Академический Документы
Профессиональный Документы
Культура Документы
Copd Clinical Practice Guideline For The Management Patient Guide
Загружено:
nurulОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Copd Clinical Practice Guideline For The Management Patient Guide
Загружено:
nurulАвторское право:
Доступные форматы
VA/DoD CLINICAL PRACTICE GUIDELINE FOR
THE MANAGEMENT OF CHRONIC OBSTRUCTIVE
PULMONARY DISEASE
Department of Veterans Affairs
Department of Defense
Patient Guide
QUALIFYING STATEMENTS
The Department of Veterans Affairs and the Department of Defense guidelines are based upon the best
information available at the time of publication. They are designed to provide information and assist
decision-making. They are not intended to define a standard of care and should not be construed as one.
Neither should they be interpreted as prescribing an exclusive course of management.
This Clinical Practice Guideline is based on a systematic review of both clinical and epidemiological
evidence. Developed by a panel of multidisciplinary experts, it provides a clear explanation of the logical
relationships between various care options and health outcomes while rating both the quality of the
evidence and the strength of the recommendations.
Variations in practice will inevitably and appropriately occur when clinicians take into account the needs of
individual patients, available resources, and limitations unique to an institution or type of practice. Every
healthcare professional making use of these guidelines is responsible for evaluating the appropriateness of
applying them in the setting of any particular clinical situation.
These guidelines are not intended to represent TRICARE policy. Further, inclusion of recommendations for
specific testing and/or therapeutic interventions within these guidelines does not guarantee coverage of
civilian sector care. Additional information on current TRICARE benefits may be found at www.tricare.mil
or by contacting your regional TRICARE Managed Care Support Contractor.
Version 3.0 2014
December 2014 Page 1 of 6
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease, or COPD, is a combination of ongoing conditions that affect
your lungs and breathing. These conditions can include chronic bronchitis and emphysema.
COPD can be prevented and treated. It can be recognized by its key characteristic: difficulty breathing,
especially when breathing out. However, if you have COPD, you may have other symptoms.
Did You Know?
Veterans are at higher risk of COPD than those in the general US population. [1]
Because some of their activities may pose a risk of environmental and occupational exposure, people
in the military should be aware of COPD and know the signs that a person may have it.
The physical activity associated with military life may uncover symptoms of COPD earlier among
people in the armed forces. Patients in the military or veterans may show signs of COPD earlier in their
lives than their civilian counterparts. [2]
What Causes COPD?
People get COPD for different reasons. Often, people with COPD have been exposed to substances that
irritate the lungs for long periods of time. They may smoke tobacco or may have smoked tobacco in the
past. They could also be exposed to substances that irritate their lungs as part of their work or home
environment. This can cause portions of the lungs to stop functioning as they should.
Figure 1: Images of healthy lungs and lungs affected by COPD
Source: https://www.nhlbi.nih.gov/health/educational/copd/what-is-copd/how-does-copd-affect- breathing.htm
December 2014 Page 2 of 6
How is COPD Diagnosed?
Your provider (which may be a doctor, physician assistant, nurse practitioner, or other health care
provider) can help you determine whether or not you have COPD. If your provider suspects you may have
COPD, he or she can arrange for a simple breathing test in order to determine whether you do or do not
have the disease.
What are the Goals of COPD Treatment?
The overall goal of treating your COPD is to optimize your health and your quality of life.
Goals of COPD Treatment
Prevent COPD from progressing
Improve symptoms:
o Breathing
o Exercise tolerance
o Quality of life
Treat and prevent:
o Exacerbations (when symptoms suddenly worsen)
o Complications
What are the Options for COPD Treatment?
There are multiple treatment options for COPD that can help you reach the previously listed goals. By
consulting with a provider, you can learn more about the available treatment options and how they can
help you. Work with your provider to identify treatments that improve your symptoms and your health.
The following treatment options are things that your provider may ask you to do at home or to make a
part of your normal routine.
Medication
Your provider may prescribe medication that you breathe in, so it goes straight to your lungs. The
medication can help you keep your symptoms from worsening or help manage your COPD. With minimal
practice and instruction, these medications can be easy to use. You should ask for help and work with your
provider to make sure that you are taking it correctly and as directed. There are many different types of
medication. These medications work in different ways and affect different parts of the lungs in order to
help improve your breathing.
Medications work for different lengths of time depending on the medication type (short-acting or long-
acting).
Short-acting medications work relatively quickly. When you are experiencing symptoms that are worse
than normal, you should use short-acting medications.
Long-acting medications help you to make sure your COPD does not worsen. You should take long-
acting medications even if you do not feel like your COPD is worse than normal.
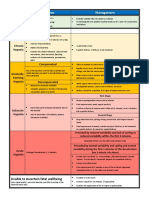
More information on types of medications can be found in Table 1.
December 2014 Page 3 of 6
Table 1: Types of Medication Used to Treat COPD
Types and Examples of the
Medication How It Works How Long It Works
Abbreviations Medications
Relaxes muscles Short-acting Works in 1-5 minutes; albuterol
around small airways (SABA) lasts 3-6 hours levalbuterol
Beta 2-agonist
to increase space Long-acting Works in 20 minutes; formoterol
inside (LABA) lasts 4-6 hours salmeterol
Short-acting Works in 15 minutes;
Prevents muscles ipratropium
(SAMA) lasts 6-8 hours
Antimuscarinic around large airways
Long-acting Works in 20 minutes;
from tightening tiotropium
(LAMA) lasts 24 hours
Reduces and
Inhaled Long-acting Works in a few days- beclomethasone
prevents swelling in
corticosteroid (ICS) a few weeks fluticasone
the airways
There are other medications such as theophylline, roflumilast, and chronic macrolides. Your provider may
prescribe one of these after consulting with a pulmonologist.
Other Treatment Options
Your provider may discuss other forms of treatment with you. These may include:
Oxygen therapy
Supported self-management (working with a case manager to help you manage your COPD), and
pulmonary rehabilitation programs
Telehealth
Breathing exercises
Nutrition referral
Surgery
What Should You Do If Your COPD Worsens?
If you are experiencing an exacerbation, which is a sudden worsening in your ability to breath, an increase
in your coughing, or a change in the color of your mucus, you should seek help immediately from the clinic
or emergency department. If your provider has given you an action plan, you may begin your medications.
What Else Can You Do to Improve Your Health?
Quit smoking and avoid secondhand smoke. Ask your provider about ways to do this. Consult the
Department of Veterans Affairs/Department of Defense Clinical Practice Guideline for Treating
Tobacco Use and Dependence (http://www.healthquality.va.gov/guidelines/CD/mtu/) or
http://smokefree.gov/.
Breathe clean air. If there is more pollution than usual in the air outside, stay inside. Avoid spraying
cleaning products or other substances, such as hairspray, that linger in the air. If you do have to use
one of these substances, make sure it is natural and free from harmful chemicals.
December 2014 Page 4 of 6
Eat right and maintain a healthy weight. If you are underweight, you may not have enough energy to
be active or to breathe as well as you can. If you are overweight, your lungs have to work harder.
Make sure you eat the right amount of healthy food to keep your body nourished and get to a healthy
weight.
Get enough rest. Some people with COPD have trouble sleeping. Do not use sleeping pills or over the
counter medications if you are having trouble sleeping. Instead, talk with your provider.
Stay positive. Take steps to reduce stress in your life. Keep a positive outlook. If you feel depressed or
anxious, talk about it with your provider.
Get vaccinated. Illnesses such as a cold or the flu may impact you more than others. Make sure to get
flu shots annually. Get additional vaccinations, such as the one for pneumonia, as they are needed.
Questions to Ask Your Provider
Is my COPD diagnosis confirmed?
How is my COPD progressing compared to an average COPD patient?
Am I taking my medication the correct way? (Take your inhaler with you when you see your provider
or clinical pharmacist and show him or her how you use it.)
What medication should I take when my symptoms are worse than usual?
Should I take any of my medications all the time?
When should I go to the emergency department?
How much activity should I have in my everyday life?
Are there any special exercises I should be doing?
Should I change my diet?
Frequently Asked Questions
If I quit smoking, will it really help my COPD?
Yes, if you still smoke, the single best thing you can do to prevent your COPD from getting worse is to
stop smoking. Ask your provider how he or she can help you stop smoking. You should also avoid
places where other people are smoking. This will help you avoid breathing in secondhand smoke.
Is it safe to be around my family and friends?
Yes, you should still spend time with your family and friends. COPD is not contagious, and you may feel
better after spending time with loved ones. However, if a family member or friend smokes, you should
make sure you are not around them when they are smoking. Also, if one of your family members has a
cold, a cough, or the flu, try to avoid contact with them; because of COPD, if you catch one of these
viruses, you are more likely to have serious complications.
Is it safe for me to receive the flu vaccine and other vaccines that my provider recommends?
Yes, it is safe for you to receive these vaccines. In fact, because of COPD, it is more important for you
to receive the flu vaccine every year and other vaccines that your provider recommends. These can
protect you from serious complications that can happen when people with COPD have these
respiratory infections.
December 2014 Page 5 of 6
You Can Find More Information on COPD and Living with COPD Here:
National Heart Lung and Blood Institute: http://www.nhlbi.nih.gov/health/health-
topics/topics/copd/; 301-592-8573 (dial 7-1-1 for access to free Telecommunications Relay
Services (TRS))
Centers for Disease Control and Prevention: http://www.cdc.gov/copd/; 800-CDC-INFO (800-232-
4636); TTY: (888) 232-6348
References
1. Finklestein J, Cha E. Association of Veteran status with COPD prevalence stratified by gender. Am J
Respir Crit Care Med. 2013;187.
2. Morris MJ, Lucero PF, Zanders TB, Zacher LL. Diagnosis and management of chronic lung disease in
deployed military personnel. Ther Adv Respir Dis. Aug 2013;7(4):235-245.
December 2014 Page 6 of 6
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Annoted Bibliography ObesityДокумент8 страницAnnoted Bibliography Obesityapi-451532782Оценок пока нет
- Pneumonia, COPD, Tuberculosis - ReportДокумент23 страницыPneumonia, COPD, Tuberculosis - ReportJoceelyyn EufemianoОценок пока нет
- Different Therepeutic Category of Drugs and Its Example Drug ProductsДокумент8 страницDifferent Therepeutic Category of Drugs and Its Example Drug ProductsGermie PosionОценок пока нет
- Calories SantosДокумент2 страницыCalories SantosVan SantosОценок пока нет
- Jsa Radiographic Test RTДокумент1 страницаJsa Radiographic Test RTHussein Adnan Fneish100% (1)
- Obstetrics and Gynecology Mock ReviewДокумент14 страницObstetrics and Gynecology Mock ReviewokurimkuriОценок пока нет
- Presentation 1Документ9 страницPresentation 1NgsfbsbsfiОценок пока нет
- Pneumonia Disease Risk FactorsДокумент3 страницыPneumonia Disease Risk FactorsPedialy AvilesОценок пока нет
- Grade 10 Reproductive HealthДокумент26 страницGrade 10 Reproductive HealthMissy BanguisОценок пока нет
- Art Danial FajriansahДокумент8 страницArt Danial FajriansahCici FarochahОценок пока нет
- Surgical MenopauseДокумент5 страницSurgical MenopauseSusan HepziОценок пока нет
- Drinking Water Contaminants in PakistanДокумент4 страницыDrinking Water Contaminants in PakistanSardar Taimur Hyat-KhanОценок пока нет
- Edward Jenner and His ContributionsДокумент2 страницыEdward Jenner and His ContributionsZUBAIDAH BINTI JAMALUDDIN MoeОценок пока нет
- Hypoxia Classification Table - Physiological-CTGДокумент1 страницаHypoxia Classification Table - Physiological-CTGKhánh Nguyễn NgọcОценок пока нет
- An WorkДокумент37 страницAn WorkRaviteja PadiriОценок пока нет
- Basic HACCP Training ModuleДокумент20 страницBasic HACCP Training Moduleyashyash_007100% (8)
- Jurnal Bumil Pingsan 3Документ4 страницыJurnal Bumil Pingsan 3rina astutiОценок пока нет
- COPARДокумент57 страницCOPARCristelle Joy RebocaОценок пока нет
- Deaths From COVID-19 in Healthcare Workers in Italy - What Can We Learn?Документ2 страницыDeaths From COVID-19 in Healthcare Workers in Italy - What Can We Learn?Dimitri MandolesiОценок пока нет
- Cancer PDFДокумент313 страницCancer PDFAmanda TrebianoОценок пока нет
- 6 Laboratory SafetyДокумент17 страниц6 Laboratory SafetyNipun ShamikaОценок пока нет
- Community Medicine PublicationsДокумент5 страницCommunity Medicine PublicationsOm AbdalrahmanОценок пока нет
- NEW - Microplanning Template For COVID-19 VaccinesДокумент43 страницыNEW - Microplanning Template For COVID-19 Vaccinesfeil amor deladaОценок пока нет
- Letter From Ottawa Public Health To Ottawa BusinessesДокумент5 страницLetter From Ottawa Public Health To Ottawa BusinessesCTV OttawaОценок пока нет
- Diplom IşiДокумент4 страницыDiplom IşiXeyal CavadovОценок пока нет
- DRUGS IN PREGNANCY - A Handbook For Pharmacist and Physician 2021 PDFДокумент465 страницDRUGS IN PREGNANCY - A Handbook For Pharmacist and Physician 2021 PDFadelia100% (1)
- Huikahi Restorative CirclesДокумент6 страницHuikahi Restorative CirclesCarl Vincent QuitorianoОценок пока нет
- Automatic Hand Sanitizer DispenserДокумент3 страницыAutomatic Hand Sanitizer DispenserGeojanni PangibitanОценок пока нет
- Hunger & ManutritionДокумент7 страницHunger & ManutritionSubodh BedreОценок пока нет
- Case Study: ScenarioДокумент4 страницыCase Study: ScenarioCheska PalomaОценок пока нет