Академический Документы
Профессиональный Документы
Культура Документы
Preeclampsia in Low and Middle Income Countries-Health Services Lessons Learned From The PRE-EMPT (PRE-Eclampsia-Eclampsia Monitoring, Prevention & Treatment) Project
Загружено:
RezaTiansahОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Preeclampsia in Low and Middle Income Countries-Health Services Lessons Learned From The PRE-EMPT (PRE-Eclampsia-Eclampsia Monitoring, Prevention & Treatment) Project
Загружено:
RezaTiansahАвторское право:
Доступные форматы
Womens Health
Preeclampsia in Low and Middle Income
CountriesHealth Services Lessons Learned
From the PRE-EMPT (PRE-EclampsiaEclampsia
Monitoring, Prevention & Treatment) Project
Peter von Dadelszen, MBChB, DPhil,1,2 Tabassum Firoz, MD,2,3
France Donnay, MD, MPH, FACOG, FRCOG,4 Rebecca Gordon, BSc,1,2
G. Justus Hofmeyr, FRCOG,5 Shifana Lalani, MSc,1 Beth A. Payne, BSc,1,2
James M. Roberts, MD,6 Katherine C. Teela, MHS,4 Marianne Vidler, MPH,1,2
Diane Sawchuck, RN, PhD,1,2 Laura A. Magee, MD, MSc1,2,3
1
Department of Obstetrics and Gynaecology, University of British Columbia, Vancouver BC
2
Child and Family Research Institute Reproduction and Healthy Pregnancy Cluster, Vancouver BC
3
Department of Medicine, University of British Columbia, Vancouver BC
4
Maternal Health, Family Health Department, Bill & Melinda Gates Foundation, Seattle WA
5
Department of Obstetrics and Gynaecology, Walter Sisulu University, East London, South Africa
6
Magee-Womens Research Institute, University of Pittsburgh, Pittsburgh PA
Abstract Rsum
The hypertensive disorders of pregnancy, in particular Les troubles hypertensifs de la grossesse, particulirement la
preeclampsia, matter because adverse events occur in women prclampsie, ont de limportance puisque des vnements
with preeclampsia and, to a lesser extent, in women with the indsirables se manifestent chez des femmes prsentant une
other hypertensive disorders. These adverse events are maternal, prclampsie et, dans une moindre mesure, chez des femmes
perinatal, and neonatal and can alter the life trajectory of each prsentant dautres troubles hypertensifs. Ces vnements
individual, should that life not be ended by complications. In this indsirables sont de nature maternelle, prinatale et nonatale,
review we discuss a number of priorities and dilemmas that we et peuvent modifier la vie des personnes qui les connaissent,
perceive to be facing health services in low and middle income lorsque celles-ci survivent aux complications. Dans cette analyse,
countries as they try to prioritize interventions to reduce the health nous discutons dun nombre de priorits et de dilemmes auxquels
burden related to preeclampsia. These priorities and dilemmas doivent faire face les services de sant des pays revenu faible
relate to calcium for preeclampsia prevention, risk stratification, ou moyen au moment de tenter de hirarchiser les interventions
antihypertensive and magnesium sulphate therapy, and mobile en vue dattnuer le fardeau de sant li la prclampsie. Ces
health. Significant progress has been and is being made to reduce priorits et ces dilemmes sont lis ladministration de calcium
the impact of preeclampsia in low and middle income countries, aux fins de la prvention de la prclampsie, la stratification
but it remains a priority focus as we attempt to achieve Millennium du risque, aux traitements aux antihypertenseurs et au sulfate
Development Goal 5. de magnsium, et la sant mobile. Bien que des progrs
significatifs aient t raliss et continuent dtre raliss en vue
dattnuer les effets de la prclampsie au sein des pays revenu
faible ou moyen, cette problmatique demeure une priorit dans le
cadre de nos tentatives datteindre lobjectif 5 du Millnaire pour le
dveloppement.
Key Words: Preeclampsia, hypertensive disorders of pregnancy,
global health
Competing Interests: None declared.
Received on July 12, 2012
Accepted on July 18, 2012
J Obstet Gynaecol Can 2012;34(10):917926
OCTOBER JOGC OCTOBRE 2012 l 917
Womens Health
BACKGROUND related outcomes may be to enhance the availability of life-
saving interventions in the communities in which vulnerable
P reeclampsia, although commonly defined by the
presence of both significant hypertension and heavy
proteinuria, is a pregnancy- and placenta-specific form
women reside. Such interventions may vary from improving
the status of pregnant women and facilitating timely decision-
making when complications arise, to initiating life-saving
of systemic inflammation with multiple target organs therapies (e.g., magnesium sulphate and antihypertensive
(Figure).1 As far as we can determine, preeclampsia and agents) prior to urgent transfer to an effective and adequately
eclampsia claim the lives of approximately 72000 women resourced emergency obstetric care facility.
and 500000 fetuses and newborns each yeara loss of
almost 1600 lives per day.2 Over 99% of these losses occur In 2011, the University of British Columbia was awarded
in low and middle income countries, particularly in sub- the four-year PRE-eclampsiaEclampsia Monitoring,
Saharan Africa and on the Indian subcontinent.2 In the Prevention & Treatment project grant by the Bill & Melinda
Americas, preeclampsia and eclampsia are the leading Gates Foundation. The overarching theme of this proposal
cause of direct maternal mortality.35 is reducing the maternal and perinatal consequences of
preeclampsia. Through this grant we aim to determine the
Currently, the singular way to initiate resolution of the impact of this program of research on those outcomes.
maternal syndrome of preeclampsia is to deliver the placenta.1
However, the maternal syndrome of preeclampsia may The primary objectives of PRE-EMPT are three community-
present de novo postpartum and, especially with early-onset level and primary health centre-level intervention studies
preeclampsia, cause transient postpartum deterioration.1 tailored to LMIC settings and related to prevention,
Therefore, even timely delivery does not necessarily avoid monitoring, and treatment. The secondary objectives are
all end-organ complications of the disorder. In addition, 1. developing a multifaceted international research
the life-altering and life-threatening complications (e.g., collaboration, and
stroke, acute renal failure, eclampsia, pulmonary edema, and
placental abruption) probably increase the significant health 2. LMIC-oriented preeclampsia knowledge translation
burden of preeclampsia by at least five-fold.6,7 activities.
As a group, we believe that the global community (clinicians, We describe here examples of what we have learned to
researchers, policy makers, governments, health authorities, date from these objectives, and the implications derived
and other stakeholders) should focus efforts on reducing from our current position for health service decision-
the excess number of adverse maternal and perinatal making, especially in resource-challenged settings.
events in women whose pregnancies are complicated by
preeclampsia, rather than focus solely on the surrogate of PREVENTION
these risks, the diagnosis of preeclampsia. Calcium Supplementation to Reduce the
Given that preeclampsia-related maternal and perinatal Incidence of Preeclampsia: Should We Provide
deaths and permanent sequelae result primarily from delays This to High-Risk Women? If Yes, at What Dose?
in diagnosis, triage, transport, and treatment,2 an important In general, preeclampsia is considerably more prevalent
direction for new initiatives related to improving preeclampsia- in low and middle income communities than in affluent
communities.8 Two striking exceptions have been identified
in Ethiopia and in the Mayan Indians of Guatemala,
ABBREVIATIONS where diets contain high levels of calcium.9,10 Subsequent
AUC ROC area under the receiver-operator characteristic curve epidemiological, clinical, and laboratory studies linking
BP blood pressure preeclampsia to calcium deficiency have been outlined in
EPIC European Prospective Investigation into Cancer and a recent systematic review of calcium supplementation
Nutrition study during pregnancy.11 The conclusion of this systematic
HR hazard ratio review, and that of a parallel meta-analysis,12 was that
LMIC low and middle income countries supplemental calcium (at least 1g daily) from mid-
MDG Millennium Development Goal pregnancy is associated with a modest reduction in rates
PIERS Pre-eclampsia Integrated Estimate of RiSk of preeclampsia, and a more notable reduction in its severe
PRE-EMPT Pre-eclampsiaEclampsia Monitoring, Prevention & manifestations, particularly among women at increased
Treatment risk or with low dietary calcium intake. However, we have
RDA recommended daily allowance found no report of randomized controlled trials of calcium
RR relative risk supplementation commenced before pregnancy.
918 l OCTOBER JOGC OCTOBRE 2012
Preeclampsia in Low and Middle Income CountriesHealth Services Lessons Learned From the PRE-EMPT Project
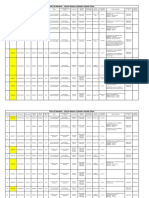
The origins and consequences of preeclampsia
immunological factors decidual immune cell - normal placentation
antigen exposure EVT interactions (late-onset preeclampsia)
primigravidity ( ) / primipaternity ( ) macrosomia
donor gamete(s) ( ) (invasion & uteroplacental multiple pregnancy
duration of cohabitation ( ) artery remodelling) lowered threshold
barrier contraception ( ) / fellatio ( )
prior miscarriage ( )
smoking ( )
inadequate placentation
(early-onset preeclampsia)
genetic factors
familial risks
SNPs uteroplacental mismatch
epigenetics
placental IUGR
intervillous soup ( maternal syndrome)
lowered threshold pre-eclampsia-specific shared with IUGR
metabolic syndrome placental debris angiogenic imbalance
chronic infection / inflammation innate immune activation
pre-existing hypertension oxidative stress
chronic renal disease / DbM eicosanoids
high altitude cytokines
endothelial cell activation
cardiorespiratory CNS renal hepatic hematological
hypertension eclampsia glomerular endotheliosis periportal inflammation microangiopathic hemolysis
ARDS TIA / RIND / CVA proteinuria hepatic dysfunction / failure thrombocytopenia
pulmonary edema PRES ATN hepatic hematoma / rupture DIC
cardiomyopathy / LV dysfunction ARF
intravascular volume constriction
generalised edema
maternal syndrome
In this model of the origins of preeclampsia, we describe preeclampsia that arises primarily because of imperfect placentation (early-onset or placental
preeclampsia) and that arises because of either a lowered maternal threshold or excessive physiological placentation (late-onset or maternal preeclampsia).
Some aspects of the preeclampsia process are specific to it, while others are shared with normotensive intrauterine growth restriction. A lowered maternal threshold
may influence the development of early-onset preeclampsia as well through direct endothelial cell activation. The consequences of the endothelial cell activation
that appears consistent between all women who develop preeclampsia include a variable impact on multiple vulnerable organ systems. Disease severity generally
correlates with the degree and number of organ dysfunctions.
: increased risk of preeclampsia; : decreased risk of preeclampsia; EVT: extravillous trophoblasts; SNP: single nucleotide polymorphism; IUGR: intrauterine
growth restriction; DbM: diabetes mellitus; ARDS: acute respiratory distress syndrome; LV: left ventricular; TIA: transient ischemic attack; RIND: reversible ischemic
neurological deficit; CVA: cerebrovascular accident; PRES: posterior reversible encephalopathy syndrome; ATN: acute tubular necrosis; ARF: acute renal failure;
DIC: disseminated intravascular coagulation
Hofmeyr and colleagues conducted an RCT nested within childhood hypertension in the children of participants in
the large World Health Organization trial of calcium RCTs of calcium supplementation.11
supplementation (1.5g daily from at least 20 weeks gestation)
in pregnant women with low dietary calcium intake13; this The fact that calcium supplementation reduces the
failed to demonstrate an effect of calcium supplementation incidence of preeclampsia without evidence of an effect on
on biochemical measures commonly elevated in preeclampsia proteinuria (but possibly an effect on heavy proteinuria by
(serum urate, platelet count, and urine protein/creatinine reducing glomerular tuft arterial pressure, once glomerular
ratio). The lack of effect on proteinuria is consistent with endothelial integrity has been lost) and other markers for
the findings of the main WHO trial, in which there was preeclampsia seems contradictory. To reconcile this, we
a trend towards a reduced risk of preeclampsia (RR 0.92; agree with the hypothesis that calcium supplementation in
95% CI 0.75 to 1.13) and severe preeclampsia (RR 0.74; the second half of pregnancy reduces blood pressure, and
95% CI 0.48 to 1.15), but no reduction in proteinuria therefore reduces the diagnosis of both preeclampsia
(RR 1.01; 95% CI 0.88 to 1.15).14 Tentative evidence for an and severe preeclampsia without having a significant
effect on the offspring is the finding of reduced rates of effect on the underlying pathology.15
OCTOBER JOGC OCTOBRE 2012 l 919
Womens Health
This may also explain an anomaly identified in the Calcium: Dietary Replacement Versus
systematic review.11 The incidence of preeclampsia Dietary Supplementation
(defined as proteinuric gestational hypertension [blood It appears that dosing studies on calcium replacement
pressure 140/90mmHg]) was reduced overall by or supplementation are required. The current WHO
55% (RR 0.45, 95% CI 0.31 to 0.65) and the composite recommendation, derived from meta-analyses, suggests
outcome maternal death or severe morbidity was a dose of 1.5g to 2g calcium/day,20 which is 30% to
reduced by 20% (RR 0.80; 95% CI 0.65 to 0.97). 80% greater than the recommended daily allowance of
The observed reduction in maternal death or severe 1200mg,21 in addition to current dietary intake. The study
morbidity includes severe hypertension, the outcome of dietary calcium intake in primiparous women cited
that is likely to be modified by the antihypertensive effect above showed a median daily dietary calcium intake of
of calcium. However, the risk of HELLP syndrome approximately 600mg.22 The recommended calcium dose
was increased 2.7-fold with calcium supplementation for supplementation during pregnancy has significant cost
(RR 2.67; 95% CI 1.05 to 6.82). implications. Ministries of health must consider cost
benefit ratios in their decisions to scale up interventions
We believe that these considerations should lead to that may affect health outcomes, and often need to
reflection prior to the programmatic introduction of justify their decisions to ministries of finance within their
calcium supplementation to pregnant women in low intake respective regional and federal governments. Without
areas. There are four main reasons to pause and reflect. substantive evaluation of the costbenefit equation for the
The first is the possible risk associated with calcium higher doses, especially in the absence of calcium dosing
supplementation, which should be balanced against the studies, many countries will be hesitant to scale up this
probable benefit; the second is the issue of calcium dose; recommendation.
the third is the timing of the intervention; and the fourth
is the issue of mineral balance. Furthermore, in a placebo-controlled calcium supple
mentation in pregnant women in The Gambia, women
Calcium: Balancing Potential Risks receiving calcium (1500g/day) had significantly lower hip,
Against Probable Benefit lumbar spine and distal radial lower bone mineral content,
While reducing the incidence of the diagnosis of bone area and bone mineral density throughout lactation
preeclampsia through its antihypertensive effect, calcium than women who received placebo.23 The authors surmise
supplementation may mask, without altering, the underlying that such levels of calcium supplementation in pregnant
pathology of preeclampsia.15 Consequently, we suggest women may disrupt metabolic adaptation to pregnancy
that any program of calcium supplementation introduced and alter bone health.
with the intent of reducing the burden of preeclampsia in
For women in LMICs, dietary replacement with 500mg
a given jurisdiction should be monitored until it is clear that
calcium/day would achieve a median daily intake of
the rate of adverse outcomes (maternal and perinatal severe
approximately 1100mg22; this could be achieved with
morbidity and mortality) actually falls, rather than increases.
food fortification, and represents the difference in daily
This is particularly relevant in view of the recent findings of
calcium intake between high income and low income
the EPIC-Heidelberg observational cohort study that, after
countries. Higher levels of true supplementation to
an average follow-up time of 11 years, having a moderate
1.5g/day to 2.0g/day are unacceptable to the palate,
total dietary and dairy calcium intake significantly reduced
are greater than RDA amounts, and are of significant
the risk of developing a myocardial infarction (HR 0.69;
programmatic cost.
95% CI 0.50 to 0.94 and HR 0.68; 95% CI 0.50 to 0.93,
respectively).16 Overall, associations between calcium intake Calcium: Timing the Intervention
and stroke risk or cardiovascular disease mortality were not Another issue requiring explanation is the modest effect
found. Users of supplements that included calcium had a of calcium supplementation on preeclampsia in contrast to
significantly higher risk of myocardial infarction (HR 1.86; the striking epidemiological differences in populations with
95% CI 1.17 to 2.96) than non-users of any supplements, good and poor dietary calcium. It is possible that calcium
and the risk was more pronounced for users of calcium supplementation in the second half of pregnancy is too late
supplements only (HR 2.39; 95% CI 1.12 to 5.12). This to influence the underlying processes of preeclampsia.15 For
parallels the evidence for a benefit from antioxidants in example, inadequate placentation occurs in early pregnancy1
the prevention of preeclampsia; a diet rich in antioxidants and would not be influenced by an intervention in the
appears to protect against preeclampsia,17,18 whereas the second half of pregnancy. While deficient dietary calcium
ingestion of isolated vitamins C and E does not.19 before and during early pregnancy may increase the risk for
920 l OCTOBER JOGC OCTOBRE 2012
Preeclampsia in Low and Middle Income CountriesHealth Services Lessons Learned From the PRE-EMPT Project
preeclampsia, there may be limited potential to reverse this resource setting, we repeated this exercise across British
effect by calcium supplementation later in the pregnancy. Columbia, with the addition of specific advice about items
of drug and fluid management, and observed a more
Therefore, in response to both the dose and timing than 30% reduction in the incidence of adverse maternal
issues, the Calcium And Pregnancy RCT is testing the outcomes across the province after a process of active
hypothesis that 500mg of calcium replacement daily (to guideline implementation.29 This latter effect was seen
the RDA), begun before pregnancy in women at high risk most in smaller units where day-to-day exposure to women
of preeclampsia or eclampsia, will reduce the incidence with preeclampsia, especially complicated preeclampsia, is
of hypertension and other pregnancy outcomes more infrequent. We presumed that the effect in smaller units
effectively than supplementation of 1.5g/day to 2.0g/day was achieved by increasing in-house competence and care
once pregnancy is diagnosed as currently recommended by provider confidence in those units.
the WHO.20 This RCT is currently recruiting women with
low calcium intake in South Africa and Zimbabwe, and, In LMICs, pregnant women often rely on community
with supplemental funding from the WHO, will recruit health professionals, many of whom have under 12 months
in Argentina. In this trial women will be randomized to training, to facilitate antenatal and maternity care. These
calcium or placebo from pre-pregnancy until 20 weeks pregnant women are often concentrated in rural areas with
gestation, after which time all women will receive open inadequate access to comprehensive emergency obstetric
label calcium (1500mg/d) to supplement calcium intake care. Therefore, to achieve reductions in adverse outcomes
to WHO-recommended amounts.24 similar to those observed in British Columbia, one must
consider cost-effective health care delivery options that
Calcium: Mineral Balance
will increase the skill level and confidence of community
Another explanation for the apparent paradox of the
health professionals. Following extensive inquiry, we
modest effect of calcium supplementation on preeclampsia,
believe that mobile health (mHealth) technologies have
in contrast to the striking epidemiological differences
the capacity to strengthen the ability of community-
in populations with good and poor dietary calcium, is
level health professionals to provide evidence-based care
the difference in mineral balance between dietary and
(decision-making and initiation of therapies) in a timely
supplemental calcium intake. As noted in the EPIC-
fashion and within the household or primary health clinic
Heidelberg study, dietary calcium intake appears beneficial
prior to transport.
in terms of cardiovascular health, whereas supplements do
not.16 It is possible that the balance of minerals (calcium, The WHO defines mHealth as mobile technologies
potassium, and magnesium, in particular) obtained as well as advancements in their innovative application
through diet provides health benefits not matched by to address health priorities.30 The mobile phone has
calcium supplements alone.2527 Other micronutrients (and become a novel tool to address public health challenges
their balance) present in dairy foods may be important in and shift the paradigm of health care access and delivery
modulating the consistently observed benefit of adequate from traditional facility-based care to community care.
calcium intake.27 The United Nations Millennium Development Goal 8,
specifically 8F, calls for the benefits of new technology,
MONITORING particularly information technology, to be made available
by increasing the number of mobile phone subscribers.31
Once a woman has developed preeclampsia or another
hypertensive disorder of pregnancy, can her risks be In 2010, a consortium of international groups called for
further stratified? We believe that they can. the use of mobile phones to reduce maternal mortality and
achieve MDG 5 by 2015.32 Mobile phones have been used
An initial step towards improved, streamlined, and effectively in a number of capacities for advancing maternal
evidence-based monitoring of women with preeclampsia is health, including data collection and management, point
to standardize care, including initial clinical and laboratory of care diagnostics and support, capacity strengthening,
assessment and ongoing surveillance. At the BC Womens health promotion, text messaging of prenatal education,
Hospital and Health Centre we achieved a greater than automated prenatal care appointment reminders, and
80% reduction in the incidence of a combined adverse access to emergency obstetric care.33
maternal outcome simply by standardizing assessment and
surveillance of women admitted with either gestational To provide such an mHealth platform, it is important to
hypertension or gestational proteinuria.28 To test this develop decision-making tools that can be integrated into
experience beyond a single tertiary centre in a high a mobile platform, such as a mobile phone, so that clinical
OCTOBER JOGC OCTOBRE 2012 l 921
Womens Health
variables (e.g., symptoms and easily observed signs) can application, with the results of the miniPIERS model
be entered and evidence-based, standardized therapeutic guiding care within the context of a planned cluster
advice generated automatically using the software capacity randomized control trial of community level, community
of the mobile device. An example is the phone oximeter, health worker-administered, interventions for preeclampsia
described below. that will recruit women in South Asia and sub-Saharan
Africa. Funding for the Community-Level Interventions
Over the past decade, we have been developing and for Pre-eclampsia trial will be obtained from PRE-EMPT.
validating two risk stratification models to be used in
women with clinical preeclampsia (i.e., time of disease, The second purpose will be to incorporate the phone
rather than prediction of disease)the Pre-eclampsia oximeter, a mobile phone-supported pulse oximeter,
Integrated Estimate of RiSk models.28,3445 The two models into a user-friendly application to guide care, as well as to
are fullPIERS (based on symptoms, signs, and laboratory recalibrate the miniPIERS model to include SpO2.48 Again,
tests)34 and miniPIERS (based on symptoms and signs).46 we envisage an mHealth application that will both stratify
Development and internal validation of fullPIERS has been risk and support clinical decision-making, building care
funded by the Canadian Institutes for Health Research, provider confidence through integral decision trees that
and miniPIERS development and full validation by the reflect best evidence-based practice and the current WHO
PRE-EMPT grant, the WHO, and Canadian Institutes of recommendations.20
Health Research.
Monitoring: Removing the Primacy of Proteinuria
In the fullPIERS data set (using data from tertiary centres in in Risk Stratification in High Resource Settings
Canada, New Zealand, Australia, and the United Kingdom), It is a historical accident that proteinuria has achieved a
we were able to identify women with preeclampsia who preeminent role in the diagnosis and ongoing surveillance
are at increased risk of maternal complications, and we of women with preeclampsia. While significant proteinuria
have been able to grade this risk.34 With 2023 women in (i.e., 300mg/24h, 30mg protein/mmol creatinine on
the fullPIERS database, the AUC ROC is 0.88 (95% CI a random urine collection, or ++ protein by urinary
0.84 to 0.92), and stratification capacity is robust. The dipstick) is central to all diagnostic criteria, the presence
independent predictors of adverse maternal outcome are of hyperuricemia, for example, is as effective for perinatal
gestational age at eligibility, chest pain/dyspnea, SpO2, risk stratification as proteinuria.49 However, there is no
serum creatinine, serum AST, and platelet count. The clear gold standard for the assessment of proteinuria in
fullPIERS model assesses risk up to seven days after pregnancy. Through the PIERS project, we have determined
eligibility (AUC ROC 0.76; 95% CI 0.72 to 0.80). The that 24-hour urine collections are vulnerable to both over-
fullPIERS model requires external validation before it can and under-collection approximately one half of the time,
be advocated for use outside research settings, and will be with under- and over-collection being equally common.50
applicable only to facilities with full laboratory support. Similarly, we have identified that the method of protein
A powerful component of the fullPIERS model is pulse measurement may alter the quantification performance of
oximetry, which has independent power to identify women proteinuria and albuminuria estimations in dilute urine,51,52
at risk of adverse outcomes of preeclampsia, including which may explain some of the uncertainties that derive
non-cardiorespiratory outcomes.39 from the literature, especially for albumin/creatinine ratios.53
The final analytical stages of developing and validating Once significant proteinuria (however defined) has been
the miniPIERS model are currently being completed. observed, is there any further benefit to be derived from
The model will use data derived from women with any ongoing risk stratification including proteinuria? In high
hypertensive disorder of pregnancy within 24 hours of resource settings, we have determined that all three methods
admission to academic centres in Brazil, Fiji, Pakistan, of proteinuria estimation perform as well (or as poorly) as
South Africa, and Uganda, and will be based on gestational each other, and none of them have adequate stratification
age, parity, symptoms, and signs.47 capacity to be used to guide clinical decision-making.54 In
the fullPIERS model, measures of proteinuria estimation
Once the miniPIERS model has been validated we will were displaced from the model by serum creatininean
transfer the model to an mHealth platform as a mobile observation made previously by Lindheimer and Kanter,
phone application, using funding from Saving Lives at as rising serum creatinine is more proximate to the
Birth and the PRE-EMPT award. This application, PIERS occurrence of an adverse outcome than is the degree of
on the Move, will be developed initially for two purposes. proteinuria.55 The level of dipstick proteinuria will not be a
The first will be to host miniPIERS on a mobile phone necessary component of the miniPIERS model.
922 l OCTOBER JOGC OCTOBRE 2012
Preeclampsia in Low and Middle Income CountriesHealth Services Lessons Learned From the PRE-EMPT Project
TREATMENT eclampsia), as well as for sexually transmitted infections and
HIV.66 In theory, medicines on this list should be available
Overcoming the Reductionist View of the within functioning health systems at all times, in adequate
Management of Severe Pregnancy Hypertension amounts, in the appropriate dosage forms, with assured
While eclampsia is the most commonly recognized and quality and adequate information, and at a price that the
visible cause of death associated with preeclampsia, the individual and the community can afford. Although the
specific causes of death for women with preeclampsia reality in each LMIC may be different, the Priority Medicines
or eclampsia in LMIC have not been well studied. for Mothers and Children is designed to be an advocacy tool.
Although the prevalence and burden of illness of severe
hypertension of preeclampsia or eclampsia is not accurately The current Priority Medicines for Mothers and Children lists only
documented in LMIC, data from well-resourced settings magnesium sulphate (and calcium gluconate for treatment of
indicate that failure to treat sustained severe hypertension magnesium toxicity) as a priority medicine for management
adequately is an important contributor to maternal of severe preeclampsia or eclampsia.66 The presence of
mortality in preeclampsia or eclampsia.5658 These findings magnesium sulphate on the list is entirely appropriate,
are supplemented by the institutional data that contribute because it reduces, by at least 50%, both the incidence and
to the Fourth Report on Confidential Enquiries into Maternal recurrence of eclampsia; in addition, it probably reduces
Deaths in South Africa, in which 45% of maternal deaths maternal mortality.6973 However, magnesium sulphate is
attributed to preeclampsia were secondary to cerebral not an effective antihypertensive agent.74 There is limited
complications other than eclampsia.59 observational evidence describing no or transient decreases
in BP; a transient decrease in BP may occur 30 minutes after
Severe hypertension is defined as a systolic blood pressure the administration of 2g to 5g of magnesium sulphate, but
160mmHg and/or a diastolic BP 110mmHg.60 The sustained reductions in BP cannot be expected.75
Confidential Enquiries into Maternal Deaths in the United
Kingdom have shown that failure to initiate effective However, as there have been no RCTs of antihypertensive
antihypertensive therapy for sustained severe hypertension therapy for severe pregnancy hypertension, some have
was the most common source of substandard care in the viewed this absence of RCT evidence as a lack of
management of women with preeclampsia or eclampsia.56,57 evidence. This apparently reductionist view (that no RCT
In the recent reports, the majority of women who died evidence equates to no evidence) may be the reason that
from preeclampsia had either intracerebral hemorrhage or antihypertensive agents have neither been prioritized in
cerebral infarction secondary to inadequately-controlled LMIC efforts in preeclampsia or eclampsia management
severe hypertension.56,57 Therefore, sustained severe nor included in the Priority Medicines for Mothers and Children,
maternal hypertension is considered an obstetric near and may have led to the avoidable burden of maternal
miss, a potentially lethal complication that women survive, mortality related to uncontrolled severe pregnancy
due either to excellent medical care or to chance alone.61 It is hypertension observed in the United Kingdom and
widely accepted in all international pregnancy hypertension elsewhere.5658
guidelines that women with severe hypertension are at
increased risk of stroke and other central nervous system Therefore, what medication should be selected as the
complications, and would therefore benefit from blood drug of choice for the treatment of severe pregnancy
pressure reduction.20,60,6265 The relevant WHO guidelines hypertension? Medications in the Priority Medicines for
rate as strong the recommendation to treat severe Mothers and Children are chosen on the principles of efficacy,
hypertension with antihypertensive therapy.20 safety, and familiarity at both the national and individual
prescriber level.66 There are a number of options for the
The Priority Medicines for Mothers and Children was published choice of antihypertensive agent. In RCTs, parenteral
in March 2011 by the WHO, United Nations Population labetalol, parenteral hydralazine, and oral nifedipine
Fund, and the United Nations Childrens Fund.66 The (intermediate-acting tablets or short-acting capsules)
New York Times has described Priority Medicines for Mothers have been evaluated most often. All are reasonable
and Children as the top 30 medicines to save mothers choices for lowering severely elevated BP. Hydralazine
and children.67 These medicines have been taken from may be associated with more maternal hypotension than
among the 350 medicines contained within the WHO the other agents.76 Labetalol is not listed in the WHO
Essential Medicines List.68 Priority Medicines specifically Essential Medicines List 68and may therefore not be widely
lists eight drugs for management of the three leading available, and prescribers may not be familiar with its use.
causes of maternal morbidity and mortality (postpartum Concurrent use of magnesium sulphate and nifedipine
hemorrhage, maternal sepsis, and preeclampsia/ may be associated with neuromuscular blockade; however,
OCTOBER JOGC OCTOBRE 2012 l 923
Womens Health
a retrospective cohort study and data synthesis found the We should not assume that preventing the diagnosis of
incidence to be <1%, and inadvertent magnesium toxicity preeclampsia will equate to reduced rates of adverse
can be treated effectively by calcium gluconate.77 Based on events. This underlies our hesitancy to recommend
this, several national guidelines have accepted that there programmatic implementation of non-dietary calcium
is no significant interaction.20,60,6375 Furthermore, the supplementation with the current level of knowledge.
American Society of Hypertension and WHO guidelines Resolving the unsettled questions related to the relationship
specifically state that there is no interaction between between calcium and preeclampsia is an urgent research
nifedipine and magnesium sulphate.20,63 priority. In the interim, it is incumbent on those initiating
programs of calcium supplementation to ensure that
Although nifedipine is not listed as an antihypertensive outcomes improve beyond reduction in the incidence of
agent in the Priority Medicines for Mothers and Children, it is the diagnosis of preeclampsia.
listed for the prevention of preterm birth.66 As nifedipine
is administered orally and there may be limited resources Risk stratification of women with preeclampsia is now
in LMIC for intravenous access, nifedipine may be an possible, so that maternal risks can be balanced against the
ideal medication for treatment of severe hypertension perinatal risks of prematurity, which are better known to
in pregnancy. Also, the oral administration of this caregivers. Importantly, we suggest that heavy proteinuria
medication opens up the possibility of administration in no longer be an indication to deliver a woman in the
the community setting. However, ultimately, the choice of absence of either a term pregnancy or other precipitants
an antihypertensive agent will depend upon the clinician, included in the PIERS models. Mobile health platforms
regional differences in practice, and availability. can deliver the PIERS models and PIERS-directed clinical
care algorithms into the hands of community health care
As we believe that the omission of antihypertensive therapy providers, to whom initiation of lifesaving therapies can be
for severe hypertension represented a missed opportunity shifted. Such mHealth platforms can be augmented through
to advocate for an affordable and effective intervention technology transfer into robust mobile applications, such
that may decrease maternal mortality and move us closer to as the mobile phone oximeter.
achieving MDG 5, we contacted the WHO Department of
Essential Medicines and Health Products. In response to We advocate that the management of severe pregnancy
our contact, we have received confirmation from Dr Clive hypertension is as important an intervention in women
Ondari, Team Coordinator, Medicine Access and Rational with preeclampsia as the RCT-supported use of magnesium
Use, Essential Medicines and Health Products, WHO that sulphate prevention and treatment of eclampsia. There
an antihypertensive for severe pregnancy hypertension will never be a randomized placebo-controlled trial of
(most logically nifedipine) will be added to the updated antihypertensives for this indication, nor should there be.
Priority Medicines for Mothers and Children in 2012. Preeclampsia is a multisystem disorder with a number
Once the issue of antihypertensive management for severe of biological pathways leading to the clinical syndrome
pregnancy hypertension has been accepted as a health that we recognize. It will be through multisystem
services priority, in addition to magnesium sulphate, the interventions (basic and clinical research methodologies,
question then is: at what level of the health system could clinical trials, implementation research, health services
and should life-saving therapy be initiated? planning, and programmatic scale-up) and multilevel
collaboration (women, their families and communities,
clinicians, researchers, policy makers, governments, health
CONCLUSION authorities, and other stakeholders) that we will reduce
The hypertensive disorders of pregnancy, in particular the unacceptable personal, family, community and societal
burden associated with preeclampsia.
preeclampsia, matter. They matter because adverse events
occur in women with preeclampsia and, to a lesser extent,
REFERENCES
the other hypertensive disorders. These adverse events
are maternal, perinatal, and neonatal, and can alter the life 1. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia.
trajectory of each individual, if that life is not cut short Lancet 2010;376:63144.
by complications. The majority of these complications 2. Firoz T, Sanghvi H, Merialdi M, von Dadelszen P. Pre-eclampsia in low
and middle income countries. Best Pract Res Clin Obstet Gynaecol
occur in LMICs. The PRE-EMPT project will attempt to 2011;25:53748.
address prevention, monitoring, and treatment through
3. Health Canada. Special report on maternal mortality and severe morbidity
three community-level and primary health centre-level in Canadaenhanced surveillance: the path to prevention. Ottawa:
intervention studies tailored to LMIC settings. Minister of Public Works and Government Services Canada; 2004.
924 l OCTOBER JOGC OCTOBRE 2012
Preeclampsia in Low and Middle Income CountriesHealth Services Lessons Learned From the PRE-EMPT Project
4. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. 23. Jarjou LM, Laskey MA, Sawo Y, Goldberg GR, Cole TJ, Prentice A. Effect
WHO analysis of causes of maternal death: a systematic review. of calcium supplementation in pregnancy on maternal bone outcomes in
Lancet 2006;367:106674. women with a low calcium intake. Am J Clin Nutr. 2010 Aug;92(2):4507.
5. US Department of Health and Human Services, Health Resources and 24. HofmeyrGJ, NovikovaN, SingataM, FawcusS, OyebajoA, MunjanjaS,
Services Administration. Womens Health USA 2011. Rockville, MD: et al. Protocol 11PRT/4028: Long term calcium supplementation in
US Department of Health and Human Services; 2011. women at high risk of pre-eclampsia: a randomised, placebo-controlled
trial (PACTR201105000267371). Available at: http://www.thelancet.com/
6. Kaye DK, Kakaire O, Osinde MO. Systematic review of the magnitude protocol-reviews/11PRT4028. Accessed August 15, 2012.
and case fatality ratio for severe maternal morbidity in sub-Saharan Africa
between 1995 and 2010. BMC Pregnancy Childbirth 2011;11:65. 25. Abbott RD, Curb JD, Rodriguez BL, Sharp DS, Burchfiel CM,
Yano K. Effect of dietary calcium and milk consumption on risk of
7. Tuncalp O, Hindin MJ, Souza JP, Chou D, Say L. The prevalence of thromboembolic stroke in older middle-aged men. The Honolulu Heart
maternal near miss: a systematic review. BJOG 2012;119:65361. Program. Stroke 1996;27:8138.
8. Langer A, Villar J, Tell K, Kim T, Kennedy S. Reducing eclampsia-related 26. Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA,
deathsa call to action. Lancet 2008;371:7056. et al. Prospective study of calcium, potassium, and magnesium intake and
risk of stroke in women. Stroke 1999;30:17729.
9. Belizn JM, Villar J. The relationship between calcium intake and edema-,
proteinuria, and hypertension-getosis: an hypothesis. Am J Clin Nutr 27. Massey LK. Dairy food consumption, blood pressure and stroke.
1980;33:220210. J Nutr 2001;131:18758.
10. Hamlin RH. The prevention of eclampsia and pre-eclampsia. 28. Menzies J, Magee LA, Li J, MacNab YC, Yin R, Stuart H, et al.;
Lancet 1952;1:648. Preeclampsia Integrated Estimate of RiSk (PIERS) Study Group.
Instituting surveillance guidelines and adverse outcomes in preeclampsia.
11. Hofmeyr GJ, Atallah AN, Duley L. Calcium supplementation during
Obstet Gynecol 2007;110:1217.
pregnancy for preventing hypertensive disorders and related problems.
Cochrane Database Syst Rev 2006;3:CD001059. 29. von Dadelszen P, Sawchuck D, McMaster R, Douglas MJ, Lee SK,
Saunders S, et al. The active implementation of pregnancy hypertension
12. Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, guidelines in British Columbia. Obstet Gynecol 2010;116:65966.
et al. Methods of prediction and prevention of pre-eclampsia: systematic
reviews of accuracy and effectiveness literature with economic modelling. 30. World Health Organization. mHealth: new horizons for health through
Health Technol Assess 2008;12(6):iiiiv, 1270. mobile technologies: based on the findings of the second global survey
on eHealth. Global observatory for eHealth series, vol 3. Geneva: WHO;
13. Hofmeyr GJ, Mlokoti Z, Nikodem VC, Mangesi L, Ferreira S, Singata M, 2011.
et al. Calcium supplementation during pregnancy for preventing
31. United Nations Statistics Division. Millennium Development
hypertensive disorders is not associated with changes in platelet count,
Goals indicators. New York: United Nations. Available at:
urate, and urinary protein: a randomized control trial. Hypertens
http://mdgs.un.org/unsd/mdg/default.aspx. Accessed April 4, 2012.
Pregnancy 2008;27:299304.
32. The Partnership for Maternal, Newborn and Child Health. International
14. Villar J, Abdel-Aleem H, Merialdi M, Mathai M, Ali M, Zavaleta
groups call for collaboration in use of mobile technology to reduce
N, et al.World Health Organization randomized trial of calcium
maternal and newborn mortality. Geneva: WHO; 2010. Available at:
supplementation among low calcium intake pregnant women. http://www.who.int/pmnch/media/press_materials/pr/2010/20100624_
Am J Obstet Gynecol 2006;194:63949. ict_use/en/index.html. Accessed April 10, 2012.
15. Hofmeyr GJ, Duley L, Atallah A. Dietary calcium supplementation for 33. Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in
prevention of pre-eclampsia and related problems: a systematic review maternal and newborn health programs and their outcomes around the
and commentary. BJOG 2007;114:93343. world. Matern Child Health J 2012;16:1092101.
16. Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium 34. von Dadelszen P, Payne B, Li J, Ansermino JM, Broughton PF,
intake and calcium supplementation with myocardial infarction and stroke Cote AM, et al. Prediction of adverse maternal outcomes in
risk and overall cardiovascular mortality in the Heidelberg cohort of the pre-eclampsia: development and validation of the fullPIERS model.
European Prospective Investigation into Cancer and Nutrition study Lancet 2011;377:21927.
(EPIC-Heidelberg). Heart 2012;98(12):9205.
35. Firoz T, Magee LA, Payne BA, Menzies JM, von Dadelszen P. The PIERS
17. Raijmakers MT, Dechend R, Poston L. Oxidative stress and preeclampsia: experience: research or quality improvement? J Obstet Gynaecol Can
rationale for antioxidant clinical trials. Hypertension 2004;44:37480. 2012;34:37981.
18. Poston L, Igosheva N, Mistry HD, Seed PT, Shennan AH, Rana S, et al. 36. Kozic JR, Benton SJ, Hutcheon JA, Payne BA, Magee LA,
Role of oxidative stress and antioxidant supplementation in pregnancy von Dadelszen P. Abnormal liver function tests as predictors of adverse
disorders. Am J Clin Nutr 2011;94(6 Suppl):1980S1985S. maternal outcomes in women with preeclampsia. J Obstet Gynaecol Can
19. Conde-Agudelo A, Romero R, Kusanovic JP, Hassan SS. 2011;33:9951004.
Supplementation with vitamins C and E during pregnancy for the 37. Laskin S, Payne B, Hutcheon JA, Qu Z, Douglas MJ, Ford J, et al.
prevention of preeclampsia and other adverse maternal and perinatal The role of platelet counts in the assessment of inpatient women with
outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol preeclampsia. J Obstet Gynaecol Can 2011;33:9008.
2011;204:50312. 38. Menzies J, Magee LA, MacNab YC, Ansermino JM, Li J, Douglas MJ,
20. World Health Organization. World Health Organization recommendations et al. Current CHS and NHBPEP criteria for severe preeclampsia do not
for prevention and treatment of pre-eclampsia and eclampsia. Geneva: uniformly predict adverse maternal or perinatal outcomes. Hypertens
World Health Organization; 2011. Pregnancy 2007;26:44762.
21. Institute of Medicine. Dietary reference intakes for calcium and vitamin 39. Millman AL, Payne B, Qu Z, Douglas MJ, Hutcheon JA, Lee T, et al.
D. Washington, DC: National Academy Press; 2010. Oxygen saturation as a predictor of adverse maternal outcomes in women
with preeclampsia. J Obstet Gynaecol Can 2011;33:70514.
22. Hofmeyr GJ, Mlokoti Z, Nikodem VC, Mangesi L, Ferreira S, Singata M,
et al.; WHO Calcium Supplementation for the Prevention of Pre- 40. Payne B, Magee LA, von Dadelszen P. Assessment, surveillance and
eclampsia Trial Group. Calcium supplementation during pregnancy prognosis in pre-eclampsia. Best Pract Res Clin Obstet Gynaecol
for preventing hypertensive disorders is not associated with changes in 2011;25:44962.
platelet count, urate, and urinary protein: a randomized control trial. 41. von Dadelszen P, Magee LA, Roberts JM. Subclassification of
Hypertens Pregnancy 2008;27:299304. preeclampsia. Hypertens Pregnancy 2003;22:1438.
OCTOBER JOGC OCTOBRE 2012 l 925
Womens Health
42. von Dadelszen P, Magee LA, Devarakonda RM, Hamilton T, 59. National Committee for the Confidential Enquiries into Maternal Deaths.
Ainsworth LM, Yin R, et al. The prediction of adverse maternal Saving mothers 20052007: fourth report on confidential enquiries
outcomes in preeclampsia. J Obstet Gynaecol Can 2004;26:8719. into maternal deaths in South Africa. Pretoria: National Department of
43. von Dadelszen P, Menzies J, Magee LA. The complications of Health; 2011.
hypertension in pregnancy. Minerva Med 2005;96:287302. 60. Magee LA, Helewa M, Moutquin JM, von Dadelszen P. Diagnosis,
44. von Dadelszen P, Menzies JM, Payne B, Magee LA. Predicting adverse evaluation, and management of the hypertensive disorders of pregnancy.
outcomes in women with severe pre-eclampsia. Semin Perinatol J Obstet Gynaecol Can 2008;30(3 Suppl):S1S48.
2009;33:1527. 61. Reichenheim ME, Zylbersztajn F, Moraes CL, Lobato G. Severe acute
45. Yen TW, Payne B, Qu Z, Hutcheon JA, Lee T, Magee LA, et al. Using obstetric morbidity (near-miss): a review of the relative use of its
clinical symptoms to predict adverse maternal and perinatal outcomes in diagnostic indicators. Arch Gynecol Obstet 2009;280:33743.
women with preeclampsia: data from the PIERS (Pre-eclampsia Integrated 62. Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin
Estimate of RiSk) study. J Obstet Gynaecol Can 2011;33:8039. JM. The classification and diagnosis of the hypertensive disorders
46. PRE-eclampsia Eclampsia Monitoring, Prevention & Treatment. The of pregnancy: statement from the International Society for the
miniPIERS (Pre-eclampsia Integrated Estimate of RiSk) model. Available Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy
at: http://pre-empt.cfri.ca/HOME.aspx. Accessed April 10, 2012. 2001;20(1):IXXIV.
47. Payne B, Hutcheon JA, Qu Z, Haniff F, Bhutta Z, Biryabarema C, et al. 63. Lindheimer MD, Taler SJ, Cunningham FG. ASH position paper:
MiniPIERS (Pre-eclampsia Integrated Estimate of RiSk): development hypertension in pregnancy. J Clin Hypertens (Greenwich) 2009;11:21425.
of a clinical prediction model for use in low and middle income countries
64. Lowe SA, Brown MA, Dekker G, Gatt S, McLintock C, McMahon L,
(LMICs) [abstract]. 18th World Congress of the International Society for
et al. Guidelines for the management of the hypertensive disorders of
the Study of Hypertension in Pregnancy, Geneva, Switzerland, July 2012.
pregnancy 2008. Society of Obstetric Medicine of Australia and New
Pregn Hypertens 2012;2(3):1956.
Zealand: 2008.
48. Saving Lives at Birth. PIERS on the move: Pre-eclampsia Integrated
65. Visintin C, Mugglestone MA, Almerie MQ, Nherera LM, James D,
Estimate of Risk assessment on a mobile phone. Available at:
Walkinshaw S; Guideline Development Group. Management of
http://savinglivesatbirth.net/summaries/37. Accessed April 10, 2012.
hypertensive disorders during pregnancy: summary of NICE guidance.
49. Roberts JM, Bodnar LM, Lain KY, Hubel CA, Markovic N, Ness RB, et al. BMJ 2010;341:c2207.
Uric acid is as important as proteinuria in identifying fetal risk in women
66. World Health Organization. Priority medicines for mothers and
with gestational hypertension. Hypertension 2005;46:12639.
children 2011. Geneva: WHO; March 2011. Available at:
50. Cote AM, Firoz T, Mattman A, Lam EM, von Dadelszen P, Magee LA. http://www.who.int/medicines/publications/A4prioritymedicines.pdf.
The 24-hour urine collection: gold standard or historical practice? Accessed April 10, 2012.
Am J Obstet Gynecol 2008;199:6256.
67. McNeil DG Jr. Treatments: WHO lists priority medicines for children and
51. De Silva DA, Halstead C, Cote AM, Sabr Y, von Dadelszen P, Magee
pregnant women. New York Times; March 28, 2011. Available at: http://
LA. Unexpected random urinary protein:creatinine ratio results
www.nytimes.com/2011/03/29/health/29global.html.
insights from clinician-laboratory medicine collaboration [abstract].
Accessed April 10, 2012.
18th World Congress of the International Society for the Study of
Hypertension in Pregnancy, Geneva, Switzerland, July 2012. Pregn 68. World Health Organization. WHO Model Lists of Essential Medicines.
Hypertens 2012;2:253. Geneva: WHO; March 2011. Available at: http://www.who.int/
medicines/publications/essentialmedicines/en. Accessed April 10, 2012.
52. De Silva DA, Halstead C, Cote AM, Sabr Y, von Dadelszen P,
Magee LA. Random urine albumin:creatinine ratio in high-risk 69. Duley L, Gulmezoglu AM, Henderson-Smart DJ, Chou D. Magnesium
pregnancyis it clinically useful? [abstract]. 18th World Congress of sulphate and other anticonvulsants for women with pre-eclampsia.
the International Society for the Study of Hypertension in Pregnancy, Cochrane Database Syst Rev 2010;(11):CD000025.
Geneva, Switzerland, July 2012. Pregn Hypertens 2012;2:25355. 70. Duley L, Henderson-Smart DJ, Walker GJ, Chou D. Magnesium
53. Cote AM, Brown MA, Lam E, von Dadelszen P, Firoz T, Liston RM, sulphate versus diazepam for eclampsia. Cochrane Database Syst Rev
et al. Diagnostic accuracy of urinary spot protein:creatinine ratio for 2010;(12):CD000127.
proteinuria in hypertensive pregnant women: systematic review. BMJ 71. Duley L, Henderson-Smart DJ, Chou D. Magnesium sulphate
2008;336:10036. versus phenytoin for eclampsia. Cochrane Database Syst Rev
54. Payne B, Magee LA, Cote AM, Hutcheon JA, Li J, Kyle PM, et al. PIERS 2010;(10):CD000128.
proteinuria: relationship with adverse maternal and perinatal outcome. 72. Duley L, Gulmezoglu AM, Chou D. Magnesium sulphate versus lytic
J Obstet Gynaecol Can 2011; 33:58897. cocktail for eclampsia. Cochrane Database Syst Rev 2010;(9):CD002960.
55. Lindheimer MD, Kanter D. Interpreting abnormal proteinuria in
73. Duley L, Matar HE, Almerie MQ, Hall DR. Alternative magnesium
pregnancy: the need for a more pathophysiological approach. Obstet
sulphate regimens for women with pre-eclampsia and eclampsia.
Gynecol 2010;115(2 Pt 1):36575.
Cochrane Database Syst Rev 2010;(8):CD007388.
56. Centre for Maternal and Child Enquiries. Saving mothers lives: reviewing
74. Magee LA, Abalos E, von Dadelszen P, Sibai B, Walkinshaw SA. Control
maternal deaths to make motherhood safer: 20062008. The eighth report
of hypertension in pregnancy. Curr Hypertens Rep 2009;11:42936.
on confidential enquiries into maternal deaths in the United Kingdom.
BJOG 2011;118(Suppl 1). 75. Mroczek WJ, Lee WR, Davidov ME. Effect of magnesium sulfate on
cardiovascular hemodynamics. Angiology 1977;28:7204.
57. Lewis G, ed. The Confidential Enquiry into Maternal and Child Health
(CEMACH). Saving mothers lives: reviewing maternal deaths to make 76. Magee LA, Cham C, Waterman EJ, Ohlsson A, von Dadelszen P.
motherhood safer20032005. The seventh report on confidential Hydralazine for treatment of severe hypertension in pregnancy: meta-
enquiries into maternal deaths in the United Kingdom. London: analysis. BMJ 2003;327:95560.
Confidential Enquiries into Maternal and Child Health; 2007. 77. Magee LA, Miremadi S, Li J, Cheng C, Ensom MH, Carleton B, et al.
58. Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Therapy with both magnesium sulfate and nifedipine does not increase
Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing the risk of serious magnesium-related maternal side effects in women with
on systolic blood pressure. Obstet Gynecol 2005;105:24654. preeclampsia. Am J Obstet Gynecol 2005;193:15363.
926 l OCTOBER JOGC OCTOBRE 2012
Вам также может понравиться
- Lubchenco Et Al 1963Документ10 страницLubchenco Et Al 1963RezaTiansahОценок пока нет
- GHFBB 7 055Документ8 страницGHFBB 7 055RezaTiansahОценок пока нет
- Prenatal 05 0041Документ13 страницPrenatal 05 0041herryОценок пока нет
- Management of Borderline Ovarian Tumours A Comprehensive Review of The LiteratureДокумент8 страницManagement of Borderline Ovarian Tumours A Comprehensive Review of The LiteratureRezaTiansahОценок пока нет
- BIEN 500 Systems Physiology for Biomedical Engineers: Hemostasis and Blood CoagulationДокумент16 страницBIEN 500 Systems Physiology for Biomedical Engineers: Hemostasis and Blood CoagulationRezaTiansahОценок пока нет
- Prevalence of Anticardiolipi PDFДокумент4 страницыPrevalence of Anticardiolipi PDFRezaTiansahОценок пока нет
- Fetomaternal Outcome in Acute Hepatitis EДокумент4 страницыFetomaternal Outcome in Acute Hepatitis ERezaTiansahОценок пока нет
- Low-Dose Calcium Supplementation ForДокумент7 страницLow-Dose Calcium Supplementation ForfaliamnisaОценок пока нет
- Correlation of Anticardiolipin Antibody Igm With First Trimester Recurrent AbortionsДокумент5 страницCorrelation of Anticardiolipin Antibody Igm With First Trimester Recurrent AbortionsRezaTiansahОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- CMC Ready ReckonerxlsxДокумент3 страницыCMC Ready ReckonerxlsxShalaniОценок пока нет
- Mtle - Hema 1Документ50 страницMtle - Hema 1Leogene Earl FranciaОценок пока нет
- FR Post-10Документ25 страницFR Post-10kulich545Оценок пока нет
- Catalogoclevite PDFДокумент6 страницCatalogoclevite PDFDomingo YañezОценок пока нет
- LM1011 Global ReverseLogДокумент4 страницыLM1011 Global ReverseLogJustinus HerdianОценок пока нет
- BPL Millipacs 2mm Hardmetrics RarДокумент3 страницыBPL Millipacs 2mm Hardmetrics RarGunter BragaОценок пока нет
- Inside Animator PDFДокумент484 страницыInside Animator PDFdonkey slapОценок пока нет
- Books of AccountsДокумент18 страницBooks of AccountsFrances Marie TemporalОценок пока нет
- Postgraduate Notes in OrthodonticsДокумент257 страницPostgraduate Notes in OrthodonticsSabrina Nitulescu100% (4)
- PROF ED 10-ACTIVITY #1 (Chapter 1)Документ4 страницыPROF ED 10-ACTIVITY #1 (Chapter 1)Nizelle Arevalo100% (1)
- SD8B 3 Part3Документ159 страницSD8B 3 Part3dan1_sbОценок пока нет
- Unit-1: Introduction: Question BankДокумент12 страницUnit-1: Introduction: Question BankAmit BharadwajОценок пока нет
- System: Boehringer Mannheim/Hitachi AnalysisДокумент20 страницSystem: Boehringer Mannheim/Hitachi Analysismaran.suguОценок пока нет
- Passenger E-Ticket: Booking DetailsДокумент1 страницаPassenger E-Ticket: Booking Detailsvarun.agarwalОценок пока нет
- GLF550 Normal ChecklistДокумент5 страницGLF550 Normal ChecklistPetar RadovićОценок пока нет
- Non Circumvention Non Disclosure Agreement (TERENCE) SGДокумент7 страницNon Circumvention Non Disclosure Agreement (TERENCE) SGLin ChrisОценок пока нет
- STAT100 Fall19 Test 2 ANSWERS Practice Problems PDFДокумент23 страницыSTAT100 Fall19 Test 2 ANSWERS Practice Problems PDFabutiОценок пока нет
- En dx300lc 5 Brochure PDFДокумент24 страницыEn dx300lc 5 Brochure PDFsaroniОценок пока нет
- Thin Film Deposition TechniquesДокумент20 страницThin Film Deposition TechniquesShayan Ahmad Khattak, BS Physics Student, UoPОценок пока нет
- Service and Maintenance Manual: Models 600A 600AJДокумент342 страницыService and Maintenance Manual: Models 600A 600AJHari Hara SuthanОценок пока нет
- National Standard Examination in Astronomy 2018-19 (NSEA) : Question Paper Code: A423Документ1 страницаNational Standard Examination in Astronomy 2018-19 (NSEA) : Question Paper Code: A423VASU JAINОценок пока нет
- Free Radical TheoryДокумент2 страницыFree Radical TheoryMIA ALVAREZОценок пока нет
- DNA Gel Electrophoresis Lab Solves MysteryДокумент8 страницDNA Gel Electrophoresis Lab Solves MysteryAmit KumarОценок пока нет
- FSRH Ukmec Summary September 2019Документ11 страницFSRH Ukmec Summary September 2019Kiran JayaprakashОценок пока нет
- Sri S T Kalairaj, Chairman: Income Tax TaxesДокумент3 страницыSri S T Kalairaj, Chairman: Income Tax TaxesvikramkkОценок пока нет
- 17BCE0552 Java DA1 PDFДокумент10 страниц17BCE0552 Java DA1 PDFABHIMAYU JENAОценок пока нет
- Kami Export - BuildingtheTranscontinentalRailroadWEBQUESTUsesQRCodes-1Документ3 страницыKami Export - BuildingtheTranscontinentalRailroadWEBQUESTUsesQRCodes-1Anna HattenОценок пока нет
- SQL Guide AdvancedДокумент26 страницSQL Guide AdvancedRustik2020Оценок пока нет
- DIN Flange Dimensions PDFДокумент1 страницаDIN Flange Dimensions PDFrasel.sheikh5000158Оценок пока нет
- Ir35 For Freelancers by YunojunoДокумент17 страницIr35 For Freelancers by YunojunoOlaf RazzoliОценок пока нет