Академический Документы
Профессиональный Документы
Культура Документы
Accuracy of Temporomandibular Joint Disc Displacement Diagnosis in Panoramic Radiography
Загружено:
Samuel Flores CalderonОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Accuracy of Temporomandibular Joint Disc Displacement Diagnosis in Panoramic Radiography
Загружено:
Samuel Flores CalderonАвторское право:
Доступные форматы
Original Article
Accuracy of temporomandibular joint disc
displacement diagnosis in panoramic radiography:
Validation by magnetic resonance imaging
Acurcia do diagnstico de deslocamento de disco da articulao
temporomandibular por radiografia panormica: validao
utilizando imagem por ressonncia magntica
Abstract Julieta P. Franaa
Bruno H. F. Matosa
Purpose: To investigate if panoramic radiography would be a suitable tool to diagnose Bernardino R. de Senaa
temporomandibular joint disc displacement. Leandro S. Marquesa
Gustavo H. Gameirob
Methods: The sample comprised 56 female patients divided into three groups: (1) Control Paula M. Casteloc
(n=30); (2) disk displacement with reduction (n=17); and (3) disc displacement without Luciano J. Pereirad
reduction (n=9). All patients were evaluated according to the Research Diagnostic Criteria
(RDC/TMD). Linear and angular measurements and proportion determinations were obtained
from tracings of panoramic radiographs. They were compared with condyle and disc positioning
obtained from Magnetic Resonance Imaging (MRI) images to assess any predictive measurement a Department of Clinical Dentistry, University of
associated with disc displacement with or without reduction. Possible relationship to clinical Vale do Rio Verde, Trs Coraes, MG, Brazil
b Department of Physiology, Federal University of
signs and symptoms of TMD was also evaluated.
Rio Grande do Sul, Porto Alegre, RS, Brazil
Results: There was no significant difference among the three groups regarding the radiograph c Department of Biological Sciences, Federal
variables. No significant association was found between radiographic variables and clinical University of So Paulo, Diadema, SP, Brazil
signs or between the radiographic and MRIs variables. d Department of Physiology and Pharmacology,
Federal University of Lavras, Lavras, MG, Brazil
Conclusion: The use of panoramic radiography imaging exam for diagnostic prediction in
clinical practice does not seem advisable.
Key words: Temporomandibular joint disorders; panoramic radiography; magnetic resonance
imaging
Resumo
Objetivo: Investigar a possibilidade de utilizao de medidas obtidas em radiografias
panormicas como instrumento preditivo para o diagnstico de deslocamento de disco da
articulao temporomandibular.
Metodologia: A amostra foi composta por 56 pacientes do sexo feminino divididos em
trs grupos: (1) controle (n=30); (2) deslocamento do disco com reduo (n=17); e
(3) deslocamento do disco sem reduo (n=9). Todas as pacientes foram avaliadas com base
nos Critrios Diagnsticos de Pesquisa para Desordens Temporomandibulares (RDC/TMD).
Medidas lineares e angulares, bem como propores foram obtidas a partir de traados em
radiografias panormicas e estas foram comparadas com o posicionamento do cndilo e Correspondence:
disco obtidos a partir de Imagens por Ressonncia Magntica (MRI). Correlaes com sinais Luciano Jos Pereira
Universidade Federal de Lavras UFLA DMV
clnicos e sintomas de disfuno temporomandibular (DTM) tambm foram avaliadas. Setor de Fisiologia e Farmacologia
Resultados: No houve diferena significativa entre os trs grupos em relao s variveis Campus Universitrio Caixa Postal 3037
Lavras, MG Brasil
estudadas nas radiografias. No foram encontradas associaes significativas entre as 37200-000
variveis radiogrficas e os sinais clnicos nem entre as variveis radiogrficas e de ressonncia E-mail: lucianojosepereira@dmv.ufla.br
magntica.
Concluso: O uso de medidas em radiografias panormicas como preditoras do diagnstico
Received: September 12, 2012
de deslocamento de disco na prtica clnica no parece ser aconselhvel. Accepted: December 27, 2012
Palavras-chave: Disfuno temporomandibular; radiografia panormica; ressonncia
magntica Conflict of Interests: The authors state that there
are no financial and personal conflicts of interest that
could have inappropriately influenced their work.
Copyright: 2012 Frana et al.; licensee EDIPUCRS.
This is an Open Access article distributed under
the terms of the Creative Commons Attribution-
Noncommercial-No Derivative Works 3.0 Unported
License.
Rev Odonto Cienc 2012;27(4):283-288 283
Temporomandibular joint disc displacement diagnosis
INTRODUCTION professional. The RDC/TMD index was used before the MRI
exam in order to investigate clinical signs and symptoms of
Temporomandibular disorder (TMD) is a multifactorial disc displacement that would justify MRI examination. The
condition and it has been associated with psychological RDC was also used to standardize jaw amplitude movements
dysfunctions and sexual dimorphism with coincidental and pain scale (13) data collection. In the control group,
occurrence along the pubertal development (1). The the clinical exam from Axis 1 of the RDC was used for the
diagnosis of TMD involves a combination of questionnaires, selection of non-symptomatic individuals.
clinical exams and complementary imaging exams (2). For
such, magnetic resonance imaging (MRI) is considered the Image assessment
gold standard for disc displacement diagnosis (3-5). The Images were obtained with positions of closed and
advantages of MRI are evident due to the visualization fully open mouth. All subjects underwent MRI of the TMJ
of both mineralized and non-mineralized structures of obtained by a 2 Tesla scanner (Elscint Prestige, Haifa, Israel)
the temporomandibular joint (TMJ) and the absence of with surface coils (14).
known accumulative biological effects of radiowaves and
magnetism. The main disadvantages of this exam are its Disc position
high cost as well as the need for sophisticated equipment The position of the disc with the mouth closed was
and specialized personnel (6). based on the clock face using the thickest part of posterior
Panoramic radiographs are extremely widespread in the band as reference (15). Discs located anteriorly to the 11
diagnosis and planning of dental treatment due to their easy oclock position were considered displaced (5,15). Images
execution and low cost (7). For the diagnosis of TMD, the with mouth open were used to confirm the clinical diagnosis
information provided by radiographs is reported as being of displacement with or without reduction as well as to
limited (8). Nevertheless, some variables encountered in this assess mandibular excursion. Discs classified as normal
type of exam were considered compatible with a diagnosis of were interposed between the lowermost portion of the
internal derangement (9). Studies assessing the reliability and eminence and the uppermost portion of the condyle (4).
accuracy of panoramic radiographs in patients with TMD are Disc displacement was considered to be with reduction when
rare and normally focus on the presence of abnormalities in the disc was positioned between the uppermost portion of
the shape of the bone structures (7,8,10). Studies associating the condyle and the lowermost portion of the eminence
linear, angle and proportion measurements with clinical with movement with the mouth open. The diagnosis of disc
signs of TMD are also scarce. displacement without reduction was considered when the
The main objective of this study was to investigate if disc remained anteriorized in relation to the structures of the
panoramic radiography would be a suitable tool to diagnose condyle and eminence in the sagittal images.
temporomandibular joint disc displacement, exploring if
any angle or proportion measured in panoramic radio- Condyle position
graphy would be more prevalent in or associated with The condyle position in the sagittal images with the
patients diagnosed with disc displacement by MRI. mouth closed was determined based on Gelbs template (in
Measurements and proportion determinations were obtained postural rest position and maximum intercuspation, since
from tracings of panoramic radiographs and they were in maximum opening the condylar position was not inside
compared with condyle and disc positioning obtained from the areas determined by the drawn lines), which classifies
MRI. the normal position of the condyle tracing five lines three
horizontal and two vertical lines. The template and positions
METHODS have been described previously (16,17).
The study was approved by the Institutional Ethics Panoramic radiographs
Committee (CAAE 0007.0.380.000-07). The sample The bilateral contours of the condyle and ramus in the
was comprised of 56 female subjects, 18 to 60 years old. panoramic radiographs were traced onto Ultrafan paper.
The patients had a diagnosis of anterior disc displacement A single investigator performed the tracing on all the
with and without reduction by MRI and were divided radiographs. Seven points were marked on each side, from
into three groups: (1) control (non-symptomatic subjects) which six variables were evaluated (3 lines, 1 angle and 2
(n=30); (2) disc displacement with reduction (n=17); and proportions). All variables were evaluated as described by
disc displacement without reduction (n=9). All clinical and Ahn et al. (9). The linear measurements consisted of ramus
MRI evaluations have been previously described (11) and height, condyle height and height of the condyle head. The
are briefly reported below. angle measurement was defined by the angle between the
condyle axis and ramus tangent (ACA-RT). The proportions
Clinical evaluation consisted of the relation between the height of the condyle
All participants underwent clinical examination based head and ramus height (HCH-RH) as well as the relation
on the Research Diagnostic Criteria (RDC/TMD) (12). between the condyle height and ramus height (CH-RH).
The clinical evaluation was performed by a single trained For the calculation of measurement error, 15 radiographs
284 Rev Odonto Cienc 2012;27(4):283-288
Frana et al.
were randomly selected and the tracing was repeated, with RESULTS
a two-week interval between measurements. The Kappa
agreement index between measurements was > 0.85. There was no statistically significant difference among
groups regarding the linear and angular measurements or
Statistical analysis the proportion determinations in the panoramic radiographs
The data for the linear, angle and proportion deter- (Table 1).
minations were analyzed by using analysis of variance Table 2 displays the results of the correlation between the
(ANOVA), Kruskal-Wallis test, Persons correlation proportions and angle obtained in the panoramic radiographs
coefficient and Spearmans correlation coefficient, at a 5% and the following clinical variables: pain (VAS), maximal
level of significance. Bivariate regression model was applied opening of the mouth and maximal lateral movement. No
for the identification of factors independently associated with significant correlations were found between the variables
the presence disc displacement with or without reduction. (P>0.05). Spearmans correlation analysis between the
Variables that achieved a P-value of 0.30 were used as variables on the panoramic radiographs and condyle position,
potential predictors of TMD and inserted as covariates in the disc position and condyle excursion obtained on the MRIs
multivariate analysis. Multivariate logistic regression was revealed no significant correlations (P>0.05) (Table 3).
performed controlling for age, with a significance level of The stepwise backward logistic regression showed no
P<0.05. The software SPSS 9.0, (Chicago, USA) was used association of radiographic variables with the studied sample
for all analyses. (Table 4).
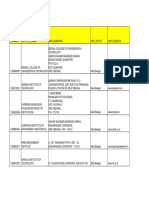
Table 1. Comparison of proportions and angles obtained in the panoramic radiographs between
the Control, Displacement with reduction and Displacement without reduction groups.
Mean standard deviation
Displacement with Displacement with P-value
Control
reduction reduction
HCH 0.6330.16 0.6410.17 0.6170.26 0.850*
CH 2.1380.41 1.9560.39 2.0940.38 0.127
RH 4.6600.443 4.6310.464 4.3890.411 0.076
HCH/RH 0.1320.03 0.1350.04 0.1400.06 0.922*
CH/RH 0.4630.11 0.4210.12 0.4700.13 0.222
ACA/RT 1.81610.29 3.09311.41 3.61110.89 0.070
HCH/RH: relation between height of condyle head and ramus height; CH/RH: relation between condyle height and
ramus height; ACA-RT angle between condyle axis and ramus tangent.
* Kruskal-Wallis test; One-Way ANOVA.
Table 2. Correlation (Pearsons coefficient) between proportions Table 3. Correlation (Spearmans coefficient) between
and angles obtained on panoramic radiographs and clinical pain proportions and angles obtained on panoramic radiographs
(VAPS), maximal opening (mm) and lateral movement (mm). and variables obtained from MRI.
Displacement Displacement Condyle Disc Condyle
with reduction without reduction position position excursion
HCH/RH and VAPS r=-0.144 r=-0.410 HCH/RH r=-0.159 r=-0.087 r=-0.037
P=0.596 P=0.274 P=0.268 P=0.547 P=0.795
CH/RH and MO r=-0.093 r=-0.102 CH/RH r=-0.114 r=0.218 r=0.052
P=0.730 P=0.793 P=0.429 P=0.127 P=0.714
ACA/RT and LAT r=-0.043 r=0.598 ACA/RT r=0.134 r=0.091 r=-0.165
P=0.873 P=0.089 P=0.353 P=0.524 P=0.250
HCH/RH: relation between height of condyle head and ramus height; HCH/RH: relation between height of condyle head and ramus height;
CH/RH: relation between condyle height and ramus height; ACA-RT angle CH/RH: relation between condyle height and ramus height; ACA-RT angle
between condyle axis and ramus tangent; VAPS: visual analogue pain scale; between condyle axis and ramus tangent.
MO: Maximal opening of mouth; LAT: Maximal lateral movement.
Rev Odonto Cienc 2012;27(4):283-288 285
Temporomandibular joint disc displacement diagnosis
Table 4. Stepwise backward logistic regression used to test the association of radiographic variables with TMD (disc displacement
with and without reduction) as the dependent variable in the studied sample.
Dependent Independent Significance of the model
Coef. P-value Odds ratio IC
variable variables R2 P-value Power
constant 2.676
15-R 0.591
16-R 0.632
11-R 0.358
15-L 0.350
16-L 0.611
TMD 11-L 0.882 0.112 0.055 0.709
HCH/R 0.521
CH/R 0.992
RH/R 0.196
HCH/L 0.293
CH/L 0.403
RH/L 0.341
TMD: temporomandibular dysfunction. 11: angle between condyle axis and ramus tangent; 15: relationship between height of the condyle head and ramus
height; 16: relationship between condyle head and ramus height. HCH: height of condyle head; CH: condyle height; RH: ramus height; R: right side; L: left side.
DISCUSSION associated with skeletal changes in the head of the mandible
(9). In the present study, however, no significant differences
Due to its economic advantages, panoramic radiography were found in the same variables studied by Ahn et al. (9)
would be an extremely useful tool if there were an association when patients with disc displacement with and without
between the diagnosis performed with this type of imaging reduction were compared to control patients. It should be
and clinical criteria or MRI for patients with internal stressed that the differences between the two studies may be
derangement of the TMJ. However, the present study related to the equipment employed (9), resolution of images,
found no significant differences in the variables obtained sample size regarding disc displacement without reduction
in panoramic radiographs in individuals with and without in particular and age of patients, since older patients tend to
internal derangement. These findings suggest the limitation present more pronounced signs of the disease (20).
of using panoramic radiography in the diagnosis of TMD. The combination of a clinical exam and imaging exam
With the enormous advance in imaging techniques, of the TMJ are often used in the diagnosis of TMD (21).
panoramic radiography has lost its place with regard to The relationship between the variables in the panoramic
precise diagnoses of the TMJ, mainly due to its limitations radiographs (ACA-RT, HCH-RH and CH-RH) and the pain
regarding the visualization of soft tissues. Even in the scale, range of mandibular movement, condyle position, disc
diagnosis of mineralized tissues, use of this imaging modality position and condyle excursion was analyzed. There were no
is restricted to delayed bone abnormalities (6). The accuracy significant correlations among these variables in the sample
and reliability of diagnoses regarding condyle shape in studied. These findings are compatible with previous studies
patients with TMD was assessed through a comparison of that have sought a correlation between the signs and symptoms
blind evaluations of the TMJ on panoramic radiographs, of TMD and imaging findings (22,23).The results suggest
using MRIs and the clinical exam as the gold standards. that the severity of internal derangement has no association
However, the results were discouraging (18). with the intensity of pain reported by the patient. This
Morphological bone variations among individuals and corroborates previous studies that found internal derange-
superposing artifacts contribute to the absence of relationship ment in 30% of asymptomatic volunteers (5) and 13.8%
between panoramic measurements and disc displacement. of discs in a normal position in symptomatic patients (24).
Besides, bone remodeling can induce changes similar The number of healthy individuals with abnormalities in disc
to those of dysfunction patients, and this could explain position ranges from 17.5% to 35% (4,5,20,25). Thus, the
the high prevalence of radiological alterations in healthy fact that the disc is not correctly positioned is not indicative
individuals (19). of the presence of signs and symptoms of TMD.
In a previous study, individuals with disc displacement The relation between the presence of signs and symptoms
without reduction exhibited resorbed, reduced condyles of TMJ and condyle position remains controversial (24). A
inclined distally when compared to individuals with discs number of studies on the position of the condyle and its
in the normal position or those with displacement with therapeutic implications have shown that pain and limited
reduction. Internal derangement in the TMJ has been opening of the mouth are not present in all cases (25).
286 Rev Odonto Cienc 2012;27(4):283-288
Frana et al.
The assessment of reliability, validity, risk, cost and MRIs and clinical signs of internal derangement, thereby
usefulness of a diagnostic procedure is an essential part contraindicating the use of this type of imaging for diagnostic
of the treatment plan for patients with TMD. Panoramic prediction in clinical practice.
radiographs are frequently solicited in initial examinations
of patients with orofacial pain. These exams may reveal bone Acknowledgments
or condyle positioning abnormalities. However, even when
these conditions are encountered, they do not normally relate The authors would like to thank the scholarships
to the clinical condition or influence decisions regarding sponsored by the Coordination for the Improvement of
the treatment plan (7). This was evidenced in the present Higher Education Personnel (CAPES), Funding Agency of
study by the lack of significant associations between clinical the State of Minas Gerais (FAPEMIG) and the National
variables (pain, range of mandible movement) and condyle Council of Science and Technology Development (CNPq)
position or disc displacement. for research grants awarded to JPF, BFM and LJP,
In conclusion, there was no relationship between the respectively.
variables obtained on the panoramic radiographs and
References 1. Aneiros-Guerrero A, Lendinez AM, Palomares AR, Perez-Nevot B, Aguado L, Mayor-Olea
A et al. Genetic polymorphisms in folate pathway enzymes, DRD4 and GSTM1 are related
to temporomandibular disorder. BMC Med Genet 2011;12:75-79.
2. Kalaykova SI, Lobbezoo F, Naeije M. Risk factors for anterior disc displacement with
reduction and intermittent locking in adolescents. J Orofac Pain 2011;25:153-60.
3. Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL et al. Research
diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image
analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 2009;107:844-60.
4. Haiter-Neto F, Hollender L, Barclay P, Maravilla KR. Disk position and the bilaminar zone
of the temporomandibular joint in asymptomatic young individuals by magnetic resonance
imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:372-8.
5. Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence
of temporomandibular joint disk displacement in patients and symptom-free volunteers.
Am J Orthod Dentofacial Orthop 1996;109:249-62.
6. Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell KA et al. Imaging of
the temporomandibular joint: a position paper of the American Academy of Oral and
Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:
609-18.
7. Epstein JB, Caldwell J, Black G. The utility of panoramic imaging of the temporomandibular
joint in patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod 2001;92:236-9.
8. Crow HC, Parks E, Campbell JH, Stucki DS, Daggy J. The utility of panoramic radiography
in temporomandibular joint assessment. Dentomaxillofac Radiol 2005;34:91-5.
9. Ahn SJ, Kim TW, Lee DY, Nahm DS. Evaluation of internal derangement of the
temporomandibular joint by panoramic radiographs compared with magnetic resonance
imaging. Am J Orthod Dentofacial Orthop 2006;129:479-85.
10. Dahlstrm L, Lindvall AM. Assessment of temporomandibular joint disease by panoramic
radiography: reliability and validity in relation to tomography. Dentomaxillofac Radiol
1996;25:197-201.
11. Robinson de Senna B, Marques LS, Frana JP, Ramos-Jorge ML, Pereira LJ. Condyle-disk-
fossa position and relationship to clinical signs and symptoms of temporomandibular
disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:
e117-24.
12. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders:
review, criteria, examinations and specifications, critique. J Craniomandib Disord
1992;6:301-55.
13. Gil IA, Barbosa CM, Pedro VM, Silverio KC, Goldfarb DP, Fusco V et al. Multidisciplinary
approach to chronic pain from myofascial pain dysfunction syndrome: a four-year
experience at a Brazilian center. Cranio 1998;16:17-25.
14. Costa AL, DAbreu A, Cendes F. Temporomandibular joint internal derangement: association
with headache, joint effusion, bruxism, and joint pain. J Contemp Dent Pract 2008;9:9-16.
15. Orsini MG, Kuboki T, Terada S, Matsuka Y, Yamashita A, Clark GT. Diagnostic value of 4
criteria to interpret temporomandibular joint normal disk position on magnetic resonance
images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86:489-97.
16. Gelb H. The optimum temporomandibular joint condyle position in clinical practice. Int J
Periodontics Restorative Dent 1985;5:34-61.
Rev Odonto Cienc 2012;27(4):283-288 287
Temporomandibular joint disc displacement diagnosis
17. Serra MD, Gavio MB. Evaluation of condylar position from transcranial projections in
primary dentition. Dentomaxillofac Radiol 2006;35:110-6.
18. Schmitter M, Gabbert O, Ohlmann B, Hassel A, Wolff D, Rammelsberg P et al. Assessment
of the reliability and validity of panoramic imaging for assessment of mandibular condyle
morphology using both MRI and clinical examination as the gold standard. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 2006;102:220-4.
19. Kircos LT, Ortendahl DA, Mark AS, Arakawa M. Magnetic resonance imaging of the TMJ
disc in asymptomatic volunteers. J Oral Maxillofac Surg 1987;45:852-4.
20. Poveda-Roda R, Bagn JV, Jimnez-Soriano Y, Fons-Font A. Retrospective study of a series
of 850 patients with temporomandibular dysfunction (TMD). Clinical and radiological
findings. Med Oral Patol Oral Cir Bucal 2009;14:e628-634.
21. Jank S, Emshoff R, Norer B, Missmann M, Nicasi A, Strobl H et al. Diagnostic quality of
dynamic high-resolution ultrasonography of the TMJ--a pilot study. Int J Oral Maxillofac
Surg 2005;34:132-7.
22. Bertram S, Rudisch A, Innerhofer K, Pmpel E, Grubwieser G, Emshoff R. Diagnosing TMJ internal
derangement and osteoarthritis with magnetic resonance imaging. J Am Dent Assoc 2001;132:
753-61.
23. Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the
temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg
1996;54:147-53.
24. Ribeiro RF, Tallents RH, Katzberg RW, Murphy WC, Moss ME, Magalhaes AC et al. The
prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to
25 years. J Orofac Pain 1997;11:37-47.
25. Pereira LJ, Gavio MB, Bonjardim LR, Castelo PM. Ultrasound and tomographic evaluation
of temporomandibular joints in adolescents with and without signs and symptoms of
temporomandibular disorders: a pilot study. Dentomaxillofac Radiol 2007;36:402-8.
288 Rev Odonto Cienc 2012;27(4):283-288
Copyright of Revista Odonto Ciencia is the property of Editora da Pontificia Universidade
Catolica do Rio Grande do Sul and its content may not be copied or emailed to multiple sites
or posted to a listserv without the copyright holder's express written permission. However,
users may print, download, or email articles for individual use.
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- 15 Day Detox ChallengeДокумент84 страницы15 Day Detox ChallengeDanii Supergirl Bailey100% (4)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Sample Monologues PDFДокумент5 страницSample Monologues PDFChristina Cannilla100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- ChatGpt PDFДокумент19 страницChatGpt PDFsanx2014100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Workbook Group TheoryДокумент62 страницыWorkbook Group TheoryLi NguyenОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Medical Risk Assessment in Dentistry: Use of The American Society of Anesthesiologists Physical Status ClassificationДокумент6 страницMedical Risk Assessment in Dentistry: Use of The American Society of Anesthesiologists Physical Status ClassificationSamuel Flores CalderonОценок пока нет
- Configuring BGP On Cisco Routers Lab Guide 3.2Документ106 страницConfiguring BGP On Cisco Routers Lab Guide 3.2skuzurov67% (3)
- Intraoral Gothic Arch Tracing PDFДокумент5 страницIntraoral Gothic Arch Tracing PDFSamuel Flores CalderonОценок пока нет
- Meno's Paradox of Inquiry and Socrates' Theory of RecollectionДокумент10 страницMeno's Paradox of Inquiry and Socrates' Theory of RecollectionPhilip DarbyОценок пока нет
- Distribución Del Estrés, Tensión Residual Del Diente y Resistencia A La Fractura de Molares Tratados EndodónticamenteДокумент13 страницDistribución Del Estrés, Tensión Residual Del Diente y Resistencia A La Fractura de Molares Tratados EndodónticamenteSamuel Flores CalderonОценок пока нет
- Universal AdhesivesДокумент5 страницUniversal AdhesivesSamuel Flores CalderonОценок пока нет
- The Periodontal Ligament: A Unique, Multifunctional Connective TissueДокумент21 страницаThe Periodontal Ligament: A Unique, Multifunctional Connective TissueSamuel Flores CalderonОценок пока нет
- Cemented Implant Restoration A Technique For Minimizing Adverse Biologic Consequences PDFДокумент4 страницыCemented Implant Restoration A Technique For Minimizing Adverse Biologic Consequences PDFSamuel Flores CalderonОценок пока нет
- Navegacion Tridimensional en ImplantologiaДокумент12 страницNavegacion Tridimensional en ImplantologiaSamuel Flores CalderonОценок пока нет
- Accuracy of Implant Placement With A Esterolitografia PDFДокумент8 страницAccuracy of Implant Placement With A Esterolitografia PDFSamuel Flores CalderonОценок пока нет
- Effect of Occlusal Vertical Dimension On Lip Positions at SmileДокумент7 страницEffect of Occlusal Vertical Dimension On Lip Positions at SmileSamuel Flores CalderonОценок пока нет
- Una Propuesta de Distancia Esquelética Lineal para Predecir La Dimensión Vertical Oclusal Un Estudio CefalométricoДокумент4 страницыUna Propuesta de Distancia Esquelética Lineal para Predecir La Dimensión Vertical Oclusal Un Estudio CefalométricoSamuel Flores CalderonОценок пока нет
- Rehabilitación de Dientes Severamente Desgastados Una Revisión SistemáticaДокумент25 страницRehabilitación de Dientes Severamente Desgastados Una Revisión SistemáticaSamuel Flores CalderonОценок пока нет
- Tooth To Implant ConnectionДокумент36 страницTooth To Implant ConnectionSamuel Flores CalderonОценок пока нет
- An All-In-One Adhesive Does Not Etch Beyond Hybrid LayersДокумент6 страницAn All-In-One Adhesive Does Not Etch Beyond Hybrid LayersSamuel Flores CalderonОценок пока нет
- Chapter 13 (Automatic Transmission)Документ26 страницChapter 13 (Automatic Transmission)ZIBA KHADIBIОценок пока нет
- Cable To Metal Surface, Cathodic - CAHAAW3Документ2 страницыCable To Metal Surface, Cathodic - CAHAAW3lhanx2Оценок пока нет
- 6GK74435DX040XE0 Datasheet enДокумент3 страницы6GK74435DX040XE0 Datasheet enLuis CortezОценок пока нет
- Hướng Dẫn Chấm: Ngày thi: 27 tháng 7 năm 2019 Thời gian làm bài: 180 phút (không kể thời gian giao đề) HDC gồm có 4 trangДокумент4 страницыHướng Dẫn Chấm: Ngày thi: 27 tháng 7 năm 2019 Thời gian làm bài: 180 phút (không kể thời gian giao đề) HDC gồm có 4 trangHưng Quân VõОценок пока нет
- Peer PressureДокумент13 страницPeer PressuremightymarcОценок пока нет
- Canoe Matlab 001Документ58 страницCanoe Matlab 001Coolboy RoadsterОценок пока нет
- Cisco BGP ASPATH FilterДокумент115 страницCisco BGP ASPATH FilterHalison SantosОценок пока нет
- WBДокумент59 страницWBsahil.singhОценок пока нет
- An Evaluation of MGNREGA in SikkimДокумент7 страницAn Evaluation of MGNREGA in SikkimBittu SubbaОценок пока нет
- Chapter 2Документ13 страницChapter 2Kumkumo Kussia KossaОценок пока нет
- Congenital Cardiac Disease: A Guide To Evaluation, Treatment and Anesthetic ManagementДокумент87 страницCongenital Cardiac Disease: A Guide To Evaluation, Treatment and Anesthetic ManagementJZОценок пока нет
- Recitation Math 001 - Term 221 (26166)Документ36 страницRecitation Math 001 - Term 221 (26166)Ma NaОценок пока нет
- Economic Review English 17-18Документ239 страницEconomic Review English 17-18Shashank SinghОценок пока нет
- LSCM Course OutlineДокумент13 страницLSCM Course OutlineDeep SachetiОценок пока нет
- Canon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFДокумент13 страницCanon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFRita CaselliОценок пока нет
- Kyle Pape - Between Queer Theory and Native Studies, A Potential For CollaborationДокумент16 страницKyle Pape - Between Queer Theory and Native Studies, A Potential For CollaborationRafael Alarcón Vidal100% (1)
- Ccoli: Bra Ica Ol A LДокумент3 страницыCcoli: Bra Ica Ol A LsychaitanyaОценок пока нет
- Sample - SOFTWARE REQUIREMENT SPECIFICATIONДокумент20 страницSample - SOFTWARE REQUIREMENT SPECIFICATIONMandula AbeyrathnaОценок пока нет
- Quiz 140322224412 Phpapp02Документ26 страницQuiz 140322224412 Phpapp02Muhammad Mubeen Iqbal PuriОценок пока нет
- Case CapsuleДокумент8 страницCase CapsuleLiza BulsaraОценок пока нет
- ASHRAE Journal - Absorption RefrigerationДокумент11 страницASHRAE Journal - Absorption Refrigerationhonisme0% (1)
- Apron CapacityДокумент10 страницApron CapacityMuchammad Ulil AidiОценок пока нет
- PDF Chapter 5 The Expenditure Cycle Part I Summary - CompressДокумент5 страницPDF Chapter 5 The Expenditure Cycle Part I Summary - CompressCassiopeia Cashmere GodheidОценок пока нет
- Quarter 1-Week 2 - Day 2.revisedДокумент4 страницыQuarter 1-Week 2 - Day 2.revisedJigz FamulaganОценок пока нет