Академический Документы
Профессиональный Документы
Культура Документы
GTG 36 PDF
Загружено:
Aloah122346Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
GTG 36 PDF
Загружено:
Aloah122346Авторское право:
Доступные форматы
The Prevention of Early-onset
Neonatal Group B
Streptococcal Disease
Greentop Guideline No. 36
2nd edition I July 2012
The Prevention of Early-onset Neonatal Group B
Streptococcal Disease
This is the second edition of this guideline. The first edition was published in 2003 under the same title.
1. Purpose and scope
The purpose of this guideline is to provide guidance for obstetricians, midwives and neonatologists on the
prevention of early-onset neonatal group B streptococcal (EOGBS) disease. Prevention of late-onset GBS and
treatment of established GBS disease is not considered beyond initial antibiotic therapy.
2. Background
Group B streptococcus (Streptococcus agalactiae) is recognised as the most frequent cause of severe early-
onset (at less than 7 days of age) infection in newborn infants. However, there is still controversy about its
prevention. Surveys in 2001 and 2008 demonstrated that less than 1% of UK maternity units were performing
systematic screening for GBS1,2 and, to date, UK clinicians have not generally adopted the US and Canadian
practice of routine screening for GBS carriage.3,4 Extrapolation of practice from the USA to the UK may,
however, be inappropriate.The incidence of EOGBS disease in the UK in the absence of systematic screening
or widespread intrapartum antibiotic prophylaxis (IAP) is 0.5/1000 births,5 which is similar to that seen in the
USA after universal screening and IAP, despite comparable vaginal carriage rates.6 The incidence of culture-
confirmed early-onset disease in the USA has fallen in association with the introduction of screening pregnant
women for GBS.3 The current US guidelines7 advise that all women colonised with GBS at 3537 weeks of
gestation (or labouring before this time) should be offered IAP, usually in the form of high-dose intravenous
benzylpenicillin or ampicillin. IAP has been shown to significantly reduce the risk of culture-positive early-
onset but not late-onset disease (occurring 7 or more days after birth). There is also indirect evidence of an
impact on neonatal deaths. A review of sepsis-related neonatal mortality in the USA showed a decline in
mortality in the first week after birth, coinciding with the introduction of IAP.8 However, a Cochrane review
concluded that, while IAP for colonised mothers reduced the incidence of EOGBS disease, it has not been
shown to reduce all causes of mortality or GBS-related mortality.9 There have been no studies addressing
whether routine screening has had any impact on all-cause mortality. Antenatal screening and treatment may
carry disadvantages for the mother and baby. These include anaphylaxis,10 increased medicalisation of labour
and the neonatal period, and possible infection with antibiotic-resistant organisms, particularly when broad-
spectrum antibiotics such as amoxicillin are used for prophylaxis.11,12 The UK National Screening Committee
examined the issue of strategies for the prevention of EOGBS disease in November 2008 and recommended
that routine screening using bacteriological culture or near-patient testing techniques should not be
introduced into UK practice.13
3. Identification and assessment of evidence
This RCOG guideline was developed in accordance with standard methodology for producing RCOG Green-
top Guidelines.1416 The Cochrane Database of Systematic Reviews, DARE, EMBASE, Medline and PubMed
(electronic databases) were searched for relevant randomised controlled trials, systematic reviews and meta-
analyses. The search was restricted to articles published between 2003 and August 2011. Search terms
included: group B streptococcus, Streptococcus agalactiae, group B streptococcus and pregnancy, beta
haemolytic streptococcus and pregnancy, and beta haemolytic streptococcus and neonatal, beta hemolytic
streptococcus and neonatal, GBS bacteriuria, and was limited to humans and the English language. The
National Library for Health and the National Guidelines Clearing House were also searched for relevant
guidelines and reviews. Studies relevant to the scope of the guideline were selected by the members of the
guideline development group. Where possible, recommendations are based on available evidence. Areas
lacking evidence are highlighted and annotated as good practice points.
RCOG Green-top Guideline No. 36 2 of 13 Royal College of Obstetricians and Gynaecologists
4. Antenatal screening
4.1 Should all pregnant women be offered bacteriological screening for GBS?
Routine bacteriological screening of all pregnant women for antenatal GBS carriage is not recommended.
D
Until it is clear that antenatal screening for GBS carriage does more good than harm and that the
benefits are cost-effective, the National Screening Committee does not recommend routine
Evidence
screening in the UK.13 Initiating national swab-based screening for antenatal GBS carriage would level 4
have a substantial impact on the provision of antenatal care within the UK. Major organisational
changes and new funding would be required to ensure an equitable and quality-assured service.
4.2 If GBS is detected incidentally earlier in the pregnancy, should women be treated before the onset of labour?
Antenatal treatment with benzylpenicillin is not recommended.
C
Antenatal prophylaxis with oral benzylpenicillin for vaginal/rectal colonisation does not reduce the
Evidence
likelihood of GBS colonisation at the time of delivery17 and so is not indicated in this situation. IAP level 2+
should be offered to GBS-colonised women (see section 5.2).
4.3 Should women be screened for GBS or receive IAP if GBS was detected in a previous pregnancy?
Current evidence does not support screening for GBS or the administration of IAP to women in whom
GBS carriage was detected in a previous pregnancy.
D
If GBS was detected in a previous pregnancy, the likelihood of carriage in a subsequent pregnancy
is around 38%.18 This gives a risk estimate of neonatal EOGBS disease of approximately 0.9
cases/1000 births versus a background risk of 0.5 cases/1000 births or 2.3 cases/1000 births in Evidence
women with GBS detected in the current pregnancy. The time interval between the two level 3
pregnancies and the intensity of colonisation in the previous pregnancy are predictive of recurrent
GBS colonisation.18
5. Reducing the risk of neonatal GBS disease in women known to be colonised with GBS.
5.1 How should GBS bacteriuria in the current pregnancy be managed?
Clinicians should offer IAP to women with GBS bacteriuria identified during the current pregnancy.
C
GBS bacteriuria is associated with a higher risk of chorioamnionitis19 and neonatal disease.20 It is
not possible to accurately quantify these increased risks. These women should be offered IAP. Evidence
Women with GBS urinary tract infection (growth of greater than 105 cfu/ml) during pregnancy level 3
should receive appropriate treatment at the time of diagnosis as well as IAP.
5.2 Should women receive IAP if GBS is detected in the current pregnancy?
IAP should be offered if GBS is detected on a vaginal swab in the current pregnancy.
C
Vaginal swabs should not be taken during pregnancy unless there is a clinical indication to do so.
P
If GBS is present in a vaginal swab, it is likely that the risk of neonatal disease is increased. A risk of
Evidence
disease of 2.3/1000 may be assumed (overall UK incidence 0.5/1000; approximately 21% women level 3
are carriers).21
RCOG Green-top Guideline No. 36 3 of 13 Royal College of Obstetricians and Gynaecologists
5.3 How should women with known GBS colonisation undergoing planned caesarean section be managed?
Antibiotic prophylaxis specific for GBS is not required for women undergoing planned caesarean section
in the absence of labour and with intact membranes.
C
All women having caesarean section should receive antibiotic prophylaxis according to NICE guideline no. 132.22
Women undergoing planned caesarean delivery in the absence of labour or membrane rupture
Evidence
do not require antibiotic prophylaxis for GBS, regardless of GBS colonisation status. The risk of level 3
neonatal EOGBS disease is extremely low in this circumstance.23
5.4 How should women known to be colonised with GBS who experience spontaneous rupture of membranes
at term be managed?
Immediate induction of labour and IAP should be offered to all women with prelabour rupture of
membranes at 37+0 weeks of gestation or more.
D
The NICE guideline on induction of labour 24 recommends that all women with prelabour rupture of
membranes at term (37 weeks + 0 days of gestation or greater) should be offered immediate induction Evidence
of labour, or induction after 24 hours. If GBS colonisation was identified earlier in the pregnancy (by level 3
a swab taken for other reasons), immediate induction of labour and IAP should be offered.
5.5 How should women with GBS colonisation and suspected chorioamnionitis be managed?
If chorioamnionitis is suspected, broad-spectrum antibiotic therapy including an agent active against
GBS should replace GBS-specific IAP and induction of labour should be considered.
A
Chorioamnionitis is known to be associated with maternal and neonatal morbidity including
Evidence
sepsis,neonatal lung and brain injury and cerebral palsy.The risk of these complications is reduced level 1+
by broad-spectrum antibiotic therapy.25
6. Management of labour (including rupture of membranes) to reduce the risk of neonatal
GBS disease in women without known GBS colonisation
6.1 Should women presenting in preterm labour with intact membranes be offered IAP?
Women presenting in established preterm labour with intact membranes with no other risk factors for
GBS should not routinely be offered IAP unless they are known to be colonised with GBS.
C
Although the risk of EOGBS infection is higher in preterm than in term infants (see Appendix I), there are
reasons to be cautious about widespread prescription of antibiotics for these women. Approximately 50% of
all women thought to be in preterm labour will not deliver preterm. Women presenting in uncomplicated
spontaneous preterm labour with intact membranes are the same group of women as those recruited to the
ORACLE trial, where there was evidence of harm in terms of adverse neurodevelopmental outcome including
cerebral palsy in their infants at 7 years of age in the absence of any demonstrable benefit in the short term.26
Although the antibiotics used in ORACLE are different from those used for IAP for GBS, there is no evidence
from long-term follow-up studies that other antibiotics, including penicillin, are safe. As the risk of EOGBS
infection in this group of infants is still low, prompt management of early-onset sepsis, if it occurs, is preferable
to IAP for large numbers of women.
There is currently no evidence to show that the subgroup of women in preterm labour with ruptured
membranes have greater benefit from IAP. The difficulty in balancing risks and benefits of IAP for women in
preterm labour could be resolved by a randomised controlled trial.
RCOG Green-top Guideline No. 36 4 of 13 Royal College of Obstetricians and Gynaecologists
6.2 How should women with clinical risk factors such as a pyrexia (>38C) in labour be managed?
IAP should be offered to women who are pyrexial in labour (>38C).
C
Women who are pyrexial in labour should be offered broad-spectrum antibiotics including an antibiotic
for prevention of neonatal EOGBS disease. P
Intrapartum pyrexia (>38C) is associated with a risk of EOGBS disease of 5.3/1000 (versus a
Evidence
background risk of 0.5/1000).5,27 In view of this increased risk, IAP should be offered in the level 3
presence of maternal pyrexia.
6.3 How should women with term prelabour rupture of membranes be managed?
The evidence for IAP for women with term prelabour rupture of membranes is unclear and NICE
recommends that it is not given, unless there are other risk factors.
C
Women with prelabour rupture of membranes at term should be offered immediate induction of labour or
induction after 24 hours (in line with the NICE guideline on induction of labour24).
6.4 How should women with preterm prelabour rupture of membranes be managed to reduce the risk of
neonatal GBS disease?
Antibiotic prophylaxis for GBS is unnecessary for women with preterm rupture of membranes.
C
Women who experience preterm rupture of membranes should be managed according to the
RCOG Green-top Guideline Preterm Prelabour Rupture of Membranes.28 Antibiotic administration
Evidence
specifically for GBS colonisation is not necessary prior to labour and should not be given just in level 3
case.18,29 If these women are known to be colonised with GBS, IAP should be offered. Induction of
labour should be considered if there is suspicion of chorioamnionitis.
6.5 Should women with a previous baby with neonatal GBS disease be offered IAP?
IAP should be offered to women with a previous baby with neonatal GBS disease.
D
Subsequent infants born to these women are likely to be at increased risk of GBS disease, although
this has not been accurately quantified. The probable increase in risk may be attributable to Evidence
persistence of low levels of maternal anti-GBS antibodies.30 Vaginal or rectal swabs are not helpful, level 3
as IAP would be recommended even if these swabs were negative for GBS.
7. Which antibiotics should be given to prevent early-onset neonatal GBS disease?
For women who have accepted IAP, benzylpenicillin should be administered as soon as possible after
the onset of labour and given regularly until delivery.
B
Clindamycin should be administered to those women allergic to benzylpenicillin.
D
It is recommended that 3 g intravenous benzylpenicillin be given as soon as possible after the onset
of labour and 1.5 g 4-hourly until delivery. Clindamycin 900 mg should be given intravenously
8-hourly to those allergic to benzylpenicillin. Current clindamycin resistance rates in England and
Wales stand at 10%;31 thus, there is a chance that clindamycin might be less effective. An alternative Evidence
agent in this situation is vancomycin. It should be noted that dosage regimens are based on tradition level 3
rather than evidence and the British National Formulary should be consulted for specific dose
recommendations. Broad-spectrum antibiotics such as ampicillin should be avoided if possible, as
concerns have been raised regarding increased rates of Gram-negative neonatal sepsis.11 To optimise
RCOG Green-top Guideline No. 36 5 of 13 Royal College of Obstetricians and Gynaecologists
the efficacy of IAP, the first dose should be given at least 2 hours prior to delivery.32,33 There is
evidence that benzylpenicillin levels in cord blood exceed the minimum inhibitory concentration
Evidence
for GBS as early as 1 hour after maternal administration,34 but it is not known how this relates to level 3
neonatal colonisation or disease. Oral antibiotics for IAP are not recommended because of variable
absorption in labour.
8. Should vaginal cleansing be performed in labour?
There is no evidence that intrapartum vaginal cleansing will reduce the risk of neonatal GBS disease.
C
Although vaginal cleansing with chlorhexidine has been shown to reduce the risk of neonatal GBS Evidence
colonisation,35 a recent large randomised controlled trial showed no impact on EOGBS disease.36 level 3
9. How should the newborn infant be managed?
The evidence base upon which to make treatment decisions for newborn infants is weak. Few randomised
controlled trials have been performed.3739 Previous guidelines have largely been based on consensus rather
than evidence. Published data permit risk estimates to be made which can be used to inform decision making
regarding the need for enhanced observation or investigation and initial treatment.There is no good evidence
to support routine blood tests to aid decision making about the management of these infants.40
The continuing management of infants with established disease is not within the scope of this guideline.
In a UK study of invasive GBS disease, 89% of early-onset cases were identified on day 1.41 Of those developing
clinical features on day 1, 97.6% were noted by 12 hours of age (where hour of onset was given).41 More recent
UK data from an infection surveillance network showed that 94% of early-onset cases occurred on day 1.42 Most
cases (6567%) have one or more risk factors prior to or during labour.41,42 A significant number will also have
had signs of fetal distress, an emergency delivery and low Apgar scores.The majority of early-onset cases in these
studies presented with sepsis (79.4%), 11.8% had meningitis, 7.8% had pneumonia and 1% focal infection.41
9.1 How should well infants at risk of EOGBS disease be monitored?
Well infants at risk of EOGBS should be observed for the first 1224 hours after birth with regular
assessments of general wellbeing, feeding, heart rate, respiratory rate and temperature. P
The great majority of infants (8994%) who develop EOGBS infection develop signs within the first 24 hours
after birth and the majority of such infants (6567%) will have had one or more conventional risk factors
evident in or before labour. A significant number will also have had signs of fetal distress, an emergency
delivery and low Apgar scores. Clearly, any baby with clinical signs and symptoms compatible with sepsis
should be evaluated and commenced on antibiotics. Other infants without clinical signs but with other risk
factors should be observed closely for such signs over the first 24 hours after birth.
9.2 Should postnatal antibiotic prophylaxis be given to low-risk term infants?
Postnatal antibiotic prophylaxis is not recommended for asymptomatic term infants without known
antenatal risk factors.
C
The incidence of EOGBS disease in asymptomatic term infants without known antenatal risk factors in the
UK is estimated at 0.2 cases/1000 births.5 No randomised controlled trial has investigated treatment in this
group. If postnatal antibiotic treatment were completely effective and there were no adverse effects, 5000
infants would need to be treated to prevent a single case and at least 80 000 infants would have to be treated
to prevent a single death from EOGBS disease.
RCOG Green-top Guideline No. 36 6 of 13 Royal College of Obstetricians and Gynaecologists
Evidence
Routine postnatal antibiotic prophylaxis is not recommended. level 3
9.3 How should the well infant with one or more risk factors be treated?
Randomised controlled trials have not provided a sufficient evidence base for clear treatment
recommendations in well newborn infants.
C
Estimates of the risk of EOGBS disease in the presence of individual antenatal risk factors, before and after IAP,
are shown in Appendix I.
Some clinicians will recommend intravenous antibiotic treatment of well infants with risk factors (and stop
therapy when cultures are negative or after a defined period if IAP was given), while others will prefer to
observe infants because the balance of risks and benefits of treatment is uncertain. Around 90% of cases
present clinically before 24 hours of age,41,42 so the risk of disease in infants who remain well without
treatment beyond this time may not be substantially elevated above that of the infant with no risk factors.
Prolonged observation of well infants is therefore not indicated. The argument for using prophylactic
treatment in well infants is stronger in the presence of multiple maternal risk factors but is still unproven.
However, in well infants whose mothers had risk factors and received appropriate IAP, the risk of EOGBS is
significantly lower and these infants can be observed for 24 hours without treatment.
9.4 How should the neonate with clinical signs of EOGBS disease be managed?
Infants with clinical signs of EOGBS should be treated promptly with appropriate antibiotics.
C
Many infants with EOGBS disease have signs at or soon after birth.41 Neonatal sepsis may present
with subtle signs initially but can progress rapidly to death. Whether they received intrapartum
antibiotics or not, any newborn infant with clinical signs compatible with infection should be
investigated and treated promptly with antibiotics which are narrow spectrum but provide cover
Evidence
against GBS and other common pathogens such as Escherichia coli 43 (for example, benzylpenicillin level 3
and gentamicin). Blood cultures should always be obtained before antibiotic treatment is
commenced, and cerebrospinal fluid cultures should be considered unless the clinical condition
precludes a lumbar puncture. A lumbar puncture should be obtained at the earliest opportunity
once the clinical condition has stabilised.
9.5 How should the infant of a mother with a previous infant with GBS disease be managed?
For a well infant whose mother has had a previous infant with GBS disease, either clinical evaluation
after birth and observation for around 24 hours are necessary, or blood cultures need to be obtained and
C
the infant treated with benzylpenicillin until the culture results are available. It is unclear whether
further action is necessary for the well infant.
The risk of GBS disease is unquantified but is probably significantly increased.27 The infant should
be evaluated clinically soon after birth and observed for at least 24 hours. It is unclear whether
Evidence
further action is necessary, but an alternative approach would be to obtain blood cultures and treat level 3
with benzylpenicillin until the culture results are available.There is insufficient evidence to suggest
that neonatal treatment should be given if IAP has been administered.
9.6 Are routine neonatal surveillance cultures of value?
It is not necessary to perform routine surface cultures or blood cultures on well infants.
P
Most infants who develop EOGBS disease present with illness soon after birth and 90% have
Evidence
presented clinically by 24 hours of age, before culture results become available.41,43 Postnatal level 3
antibiotic treatment has not been shown to eradicate carriage of GBS or to influence the risk of
RCOG Green-top Guideline No. 36 7 of 13 Royal College of Obstetricians and Gynaecologists
late-onset GBS disease. It is therefore unnecessary to perform routine surface cultures or blood Evidence
cultures on well infants, whether they received IAP or not. level 3
9.7 Is there any need for breastfeeding to be avoided?
There is no evidence to discourage breastfeeding where there are concerns regarding the possible risk of
transmission of GBS disease.
10. Suggested audit topics
Percentage of eligible women with various risk factors receiving IAP.
Percentage of women receiving IAP for at least 2 hours prior to delivery.
Percentage of women with pyrexia receiving broad-spectrum antibiotics.
Percentage of infants with risk factors being observed for 1224 hours.
Percentage of infants with signs of possible GBS disease receiving appropriate investigation and treatment.
References
1. Kenyon S, Brocklehurst P, Blackburn A,Taylor DJ. Antenatal 13. UK National Screening Committee. Group B Streptococcus:The
screening and intrapartum management of Group B UK NSC policy on Group B Streptococcus screening in
Streptococcus in the UK. BJOG 2004;111:22630. pregnancy. London: NSC; 2008
2. Royal College of Obstetricians and Gynaecologists and London [http://www.screening.nhs.uk/groupbstreptococcus].
School of Hygiene and Tropical Medicine. The Prevention of 14. Royal College of Obstetricians and Gynaecologists.
Early-onset Neonatal Group B Streptococcal Disease in UK Development of RCOG Green-top Guidelines: Policies and
Obstetric Units. An audit of reported practice in England, Processes. Clinical Governance Advice No. 1a. London: RCOG;
Scotland, Wales and Northern Ireland. London: RCOG Press; 2006 [http://www.rcog.org.uk/green-top-development].
2007 [http://www.rcog.org.uk/our-profession/good-practice/ 15. Royal College of Obstetricians and Gynaecologists.
audit/prevention-neonatal-group-b-streptoccocal-disease-audit]. Development of RCOG Green-top Guidelines: Producing a
3. Prevention of perinatal group B streptococcal disease: a public Scope. Clinical Governance Advice No. 1b. London: RCOG; 2006
health perspective. Centers for Disease Control and Prevention. [http://www.rcog.org.uk/womens-health/clinical-
MMWR 1996;45:124. guidance/development-rcog-green-top-guidelines-producing-
4. Shah V, Ohlsson A; Canadian Task Force on Preventive Health scope].
Care. Prevention of Early-onset Group B Streptococcal (GBS) 16. Royal College of Obstetricians and Gynaecologists.
Infection in the Newborn: Systematic Review and Development of RCOG Green-top Guidelines: Producing a
Recommendations. CTFPHC Technical Report #016. London, Clinical Practice Guideline. Clinical Governance Advice No. 1c.
ON, Canada: Canadian Task Force; 2001. London: RCOG; 2006 [http://www.rcog.org.uk/womens-
5. Heath PT, Balfour G, Weisner AM, Efstratiou A, Lamagni TL,Tighe health/clinical-guidance/development-rcog-green-top-guidelines-
H, et al.; PHLS Group B Streptococcus Working Group. Group B producing-clinical-practice-gu].
streptococcal disease in UK and Irish infants younger than 90 17. Gardner SE,Yow MD, Leeds LJ,Thompson PK, Mason EO Jr,
days. Lancet 2004;363:2924. Clark DJ. Failure of penicillin to eradicate group B streptococcal
6. Easmon CS.The carrier state: group B streptococcus. J colonization in the pregnant woman. A couple study. Am J
Antimicrob Chemother 1986;18 Suppl A:5965. Obstet Gynecol 1979;135:10625.
7. Verani JR, McGee L, Schrag SJ; Division of Bacterial Diseases, 18. Cheng PJ, Chueh HY, Liu CM, Hsu JJ, Hsieh TT, Soong YK. Risk
National Center for Immunization and Respiratory Diseases, factors for recurrence of group B streptococcus colonization in
Centers for Disease Control and Prevention (CDC). Prevention a subsequent pregnancy. Obstet Gynecol 2008;111:7049.
of perinatal group B streptococcal disease revised guidelines 19. Anderson BL, Simhan HN, Simons KM, Wiesenfeld HC. Untreated
from CDC, 2010. MMWR 2010;59:136. asymptomatic group B streptococcal bacteriuria early in
8. Lukacs SL, Schoendorf KC, Schuchat A.Trends in sepsis-related pregnancy and chorioamnionitis at delivery. Am J Obstet
neonatal mortality in the United States, 19851998. Pediatr Gynecol 2007;196:524.e15.
Infect Dis J 2004;23:599603. 20. Wood EG, Dillon HC Jr. A prospective study of group B
9. Ohlsson A, Shah VS. Intrapartum antibiotics for known maternal streptococcal bacteriuria in pregnancy. Am J Obstet Gynecol
group B streptococcal colonization. Cochrane Database Syst 1981;140:51520.
Rev 2009;(3):CD007467. 21. Colbourn T, Gilbert R. An overview of the natural history of
10. Chaudhuri K, Gonzales J, Jesurun CA, Ambat MT, Mandal- early onset group B streptococcal disease in the UK. Early Hum
Chaudhuri S. Anaphylactic shock in pregnancy: a case study and Dev 2007;83:14956.
review of the literature. Int J Obstet Anesth 2008;17:3507. 22. National Institute for Health and Clinical Excellence. Caesarean
11. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz section. NICE Clinical Guideline No. 132. London: NICE; 2011.
RA, et al. Changes in pathogens causing early-onset sepsis in 23. Ramus RM, McIntire DD, Wendel Jr GD. Antibiotic
very-low-birth-weight infants. N Engl J Med 2002;347:2407. chemoprophylaxis for group B strep is not necessary with
12. Moore MR, Schrag SJ, Schuchat A. Effects of intrapartum elective cesarean section at term. Am J Obstet Gynecol
antimicrobial prophylaxis for prevention of group-B- 1999;180:S85.
streptococcal disease on the incidence and ecology of early- 24. National Institute for Health and Clinical Excellence. Induction
onset neonatal sepsis. Lancet Infect Dis 2003;3:20113. of labour. NICE Clinical Guideline No. 70. London: NICE; 2008.
RCOG Green-top Guideline No. 36 8 of 13 Royal College of Obstetricians and Gynaecologists
25. Tita AT, Andrews WW. Diagnosis and management of clinical 37. Siegel JD, McCracken GH,Threlkeld N, DePasse BM, Rosenfield
chorioamnionitis. Clin Perinatol 2010;37:33954. CR. Single-dose penicillin prophylaxis of neonatal group-B
26. Kenyon S, Pike K, Jones DR, Brocklehurst P, Marlow N, Salt A, et streptococcal disease. Lancet 1982;1:142630.
al. Childhood outcomes after prescription of antibiotics to 38. Pyati SP, Pildes RS, Jacobs NM, Ramamurthy RS,Yeh TF, Raval DS,
pregnant women with spontaneous preterm labour: 7-year et al. Penicillin in infants weighing two kilograms or less with
follow-up of the ORACLE II trial. Lancet 2008;372:131927. early-onset group B streptococcal disease. N Engl J Med
27. Oddie S, Embleton ND. Risk factors for early onset neonatal 1983;308:13839.
group B streptococcal sepsis: casecontrol study. BMJ 39. Patel DM, Rhodes PG, LeBlanc MH, Graves GR, Glick C, Morrison
2002;325:308. J. Role of postnatal penicillin prophylaxis in prevention of
28. Royal College of Obstetricians and Gynaecologsts. Preterm neonatal group B streptococcus infection. Acta Paediatr
prelabour rupture of membranes. Green-top Guideline No. 44. 1999;88:8749.
London: RCOG; 2006 [http://www.rcog.org.uk/womens- 40. Buckler B, Bell J, Sams R, Cagle W, Bell SA, Allen C, et al.
health/clinical-guidance/preterm-prelabour-rupture-membranes- Unnecessary workup of asymptomatic neonates in the era of
green-top-44]. group B streptococcus prophylaxis. Infect Dis Obstet Gynecol
29. Alvarez JR, Williams SF, Ganesh VL, Apuzzio JJ. Duration of 2010. Epub 2010 Aug 22.
antimicrobial prophylaxis for group B streptococcus in patients 41. Heath PT, Balfour GF,Tighe H, Verlander NQ, Lamagni TL,
with preterm premature rupture of membranes who are not in Efstratiou A; HPA GBS Working Group. Group B streptococcal
labor. Am J Obstet Gynecol 2007;197:390.e14. disease in infants: a case control study. Arch Dis Child
30. Carstensen H, Christensen KK, Grennert L, Persson K, Polberger 2009;94:67480.
S. Early-onset neonatal group B streptococcal septicaemia in 42. Vergnano S, Embleton N, Collinson A, Menson E, Russell AB,
siblings. J Infect 1988;17:2014. Heath P. Missed opportunities for preventing group B
31. Health Protection Agency. Health Protection Report. 2009;3(46) streptococcus infections. Arch Dis Child Fetal Neonatal Ed
[http://www.hpa.org.uk/hpr/archives/2009/hpr4609.pdf]. 2010;95:F723.
32. Lin FY, Brenner RA, Johnson YR, Azimi PH, Philips JB 3rd, Regan 43. Vergnano S, Menson E, Kennea N, Embleton N, Russell AB, Watts
JA, et al.The effectiveness of risk-based intrapartum T, et al. Neonatal infections in England: the NeonIN surveillance
chemoprophylaxis for the prevention of early-onset neonatal network. Arch Dis Child Fetal Neonatal Ed 2011;96:F9F14.
group B streptococcal disease. Am J Obstet Gynecol 44. Office for National Statistics, Northern Ireland Statistics and
2001;184:120410. Research Agency, General Registry Office for Scotland websites.
33. de Cueto M, Sanchez MJ, Sampedro A, Miranda JA, Herruzo AJ, Prevalence of risk factors in pregnancy
Rosa-Fraile M.Timing of intrapartum ampicillin and prevention [http://www.ons.gov.uk/ons/rel/ukhs/united-kingdom-health-
of vertical transmission of group B streptococcus. Obstet statistics/2010/chapter-2-tables.xls, Accessed 29 March 2010.
Gynecol 1998;91:1124. 45. Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et
34. Barber EL, Zhao G, Buhimschi IA, Illuzzi JL. Duration of al. Prenatal screening and treatment strategies to prevent group
intrapartum prophylaxis and concentration of penicillin G in B streptococcal and other bacterial infections in early infancy:
fetal serum at delivery. Obstet Gynecol 2008;112:26570. cost-effectiveness and expected value of information analyses.
Health Technol Assess 2007;11:1226, iii.
35. Stade BC, Shah V, Ohlsson A. Vaginal chlorhexidine during labour
to prevent early-onset neonatal group B streptococcal infection. 46. Hospital Episode Statistics. Maternity data 200809
Cochrane Database Syst Rev 2004;(3):CD003520. [http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteI
D=1937&categoryID=1009].
36. Cutland CL, Madhi SA, Zell ER, Kuwanda L, Laque M, Groome M,
et al. ; PoPS Trial Team. Chlorhexidine maternal-vaginal and
neonate body wipes in sepsis and vertical transmission of
pathogenic bacteria in South Africa: a randomised, controlled
trial. Lancet 2009;374:190916.
RCOG Green-top Guideline No. 36 9 of 13 Royal College of Obstetricians and Gynaecologists
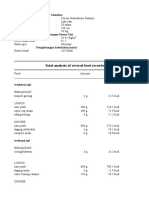
APPENDIX I
Estimates of the risk of EOGBS disease in the presence of individual antenatal risk factors, with
and without IAP.
These estimates are based on an incidence of EOGBS disease in the UK of 0.5/1000,5 which is likely to be the
minimum incidence.
Risk factor Risk of EOGBS Risk of EOGBS Risk of death from Risk of death from
disease if IAP disease if full EOGBS disease if EOGBS disease if
not given IAP given IAP not given full IAP given
Intrapartum fever (>38C) 1:189 1:943 1:1783 1:8915
Prolonged rupture of 1:556 1:2777 1:9754 1:48 772
membranes (>18 hours)
at term
Prematurity 1:435 1:2173 1:2377 1:11 885
(<37+0 weeks of gestation)
Prematurity 1:357 1:1786 1:1566 1:7829
(<35+0 weeks of gestation)
Positive GBS swab in a 1:1105 1:5525 1:10 424 1:52 122
previous pregnancy
Positive GBS swab in 1:434 1:2170 1:4094 1:20 471
current pregnancy
EOGBS = early-onset group B streptococcus; IAP = intrapartum antibiotic prophylaxis.
The assumptions on which the figures in the table above are based are as follows:
Live birth rate in the UK in 2008: 793 38844
1.9% intrapartum fever >38C45
9.4% PROM at term45
7.9% <37 weeks of gestation46
4.0% <35 weeks of gestation46
Prevalence of maternal risk factors in infants with EOGBS disease:
19.9% intrapartum fever >38C41,45
34% PROM at term5
37% <37 weeks of gestation5
22% <35 weeks of gestation5
Incidence of EOGBS in the UK: 0.5/10005
Mortality of EOGBS in the UK is:
10.6% overall5
18.3% <37 weeks of gestation
22.8% <35 weeks of gestation
5.7% >37 weeks of gestation
80% effectiveness of IAP in preventing EOGBS12
It should be noted that GBS bacteriuria is a risk factor for neonatal disease but the magnitude of risk cannot
be quantified.
RCOG Green-top Guideline No. 36 10 of 13 Royal College of Obstetricians and Gynaecologists
APPENDIX II
Indications for offering GBS-specific IAP:
Previous baby with invasive GBS infection.
GBS bacteriuria in the current pregnancy.
Vaginal swab positive for GBS in current pregnancy.
Pyrexia (>38C) in labour (give broad-spectrum antibiotics to include GBS cover).
Chorioamnionitis (give broad-spectrum antibiotics to include GBS cover).
IAP for GBS is not necessary if delivering by pre-labour lower segment caesarean section with intact
membranes.
RCOG Green-top Guideline No. 36 11 of 13 Royal College of Obstetricians and Gynaecologists
APPENDIX III
Clinical guidelines are systematically developed statements which assist clinicians and women in making
decisions about appropriate treatment for specific conditions. Each guideline is systematically developed
using a standardised methodology. Exact details of this process can be found in Clinical Governance
Advice No.1: Development of RCOG Green-top Guidelines (available on the RCOG website at
http://www.rcog.org.uk/guidelines). These recommendations are not intended to dictate an exclusive
course of management or treatment. They must be evaluated with reference to individual patient needs,
resources and limitations unique to the institution and variations in local populations. It is hoped that this
process of local ownership will help to incorporate these guidelines into routine practice. Attention is
drawn to areas of clinical uncertainty where further research might be indicated.
The evidence used in this guideline was graded using the scheme below and the recommendations
formulated in a similar fashion with a standardised grading scheme.
Classification of evidence levels Grades of recommendations
1++ High-quality meta-analyses, systematic At least one meta-analysis, systematic review or
reviews of randomised controlled trials A randomised controlled trial rated as 1++ and
or randomised controlled trials with a directly applicable to the target population; or
very low risk of bias
A systematic review of randomised controlled
1+ Well-conducted meta-analyses, systematic trials or a body of evidence consisting
reviews of randomised controlled trials principally of studies rated as 1+ directly
or randomised controlled trials with a applicable to the target population and
low risk of bias demonstrating overall consistency of results
1 Meta-analyses, systematic reviews of A body of evidence including studies rated as
randomised controlled trials or B 2++ directly applicable to the target
randomised controlled trials with a high population, and demonstrating overall
risk of bias consistency of results; or
2++ High-quality systematic reviews of Extrapolated evidence from studies rated as
casecontrol or cohort studies or high- 1++ or 1+
quality casecontrol or cohort studies
with a very low risk of confounding, bias A body of evidence including studies rated as
C 2+ directly applicable to the target population
or chance and a high probability that the
relationship is causal and demonstrating overall consistency of
results; or
2+ Well-conducted casecontrol or cohort
studies with a low risk of confounding, Extrapolated evidence from studies rated as
bias or chance and a moderate 2++
probability that the relationship is causal Evidence level 3 or 4; or
D
2- Casecontrol or cohort studies with a Extrapolated evidence from studies rated as 2+
high risk of confounding, bias or chance
and a significant risk that the
relationship is not causal Good practice point
3 Non-analytical studies, e.g. case reports, Recommended best practice based on the
case series P clinical experience of the guideline
4 Expert opinion development group
RCOG Green-top Guideline No. 36 12 of 21 Royal College of Obstetricians and Gynaecologists
This guideline was produced on behalf of the Guidelines Committee of the Royal College of Obstetricians and
Gynaecologists by:
Dr RG Hughes FRCOG, Edinburgh; Professor P Brocklehurst FRCOG, Oxford; Dr P Heath FRACP FRCPCH,
Paediatrics Infectious Diseases Unit, St Georges Hospital, London; and Dr B Stenson FRCPCH FRCPE,
Neonatolog
y Department, Simpson Centre for Reproductive Health, Edinburgh
and peer reviewed by: British Association of Perinatal Medicine; British Maternal and Fetal Medicine Society;
British Infection Association; Consumers Forum; Group B Strep Support; Womens Services Pharmacists Group, Leeds;
National Childbirth Trust; Royal College of Paediatrics and Child Health; UK National Screening Committee;
Department of Health; Mr FA Boret FRCOG, London; Dr N El Helali, Paris Saint-Joseph; Mr M J Heard FRCOG,
Winchester; Dr R Imtiaz MRCOG, Worcestershire; Dr G Kumar FRCOG, Chester; Dr PT Lynch MRCOG, Dundee;
Ms L Muir, Ayrshire Maternity Unit, Crosshouse Hospital, Kilmarnock; Dr J Sandoe, Leeds Teaching Hospitals NHS Trust,
Leeds General Infirmary; Dr A Simm MRCOG, Nottingham; Professor PJ Steer FRCOG, London.
Committee lead reviewers were: Mr M Griffiths FRCOG, Luton and Dr P Owen MRCOG, Glasgow.
Conflicts of interest: none declared.
The final version is the responsibility of the Guidelines Committee of the RCOG.
The guidelines review process will commence in 2015 unless evidence requires an earlier review.
DISCLAIMER
The Royal College of Obstetricians and Gynaecologists produces guidelines as an educational aid to good clinical
practice. They present recognised methods and techniques of clinical practice, based on published evidence, for
consideration by obstetricians and gynaecologists and other relevant health professionals. The ultimate judgement
regarding a particular clinical procedure or treatment plan must be made by the doctor or other attendant in the light
of clinical data presented by the patient and the diagnostic and treatment options available within the appropriate
health services.
This means that RCOG Guidelines are unlike protocols or guidelines issued by employers, as they are not intended to
be prescriptive directions defining a single course of management. Departure from the local prescriptive protocols or
guidelines should be fully documented in the patients case notes at the time the relevant decision is taken.
RCOG Green-top Guideline No. 36 13 of 13 Royal College of Obstetricians and Gynaecologists
Вам также может понравиться
- Urinary Tract Infection (UTI) - 4 Nursing Diagnosis InterventionsДокумент4 страницыUrinary Tract Infection (UTI) - 4 Nursing Diagnosis InterventionsEricsonMitra0% (2)
- School: Sta. Maria Integrated School Group No. Names: Energy Forms & Changes Virtual LabДокумент3 страницыSchool: Sta. Maria Integrated School Group No. Names: Energy Forms & Changes Virtual LabNanette Morado0% (1)
- Uterine Fibroids (Leiomyomas) - Treatment Overview - UpToDateДокумент40 страницUterine Fibroids (Leiomyomas) - Treatment Overview - UpToDateCristinaCapros100% (1)
- The Handbook of Continuing Professional Development For The Health IT ProfessionalДокумент315 страницThe Handbook of Continuing Professional Development For The Health IT ProfessionalAloah122346100% (2)
- Routine Antenatal Screening DR - Amy MellorДокумент3 страницыRoutine Antenatal Screening DR - Amy MellorYwagar Ywagar100% (1)
- Jurnal Inggris PDFДокумент4 страницыJurnal Inggris PDFTom PrasОценок пока нет
- Mohsen AttiaДокумент3 страницыMohsen AttiaAloah122346100% (1)
- Obstetric and Gynecology: A. ColpotomyДокумент44 страницыObstetric and Gynecology: A. ColpotomyAloah122346100% (1)
- Writing The Motherland From The DiasporaДокумент23 страницыWriting The Motherland From The DiasporaIfeoluwa Watson100% (1)
- Nausea and Vomiting of Pregnancy and Hyperemesis GravidarumДокумент27 страницNausea and Vomiting of Pregnancy and Hyperemesis GravidarumxxdrivexxОценок пока нет
- Green Top Guidelines 13Документ29 страницGreen Top Guidelines 13garfield1Оценок пока нет
- Green Top Guidelines 1Документ22 страницыGreen Top Guidelines 1garfield1Оценок пока нет
- Cardiff CountДокумент16 страницCardiff CountmohiiieОценок пока нет
- GTG 17 PDFДокумент18 страницGTG 17 PDFFlorida RahmanОценок пока нет
- GTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2Документ33 страницыGTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2fahlevyОценок пока нет
- Management of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51Документ13 страницManagement of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51indra_strongОценок пока нет
- 9 Antenatal Corticosteroid Green Top PDFДокумент13 страниц9 Antenatal Corticosteroid Green Top PDFangela_karenina_1Оценок пока нет
- RCOG - Management of Suspected Ovarian Masses in Premenopausal WomenДокумент14 страницRCOG - Management of Suspected Ovarian Masses in Premenopausal Womenestridente81Оценок пока нет
- Breech PresentationДокумент27 страницBreech PresentationNurkamilawati AristaОценок пока нет
- GTG 37bДокумент32 страницыGTG 37bKadelsy BristolОценок пока нет
- Deep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateДокумент26 страницDeep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateCristinaCaprosОценок пока нет
- Antepartum Hemorrhage PDFДокумент23 страницыAntepartum Hemorrhage PDFfrizkapfОценок пока нет
- gtg60 Cervicalcerclage PDFДокумент21 страницаgtg60 Cervicalcerclage PDFLijoeliyas100% (1)
- Ante Partum HemorrhageДокумент30 страницAnte Partum Hemorrhagetanmai nooluОценок пока нет
- Amniocentesis and CVS UHL Obstetric GuidelineДокумент8 страницAmniocentesis and CVS UHL Obstetric GuidelineGzz JoengОценок пока нет
- Case Title: PreeclampsiaДокумент6 страницCase Title: PreeclampsiaLanaОценок пока нет
- Vaginal Birth After Cesarean Section - Literature Review and Modern GuidelinesДокумент6 страницVaginal Birth After Cesarean Section - Literature Review and Modern GuidelinesCristinaCaprosОценок пока нет
- Recurrent Pregnancy LossДокумент61 страницаRecurrent Pregnancy LossHerman FiraОценок пока нет
- Gynecological History Taking and ExaminationДокумент17 страницGynecological History Taking and Examinationnmsiswaridewi100% (1)
- Revision Long Case Obs GynaeДокумент10 страницRevision Long Case Obs GynaeHo Yong WaiОценок пока нет
- Puerpera L Mental DisordersДокумент13 страницPuerpera L Mental DisordersclarheenaОценок пока нет
- Management of Septic Abortion and ComplicationsДокумент19 страницManagement of Septic Abortion and Complicationsapi-370504683% (6)
- Premature Rupture of MembraneДокумент6 страницPremature Rupture of MembraneSabna AjasОценок пока нет
- Approach To Patient With Ovarian Cysts: Done By: Yahyia Al-Abri 90440Документ53 страницыApproach To Patient With Ovarian Cysts: Done By: Yahyia Al-Abri 90440NinaОценок пока нет
- Breast Abcess PDFДокумент4 страницыBreast Abcess PDFponekОценок пока нет
- GTG 67 Endometrial HyperplasiaДокумент31 страницаGTG 67 Endometrial HyperplasiaFinka Inarae100% (1)
- Obgyn Anemia in Pregnancy For UG ClassДокумент35 страницObgyn Anemia in Pregnancy For UG ClassimranОценок пока нет
- Bacterial Sepsis in PregnancyДокумент14 страницBacterial Sepsis in PregnancydraasfourОценок пока нет
- Anemia in PregnancyДокумент79 страницAnemia in Pregnancypat duaОценок пока нет
- Prom 1Документ48 страницProm 1Tesfahun TekleОценок пока нет
- Anaemia in PregnancyДокумент41 страницаAnaemia in PregnancyWan Ahmad FaizFaizalОценок пока нет
- Hepatitis B in PregnancyДокумент17 страницHepatitis B in PregnancysnazzyОценок пока нет
- Antenatal Care During The First, SecondДокумент85 страницAntenatal Care During The First, SecondhemihemaОценок пока нет
- Infection in Pregnancy PDFДокумент39 страницInfection in Pregnancy PDFsimmyvashisht100% (1)
- Hypertension in PregnancyДокумент45 страницHypertension in PregnancyMary Anne Cabalza ApinardoОценок пока нет
- Preterm Prelabour Rupture of MembranesДокумент12 страницPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanОценок пока нет
- Blood Transfusiopn in Obstetrics (RCOG, May 2015) PDFДокумент23 страницыBlood Transfusiopn in Obstetrics (RCOG, May 2015) PDFwebcob246Оценок пока нет
- Uterine Fibroids (Leiomyomas) - Differentiating Fibroids From Uterine Sarcomas - UpToDateДокумент31 страницаUterine Fibroids (Leiomyomas) - Differentiating Fibroids From Uterine Sarcomas - UpToDateCristinaCaprosОценок пока нет
- CV Europass CaprosДокумент3 страницыCV Europass CaprosCristinaCaprosОценок пока нет
- Intra Uterin Fetal DeathДокумент15 страницIntra Uterin Fetal DeathanojanОценок пока нет
- Recurrent AbortionsДокумент33 страницыRecurrent AbortionsnasibdinОценок пока нет
- Multiple Pregnancy: Dr. A. Farid Abdullah, SP - OG, M.KesДокумент33 страницыMultiple Pregnancy: Dr. A. Farid Abdullah, SP - OG, M.KesAndi Farid AОценок пока нет
- RCOG Guidelines - Gestational Trophoblastic DiseaseДокумент12 страницRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- Obstetrics and GynacologyДокумент14 страницObstetrics and GynacologykalkidanОценок пока нет
- Ovarian TorsionДокумент48 страницOvarian Torsionmaria ilyasОценок пока нет
- Bicornuate Unicolli Uterus 2Документ46 страницBicornuate Unicolli Uterus 2Anjali LimbuОценок пока нет
- Thromboembolic Disease in Pregnancy د.علية شعيبДокумент50 страницThromboembolic Disease in Pregnancy د.علية شعيبMohammad Belbahaith0% (1)
- Overview Antenatal CareДокумент54 страницыOverview Antenatal CareRizky Dwidya AmirtasariОценок пока нет
- Intrauterine Growth Restriction IUGR: TH THДокумент2 страницыIntrauterine Growth Restriction IUGR: TH THZahra AlaradiОценок пока нет
- Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015Документ36 страницVaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015kikyОценок пока нет
- Uterine Malformations PDFДокумент6 страницUterine Malformations PDFsaritha OrugantiОценок пока нет
- Ectopic PregnancyДокумент26 страницEctopic PregnancyDavid SitinjakОценок пока нет
- VBACДокумент31 страницаVBACAnonymous VlpThs35AОценок пока нет
- Uterine Fibroid-IzzatДокумент20 страницUterine Fibroid-IzzatcopperОценок пока нет
- Drug List by Therapeutic Category: Cardiovascular DrugsДокумент7 страницDrug List by Therapeutic Category: Cardiovascular DrugsAloah122346Оценок пока нет
- Part I سنه القمله 2016Документ20 страницPart I سنه القمله 2016Aloah122346Оценок пока нет
- In The Classroom Study Strategies: Better GradesДокумент4 страницыIn The Classroom Study Strategies: Better GradesAloah122346100% (1)
- Saudi Board OSCE2015Документ8 страницSaudi Board OSCE2015Aloah122346Оценок пока нет
- Part ,, Online Contraceptive Related Information Seeking Behaviour QuestionsДокумент15 страницPart ,, Online Contraceptive Related Information Seeking Behaviour QuestionsAloah122346Оценок пока нет
- Final Exam Saudi Board 2009Документ38 страницFinal Exam Saudi Board 2009Aloah122346Оценок пока нет
- Pre NEET Obstetrics and Gynaecology (2013) (PDF) (UnitedVRG)Документ320 страницPre NEET Obstetrics and Gynaecology (2013) (PDF) (UnitedVRG)Aloah122346100% (2)
- Saudi Board Exam 2015: These Answers Are Mine, They May Be Right, May Be WrongДокумент22 страницыSaudi Board Exam 2015: These Answers Are Mine, They May Be Right, May Be WrongAloah122346Оценок пока нет
- Promotion OBGYNДокумент30 страницPromotion OBGYNAloah122346Оценок пока нет
- Promotion 2013-2014 With AnswerДокумент36 страницPromotion 2013-2014 With AnswerAloah122346Оценок пока нет
- 1 PromtionДокумент14 страниц1 PromtionAloah122346Оценок пока нет
- Workshops, Seminars, Conferences and Symposia Attended During Assistant ProfessorДокумент4 страницыWorkshops, Seminars, Conferences and Symposia Attended During Assistant ProfessorAloah122346Оценок пока нет
- DRTP Specialty Handbook Obstetrics and GynaecologyДокумент48 страницDRTP Specialty Handbook Obstetrics and GynaecologyAloah122346Оценок пока нет
- Obesity & It'S Management: Supervised By: Dr. AlnaamiДокумент58 страницObesity & It'S Management: Supervised By: Dr. AlnaamiAloah122346Оценок пока нет
- 2014reVITALizeObstetricDataDefinitionsV10 PDFДокумент5 страниц2014reVITALizeObstetricDataDefinitionsV10 PDFAloah122346Оценок пока нет
- 25 IcuДокумент78 страниц25 IcuAloah122346Оценок пока нет
- Case Diagnosis For RomanДокумент4 страницыCase Diagnosis For RomanChris Marie JuntillaОценок пока нет
- Emissivity Table E4Документ11 страницEmissivity Table E4Mekro Permana PinemОценок пока нет
- 6th Grade Spelling ListsДокумент10 страниц6th Grade Spelling Listsapi-326416336Оценок пока нет
- Gpat Reference NotesДокумент9 страницGpat Reference NotesPreethi KiranОценок пока нет
- Aplication Pipe and Tube - Nippon SteelДокумент29 страницAplication Pipe and Tube - Nippon Steelmatheus david100% (1)
- Gulayan Sa Barangay OrdinanceДокумент2 страницыGulayan Sa Barangay OrdinancekonsinoyeОценок пока нет
- Huayi: Refrigeration CompressorДокумент2 страницыHuayi: Refrigeration CompressorVARDANОценок пока нет
- Profile of RespondentsДокумент36 страницProfile of RespondentsPratibha SharmaОценок пока нет
- 134.4902.06 - DM4170 - DatasheetДокумент7 страниц134.4902.06 - DM4170 - DatasheetVinicius MollОценок пока нет
- Barangay Clearance SampleДокумент1 страницаBarangay Clearance SampleBarangay Onse Malaybalay100% (3)
- Sathyamangalam Chennai MR Sivakumar N: Rolsun TravelsДокумент2 страницыSathyamangalam Chennai MR Sivakumar N: Rolsun TravelsGayu carita catoОценок пока нет
- Peseshet - The First Female Physician - (International Journal of Gynecology & Obstetrics, Vol. 32, Issue 3) (1990)Документ1 страницаPeseshet - The First Female Physician - (International Journal of Gynecology & Obstetrics, Vol. 32, Issue 3) (1990)Kelly DIOGOОценок пока нет
- C 08 S 09Документ8 страницC 08 S 09Marnel Roy MayorОценок пока нет
- Unit Plan Adult Health Nursing Unit IIДокумент7 страницUnit Plan Adult Health Nursing Unit IIDelphy VargheseОценок пока нет
- 6 Adjective ClauseДокумент16 страниц6 Adjective ClauseMaharRkpОценок пока нет
- Training and BreathingДокумент6 страницTraining and BreathingMIIIBОценок пока нет
- Green Partnership of The Future: DieselfactsДокумент12 страницGreen Partnership of The Future: DieselfactsKamal WanniarachchiОценок пока нет
- Good Laboratory Practice GLP Compliance Monitoring ProgrammeДокумент17 страницGood Laboratory Practice GLP Compliance Monitoring ProgrammeamgranadosvОценок пока нет
- FRMUnit IДокумент17 страницFRMUnit IAnonОценок пока нет
- 5219-PRP Support Tool CounsellingДокумент10 страниц5219-PRP Support Tool CounsellingRodhi AnshariОценок пока нет
- Stats Review CH 1-6Документ15 страницStats Review CH 1-6Megha BanerjeeОценок пока нет
- Revised Man As A Biological BeingДокумент8 страницRevised Man As A Biological Beingapi-3832208Оценок пока нет
- Performance Management and Strategic Planning:: Organization's Strategic PlanДокумент7 страницPerformance Management and Strategic Planning:: Organization's Strategic PlanSara AbidОценок пока нет
- Tugas Gizi Caesar Nurhadiono RДокумент2 страницыTugas Gizi Caesar Nurhadiono RCaesar 'nche' NurhadionoОценок пока нет
- Chuyên Anh S Hà N I 2021Документ5 страницChuyên Anh S Hà N I 2021Jennifer WatsonОценок пока нет
- Republic Act No. 10070Документ3 страницыRepublic Act No. 10070Ganiela MCОценок пока нет
- Annual Sustainability Report 2022-23 FinalДокумент93 страницыAnnual Sustainability Report 2022-23 FinalLakshay JajuОценок пока нет