Академический Документы
Профессиональный Документы
Культура Документы
Clayton, 2009
Загружено:
Anggie AnggriyanaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Clayton, 2009
Загружено:
Anggie AnggriyanaАвторское право:
Доступные форматы
F e a t u r e a r t i c l e
A Review of the Pathophysiology, Classification, and
Treatment of Foot Ulcers in Diabetic Patients
Warren Clayton, Jr., MD, and Tom A. Elasy, MD, MPH
T
he number of people with in animal and in vitro models to be tion leading to ischemia, which will
diabetes worldwide was esti- a result of hyperglycemia-induced promote nerve cell injury and death.
mated at 131 million in 2000; it metabolic abnormalities.911 One Hyperglycemia and oxidative stress
is projected to increase to 366 mil- of the more commonly described also contribute to the abnormal gly-
lion by 2030.1 Previous studies have mechanisms of action is the polyol cation of nerve cell proteins and the
indicated that diabetic patients have pathway.10 In the development of inappropriate activation of protein
up to a 25% lifetime risk of developing neuropathy, the hyperglycemic state kinase C, resulting in further nerve
a foot ulcer.2 The annual incidence of leads to an increase in action of the dysfunction and ischemia.
diabetic foot ulcers is ~ 3%, and the enzymes aldose reductase and sorbi- Neuropathy in diabetic patients
reported incidence in U.S. and U.K. tol dehydrogenase. This results in the is manifested in the motor, auto-
studies ranges as high as 10%.3 conversion of intracellular glucose to nomic, and sensory components
Once an ulcer has developed, sorbitol and fructose. of the nervous system.7 Damage
there is an increased risk of wound The accumulation of these sugar to the innervations of the intrinsic
progression that may ultimately lead products results in a decrease in the foot muscles leads to an imbalance
to amputation; diabetic ulceration between flexion and extension of
synthesis of nerve cell myoinositol,
has been shown to precede amputa- the affected foot. This produces
required for normal neuron con-
tion in up to 85% of cases.3 At least anatomic foot deformities that cre-
duction. Additionally, the chemical
40% of amputations in diabetic ate abnormal bony prominences
conversion of glucose results in a
patients can be prevented with a and pressure points, which gradu-
depletion of nicotinamide adenine
team approach to wound care.4 The ally cause skin breakdown and
purpose of this review is to describe dinucleotide phosphate stores, which
are necessary for the detoxification ulceration.
the causes of lower-extremity ulcer- Autonomic neuropathy leads to
ation in diabetic patients and to of reactive oxygen species and for
the synthesis of the vasodilator nitric a diminution in sweat and oil gland
identify common methods of classifi- functionality. As a result, the foot
cation and treatment to aid primary oxide. There is a resultant increase
loses its natural ability to moisturize
care providers in determining appro- in oxidative stress on the nerve cell
the overlying skin and becomes dry
priate treatment approaches for their and an increase in vasoconstric-
and increasingly susceptible to tears
patients. and the subsequent development of
In Brief
Pathogenesis of Ulceration infection.
Diabetic foot ulcers result from the The development of lower The loss of sensation as a part of
simultaneous action of multiple extremity ulcers is a well known peripheral neuropathy exacerbates
contributing causes.5,6 The major potential complication for the development of ulcerations. As
underlying causes are noted to be patients with diabetes. This arti- trauma occurs at the affected site,
peripheral neuropathy and ischemia cle reviews the common causes patients are often unable to detect
from peripheral vascular disease.7 of diabetic foot ulceration and the insult to their lower extremi-
discusses methods for assessment ties. As a result, many wounds go
Neuropathy and treatment to aid providers in unnoticed and progressively worsen
More than 60% of diabetic foot ulcers developing appropriate strategies as the affected area is continuously
are the result of underlying neuropa- for foot care in individuals with subjected to repetitive pressure and
thy.7,8 The development of neuropathy diabetes shear forces from ambulation and
in affected patients has been shown weight bearing.
52 Volume 27, Number 2, 2009 Clinical Diabetes
F e a t u r e A r t i c l e
Figure 1. Common foot deformities resulting from diabetes complications: A) claw toe deformity (increased pressure is placed
on the dorsal and plantar aspects of the deformity as indicated by the triple arrows); and B) Charcot arthropathy (the rocker-
bottom deformity leads to increased pressure on the plantar midfoot). Adapted from Ref. 13.
Vascular Disease Assessment of Diabetic Foot Ulcers factor to the development of foot
Peripheral arterial disease (PAD) is A task force of the Foot Care Interest ulceration. In the visual inspection
a contributing factor to the develop- Group of the American Diabetes of the foot, the evaluator should
ment of foot ulcers in up to 50% of Association (ADA) released a 2008 check between the toes for the
cases.12,13 It commonly affects the report that specifies recommended presence of ulceration or signs of
tibial and peroneal arteries of the components of foot examinations for infection. The presence of callus or
calf. Endothelial cell dysfunction and patients with diabetes.13 Providers nail abnormalities should be noted.
smooth cell abnormalities develop in should take a history that takes into Additionally, a temperature differ-
peripheral arteries as a consequence consideration previous ulceration or ence between feet is suggestive of
of the persistent hyperglycemic amputation. The history should also vascular disease.
state.9 There is a resultant decrease include any neuropathic symptoms The foot should also be examined
in endothelium-derived vasodilators or symptoms that are suggestive of for deformities. The imbalance in
leading to constriction. Further, the peripheral vascular disease. Further, the innervations of the foot muscles
hyperglycemia in diabetes is associ- providers should inquire about other from neuropathic damage can
ated with an increase in thromboxane complications of diabetes, including lead to the development of com-
A2, a vasoconstrictor and platelet vision impairment suggestive of retin- mon deformities seen in affected
aggregation agonist, which leads to an opathy and nephropathy, especially patients. Hyperextension of the
increased risk for plasma hypercoagu- dialysis or renal transplantation. metatarsal-phalangeal joint with
lability.14 There is also the potential Finally, patients should be questioned interphalangeal or distal phalangeal
for alterations in the vascular extra- regarding smoking because smok- joint flexion leads to hammer toe
cellular matrix leading to stenosis of ing is linked to the development of and claw toe deformities, respec-
the arterial lumen.14 Moreover, smok- neuropathic and vascular disease. A tively. The Charcot arthropathy is
ing, hypertension, and hyperlipidemia complete history will aid in assessing another commonly mentioned defor-
are other factors that are common in the risk for foot ulceration.13 mity found in some affected diabetic
diabetic patients and contribute to the In examining the foot, visual patients. It is the result of a com-
development of PAD.5 Cumulatively, inspection of the bare foot should bination of motor, autonomic, and
this leads to occlusive arterial disease be performed in a well-lit room. sensory neuropathies in which there
that results in ischemia in the lower The examination should include an is muscle and joint laxity that lead
extremity and an increased risk of assessment of the shoes; inappropri- to changes in the arches of the foot.
ulceration in diabetic patients. ate footwear can be a contributing Further, the autonomic denervation
Clinical Diabetes Volume 27, Number 2, 2009 53
F e a t u r e A r t i c l e
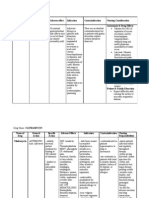
leads to bone demineralization via Table 1. Wagner Ulcer Classification System
the impairment of vascular smooth
muscle, which leads to an increase in Grade Lesion
blood flow to the bone with a conse- 1 Superficial diabetic ulcer
quential osteolysis. An illustration of 2 Ulcer extension involving ligament, tendon, joint capsule, or fascia
some commonly described abnor- with no abscess or osteomyelitis
malities is shown in Figure 1.
In examining for vascular 3 Deep ulcer with abscess or osteomyelitis
abnormalities of the foot, the 4 Gangrene to portion of forefoot
dorsalis pedis and posterior tibial
5 Extensive gangrene of foot
pulses should be palpated and
characterized as present or absent.15 Table 2. University of Texas Wound Classification System
Claudication, loss of hair, and the
Stages Description
presence of pale, thin, shiny, or cool
skin are physical findings suggestive Stage A No infection or ischemia
of potential ischemia. If vascular Stage B Infection present
disease is a concern, measuring the
ankle brachial index (ABI) can be Stage C Ischemia present
used in the outpatient setting for Stage D Infection and ischemia present
determining the extent of vascu-
lar disease and need for referral to
a vascular specialist. The ABI is Grading Description
obtained by measuring the systolic Grade 0 Epithelialized wound
blood pressures in the ankles (dorsa- Grade 1 Superficial wound
lis pedis and posterior tibial arteries)
and arms (brachial artery) using a Grade 2 Wound penetrates to tendon or capsule
handheld Doppler and then calcu- Grade 3 Wound penetrates to bone or joint
lating a ratio. Ratios below 0.91 are
suggestive of obstruction. However, the foot with enough pressure to for wound depth and appearance
in patients with calcified, poorly bend it.17 Areas of callus should not and does not consider the presence
compressible vessels or aortoiliac be tested.13 of ischemia or infection.13,21
stenosis, the results of the ABI can The University of Texas system
Classification of Diabetic Foot Ulcers is another classification system
be complicated.16 If there is a strong
The results of the foot evaluation that addresses ulcer depth and
suspicion of vascular disease, the
patient should undergo vascular should aid in developing an appropri- includes the presence of infection
imaging as an alternate method of ate management plan.18 If an ulcer is and ischemia (Table 2).22 Wounds of
testing to determine the extent of discovered, the description should increasing grade and stage are less
disease and possible ischemia.5 include characteristics of the ulcer, likely to heal without vascular repair
The loss of pressure sensation including size, depth, appearance, and or amputation.21
in the foot has been identified as location.19 There are many classifica-
a significant predictive factor for tion systems used to depict ulcers that Treatment Modalities
the likelihood of ulceration. A can aid in developing a standardized The management of diabetic foot
screening tool in the examination method of description. These classifi- ulcers includes several facets of care.
of the diabetic foot is the 10-gauge cation systems are based on a variety Offloading and debridement are
monofilament. The monofilament of physical findings. considered vital to the healing process
is tested on various sites along the One of the most popular systems for diabetic foot wounds.23 The goal of
plantar aspect of the toes, the ball of classification is the Wagner Ulcer offloading is to redistribute force from
of the foot, and between the great Classification System, which is based ulcers sites and pressure points at
and second toe. The test is consid- on wound depth and the extent of risk to a wider area of contact. There
ered reflective of an ulcer risk if the tissue necrosis (Table 1).20 Several are multiple methods of pressure
patient is unable to sense the mono- authors have noted a disadvantage of relief, including total contact casting,
filament when it is pressed against this system in that it only accounts half shoes, removable cast walkers,
54 Volume 27, Number 2, 2009 Clinical Diabetes
F e a t u r e A r t i c l e
wheelchairs, and crutches. There are changes and wound inspection antibiotic therapy or who need close
advantages and disadvantages to each should occur on a daily basis.26 monitoring for treatment response.28
modality, and factors such as overall If infection is suspected in the In the absence of serious signs,
wound condition, required frequency wound, the selection of appropriate patients can be treated with out-
for assessment, presence of infec- treatments should be based on the patient therapy and frequent
tion, and the likelihood for patient results of a wound culture. Tissue follow-up.30 Although a detailed
compliance should be considered in curettage from the base of the ulcer discussion of the range of antibi-
determining which modality would be after debridement will reveal more otic therapy is beyond the scope
most beneficial to the patient.24 accurate results than a superficial of this review, common classes of
The open diabetic foot ulcer wound swab.28In the case of deep agents used include cephalosporins,
may require debridement if necrotic tissue infections, specimens obtained fluoroquinolones, and penicillin/B-
or unhealthy tissue is present. The aseptically during surgery provide lactamase inhibitors. Information
debridement of the wound will optimalresults.28 about specificagents that have
include the removal of surround- Gram-positive cocci are typi- shown clinical effectiveness and sug-
ing callus and will aid in decreasing cally the most common pathogens gested treatment schemes based on
pressure points at callused sites on isolated. However, chronic or previ- infection severity has been published
the foot. Additionally, the removal of ously treated wounds often show elsewhere.25,28
unhealthy tissue can aid in removing polymicrobial growth, including The possibility of underlying
colonizing bacteria in the wound. It gram-negative rods or anaerobes. osteomyelitis should be considered
will also facilitate the collection of Pseudomonas, for example, is often with the presence of exposed bone
appropriate specimens for culture cultured from wounds that have been or bone that can be palpated with
soaked or treated with wet dress- a blunt probe. If osteomyelitis is
and permit examination for the
ings. Anaerobic bacteria are often diagnosed, the patient may undergo
involvement of deep tissues in the
cultured from ulcers with ischemic surgical excision of the affected bone
ulceration.25
necrosis or deep tissue involvement. or an extensive course of antibiotic
The selection of wound dressings
Antibiotic-resistant organisms such therapy.5
is also an important component of
as methicillin-resistant staphylo- Consideration is also given to
diabetic wound care management.
coccus aureus are frequently found the presence of underlying isch-
There are a number of available
in patients previously treated with emia because an adequate arterial
dressing types to consider in the
antibiotic therapy or patientswith a blood supply is necessary to facili-
course of wound care. Although
recent history of hospitalization or tate wound healing and to resolve
there is a dearth of published trials residence in a long-term care facility. underlying infections. Patients with
to support the use of one type of The selection of appropriate evidence of decreased distal blood
dressing compared to another,26 the antimicrobial therapy, including flow or ulceration that does not
characteristics of specific dressing the agent, route of administration, progress toward healing with appro-
types can prove beneficial depending and need for inpatientor outpatient priate therapy should be referred to
on the characteristics of the indi- treatment will be determined in a vascular specialist. Upon deter-
vidual wound. Saline-soaked gauze part by the severity of the infection. mination of the patients anatomy
dressings, for example, are inexpen- Clinical signs of purulent drainage, and a vascular route amenable to
sive, well tolerated, and contribute to inflammatory signs of increased restoration, the patient may undergo
an atraumatic, moist wound environ- warmth, erythema, pain and indura- arterial revascularization.
ment. Foam and alginate dressings tion, or systemic signs such as fever Surgical bypass is a common
are highly absorbent and can aid in or leukocytosis should be consid- method of treatment for ischemic
decreasing the risk for maceration ered. Patients with systemic signs of limbs, and favorable long-term
in wounds with heavy exudates. A severe infection should be admitted results have been reported.31 Up
complete discussion of the various for supportive care and intravenous to a 90% 10-year limb-salvage rate
classes of wound dressings is beyond antibiotic therapy; additionally, a has been demonstrated with surgi-
the scope of this review; however, an surgical evaluation is warranted to cal bypass procedures of the lower
ideal dressing should contribute to evaluate for a deep occult infection.29 extremity.32 In cases in which there
a moist wound environment, absorb Inpatient care is also suggested for are multiple levels of occlusion,
excessive exudates, and not increase patients who are not able to provide revascularization at each point is
the risk for infections.27 Dressing proper self-care or comply with necessary to restore arterial blood
Clinical Diabetes Volume 27, Number 2, 2009 55
F e a t u r e A r t i c l e
flow and increase the chance for limb use of granulocyte colony stimulat- adequately powered randomized
salvage.31 Transluminal angioplasty ing factors (G-CSF). HBOT is the trial.39
of the iliac arteries in conjunction delivery of oxygen to patients at However, the Center for Medicare
with surgical bypass in the distal higher than normal atmospheric & Medicaid Services has approved
extremity may be implemented, and
pressures. This results in an increase reimbursement of HBOT for 14
efficacy has been demonstrated in
diabetic patients.33 in the concentration of oxygen in the conditions, including diabetic
A number of adjunctive wound blood and an increase in the dif- ulcers. Diabetic wounds that meet
care treatments are under investi- fusion capacity to the tissues. The the appropriate criteria are classi-
gation and in practice for treating partial pressure of oxygen in the fied as WagnerGrade 3 wounds that
diabetic foot ulcers. The use of tissues is increased, which stimulates
have failed to resolve after a 30-day
human skin equivalents has been neovascularization and fibroblast
shown to promote wound healing course of standard treatment.
replication and increases phagocyto-
in diabetic ulcers via the action The use of G-CSF is another new
sis and leukocyte-mediated killing of
of cytokines and dermal matrix adjunctive therapy under inves-
components that stimulate tissue bacterial pathogens in the wound.
tigation. G-CSF has been found
growth and wound closure.34,35 A Presently, there are conflicting
to enhance the activity of neutro-
recombinant platelet-derived growth data regarding the efficacy of this
factor is also currently in use and therapy. Although small random- phils in diabetic patients.40 A small
has been shown to stimulate wound izedstudies have demonstrated an number of studies have investigated
healing.36 However, the present data improvement in the rate of wound the use of G-CSF as an adjunctive
for most of these modalities are not healing and a decrease in the num- therapy. A meta-analysis of these
considered sufficient for routine studies41 revealed that, although the
ber of amputations,37,38 other studies
implementation in the treatment of
contest these data. The quality of use of G-CSF did not significantly
diabetic wounds.25
Two of the more popular adjunc- the studies to date has been poor, accelerate the resolution of infec-
tive therapies in use are hyperbaric and their findings have not been tion in diabetic wounds, there was a
oxygen therapy (HBOT) and the confirmed in a large, blinded, and decreased likelihood of amputation
Table 3. Risk Classification System of the Task Force of the Foot Care Interest Group of the ADA
Risk Category Definition Treatment Recommendations Suggested Follow-up
0 No LOPS, no PAD, no Consider patient education on Annually (by generalist and/or specialist)
deformity foot care, including information
on appropriate footwear.
1 LOPS deformity Consider prescriptive or accom- Every 36 months (by generalist or
modative footwear. specialist)
Consider prophylactic surgery
if deformity is not able to be
safely accommodated in shoes.
Continue patient education.
2 PAD LOPS Consider the use of accommoda- Every 23 months (by specialist)
tive footwear.
Consider a vascular consultation
for combined follow-up.
3 History of ulcer or Consider patient education on Every 12 months (by specialist)
amputation foot care.
Consider vascular consultation
for combined follow-up if PAD
present.
LOPS, loss of protective sensation; PAD, peripheral arterial disease. Adapted from Ref. 13.
56 Volume 27, Number 2, 2009 Clinical Diabetes
F e a t u r e A r t i c l e
and the need for other surgical thera- If ulcers are present, the treat- esis of diabetic neuropathy. Curr Opin Neurol
5:553563, 1999
pies in treated wounds. ment strategy should include 11
Simmons Z, Feldman E: Update on
offloading, debridement, and diabetic neuropathy. Curr Opin Neurol
Prevention appropriate dressings. Further, the 15:595603, 2002
Early detection of potential risk fac- presence of infections should be 12
Huijberts MS, Schaper NC, Schalkwijk
tors for ulceration can decrease the determined by clinical findings and CG: Advanced glycation end products and
diabetic foot disease. Diabetes Metab Res Rev
frequency of wound development. It appropriate wound cultures and 24 (Suppl. 1):S19S24, 2008
is recommended that all patients with treated based on the culture results. 13
Boulton AJ, Armstrong DG, Albert
diabetes undergo foot examinations at If evidence for ischemia is present, SF, Frykberg RG, Hellman R, Kirkman
least annually to determine predis- MS, Lavery LA, LeMaster JW, Mills JL
revascularization may be indicated Sr, Mueller MJ, Sheehan P, Wukich DK:
posing conditions to ulceration.13 to restore arterial blood flow and Comprehensive foot examination and risk
Patients should be educated regarding assessment. Diabetes Care 31:16791685, 2008
increase the chance for limb sal-
the importance of maintaining good vage. There are adjunctive therapies
14
Paraskevas KI, Baker DM, Pompella
A, Mikhailidis DP: Does diabetes mellitus
glycemic control, wearing appropriate available that can also contribute play a role in restenosis and patency rates
footwear, avoiding trauma, and per- to the overall healing process of the following lower extremity peripheral arterial
revascularization? A critical overview. Ann
forming frequent self-examinations.25 wounds in affected patients. Vasc Surg 22:481491, 2008
A risk classification scheme By conducting a periodic foot 15
Khan NA, Rahim SA, Anand SS, Simel
has been created in the report of survey in diabetic patients and incor- DL, Panju A: Does the clinical examination
the task force of the Foot Care predict lower extremity peripheral arterial
porating the appropriate basic and disease? JAMA 295:536546, 2006
Interest Group of the ADA13 that is specialized care as warranted, the 16
American Diabetes Association:
reportedly designed to make basic risk of ulceration and its associated Peripheral arterial disease in people with
recommendations regarding the diabetes. Diabetes Care 26:33333341, 2003
morbidities can be reduced.
need for specialist referral and the 17
Armstrong DG, Lavery LA, Vela SA,
Quebedeaux TL, Fleischli JG: Choosing a
frequency of follow-up by primary References practical screening instrument to identify
providers and specialists (Table 3). 1
Wild S, Roglic G, Green A, Sicree R, patients at risk for diabetic foot ulceration.
King H: Global prevalence of diabetes: esti- Arch Intern Med 158:289292, 1998
Patients in the lowest risk category mates for the year 2000 and projections for 18
Frykberg RG, Armstrong DG, Giurini
are recommended to receive educa- 2030. Diabetes Care 27:10471053, 2004 J, Edwards A, Kravette M, Kravitz S, Ross
tion on general foot care and annual 2
Singh N, Armstrong DG, Lipsky BA: C, Stavosky J, Stuck R, Vanore J: Diabetic
follow-up. Increasing risk catego- Preventing foot ulcers in patients with diabe- foot disorders: a clinical practice guideline.
tes. JAMA 293:217228, 2005 J Foot Ankle Surg 39 (5 Suppl.):S1S60, 2000
ries require more components of American Diabetes Association:
3
Reiber GE, Vileikyte L, Boyko EJ, del 19
care and are more likely to benefit Aguila M, Smith DG, Lavery LA, Boulton Consensus development conference on
from specialist care and follow- AJ: Causal pathways for incident lower diabetic foot wound care: 78 April 1999,
extremity ulcers in patients with diabetes Boston, Massachusetts. Diabetes Care
up. A recommended frequency of from two settings. Diabetes Care 22:157162, 22:13541360, 1999
follow-up for each risk category is 1999 20
Wagner FW Jr: The diabetic foot.
also included in the table; follow-
4
Lavery LA, Armstrong DG, Vela SA, Orthopedics 10:163172, 1987
Quebedeaux TL, Fleischli JG: Practical
up increases in frequency with an criteria for screening patients at high risk
21
Frykberg RG: Diabetic foot ulcers:
for diabetic foot ulceration. Arch Intern Med pathogenesis and management. Am Fam Phys
increase in risk category. 66:16551662, 2002
158:157162, 1998
5
Armstrong DG, Lavery LA: Diabetic
22
Oyibo SO, Jude EB, Tarawneh I,
Conclusion Nguyen HC, Harkless LB, Boulton AJ:
foot ulcers: prevention, diagnosis and clas-
Patients with diabetes are at an sification. Am Fam Phys 57:6:13251332, A comparison of two diabetic foot ulcer
13371338, 1998 classification systems: the Wagner and the
increased risk for developing foot University of Texas wound classification
ulcerations. The consequences of 6
Kelkar P: Diabetic neuropathy. Sem systems. Diabetes Care 24:8488, 2001
Neurol 25:168173, 2006
persistent and poorly controlled 23
Armstrong DG, Lavery LA, Nixon BP,
7
Bowering CK: Diabetic foot ulcers: Boulton AJ: Its not what you put on, but
hyperglycemia lead to neuropathic pathophysiology, assessment, and therapy. what you take off: techniques for debriding
and vascular abnormalities that Can Fam Phys 47:10071016, 2001 and off-loading the diabetic foot wound. Clin
cause foot deformities and ulceration. 8
Dyck PJ, Davies JL, Wilson DM, Service Infect Dis 39:S92S99, 2004
FJ, Melton LJ III, Obrien PC: Risk factors
The feet of diabetic patients should for severity of diabetic polyneuropathy.
24
Armstrong DG, Nguyen HC, Lavery
LA, Van Schie CH, Boulton AJ, Harkless LB:
be examined at least annually to Diabetes Care 22:14791486, 1999 Off-loading the diabetic foot wound. Diabetes
determine predisposing conditions to 9
Zochodone DW: Diabetic polyneuropa- Care 24:10191022, 2001
thy: an update. Curr Opin Neurol 21:527533,
ulceration. Treatment plans should be 2008
25
Lipsky BA, Berendt AR, Deery HG,
Embil JM, Joseph WS, Karchmer AW,
based on examination findings and 10
Feldman EL, Russell JW, Sullivan KA, LeFrock JL, Lew DP, Mader JT, Norden C,
the individual risk for ulceration. Golovoy D: New insights into the pathogen- Tan JS: Diagnosis and treatment of diabetic
Clinical Diabetes Volume 27, Number 2, 2009 57
F e a t u r e A r t i c l e
foot infections. Plastic Reconstr Surg 117 222:438448, 1995 38
Barnes RC: Point: hyperbaric oxygen
(7 Suppl.):212S238S, 2006 is beneficial for diabetic foot wounds. Clin
33
Faries PL, Brophy D, LoGerfo FW, Infect Dis 43:188192, 2006
Hilton JR, Williams DT, Beuker B,
26
Akbari CM, Campbell DR, Spence LD,
Miller DR, Harding KG: Wound dress- Hook SC, Pomposelli FB Jr: Combined iliac
39
Berendt AR: Counterpoint: hyperbaric
ings in diabetic foot disease. Clin Infect Dis angioplasty and infrainguinal revasculariza- oxygen for diabetic foot wounds is not effec-
39:S100S103, 2004 tion surgery are effective in diabetic patients tive. Clin Infect Dis 43:193198, 2006
27
Foster AVM, Greenhill MT, Edmonds with multilevel arterial disease. Ann Vasc 40
Sato N, Kashima K, Tanaka Y, Shimizu
ME: Comparing two dressings in the treat- Surg 15:6772, 2001 H, Mori M: Effect of granulocyte-colony
ment of diabetic foot ulcers. J Wound Care stimulating factor on generation of oxygen-
3:224228, 1994
34
Gentzkow GD, Iwasaki SD, Hershon derived free radicals and myeloperoxidase
KS, Mengel M, Prendergast JJ, Ricotta JJ, activity in neutrophils from poorly controlled
28
Lipsky BA: Medical treatment of Steed DP, Lipkin S: Use of Dermagraft, a NIDDM patients. Diabetes 46:133137, 1997
diabetic foot infections. Clin Infect Dis cultured human dermis, to treat foot ulcers.
39:S104S114, 2004
41
Cruciani M, Lipsky BA, Mengoli C, de
Diabetes Care 19:350354, 1996 Lalla F: Are granulocyte-colony stimulating
29
Bridges RM, Deitch EA: Diabetic foot 35
Brem H, Balledux J, Bloom T, Kerstein factors beneficial in treating diabetic foot
infections: pathophysiology and treatment. infections? A meta-analysis. Diabetes Care
MD, Hollier L: Healing of diabetic foot
Surg Clin North Am 74:537555, 1994 28:454460, 2005
ulcers and pressure ulcers with human skin
30
Lipsky BA, Pecoraro RE, Larson SA, equivalent: a new paradigm in wound heal-
Ahroni JH: Outpatient management of ing. Arch Surg 135:627634, 2000
uncomplicated lower-extremity infections in Warren Clayton, Jr., MD, is a clinical
diabetic patients. Arch Intern Med 150:790
36
Steed D: Clinical evaluation of recom-
797, 1990 binant human platelet-derived growth factor fellow, and Tom A. Elasy, MD, MPH,
for the treatment of lower extremity diabetic is medical director of the Vanderbilt
31
Faries PL, Teodorescu VJ, Morrissey ulcers. J Vasc Surg 1:7181, 1995
NJ, Hollier LH, Marin ML: The role of Eskind Diabetes Center in the Division
surgical revascularization in the manage- 37
Faglia E, Favales F, Aldeghi A, Calia
ment of diabetic foot wounds. Am J Surg P, Quarantiello A, Oriani G, Michael M,
of Endocrinology, Diabetes, and
187:34S37S, 2004 Campagnoli P, Morabito A: Adjunctive Metabolism at Vanderbilt University
32
Shah DM, Darling RC III, Chang systemic hyperbaric oxygen therapy in treat- Medical Center in Nashville, Tenn.
BB, Fitzgerald KM, Paty PS, Leather RP: ment of severe prevalently ischemic diabetic
Long-term results of in situ saphenous vein foot ulcer: a randomized study. Diabetes Care Dr. Elasy is editor-in-chief of Clinical
bypass: analysis of 2,058 cases. Ann Surg 19:13391343, 1996 Diabetes.
58 Volume 27, Number 2, 2009 Clinical Diabetes
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- 365 Health Tips - Learn Quick-n-Easy Health Tips For Everyday of The YearДокумент38 страниц365 Health Tips - Learn Quick-n-Easy Health Tips For Everyday of The YearKellieKeeОценок пока нет
- نموذج خطة السلامة والصحة المهنيةДокумент22 страницыنموذج خطة السلامة والصحة المهنيةFadi Abu sfaОценок пока нет
- Emergency First Aid Made Easy Training PresentationДокумент92 страницыEmergency First Aid Made Easy Training PresentationRyan-Jay AbolenciaОценок пока нет
- Stanford University Ulcer StudyДокумент6 страницStanford University Ulcer Studyleeanna29Оценок пока нет
- Lim, 2014, Adapted Cognitive Behavioral Therapy For Religious Individuals With Mental Disorder A Systematic Review PDFДокумент11 страницLim, 2014, Adapted Cognitive Behavioral Therapy For Religious Individuals With Mental Disorder A Systematic Review PDFAnggie AnggriyanaОценок пока нет
- Living With A Chronic Leg UlcerДокумент6 страницLiving With A Chronic Leg UlcerAnggie AnggriyanaОценок пока нет
- Weiner, 2007 PDFДокумент12 страницWeiner, 2007 PDFAnggie AnggriyanaОценок пока нет
- Moyal, 2014, Cognitive Strategies To Regulate Emotions Current Evidence and Future Directions PDFДокумент4 страницыMoyal, 2014, Cognitive Strategies To Regulate Emotions Current Evidence and Future Directions PDFAnggie AnggriyanaОценок пока нет
- Caring For Cancer PatientsДокумент13 страницCaring For Cancer PatientsAnggie AnggriyanaОценок пока нет
- Clin Diabetes 2008 Anderson 22 7Документ6 страницClin Diabetes 2008 Anderson 22 7Anggie AnggriyanaОценок пока нет
- Benson, 2011Документ135 страницBenson, 2011Anggie AnggriyanaОценок пока нет
- Cognitive Defusion vs. Restructuring JCPДокумент15 страницCognitive Defusion vs. Restructuring JCPKalajanОценок пока нет
- Nurse Care PlanДокумент1 страницаNurse Care PlanAnggie AnggriyanaОценок пока нет
- Living With A Chronic Leg UlcerДокумент6 страницLiving With A Chronic Leg UlcerAnggie AnggriyanaОценок пока нет
- Yazdanpanah, 2015Документ18 страницYazdanpanah, 2015Anggie AnggriyanaОценок пока нет
- Management of Clients With Immunology ProblemsДокумент12 страницManagement of Clients With Immunology ProblemsAnggie AnggriyanaОценок пока нет
- Role of Self-Care in Management of DiabetesДокумент5 страницRole of Self-Care in Management of DiabetesAnggie AnggriyanaОценок пока нет
- Diabetes Self Managment Education Barrier Study SeptemberДокумент39 страницDiabetes Self Managment Education Barrier Study SeptemberAnggie AnggriyanaОценок пока нет
- Al KhawaldehДокумент8 страницAl KhawaldehAnggie AnggriyanaОценок пока нет
- Clin Diabetes 2008 Anderson 22 7Документ6 страницClin Diabetes 2008 Anderson 22 7Anggie AnggriyanaОценок пока нет
- Original Article: Nancy J. Wei, MD, MMSC David M. Nathan, MD Deborah J. Wexler, MD, MSCДокумент8 страницOriginal Article: Nancy J. Wei, MD, MMSC David M. Nathan, MD Deborah J. Wexler, MD, MSCAnggie AnggriyanaОценок пока нет
- Pemphigus VulgarisДокумент12 страницPemphigus Vulgarisamirz_4Оценок пока нет
- Derma 1Документ6 страницDerma 1Anggie AnggriyanaОценок пока нет
- Development and Validation of A Diabetes Foot.5Документ7 страницDevelopment and Validation of A Diabetes Foot.5Anggie AnggriyanaОценок пока нет
- Understanding The Immune System How It WorksДокумент63 страницыUnderstanding The Immune System How It WorksbinthunderОценок пока нет
- Derma 5Документ6 страницDerma 5Anggie AnggriyanaОценок пока нет
- Analisis Morfometri Dan Morfostruktur Lereng KejadianДокумент13 страницAnalisis Morfometri Dan Morfostruktur Lereng KejadianMuhammad Arya Azari100% (1)
- 1 Writing An Effective TitleДокумент10 страниц1 Writing An Effective TitleAnggie Anggriyana100% (1)
- 14 Rev. Enf. Ref. Riv16011 EnglДокумент12 страниц14 Rev. Enf. Ref. Riv16011 EnglAnggie AnggriyanaОценок пока нет
- Constipation Risk Assessment ToolДокумент2 страницыConstipation Risk Assessment ToolAnggie Anggriyana100% (1)
- Pathophysiology AnemiaДокумент34 страницыPathophysiology AnemiaAnggie AnggriyanaОценок пока нет
- Megaloblastic Anemia PanelДокумент5 страницMegaloblastic Anemia PanelAnggie AnggriyanaОценок пока нет
- Nursing Management For Patients With Hematology Problems PDFДокумент44 страницыNursing Management For Patients With Hematology Problems PDFAnggie AnggriyanaОценок пока нет
- NCM 103 Chapter 36 Skin Integrity and Wound Care (Canvas)Документ121 страницаNCM 103 Chapter 36 Skin Integrity and Wound Care (Canvas)AinaB ManaloОценок пока нет
- Drug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeДокумент6 страницDrug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeJaymark LambinoОценок пока нет
- Curriculum Vitae: The European Journal of Orthopaedic Surgery and Traumatology (Springer)Документ56 страницCurriculum Vitae: The European Journal of Orthopaedic Surgery and Traumatology (Springer)Always At workОценок пока нет
- ANSWERS MRS lAJOWSKIДокумент20 страницANSWERS MRS lAJOWSKISamia FarooqОценок пока нет
- Musculoskeletal Care ModalitiesДокумент45 страницMusculoskeletal Care ModalitiesAia JavierОценок пока нет
- Repair Vaginal & Perineal TearsДокумент4 страницыRepair Vaginal & Perineal TearsFrancez Anne GuanzonОценок пока нет
- Rnbe-16-0312-Nae High Output Sell SheetДокумент2 страницыRnbe-16-0312-Nae High Output Sell SheetYacine Tarik AizelОценок пока нет
- Revolutionizing Non-Conventional Wound Healing Using Honey by Simultaneously Targeting Multiple Molecular Mechanisms PDFДокумент10 страницRevolutionizing Non-Conventional Wound Healing Using Honey by Simultaneously Targeting Multiple Molecular Mechanisms PDFAbdoОценок пока нет
- Basic fire extinguishing methodsДокумент176 страницBasic fire extinguishing methodsozveoz100% (1)
- First AideДокумент38 страницFirst AideJella BandalanОценок пока нет
- 4 Amputation Nursing Care Plans - Nurseslabs-1 PDFДокумент12 страниц4 Amputation Nursing Care Plans - Nurseslabs-1 PDFsaidi MwanamongaОценок пока нет
- General Principles of Fracture ManagementДокумент60 страницGeneral Principles of Fracture ManagementAdrian Joel Quispe AlataОценок пока нет
- Hand SafetyДокумент42 страницыHand SafetyjelowpyОценок пока нет
- Pretibial LacsДокумент8 страницPretibial LacsMiguel JohnsonОценок пока нет
- Giatric NurseДокумент5 страницGiatric NurseKim TanОценок пока нет
- Owbn Infernalism: Guide To Dark Thaumaturgy: A Sourcebook For One World by NightДокумент35 страницOwbn Infernalism: Guide To Dark Thaumaturgy: A Sourcebook For One World by NightJuhász ZoltánОценок пока нет
- Nursing Care Plan SummaryДокумент15 страницNursing Care Plan SummaryJemina Rafanan RacadioОценок пока нет
- AFMM2023 - 5 - Antibacterial Electrospun Nanofibrous Materials For Wound HealingДокумент23 страницыAFMM2023 - 5 - Antibacterial Electrospun Nanofibrous Materials For Wound Healingmaolei0101Оценок пока нет
- KIT Volume XXI No 1 April 2009 PropДокумент16 страницKIT Volume XXI No 1 April 2009 PropKITexBruderhofCCIОценок пока нет
- Ultima Forsan - A Taste of Macabre SWДокумент31 страницаUltima Forsan - A Taste of Macabre SWMaya Karasova100% (1)
- Wallace State Community College NURSING DATABASE: Nursing HomeДокумент9 страницWallace State Community College NURSING DATABASE: Nursing HomeEnger NushunОценок пока нет
- Is 3786 1983 PDFДокумент33 страницыIs 3786 1983 PDFsinegapriya100% (1)
- Module 11 Muscular Skeleton SystemДокумент20 страницModule 11 Muscular Skeleton SystemeroolifyОценок пока нет
- Anemia Effect On Burn Wound HealingДокумент5 страницAnemia Effect On Burn Wound HealingAgung Widya PramanaОценок пока нет
- Wound InfectionДокумент21 страницаWound Infectionmaak85Оценок пока нет
- Basic Principles of Wound MGMT - Poengki DP-ilovepdf-compressedДокумент38 страницBasic Principles of Wound MGMT - Poengki DP-ilovepdf-compressednugrahaОценок пока нет