have difficulty managing complex tasks
bewildered by the concerns of others that can have dangerous consequences
or may express childlike denial. Diffi- such as cooking and administering
culty with perspective taking also can medications. Access to finances and
interfere with social interactions, which the Internet or telephone should be
can be seen commonly in conversation- assessed to protect patients with frontal
al or behavioral exchanges where there disease and poor judgment from being
may be limited empathy for a conversa- financially exploited, as in Case 1<3.
tional partner. Frequent interruptions Finally, determining the level of super-
with tangential comments and poorly vision provided on an average day is
organized narrative speech (ie, poor important in more severely impaired
social discourse) may be seen. Likewise, patients in order to prevent wandering
there are inappropriate responses to or other dangerous events.
392 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
MENTAL STATUS EXAMINATION common method involves presenting h Screening cognitive
Several brief mental status assessment an individual with a list of words at a instruments provide a
tools have been developed for ease of pace of about one per second, and then brief sample of different
use in a busy clinical setting. These can asking the individual to repeat the cognitive domains that
be used at times to serve as screening words in order to confirm registration. can be useful to track
devices and may be useful for following The individual is asked to retain the patients longitudinally
an individual longitudinally. However, words in memory during the perfor- but do not substitute for
mance of another task in order to block a thorough examination.
these screening instruments should not
be considered a reasonable substitute subvocal repetition and to examine h Episodic memory is
for a comprehensive mental status exam- fading of the memory trace over time. often tested by using
ination. Examples of brief instruments Subsequently, recall is requested. There list-learning tasks where
are many variations of this basic format. a sequence of words is
include the Mini-Mental State Exam-
The number of words in the list may repeated after several
ination (MMSE),13 the Addenbrooke
vary from three up to 15, and the num- trials and then recalled
Cognitive Examination (ACE),14 and the after a brief delay.
Montreal Cognitive Assessment (MoCA).15 ber of repetitions requested may vary
Recognition is assessed
Each of these brief surveys covers slightly from one to five, depending on the
through use of cues or
different domains. There are also several level of difficulty that is sought and the semantic foils. Difficulty
more comprehensive but slightly longer desire to document a learning curve. can be adjusted
surveys that probe all of the major cog- The amount of time between presen- depending on length of
nitive domains. One example is the tation and recall may vary from list and delay time.
Philadelphia Brief Assessment of Cogni- 30 seconds to many minutes. In the
tion.16 A more comprehensive mental event of failure to recall some of the
status evaluation of each cognitive do- target words, prompts can be offered.
main is outlined in the following sections. These can include a superordinate cue
(eg, a kind of clothing) or a rhyming
Attention word (eg, sounds like block). After
It is valuable to begin the mental status spontaneous recall and prompted re-
evaluation with a consideration of at- call, a recognition procedure may be
tention. This can be derived in part administered. During this phase, some
during the history by observing whether of the previously mentioned target
the individual is maintaining a reason- words are offered, intermixed among
able, sustained level of arousal or is foils that may be semantically similar
easily distracted. A more systematic to the target, phonologically similar to
approach is obtained by performing a the target, or random words. In the
simple assessment of vigilance. This authors screening mental status eval-
can involve asking an individual to lift a uation, we administer a six-word list
hand whenever a target letter (eg, A) is presented for three learning trials, use
heard in a string of random letters a 1 minuteYfilled interval, obtain free
delivered at a pace of about one per recall, and administer a yes-no recog-
second. Alternatively, repetition of a nition procedure for words that are
sequence of digits can be performed, not remembered during free recall. We
starting at two and gradually increas- monitor the number of words pro-
ing the digit length, delivering the digits duced during learning trials to see if
at a rate of one per second. Seven digits there is a learning curve, the number of
or more is considered normal. words freely recalled, and recognition
accuracy. Regardless of the examiners
Memory preferred form of episodic memory
There are several different ways to as- testing, it is important to document the
sess episodic memory. Perhaps the most parameters used to assess memory.
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 393
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Nonverbal methods Other memory tasks can include ask- tation can be viewed as a test of
of testing memory, such ing an individual to listen to a sentence incidental memory. In the authors as-
as figure-recall tasks, are or a paragraph and then probing recall sessment of memory, we include eval-
useful in patients of the sentence or paragraph at a later uation of incidental recall of a visual
with significant time. A memory score is derived from geometric design. Other forms of mem-
left-hemispheric disease. the ability to recall critical key words ory that can be assessed include habit
h Language dysfunction from the sentence or paragraph. In ad- learning (ie, asking an individual to
can be detected during dition to verbal memory, assessing epi- repeat a sequence of novel hand ges-
the clinical examination sodic memory recall with another kind tures), semantic memory (ability to rec-
through identification of of material is often helpful as this mini- ognize familiar but infrequent objects
abnormal prosody, [eg, a shoehorn] and to answer ques-
mizes confounds associated with the
word-finding pauses, tions about these objects [eg, Is it
specific learning material and depen-
circumlocutions, found in the kitchen?]), auditory-verbal
grammatical dence on left hemispheric function. One
method is to perform episodic mem- short-term memory (repetition of digits,
sophistication, and
ory testing using visual presentation of multisyllabic words, and sentences of
frank agrammatisms in
words or recall of a visual geometric various lengths), and working mem-
spontaneous speech.
ory (reproducing a list of digits in the
h Language comprehension design. Recall of a visual geometric de-
reverse order of presentation). Further
should be performed on sign often takes the form of copying a
details on object knowledge/semantics
the single-word and visual design, removing the target de-
and working memory are discussed in
sentence level. Single-word sign and its copy, engaging the individ-
comprehension can be
the sections on language and executive
ual in another visual-perceptual-spatial
assessed through word functioning that follow.
activity for a brief period of time, and
and object meaning and
then asking the patient to reproduce Language
sentence comprehension
through repetition and
the visual design. As with verbal episodic Language is a complex process that is
verbal commands of memory, visual episodic memory test- crucial for daily functioning. Several
sequenced tasks. ing can be manipulated by varying the components of language should be as-
complexity of the visual stimulus, the certained in a comprehensive mental
meaningfulness of the stimulus (eg, a status evaluation. We first evaluate
nameable design such as a clock face or single-word processing. During speech
a non-nameable multicomponent geo- production, listening for word-finding
metric design), and the amount of time pauses and circumlocutions is impor-
between presentation and recall (refer tant. An individual also may make
to Case 1<1 for an example). Recogni- frequent lexical substitutions or speech
tion for elements of a visual stimulus sound errors. Confrontation naming is a
(eg, the position of the clock hands) more formal way to assess single-word
can be tested as well. use and word finding and typically takes
These verbal and visual memory tests the form of asking an individual to
involve an explicit request to learn, name a pictured object or a real object.
remember, and then recall specific The frequency of the words occur-
information (ie, intentional memory). rence and familiarity of the target object
In our daily lives, we often also learn can be manipulated. Confrontation nam-
and retain information without con- ing also can be assessed using other
scious effort (ie, incidental memory), nonvisual modalities. Thus, naming can
and it is not unreasonable to assess be performed in response to a sound or
incidental memory by asking an indi- the feel of a target object. This is im-
vidual to recall words or designs when portant for an individual who has
there is no explicit request to remem- difficulty with visual-perceptual-spatial
ber at the time of presentation. Orien- functioning. Some patients may have a
394 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
modality-specific naming problem in- quality of speech, in which prosodic h Lexical comprehension
terfering with interpretation of a visual difficulty may be reflected in a limited should be assessed in
stimulus such as visual agnosia, while a or exaggerated range of pitch. Disrup- parallel with assessment
more general deficit in semantic mem- tion of the coordination of the motor of object meaning in
ory interferes with interpretation of an speech apparatus may occur, such as semantic memory. This
object in any modality. apraxia of speech, where the timing of can be done by asking
Comprehension can be assessed for speech is irregular and speech sound for the definition of a
a word, paralleling the assessment of errors are produced that consist of single word or asking to
the representation of object meaning sounds that are not from the native name attributes of a
in semantic memory. Lexical compre- speakers lexicon. This should be dis- words referent.
hension can be assessed by asking an tinguished from dysarthria, which is a h Apraxia of speech refers
individual to provide a definition of a dysfunction of the muscles involved in to disruption of
word. Word meaning can be assessed speech. Sentence comprehension can coordination of the
in a multiple-choice manner as well. be assessed by asking an individual to motor speech apparatus
and should be
Specific attributes of a words referent perform a brief series of simple tasks
distinguished from
can be assessed as well, such as asking in the mentioned order. Sentence com-
dysarthria, which is a
whether a camel lives in the ocean or prehension also involves a uniquely dysfunction of the muscles
whether asparagus is red in color. An language component, namely, grammar. involved in speech.
individual also can be asked whether An individual can be asked to point to
h Grammatical
two words are from the same category, objects in an order that differs from the
comprehension can be
such as deciding whether a lemon and order of mention through the use of a assessed through use of
an apple are both fruit. preposition, as in Case 1<2. Also, an simple questions of
Language comprehension should individual can be asked to choose the who did what to
also be assessed at a multiword or sen- agent of an action in a simple, brief whom in sentences
tence level. Sentence processing is a sentence such as It was the boy that with increasing
complex process. Since words in a sen- the girl chased. Who did the chasing?18 grammatical complexity
tence emerge over time, it is valuable to It is also important to assess written (ie, The car that hit the
assess repetition, a form of auditory- communication such as reading and truck was green. Who
verbal short-term memory. Repetition writing. Letter-by-letter reading involves was hit?).
can be assessed by asking an individual slowed interpretation of the geometric h Surface dyslexia is the
to repeat a monosyllabic word, a mul- shapes that constitute a written word, reading of a sight
tisyllabic word, a multisyllabic phrase, and, thus, the amount of time needed (orthographically irregular)
and sentences of various lengths. In to read a word is directly proportional word that requires
sentence expression, pathologic speech to its length. Single-word reading also semantic knowledge
rather than phonetics for
is often characterized as effortful. The assesses the spelling system. In English,
proper pronunciation,
rate of nonfluent speech production is many words involve letter-sound corre-
examples of which include
about 45 words per minute (refer to spondence rules, and this can be as- cough, choir, and pint.
Case 1<2 for an example), much slower sessed by asking an individual to read a
than the normal adult speech rate of pseudoword such as tig. English also
more than 140 words per minute.17 contains sight vocabulary words, and an
There may be omissions of bound or individual with surface dyslexia who
free grammatical morphemes (ie, cannot correctly pronounce sight words
words, prefixes, or suffixes with gram- (ie, orthographically irregular) like
matical function), giving speech a dough, choir, or pint will often attempt
telegraphic quality. It is important to to pronounce them using letter-sound
listen for the variety of grammatical correspondence rules. Reading compre-
forms used in conversational speech. hension can be assessed by asking an
Other errors in speech include dis- individual to perform a simple written
orders of prosody, or the sing-song act, such as Close your eyes. Spatial
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 395
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Executive impairment neglect can interfere with reading, and tion). Perhaps the simplest assessment
can cause impairments this can be demonstrated by asking an of visuospatial functioning involves the
in construction tasks individual to read a compound word location of an object in space, which
through poor such as cowboy. Writing can be as- can be tested by asking an individual to
organization and sessed by asking an individual to write reach for an object. An individual also
omission of elements. In to dictation, including both words that can be asked to imitate a meaningless
contrast, visuospatial obey letter-sound correspondence gesture, such as placing the dorsum of
impairments manifest in rules and orthographically irregular one hand against the contralateral
spatial displacements words. A motor coordination disorder cheek. A more formal assessment of
and distortions on known as apractic agraphia results spatial relationships includes the judg-
construction tasks.
in difficulty with the automatic me- ment of line orientation, where an
h Visuospatial function chanical formation of letters, which individual is asked to evaluate whether
can be assessed through will significantly slow writing. It is a pair of lines is parallel. An element of
construction of figures important to keep in mind that liter- visuospatial functioning may involve
with varying familiarity
acy is highly variable, and reading and part-whole discrimination, also known
and complexity.
writing abilities will vary depending as simultagnosia. One task frequently
h Ideomotor apraxia is on experience. used to assess this involves using many
difficulty in small letter A characters to form a
demonstrating learned Visual-Perceptual-Spatial shape that looks like a large letter E
gestures. Transitive Functioning (ie, Navon figure)21 and asking an
gestures involve use of
tools while intransitive
Visual-perceptual-spatial functioning is individual to name the letter. Individ-
gestures do not involve an important aspect of the bedside uals with difficulty involving whole-part
an implement. mental status examination that is fre- discrimination name the small letter and
quently neglected. Perhaps the most do not recognize that these are in a
common assessment involves copying configuration forming a large letter.
a visual geometric design. The design Another visual-perceptual-spatial task
itself may vary in complexity, from a involves face processing. An individual
simple nameable geometric form to a can be asked to recognize a photo-
nameable object or a more complex graph of a famous face. It is also pos-
non-nameable geometric design. Ex- sible to use the examiners face as a
amples include overlapping pentagons stimulus and query whether there are
and the more complex designs devel- features such as a full head of hair or a
oped by Rey and Osterrieth or Benson beard. Visual agnosia may manifest
(refer to Case 1<1 for an example).19,20 itself as difficulty recognizing the visu-
These designs should be scored for al presentation of an object, although
accuracy as well as the manner in which the object can be recognized from its
they were executed. This includes poor sound or feel. Color processing can be
organization and the omission of ele- assessed by asking an individual to
ments, which may reflect executive name or recognize a color and asking
impairment and spatial displacements, whether two colors match.
such as the placement of an individual There are a variety of other disor-
component in an inappropriate spatial ders associated with diseases of the
location relative to other elements of parietal lobe that can be assessed as
the design. Sometimes one-half of a well. Apraxia is difficulty demonstrat-
figure can be impoverished or ne- ing learned gestures, which involves
glected. Spatial difficulty can interfere transitive gestures that use an imple-
with reading (eg, difficulty finding a ment such as demonstrating the use of
line on a printed page) and writing (eg, a hammer, or intransitive gestures that
spatially disordered written produc- do not involve an implement such
396 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
as waving good-bye.22 These gestures Executive Functioning h Higher-order parietal
can be elicited in response to a verbal Executive functioning is a complex lobe functions include
request or with imitation. Imitation domain that involves the efficient exe- calculations, cortical
(pantomiming) can help dissociate a cution of tasks. Perhaps the most com- sensation, left-right
disorder of verbal comprehension from mon assessment of executive functioning discrimination,
true apraxia. Oral praxis also can be as- is category naming fluency. This can somatosensory maps
sessed as well (eg, blow out a match), involve naming words beginning with (ie, limb position),
and this does not necessarily track a target letter (eg, F) or naming words and apraxia.
apraxia of speech or limb apraxia, as from a target semantic category (eg, h Executive functioning
in Case 1<2. animals). Task performance is evalu- involves mental
Calculations and other assessments ated by counting the number of manipulation of
of number knowledge also are associ- words produced during a period of information and shifting
ated with the integrity of the parietal time, such as 60 seconds. Category between tasks. These
lobe.23 This can be assessed by asking functions can be tested
naming fluency in response to a target
through an alternating
an individual to select the one of two letter is a more challenging measure of
sequence of written,
numbers that is larger, to perform executive functioning, while the seman- oral, or manual tasks.
simple calculations orally or in writing tic guidance provided by a meaningful
(eg, 7 + 9 =___), or to solve a simple category like animals generally facili-
day-to-day problem that depends on tates category naming fluency. It can
calculations (eg, How much change be informative to monitor whether
from a dollar should you receive after production is organized, such as nam-
buying a 65-cent candy?). Like spatial ing farm animals, then jungle animals,
aspects of reading and writing, spatial then varieties of fish. Another sign of
difficulties can interfere with the align- executive dysfunction is perseveration
ment of numbers in a multidigit cal- or difficulty shifting set between tasks.
culation and consequently result in a One sign of this is frequent repetition of
calculation error. Higher-order parie- words in category naming fluency. A
tal lobe sensory integration can be as- visual analogue of category naming
sessed by cortical sensation; a letter or fluency involves design fluency. The
a number can be written in the palm most common form of this measure
of the hand and named by the patient involves connecting a number of dots,
(testing for graphesthesia), or an ob- such as nine dots, to form different
ject can be placed in the hand and designs.
named (testing for stereognosis). Body Another common executive mea-
part localization can be assessed by sure involves alternating patterns. This
touching a body part of an individual entails performing a task, and then
with his or her eyes closed, and asking inhibiting that performance to perform
the individual to indicate the part of a second task. The material can be quite
the body that was touched. Left-right simple or more complex. Simple ver-
discrimination can be assessed by iden- sions of this kind of alternating task
tifying a body part bilaterally on an in- involve a simple rule such as tapping
dividual (eg, ears) and asking the once on a table when the examiner taps
individual to identify the right one or twice and not tapping when the exam-
the left one of the pair. A more difficult iner taps once. The examiner provides
assessment of left-right orientation a random sequence of single or double
asks an individual to identify the left tapping. Another variety of alternat-
or right body part on the examiner. ing pattern involves the examiner
Finger agnosia also may be evident in touching an individuals right hand or
an individual with parietal disease. left hand in a random order with the
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 397
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
KEY POINTS
h Working memory is the eyes closed, and the individual responds page and asking an individual to point
ability to hold and by lifting the touched hand. After this to these in an order reversing the
manipulate data. task has been well learned, the examiner order of demonstration.
Assessment of the reverses the association and asks the
number of digits individual to lift the right hand when Social Functioning and Behavior
recalled in reverse can the left hand is touched, and lift the Examination of social comportment is
be useful to test left hand when the right hand is challenging and often requires infor-
working memory. touched. More complex versions of mation from a reliable caregiver, as pa-
h Social functioning and alternating patterns involve reproduc- tients with ventral frontal disease often
behavior difficulties ing two intermixed, overlearned se- have little insight or concern into their
should be considered in quences, such as alternating production difficulties. There are several valuable
any patient who has of a letter and a number in ascending social questionnaires that can be com-
difficulties with social order, such as A, 1, B, 2, C, 3. This can be pleted by spouses, family members, or
discourse, simple performed orally or as a written trails close friends concerning changes in
repetitive motor rituals,
procedure, where letters and numbers personality, behavior, and social func-
or inappropriate behavior
are randomly distributed on a page tioning. Examples include the Neuro-
during the interview. A
reliable informant should
and an individual is asked to draw a psychiatric Inventory and the Frontal
be obtained to gather line between a letter and a number in Behavioral Inventory, which probe day-
additional history. ascending sequence. to-day functioning, looking for changes
Two related components include in personality and behavior compared
h A major limitation in
the development of
parsing a sequence into smaller, re- to baseline.24,25 The previous section
meaningful treatment peated units and inhibitory control. A on history details specific domains of
for neurodegenerative repeated series of three hand gestures social comportment that are affected
diseases is that is demonstrated to the patient three by frontal lobe disease. Observation
definitive diagnosis is times, and then the patient is asked to of patient interactions in clinic are
obtained only at autopsy. demonstrate the hand gestures. A mea- also important as detection of be-
sure intended to assess inhibitory con- havioral disinhibition, simple repet-
trol is a Stroop test, where words are itive motor rituals, and poor social
written in a colored font that differs discourse (Case 1<3) should prompt a
from the color name, and an individual more thorough examination for evi-
is asked to name the color of the font dence of social comportment disorder
and not read the printed word. When and executive limitations. Other be-
seeing the word blue printed in a red havioral and emotional changes that
font, for example, the individual is should be noted include depression
asked to respond red. and anxiety since these can be signif-
Working memory is often thought icant and can also interfere with the
to be a component of executive func- mental status examination.
tioning and involves the ability to main-
tain some material in an active form
and do some work on this material. DIFFERENTIAL DIAGNOSIS AND
Common tests of working memory ANCILLARY TESTING FOR
involve reproducing a list of numbers NEURODEGENERATIVE DISEASE
in the reverse order or reordering a A major limitation in the development
random sequence of letters and num- of meaningful treatment for neurode-
bers into their ascending orders, using generative diseases is that definitive
progressively longer sequences. A sim- diagnosis is obtained only at autopsy.
ilar kind of assessment can be per- Furthermore, significant clinicopatho-
formed in the visual domain by pointing logic overlap exists between neuro-
to randomly distributed circles on a degenerative diseases, and clinically
398 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
defined phenotypes of AD, PD, FTD, neurodegenerative condition. EEGs can h Careful selection of
and ALS often vary in the ability to be helpful to identify partial status ancillary laboratory and
accurately predict underlying neuro- epilepticus, or periodic discharges as- neuroimaging studies
pathology. This is of significance as sociated with prion disease, some can be useful to rule
emerging therapies are targeting steroid-responsive encephalopathies, out common
disease-specific misfolded proteins and other rapidly progressive demen- non-neurodegenerative
(eg, tau, amyloid-" [A"], synuclein). A tias. EEG recordings in neurodegenera- etiologies of cognitive
focus of current neurodegenerative tive disease usually show nonspecific impairment.
disease research includes early diag- slowing, although DLB may have fluc-
nosis as patients may potentially show tuations in slowing.33 CSF analysis can
a greater benefit from emerging be particularly useful to evaluate vascu-
disease-modifying therapies earlier in litides or other inflammatory conditions
the disease course.11,26Y28 This includes that can mimic neurologic conditions
focus on mild cognitive impairment that may not be evident in blood se-
(MCI) or prodromal states for AD, PD, rologic testing.34 The authors routinely
dementia with Lewy bodies (DLB), and check CSF protein, cell count, IgG
ALS.27,29Y32 Additionally, patients with levels, cytology, cryptococcus antigen,
FTD may often present with minimal and cultures in all patients with
cognitive dysfunction and feature def- suspected FTD, ALS, and atypical
icits that are largely restricted to social AD to rule out alternative non-
functioning.11 Moreover, many of the neurodegenerative etiologies.
cognitive and social deficits seen in Current biomarker research is aimed
neurodegenerative diseases also can at developing neurodegenerative
be manifested in non-neurodegenerative diseaseYspecific tests,11,27,28 and, cur-
disorders of the cerebrum. Thus, a rently, the only biomarker test ap-
detailed evaluation, including ancillary proved by the US Food and Drug
laboratory and neuroimaging studies, is Administration (FDA) is in vivo amy-
necessary to rule out common meta- loid imaging for AD using positron
bolic, toxic, inflammatory, or infectious emission tomography (PET) with
mimics of a neurodegenerative disease. amyloid-specific radiotracers. However,
In individuals without prior testing, due to clinicopathologic complexities in
it is often valuable to have additional aging and cognitive impairment, scan-
laboratory studies to supplement the ning is currently recommended only for
mental status examination and screen younger patients with a progressive
for common etiologies that can con- dementia, those with atypical AD clin-
tribute to cognitive impairment. Among ical symptoms, or unexplained pro-
these are a complete blood count, longed MCI.35 CSF measurements of
electrolyte panel, liver and kidney func- tau and A" can also be a potentially
tion tests, thyroid-stimulating hormone useful biomarker for AD neuropathol-
(TSH), vitamin B12 level, and sedimen- ogy. Indeed, an AD CSF signature of
tation rate. These may be supple- elevated total tau (t-tau) and phosphory-
mented depending on the specific lated tau (p-tau) with lower A"1-42 is
medical history and mental status highly consistent with AD and MCI at
examination findings. risk for progression to AD compared
Structural brain MRI images can help with cognitively normal controls, and
exclude cerebrovascular disease, neu- correlates well with AD neuropathology
roinflammatory conditions, or other at autopsy.36Y38 Lab-to-lab variation cur-
structural lesions such as hydroceph- rently precludes this test from being
alus or malignancy that can mimic a clinically available, but international
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 399
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
efforts to standardize detection assays if there is hypometabolism in fron-
will likely lead to clinical availability totemporal regions suggestive of FTD
in the near future.39,40 AD CSF bio- in the absence of cortical atrophy. Fi-
markers also may have value in nally, FTD syndromes may be difficult
other neurodegenerative diseases. In- to differentiate from AD if episodic
deed, many patients with PD have memory or visuospatial difficulties are
considerable plaque and tangle pa- prominent. FDG-PET can identify pa-
thology at autopsy associated with de- tients likely to have AD neuropathology,
mentia, and low CSF A"1-42 may predict with posterior parietal and medial tem-
cognitive decline in PD.8,41 Additionally, poral hypometabolism, or DLB, which
lower CSF !-synuclein may differentiate may be characterized by parietal-
PD from normal control patients.42 Fi- occipital hypometabolism. The authors
nally, since half of all FTD cases and have also found high diagnostic accu-
virtually all ALS cases have a TDP-43 racy to differentiate atypical AD from
proteinopathy, CSF p-tau levels appear FTD in autopsy-confirmed CSF cases
to be lower than seen in tauopathies using the t-tau to A"1-42 ratio.46 Future
and healthy controls.43,44 Thus, CSF is a FTD-specific biomarkers will be useful
promising modality for neurodegener- to improve antemortem diagnosis, and
ative disease biomarker discovery. a combination of clinical, biofluid, and
The clinical diagnosis of FTD and neuroimaging modalities may be
primary progressive aphasia syn- most effective.11
dromes can be especially difficult as
these patients are usually younger, CONCLUSION
and some patients may have a non- The mental status examination has sev-
progressive neuropsychiatric condition eral components focused on each cog-
that resembles bvFTD (ie, phenocopy nitive domain (ie, attention, memory,
syndrome, which is a recently described language, visuospatial perception, ex-
clinical syndrome of nonprogressive ecutive functioning, and social com-
social comportment disorder that is portment). A thorough mental status
not due to underlying frontotemporal examination includes a detailed med-
lobar degeneration or other neurode- ical and neurologic history with focus
generative disease. The etiology of these on features of each cognitive domain
cases is currently unclear, but many are to guide the examination and provide
thought to be due to decompensated details for onset and tempo of disease.
psychiatric disease later in life and, thus, Several bedside assessments are effec-
clinically mimic bvFTD initially).45 Due tive in probing these areas and pro-
to the lack of biomarkers or laboratory viding insight into the underlying
tests that are specific for frontotemporal neurologic condition, and formal neu-
lobar degeneration neuropathology,11 ropsychological testing with normative
excluding these alternative etiologies scores can be helpful to detect subtle
with ancillary testing is important. In deficits in highly educated patients.
Case 1<3, knife-edge frontal atrophy Longitudinal assessment in neurode-
associated with FTD can be seen clearly, generative conditions that are char-
but many patients may have equivocal acteristically progressive can be
or no signs of cortical atrophy at diag- particularly informative. Finally, history
nosis despite florid behavioral changes. taking should include a detailed ac-
In these circumstances, fluorodeoxy- count of events at home for activities
glucose positron emission tomography of daily living to prevent cognitive
(FDG-PET) can be helpful to determine impairmentYinduced morbidity and
400 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
mortality. Since neurodegenerative 9. Evans J, Olm C, McCluskey L, et al. Impaired
cognitive flexibility in amyotrophic lateral
disease diagnosis is obtained at au- sclerosis. Cogn Behav Neurol 2015;28(1):
topsy, careful evaluation with laboratory 17Y26. doi:10.1097/WNN.0000000000000049.
and neuroimaging testing is neces- 10. Irwin D, Lippa CF, Swearer JM. Cognition and
sary to rule out non-neurodegenerative amyotrophic lateral sclerosis (ALS). Am J
mimics. Emerging biomarkers for AD, Alzheimers Dis Other Demen 2007;22(4):
300Y312. doi:10.1177/1533317507301613.
PD, DLB, ALS, and FTD will be helpful
to improve diagnosis, especially in 11. Irwin DJ, Cairns NJ, Grossman M, et al.
Frontotemporal lobar degeneration: defining
early-stage or prodromal cases, which phenotypic diversity through personalized
will enhance development of mean- medicine. Acta Neuropathol 2015;129(4):
ingful disease-modifying therapies for 469Y491. doi:10.1007/s00401-014-1380-1.
these conditions. 12. Weintraub D. Dopamine and impulse
control disorders in Parkinsons disease.
Ann Neurol 2008;64(suppl 2):S93YS100.
REFERENCES doi:10.1002/ana.21454.
1. Avants BB, Libon DJ, Rascovsky K, et al.
Sparse canonical correlation analysis relates 13. Folstein MF, Folstein SE, McHugh PR.
network-level atrophy to multivariate Mini-mental state. A practical method for
cognitive measures in a neurodegenerative grading the cognitive state of patients for
population. Neuroimage 2014;84:698Y711. the clinician. J Psychiatr Res 1975;12(3):
doi:10.1016/j.neuroimage.2013.09.048. 189Y198. doi:10.1016/0022-3956(75)90026-6.
2. Bonner MF, Peelle JE, Cook PA, Grossman M. 14. Mathuranath PS, Nestor PJ, Berrios GE, et al.
Heteromodal conceptual processing in the A brief cognitive test battery to differentiate
angular gyrus. Neuroimage 2013;71:175Y186. Alzheimers disease and frontotemporal
doi:10.1016/j.neuroimage.2013.01.006. dementia. Neurology 2000;55(11):1613Y1620.
3. Grossman M, Peelle JE, Smith EE, et al. doi:10.1212/01.wnl.0000434309.85312.19.
Category-specific semantic memory: 15. Nasreddine ZS, Phillips NA, Bedirian V, et al.
converging evidence from bold fMRI and The Montreal Cognitive Assessment, MoCA:
Alzheimers disease. Neuroimage 2013;68: a brief screening tool for mild cognitive
263Y274. doi:10.1016/j.neuroimage.2012.11.057. impairment. J Am Geriatr Soc 2005;53(4):
4. Cooke A, Grossman M, DeVita C, et al. 695Y699. doi:10.1111/j.1532-5415.2005.53221.x.
Large-scale neural network for sentence
16. Libon DJ, Rascovsky K, Gross RG, et al. The
processing. Brain Lang 2006;96(1):14Y36. Philadelphia Brief Assessment of Cognition
doi:10.1016/j.bandl.2005.07.072. (PBAC): a validated screening measure for
5. Grossman M, McMillan C, Moore P, et al. dementia. Clin Neuropsychol 2011;25(8):
Whats in a name: voxel-based morphometric 1314Y1330. doi:10.1080/13854046.2011.631585.
analyses of MRI and naming difficulty in
17. Ash S, Evans E, OShea J, et al. Differentiating
Alzheimers disease, frontotemporal
dementia and corticobasal degeneration. primary progressive aphasias in a brief
Brain 2004;127(pt 3):628Y649. doi:10.1093/ sample of connected speech. Neurology
2013;81(4):329Y336. doi:10.1212/WNL.
brain/awh075.
0b013e31829c5d0e.
6. Healey ML, McMillan CT, Golob S, et al.
Getting on the same page: the neural basis 18. Charles D, Olm C, Powers J, et al. Grammatical
for social coordination deficits in behavioral comprehension deficits in non-fluent/agrammatic
variant frontotemporal degeneration. primary progressive aphasia. J Neurol Neurosurg
Neuropsychologia 2015;69:56Y66. doi:10. Psychiatry 2014;85(3):249Y256. doi:10.1136/
1016/j.neuropsychologia.2015.01.028. jnnp-2013-305749.
7. Grossman M, Powers J, Ash S, et al. 19. Loring DW, Martin RC, Meador KJ,
Disruption of large-scale neural networks in Lee GP. Psychometric construction of
non-fluent/agrammatic variant primary the Rey-Osterrieth Complex Figure:
progressive aphasia associated with methodological considerations and
frontotemporal degeneration pathology. interrater reliability. Arch Clin Neuropsychol
Brain Lang 2013;127(2):106Y120. doi:10. 1990;5(1):1Y14. doi:10.1093/arclin/5.1.1.
1016/j.bandl.2012.10.005. 20. Spencer RJ, Wendell CR, Giggey PP, et al.
8. Irwin DJ, White MT, Toledo JB, et al. Judgment of Line Orientation: an examination
Neuropathologic substrates of Parkinson of eight short forms. J Clin Exp Neuropsychol
disease dementia. Ann Neurol 2012;72(4): 2013;35(2):160Y166. doi:10.1080/13803395.
587Y598. doi:10.1002/ana.23659. 2012.760535.
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 401
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Mental Status Examination
21. Marshall JC, Halligan PW. Seeing the Alzheimers Res Ther 2014;6(4):46.
forest but only half the trees? Nature doi:10.1186/alzrt274.
1995;373(6514):521Y523. doi:10.1038/
32. Strong MJ, Grace GM, Freedman M, et al.
373521a0.
Consensus criteria for the diagnosis of
22. Heilman KM, Watson RT. The disconnection frontotemporal cognitive and behavioural
apraxias. Cortex 2008;44(8):975Y982. syndromes in amyotrophic lateral sclerosis.
doi:10.1016/j.cortex.2007.10.010. Amyotroph Lateral Scler 2009;10(3):131Y146.
doi:10.1080/17482960802654364.
23. Spotorno N, McMillan CT, Powers JP, et al.
Counting or chunking? Mathematical 33. McKeith IG, Dickson DW, Lowe J, et al.
and heuristic abilities in patients with Diagnosis and management of dementia
corticobasal syndrome and posterior with Lewy bodies: third report of the DLB
cortical atrophy. Neuropsychologia Consortium. Neurology 2005;65(12):
2014;64C:176Y183. doi:10.1016/ 1863Y1872. doi:10.1212/01.wnl.
j.neuropsychologia.2014.09.030. 0000187889.17253.b1.
24. Cummings JL, Mega M, Gray K, et al. The 34. Kansal K, Irwin DJ. The use of cerebrospinal
Neuropsychiatric Inventory: comprehensive fluid and neuropathologic studies in
assessment of psychopathology in dementia. neuropsychiatry practice and research.
Neurology 1994;44(12):2308Y2314. Psychiatr Clin North Am 2015;38(2):309Y322.
doi:10.1212/WNL.44.12.2308. doi:10.1016/j.psc.2015.02.002.
25. Kertesz A, Davidson W, Fox H. Frontal behavioral 35. Johnson KA, Minoshima S, Bohnen NI, et al.
inventory: diagnostic criteria for frontal lobe Appropriate use criteria for amyloid PET: a
dementia. Can J Neurol Sci 1997;24(1):29Y36. report of the Amyloid Imaging Task Force,
the Society of Nuclear Medicine and Molecular
26. Jack CR Jr, Albert MS, Knopman DS, et al.
Imaging, and the Alzheimers Association.
Introduction to the recommendations from the
National Institute on Aging-Alzheimers Alzheimers Dement 2013;9(1):e-1Ye-16.
Association workgroups on diagnostic doi:10.1016/j.jalz.2013.01.002.
guidelines for Alzheimers disease. Alzheimers 36. Shaw LM, Vanderstichele H, Knapik-Czajka
Dement 2011;7(3):257Y262. doi:10.1016/j. M, et al. Cerebrospinal fluid biomarker
jalz.2011.03.004. signature in Alzheimers disease neuroimaging
initiative subjects. Ann Neurol 2009;65(4):
27. Sperling RA, Aisen PS, Beckett LA, et al.
403Y413. doi:10.1002/ana.21610.
Toward defining the preclinical stages of
Alzheimers disease: recommendations from 37. De Meyer G, Shapiro F, Vanderstichele H,
the National Institute on Aging-Alzheimers et al. Diagnosis-independent Alzheimer
Association workgroups on diagnostic disease biomarker signature in cognitively
guidelines for Alzheimers disease. Alzheimers normal elderly people. Arch Neurol
Dement 2011;7(3):280Y292. doi:10.1016/j. 2010;67(8):949Y956. doi:10.1001/
jalz.2011.03.003. archneurol.2010.179.
28. Irwin DJ, Lee VM, Trojanowski JQ. 38. Tapiola T, Alafuzoff I, Herukka SK, et al.
Parkinsons disease dementia: convergence Cerebrospinal fluid {beta}-amyloid 42 and
of !-synuclein, tau and amyloid-" pathologies. tau proteins as biomarkers of Alzheimer-type
Nat Rev Neurosci 2013;14(9):626Y636. pathologic changes in the brain. Arch Neurol
doi:10.1038/nrn3549. 2009;66(3):382Y389. doi:10.1001/
archneurol.2008.596.
29. Albert MS, DeKosky ST, Dickson D, et al. The
diagnosis of mild cognitive impairment due 39. Mattsson N, Andreasson U, Persson S, et al.
to Alzheimers disease: recommendations The Alzheimers Association external
from the National Institute on Aging-Alzheimers quality control program for cerebrospinal
Association workgroups on diagnostic fluid biomarkers. Alzheimers Dement
guidelines for Alzheimers disease. Alzheimers 2011;7(4):386Y395.e6. doi:10.1016/
Dement 2011;7(3):270Y279. doi:10.1016/ j.jalz.2011.05.2243.
j.jalz.2011.03.008. 40. Shaw LM, Vanderstichele H, Knapik-Czajka M,
30. Litvan I, Goldman JG, Troster AI, et al. Diagnostic et al. Qualification of the analytical and
criteria for mild cognitive impairment in clinical performance of CSF biomarker analyses
Parkinsons disease: Movement Disorder in ADNI. Acta Neuropathol 2011;121(5):
Society Task Force guidelines. Mov Disord 597Y609. doi:10.1007/s00401-011-0808-0.
2012;27(3):349Y356. doi:10.1002/mds.24893.
41. Siderowf A, Xie SX, Hurtig H, et al. CSF
31. Donaghy PC, McKeith IG. The clinical amyloid {beta} 1-42 predicts cognitive decline
characteristics of dementia with Lewy bodies in Parkinson disease. Neurology 2010;75(12):
and a consideration of prodromal diagnosis. 1055Y1061. doi:10.1212/WNL.0b013e3181f39a78.
402 www.ContinuumJournal.com April 2016
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
42. Kang JH, Irwin DJ, Chen-Plotkin AS, et al. 1945Y1952. doi:10.1212/01.wnl.
Association of cerebrospinal fluid "-amyloid 0000436625.63650.27.
1-42, T-tau, P-tau181, and !-synuclein levels 45. Kipps CM, Hodges JR, Hornberger M.
with clinical features of drug-naive patients Nonprogressive behavioural frontotemporal
with early Parkinson disease. JAMA Neurol dementia: recent developments and
2013;70(10):1277Y1287. doi:10.1001/ clinical implications of the bvFTD
jamaneurol.2013.3861. phenocopy syndrome. Curr Opin Neurol
43. Grossman M, Elman L, McCluskey L, et al. 2010;23(6):628Y632. doi:10.1097/WCO.
Phosphorylated tau as a candidate biomarker 0b013e3283404309.
for amyotrophic lateral sclerosis. JAMA Neurol 46. Irwin DJ, McMillan CT, Toledo JB, et al.
2014;71(4):442Y448. doi:10.1001/
Comparison of cerebrospinal fluid levels of
jamaneurol.2013.6064.
tau and A" 1-42 in Alzheimer disease and
44. Hu WT, Watts K, Grossman M, et al. frontotemporal degeneration using 2
Reduced CSF p-Tau181 to Tau ratio is a analytical platforms. Arch Neurol 2012;69(8):
biomarker for FTLD-TDP. Neurology 2013;81(22): 1018Y1025. doi:10.1001/archneurol.2012.26.
Continuum (Minneap Minn) 2016;22(2):385403 www.ContinuumJournal.com 403
Copyright American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- ChakraДокумент29 страницChakrapangsai3000100% (6)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Personality DisordersДокумент4 страницыPersonality DisordersZam Pamate100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Neuropsychological Neurology The Neurocognitive Impairments of Neurological Disorders PDFДокумент244 страницыNeuropsychological Neurology The Neurocognitive Impairments of Neurological Disorders PDFIKFR Unpad100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- BoardReviewClass PsychiatryДокумент28 страницBoardReviewClass PsychiatryyepherenowОценок пока нет
- Youre CrazyДокумент229 страницYoure CrazyNancy Deloach100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- DementiaДокумент874 страницыDementiaKoko Riko100% (3)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Shop Resource PackДокумент130 страницShop Resource PackAndreea BirceaОценок пока нет
- Examination Skills of The Musculoskeletal SystemДокумент80 страницExamination Skills of The Musculoskeletal SystemMarcela Garzon O VelezОценок пока нет
- Kenneth M Heilman (Editor) - Cognitive Changes and The Aging Brain-Cambridge University Press (2019)Документ331 страницаKenneth M Heilman (Editor) - Cognitive Changes and The Aging Brain-Cambridge University Press (2019)da ma100% (1)
- Geriatric Medicine CasesДокумент311 страницGeriatric Medicine CasesShahnaaz Shah100% (7)
- DementiaДокумент26 страницDementianadya100% (4)
- Ageing Myth RealityДокумент44 страницыAgeing Myth RealityVijaya RaniОценок пока нет
- CHCAGE005 Student Assessment Booklet - AGE (ID 97114)Документ109 страницCHCAGE005 Student Assessment Booklet - AGE (ID 97114)Francis Dave Peralta BitongОценок пока нет
- CJL NCM 105 Obe Lec FinalДокумент11 страницCJL NCM 105 Obe Lec FinalCarissa De Luzuriaga-BalariaОценок пока нет
- CBT 2021 ReviewerДокумент63 страницыCBT 2021 ReviewerJasmine100% (5)
- Lecture1 Care of Older AdultДокумент3 страницыLecture1 Care of Older AdultAlliah Grejie AnneОценок пока нет
- Standard Operating Procedure 180 - Missing Persons - 180-MissingpersonsДокумент15 страницStandard Operating Procedure 180 - Missing Persons - 180-MissingpersonsDisability Rights AllianceОценок пока нет
- A Predictive Diagnostic Model Using Multiparametric MRI For Differentiating Uterine Carcinosarcoma From Carcinoma of The Uterine CorpusДокумент12 страницA Predictive Diagnostic Model Using Multiparametric MRI For Differentiating Uterine Carcinosarcoma From Carcinoma of The Uterine CorpusMarcela Garzon O VelezОценок пока нет
- Surgical Treatment of Epilepsy in Adults - UpToDateДокумент24 страницыSurgical Treatment of Epilepsy in Adults - UpToDateMarcela Garzon O VelezОценок пока нет
- Management of Severe Asymptomatic Hypertension (Hypertensive Urgencies) in Adults - UpToDateДокумент16 страницManagement of Severe Asymptomatic Hypertension (Hypertensive Urgencies) in Adults - UpToDateMarcela Garzon O VelezОценок пока нет
- Medication Overuse Headache - Treatment and Prognosis - UpToDateДокумент16 страницMedication Overuse Headache - Treatment and Prognosis - UpToDateMarcela Garzon O VelezОценок пока нет
- COVID-19: A Brief Overview of The Discovery Clinical Trial: PharmaceuticalsДокумент8 страницCOVID-19: A Brief Overview of The Discovery Clinical Trial: PharmaceuticalsMarcela Garzon O VelezОценок пока нет
- Alterations of The Gut Microbiome in Chinese PatieДокумент7 страницAlterations of The Gut Microbiome in Chinese PatieMarcela Garzon O VelezОценок пока нет
- Patient Blood Management. A Fresh Look at A Fresh Approach To Blood Transfusion PDFДокумент11 страницPatient Blood Management. A Fresh Look at A Fresh Approach To Blood Transfusion PDFMarcela Garzon O VelezОценок пока нет
- Cholinesterase Inhibitors in The Treatment of Alzheimer Disease - UpToDate PDFДокумент22 страницыCholinesterase Inhibitors in The Treatment of Alzheimer Disease - UpToDate PDFMarcela Garzon O VelezОценок пока нет
- BullFacPhysTher23294-5840368 161323Документ7 страницBullFacPhysTher23294-5840368 161323Marcela Garzon O VelezОценок пока нет
- Antenatal Betamethasone For WomenДокумент10 страницAntenatal Betamethasone For WomenMarcela Garzon O VelezОценок пока нет
- Med StudyДокумент7 страницMed StudyMarcela Garzon O VelezОценок пока нет
- Ags Panel On Persistent Pain in Older Persons PDFДокумент20 страницAgs Panel On Persistent Pain in Older Persons PDFHery SezanoОценок пока нет
- 2007, Vol.25, Issues 3, DementiaДокумент279 страниц2007, Vol.25, Issues 3, Dementiajeaje100% (1)
- Specimen Bmat 2014 Section 1 Question PaperДокумент32 страницыSpecimen Bmat 2014 Section 1 Question PaperElena EngiОценок пока нет
- Kinsella 2015Документ13 страницKinsella 2015Lia UsatiucОценок пока нет
- Early Alzheimer's Guide For FamiliesДокумент8 страницEarly Alzheimer's Guide For FamiliesAngela Carrillo TrianoОценок пока нет
- Dissertation Questions Mental HealthДокумент4 страницыDissertation Questions Mental HealthWriteMySociologyPaperCanada100% (1)
- Home Safety For People With Alzheimer's DiseaseДокумент44 страницыHome Safety For People With Alzheimer's DiseaseInternational Business Times100% (3)
- Validation of Malay Mini Mental State ExaminationДокумент4 страницыValidation of Malay Mini Mental State ExaminationlawangОценок пока нет
- MHN AbbreviationsДокумент12 страницMHN AbbreviationsRiju DasОценок пока нет
- Neurological Disorders: Causes and Treatments Strategies: April 2018Документ10 страницNeurological Disorders: Causes and Treatments Strategies: April 2018Friska HarianjaОценок пока нет
- Bilingualism As Protection Against The Onset of Symptoms of Dementia Bialystok - Craik - FreedmanДокумент7 страницBilingualism As Protection Against The Onset of Symptoms of Dementia Bialystok - Craik - FreedmanFaruk AcarОценок пока нет
- 10 Benefits of ReadingДокумент4 страницы10 Benefits of Readingkanand_7Оценок пока нет
- Caregivers For Compromise PaperДокумент2 страницыCaregivers For Compromise PaperChris VaughnОценок пока нет
- Dementia Conversion DisordersДокумент28 страницDementia Conversion DisordersAYO NELSON100% (1)