Академический Документы
Профессиональный Документы
Культура Документы
Scandinavian Fellowship For Oral Pathology and Oral Medicine Guidelines For Oral Pathology and Oral Medicine in The Dental Curriculum.
Загружено:
desantosalbaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Scandinavian Fellowship For Oral Pathology and Oral Medicine Guidelines For Oral Pathology and Oral Medicine in The Dental Curriculum.
Загружено:
desantosalbaАвторское право:
Доступные форматы
European Journal of Dental Education ISSN 1396-5883
Scandinavian Fellowship for Oral Pathology and Oral
Medicine: guidelines for oral pathology and oral medicine in
the dental curriculum
C. Kragelund1, J. Reibel1, J. Hietanen2, E. Hadler-Olsen3, A. C. Johannessen4, B. Kenrad5, K. Nylander6,
M. Puranen7, T. Salo8, S. Syrjanen9, T. M. Sland10, I.van der Waal11, J. E.van der Wal12 and G.
Warfvinge13
1
Department of Oral Medicine, Section of Oral Pathology & Medicine, University of Copenhagen, Copenhagen, Denmark,
2
Department of Oral Pathology, University of Helsinki and HUSLAB, Helsinki, Finland,
3
Department of Medical Biology, University of Tromso, Tromso, Norway,
4
Section of Pathology, The Gade Institute, University of Bergen, Bergen, Norway,
5
Department of Oral Surgery & Oral Pathology, Aarhus University, Aarhus, Denmark,
6
Department of Medical Biosciences, Umea University, Umea, Sweden,
7
Oral and Maxillofacial Department, Kuopio University Hospital, Kuopio, Finland,
8
Department of Diagnostics & Oral Medicine, University of Oulu, Oulu, Finland,
9
Department of Oral Pathology & Oral Radiology, University of Turku, Turku, Finland,
10
Department of Oral Biology, University of Oslo, Oslo, Norway,
11
Department of Oral and Maxillofacial Surgery/Pathology, VU Medical Center/ACTA, Amsterdam, The Netherlands,
12
Department of Pathology, Martini Hospital/UMCG, Groningen, The Netherlands,
13
Department of Oral Pathology, Malmo University, Malmo and Karolinska Institute, Stockholm, Sweden
Keywords Abstract
dental curriculum; oral medicine; oral
pathology; Scandinavian Fellowship for Oral In Scandinavia, as in many European countries, most patients consult their general
Pathology and Oral Medicine. dentist once a year or more. This gives the dentist a unique opportunity and an obli-
gation to make an early diagnosis of oral diseases, which is beneficial for both the
Correspondence patient and the society. Thus, the dentist must have knowledge of clinical symptoms,
Gunnar Warfvinge local and systemic signs and clinical differential diagnoses to make an accurate diagno-
Department of Oral Pathology sis. The dentist must be competent in selecting appropriate diagnostic tests, for exam-
Faculty of Odontology, Malmo University ple, tissue biopsy and microbiological samples, and conducting them correctly, as well
SE 205 06 Malmo, Sweden as in interpreting test results and taking appropriate action accordingly. Furthermore,
Tel: +46 40 665 85 73 the dentist must be aware of diseases demanding multidisciplinary cooperation and be
Fax: +46 40 665 84 90 able to recognise his/her professional limitation, and to refer to other specialists when
e-mail: gunnar.warfvinge@mah.se required. The dental curriculum changes over time as new approaches, treatments and
diagnostic possibilities develop. Likewise, the role of the dentist in the community
Accepted: 16 April 2012 changes and may vary in different countries. As members of the Scandinavian Fellow-
ship for Oral Pathology and Oral Medicine and subject representatives of oral pathol-
doi: 10.1111/j.1600-0579.2012.00758.x
ogy and oral medicine, we feel obliged to contribute to the discussion of how the
guidelines of the dental curriculum support the highest possible standards of dental
education. This article is meant to delineate a reasonable standard of oral pathology
and oral medicine in the European dental curriculum and to guide subject representa-
tives in curriculum development and planning. We have created an advisory topic list
in oral pathology and oral medicine.
The Scandinavian Fellowship for Oral Pathology and Oral guidelines of the dental curriculum support the highest possible
Medicine (SFOPOM) was founded in 1972, and today, there standards of dental education. Recently, Scandinavian Fellow-
are fourteen SFOPOM-associated universities, all offering a ship for Oral Pathology and Oral Medicine: Statement on Oral
dental education. Pathology and Oral Medicine in the European Dental Curricu-
As subject representatives of oral pathology and oral medi- lum was published in the Journal of Oral Pathology & Medi-
cine, we feel obliged to contribute to the discussion of how the cine (1) as a comment to the Profile and Competences for the
2012 John Wiley & Sons A/S 1
Curriculum guidelines for oral pathology & medicine Kragelund et al.
European Dentist (PCD) from 2009 generated by the Associa- ferred teaching method will be proposed, we suggest that oral
tion for Dental Education in Europe (ADEE) and the thematic pathology and oral medicine are integrated whenever possible.
network DentEd, which is the latest step towards a European
Dental Curriculum (2).
The dental curriculum changes over time as new approaches,
The competences of the contemporary
Scandinavian/European dentist
treatments and diagnostic possibilities develop, but also, to
some extent, mirrors its social context. Likewise, the role of the In Scandinavia, as in many European countries, most patients
dentist in the community changes and may vary in different consult their general dentist once a year or more. This gives
countries. In response to these changes, several articles offering the dentist a unique opportunity and an obligation to make an
guidelines for oral pathology and oral medicine in the dental early diagnosis of oral diseases, which is beneficial for both the
curriculum have been published (3,4). patient and the society (5). It is, therefore, important that the
dentist is familiar with oral signs of both local and systemic
diseases/medical conditions, genetic disorders and oral manifes-
Defining oral pathology and oral
tations of adverse drug reactions, as no other healthcare person
medicine is educated or trained to diagnose these. Proficient history tak-
To define a recommended curriculum of oral pathology and ing, clinical examination, differential diagnosing and interpreta-
oral medicine, the following definitions of oral pathology and tion of para-clinical investigations in the diagnostic approach
oral medicine were agreed upon at the SFOPOM meeting in are all expected from the contemporary European dentist. To
Stockholm 2009: inform, treat and counsel patients, the dentist needs a profound
Oral pathology: Causes, progression and effects of diseases in knowledge of disease aetiology and progression and the possible
the oral mucosa, teeth, jaws and salivary glands and knowledge impact of lifestyle factors as well as of therapeutics and phar-
necessary for understanding diagnosis, prevention and manage- macology. In particular, the dentist must have profound knowl-
ment of such diseases. Oral pathology in general includes: clas- edge of predispositions and risk factors of diseases of the oral
sification, including terminology and definitions, epidemiology, region and be competent in informing patients of how to avoid
aetiology and pathogenesis, including molecular and genetic hazardous behaviour.
aspects, symptoms, morphology/diagnosis (macro/micro), pro- The competences in oral pathology and oral medicine were
gression and prognosis, indications for and interpretation of concretised at the SFOPOM meeting in Stockholm 2009:
diagnostic tests. The contemporary dentist must be able to:
Oral medicine: Aetiology, pathogenesis, epidemiology, diagnosis,
prevention and management of oral disorders and symptoms,
synthesise diagnosis, differential diagnoses and prognosis of
common diseases and disorders of the oral mucosa, teeth,
which may be either primary oral diseases or manifestations of jaws and salivary glands;
systemic diseases and which may be related to medically com-
plex states including side effects of medical treatments.
comprehend cellular and molecular processes, aetiology,
pathogenesis and classifications of diseases/disorders of the
Oral pathology and oral medicine overlap in the understand- oral mucosa, teeth, jaws and salivary glands;
ing of disease management and to underscore the relevance of
both to the practicing dentist; SFOPOM takes a stand for the
evaluate (react, treat, prevent and/or refer) diseases and dis-
orders in the maxillofacial area and maxillofacial manifesta-
integration of the two subject areas in dental education. tions of systemic diseases and medical disorders on the
This article is meant to delineate a reasonable standard of basis of clinical presentation (including radiography) and/
oral pathology and oral medicine in the European dental cur- or histological diagnosis;
riculum and to help subject representatives in curriculum undertake soft tissue biopsies of presumably benign lesions;
development and planning. We have created an advisory topic
list in oral pathology and oral medicine but we refrain from
be capable of detailed professional communication with
other health professions (orally and in writing) (1).
commenting on topics that predominantly belong to other den-
tal specialities, for example, cariology, endodontics, periodon-
tology and gerodontology. Whilst some overlap cannot be
Diagnostic approach
avoided, we also avoid commenting directly on supporting sub- It is fundamental that the dentist must be familiar with the
ject areas such as anatomy, cell biology and microbiology. Nor- normal variation in tissues of the oral cavity and the associated
mal variation in the oral tissues and developmental tissues of the head and neck and must be able to differentiate
disturbances should be given attention in the dental curriculum this from diseases/conditions affecting the region. In the diag-
and are believed to be part of oral anatomy and embryology, nostic process, the dentist must be able to consider the patho-
for example, Fordyces granules and fissured tongue, although genesis of the disease/condition and understand the differences
it should be recognised that the latter may also be associated between neoplastic, reactive, infectious and hamartomatous/
with various pathological conditions. In the SFOPOM-associ- developmental origin and between benign and malignant dis-
ated universities, oral pathology and oral medicine are taught eases.
in various ways, for example, lecture-based teaching, problem- The dentist must have knowledge of clinical symptoms,
based learning. Also, the extent of microscopy training varies local and systemic signs, and clinical differential diagnoses to
from none to rather extensive. However, the proposed advisory make an accurate diagnosis. The dentist must also be compe-
lists of diseases/conditions are meant to facilitate curriculum tent in selecting appropriate diagnostic tests, for example, tis-
planning regardless of pedagogical format but whilst no pre- sue biopsy and microbiological samples, and conducting
2 2012 John Wiley & Sons A/S
Kragelund et al. Curriculum guidelines for oral pathology & medicine
them correctly, as well as in interpreting test results and tak-
ing appropriate action accordingly. Furthermore, the dentist
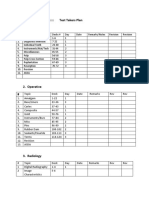
Guidelines for topic selection
must be aware of diseases demanding multidisciplinary coop- Diseases/conditions of the oral tissues may present as changes
eration and be able to recognise his/her professional limita- in colour, integrity, size, morphology and function. We have
tion, and to refer to specialists when required (5). In view organised a topic list according to clinical manifestation in the
of the rapid increase in the understanding of disease pro- oral cavity, categorising the diseases/conditions according to
cesses and the development of new treatment modalities, it their most characteristic clinical presentation (Table 1). Sys-
is also imperative that the dentist becomes a life-long learner temic diseases/disorders that may present oral manifestations
and proficiently utilises modern information technology in and that should be recognised by the dentist are presented in
his/her profession. Table 2. For simplicity, the number of disease categories has
TABLE 1. Advisory topic list of oral diseases/conditions categorised by most characteristic presentation and specified according to commonness, signifi-
cance, and uniqueness
Clinical
Primary changes presentation Origin Disease/condition Disease subgroup Commonness Significance Uniqueness
Colour changes Whitish and Developmental White sponge nevus 1 0 2
reddish Immune- Allegic reactions 2 13 1
mediated
Immune- Lingua geographica 3 1 3
mediated
Immune- Lichen planus/lichenoid lesions 3 2 2
mediated
Immune- Lupus erythematosus 2 2 2
mediated
Infection Hairy leukoplakia 1 3 3
Infection Candida infection 3 13 2
Neoplasia Squamous cell carcinoma incl 2 3 2
verrucous carcinoma
Premalignant Leukoplakia (homogenous, 3 3 3
non-homogenous, verrucous)
Premalignant Erythroplakia 1 3 3
Premalignant Actinic elastosis 3 1 2
Premalignant Actinic keratosis 2 3 2
Reactive Frictional keratosis 3 0 2
Reactive Morsicatio and linea alba 3 1 3
Reactive Tobacco-associated lesions 3 03 3
Reactive Toxic reactions 2 13 1
Reactive Foreign body reaction 2 1 2
Reactive Drug-induced lesions 1 2 1
Reactive Radiation and chemotherapy- 3 3 2
induced changes
Miscellaneous Anaemia 1 23 1
Reddish and Developmental Arteriovenous malformation 1 01 1
blueish Neoplasia Haemangioma 2 01 1
Neoplasia Kaposis sarcoma 1 3 2
Reactive Petechiae, ecchymosis, 3 03 2
haematoma
Brownish Neoplasia Nevi 1 01 1
Neoplasia Malignant melanoma 0 3 1
Physiological Physiologic pigmentation 3 0 2
Reactive Melanoplakia (idiopathic) 1 0 1
Reactive Disease-related pigmentations 1 3 3
Reactive Tobacco-associated 2 0 3
pigmentation
Reactive Drug-induced pigmentation 2 0 2
Reactive Foreign body reaction 2 1 2
2012 John Wiley & Sons A/S 3
Curriculum guidelines for oral pathology & medicine Kragelund et al.
Table 1. Continued
Clinical
Primary changes presentation Origin Disease/condition Disease subgroup Commonness Significance Uniqueness
Loss of epithelial Ulcerative Immune- Recurrent aphthous lesions 3 2 3
integrity mediated (minor/major/herpetiform)
Immune- Behcets disease 1 3 2
mediated
Infection Sexually transmitted infections 0 3 1
Infection Acute necrotising ulcerative 2 2 3
gingivitis
Neoplasia Squamous cell carcinoma 2 3 2
Reactive Traumatic injury, that is, 3 1 2
thermal, chemical and
mechanical
Reactive Drug-induced ulcerations 1 2 2
Reactive Necrotising sialometaplasia 1 1 3
Vesciculo- Immune- Pemphigoid 2 2 2
bullous mediated
Immune- Pemphigus vulgaris 1 3 2
mediated
Immune- Erythema multiforme 1 2 2
mediated
Infection Herpes simplex (herpes simplex 3 2 2
1 & 2)
Infection Chicken pox (varicella-zoster 3 2 2
virus)
Infection Herpes zoster (varicella-zoster 1 2 1
virus)
Infection Hand, foot, and mouth disease 2 1 2
(coxsackie virus)
Infection Morbilli (paramyxo virus) 1 1 2
Dysfunction Salivary Immune- Sjogrens syndrome 2 2 2
hypofunction mediated
Reactive Drug-induced 3 2 3
Reactive Radiation and chemotherapy- 3 2 3
induced
Neurological Unknown Burning mouth disease 2 2 3
Miscellaneous Facial pain 2 12 3
4 2012 John Wiley & Sons A/S
Kragelund et al. Curriculum guidelines for oral pathology & medicine
Table 1. Continued
Clinical
Primary changes presentation Origin Disease/condition Disease subgroup Commonness Significance Uniqueness
Swellings/ Deep Developmental Nasolabial cyst 1 1 3
hyperplasias Immune- Angioedema 1 3 2
mediated
Immune- Orofacial granulomatosis 2 3 3
mediated
Infection Dento-alveolar abscess 3 13 3
Infection Sialoadenitis (mumps) 1 1 3
Neoplasia Benign salivary gland tumours Pleomorphic 2 3 3
adenoma
Neoplasia Malignant salivary gland Mucoepidermoid 2 3 2
tumours carcinoma
Neoplasia Lymphangioma 2 1 1
Neoplasia Peripheral nerve tumours 2 1 1
Neoplasia Benign and malignant 2 3 1
neoplasias of the supporting
tissues
Neoplasia Metastases 2 3 1
Reactive Traumatic neuroma 2 2 2
Reactive Foreign body reaction 1 1 2
Reactive Sialolithiasis 2 2 3
Reactive Sialoadenosis 1 1 3
Exophytic Neoplasia Malignancy of the 1 3 1
haematopoietic system
Reactive Pyogenic granuloma 3 1 2
Reactive Fibro-epithelial hyperplasia 3 1 2
Reactive Gingival hyperplasia Giant cell 2 1 3
granuloma
Reactive Gingival hyperplasia Calcifying/ 2 1 3
ossifying/
fibroblastic
Reactive Gingival hyperplasia Hereditary 1 2 3
Reactive Gingival hyperplasia Drug-induced 2 2 3
Reactive Mucous retention cyst 3 1 2
Reactive Necrotising sialometaplasia 1 1 3
Papillary Infection Human papilloma virus-induced 3 13 2
hyperplasia
Infection Candida-associated hyperplasia 2 1 2
2012 John Wiley & Sons A/S 5
Curriculum guidelines for oral pathology & medicine Kragelund et al.
Table 1. Continued
Clinical
Primary changes presentation Origin Disease/condition Disease subgroup Commonness Significance Uniqueness
Radiological Radiolucent Developmental Non-odontogenic cysts or Nasopalatine cyst 2 1 3
changes pseudocysts
Developmental Odontogenic cysts Follicular cyst 2 2 3
Developmental Odontogenic cysts Eruption cyst 2 1 3
Developmental Odontogenic cysts Lateral periodontal 1 1 3
cyst
Developmental Odontogenic cysts Paradental cyst 1 1 3
Developmental Odontogenic cysts Glandular 2 2 3
odontogenic cyst
Developmental Odontogenic cysts Gorlins syndrome 1 2 2
Infection Periapical inflammation 3 2 3
Neoplasia Odontogenic cysts Keratocystic 2 2 3
odontogenic
tumour
Neoplasia Odontogenic tumours Ameloblastoma 2 2 3
Neoplasia Odontogenic tumours Adenomatoid 1 2 3
odontogenic
tumour
Neoplasia Odontogenic tumours Ameloblastic 1 2 3
fibroma
Neoplasia Odontogenic tumours Myxoma 1 2 3
Neoplasia Metastases 1 3 1
Reactive Odontogenic cysts Radicular cyst 3 2 3
Reactive Non-odontogenic cysts or Simple bone cyst 1 1 2
pseudocysts
Reactive Giant cell granuloma 1 2 2
Radiopaque Developmental Fibro-osseous lesions Osseous dysplasias 2 1 3
or mixed Developmental Fibro-osseous lesions Fibrous dysplasia 1 2 2
Infection Osteomyelitis 1 2 2
Neoplasia Odontogenic tumours Odontoma 2 1 3
Neoplasia Fibro-osseous lesions Ossifying fibroma 1 1 2
Reactive Osteoradionecrosis 1 2 2
Reactive Drug-induced osteonecrosis 2 2 3
(bisphosphonate)
Morphological Wear Tooth wear, that is, attrition, Wear 3 1 3
changes in abrasion and erosion
teeth Developmental Hypercementosis Developmental/ 2 1 3
reactive
Developmental Dentinogenesis imperfecta Developmental 1 2 3
Developmental Amelogenesis imperfecta Developmental 1 2 3
6 2012 John Wiley & Sons A/S
Kragelund et al. Curriculum guidelines for oral pathology & medicine
TABLE 2. Advisory topic list of systemic diseases/disorders that may present oral manifestations specified according to commonness, significance and
uniqueness
Disease/conditions Subgroup Commonness Significance Uniqueness
Muco-cutaneous diseases Lichen planus 3 2 2
Pemphigoid 2 2 2
Pemphigus vulgaris 1 3 2
Erythema multiforme 1 2 2
Behcets disease 1 3 1
Inflammatory bowel diseases Crohns disease 2 2 2
Ulcerative colitis 2 2 2
Celiac disease 23 2 2
Rheumatoid diseases/autoimmune diseases Sjogrens syndrome 2 2 2
Lupus erythematosus 2 2 2
Rheumatoid arthritis 2 2 1
Endocrine disorders Diabetes 3 2 1
Hypothyroidism 2 2 1
Hypophosphatasia 1 3 2
Hyperparathyroidism 1 3 1
Deficiencies Anaemia 1 23 1
Iron, vitamin-B deficiency 2 3 2
Eating disorders 3 3 2
Infectious diseases HIV 1 3 2
Sexually transmitted infections (incl. HPV) 12 3 1
Tuberculosis 1 3 1
Morbilli (paramyxovirus) 1 1 2
Malignancies Leukaemia 1 3 2
Lymphoma 1 3 1
Signs of malignancy incl. metastases 1 3 1
Drug reactions associated with Bone diseases 1 2 2
Cardiovascular diseases 1 13 2
Immunosuppression 1 2 2
Infectious diseases 2 1 2
Malignant diseases 1 3 2
CNS diseases 1 2 2
Polypharmacy 3 13 23
been kept at a minimum and the grouping may therefore seem Score 0 trivial, of no clinical significance.
slightly imprecise. In addition, there is a slight redundancy 1 may cause mild to moderate morbidity.
owing to the multitude of clinical presentations displayed by 2 causes significant morbidity.
some conditions. 3 potentially fatal or indicates fatal disease.
Some diseases/conditions are common, others have signifi- Domain 3: Uniqueness
cant consequences for the patients health, and others again Score 0 a condition or lesion that is not seen and does
are unique to the oral cavity. The commonness of a disease not affect the omfa.
may vary between different populations and may be difficult, 1 when a lesion or condition occurs, it uncommonly
if not impossible, to establish for some oral conditions. In affects the omfa.
the presented guidelines, the commonness reflects that of 2 when a lesion or condition occurs, it commonly affects
the Scandinavian and European population. We have speci- the omfa.
fied the commonness, significance and uniqueness of the 3 exclusively an oral condition or lesion.
diseases/conditions by modifying the scoring of Darling & The criteria for the selection of the topics are based on
Daley. (4): how often the dentist will meet the disease/condition in gen-
Domain 1: Commonness eral dental practice, how significant it is for the morbidity
Score 0 never or rarely occurs in the oral and maxillofa- and quality of life of the patient and how unique it is in the
cial area (omfa). oral cavity. The latter is important as the dentist most likely
1 uncommonly occurs in the omfa. is the only specialist with detailed knowledge of the disease/
2 sometimes occurs in the omfa. condition. To understand the aetiology and mechanisms of
3 commonly occurs in the omfa or commonly occurs in disease progression, the dentist must also understand the prin-
the omfa secondary to other disease or treatment. ciples for classification of jaw cysts, odontogenic and salivary
Domain 2: Significance gland tumours.
2012 John Wiley & Sons A/S 7
Curriculum guidelines for oral pathology & medicine Kragelund et al.
Procedure from draft to manuscript References
It was decided at the 39th SFOPOM meeting in Troms 2010 1 Kragelund C, Reibel J, Hadler-Olsen ES, et al. Scandinavian
to make an advisory topic list to assist subject representatives Fellowship for Oral Pathology and Oral Medicine: statement on oral
in the development and planning of dental curricula in oral pathology and oral medicine in the European Dental Curriculum. J
pathology and oral medicine. A first draft was written by CK Oral Pathol Med 2010: 39: 800e1.
and GW and sent to the co-authors to discuss with their col- 2 Cowpe J, Plasschaert A, Harzer W, Vinkka-Puhakka H, Walmsley
AD. Profile and competences for the graduating European dentist
leagues at their departments. Representatives from seven uni-
update 2009. Eur J Dent Educ 2010: 14: 193202.
versities completed the scoring of the topics listed and 3 Odell EW, Farthing PM, High A, et al. British Society for Oral and
suggested topics to be added to the list. The scorings were Maxillofacial Pathology, UK: minimum curriculum in oral
compiled and summarised by CK and GW. A revised draft was pathology. Eur J Dent Educ 2004: 8: 177184.
sent to the co-authors and to the participants of the 40th SFO- 4 Darling MR, Daley TD. Oral pathology in the dental curriculum: a
POM meeting in Turku 2011 and was discussed at a seminar. guide on what to teach. J Dent Educ 2006: 70: 355360.
A final draft was composed by CK and GW and after agree- 5 Epstein JB, Sciubba JJ, Banasek TE, Hay LJ. Failure to diagnose and
ment of the co-authors submitted for publication in Eur J Dent delayed diagnosis of cancer: medicolegal issues. J Am Dent Assoc
Education. The tables are available at http://www.sfopom.org/. 2009: 140: 14941503.
Acknowledgements
The authors thank the participants of curriculum discussions at
the 39th and 40th SFOPOM meetings.
8 2012 John Wiley & Sons A/S
Вам также может понравиться
- Oral PathДокумент49 страницOral PathAnca NeaguОценок пока нет
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Must Knows For Nbde Part IIДокумент1 страницаMust Knows For Nbde Part IIshalom1413Оценок пока нет
- Aa 1 MasterRQsДокумент93 страницыAa 1 MasterRQsSadhana SabhandasaniОценок пока нет
- DENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideОт EverandDENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideОценок пока нет
- Oral Maxillofacial Surgery 020512Документ14 страницOral Maxillofacial Surgery 020512Sagar JangamОценок пока нет
- Paget Disease of Bone, A Simple Guide to the Condition, Treatment and Related DiseasesОт EverandPaget Disease of Bone, A Simple Guide to the Condition, Treatment and Related DiseasesОценок пока нет
- Chapter 1Документ38 страницChapter 1synap5esОценок пока нет
- Lowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandLowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Orofacial Infections in Children PedoДокумент40 страницOrofacial Infections in Children PedoFourthMolar.comОценок пока нет
- Good Morning: by Ibrahim GBRДокумент34 страницыGood Morning: by Ibrahim GBRDento - PhilicОценок пока нет
- Median Rhomboid GlossitisДокумент2 страницыMedian Rhomboid Glossitisdianzalerti9240Оценок пока нет
- Fundamentals of Oral-Maxillofacial Pathology & MedicineДокумент80 страницFundamentals of Oral-Maxillofacial Pathology & Medicinesammy0% (2)
- 2020 Tongue Disorders Ods 210Документ25 страниц2020 Tongue Disorders Ods 210Farhaana ShaboodienОценок пока нет
- Lecture 2A The Chief Complaint Its HistoryДокумент20 страницLecture 2A The Chief Complaint Its HistoryAhmed HegazyОценок пока нет
- Dev Disturbances of Gingiva and TongueДокумент77 страницDev Disturbances of Gingiva and TongueNavyy DentОценок пока нет
- 300 DA Facts For NBDE IДокумент13 страниц300 DA Facts For NBDE IAarrthi SОценок пока нет
- Fluoridation - Seminar TopicДокумент4 страницыFluoridation - Seminar Topicnawafaslam100% (1)
- Application Package Toronto College of Dental HygieneДокумент12 страницApplication Package Toronto College of Dental Hygienervdh71Оценок пока нет
- Dry Mouth (Xerostomia)Документ18 страницDry Mouth (Xerostomia)dr_jamal1983Оценок пока нет
- Sample Questions MJDF Part 1 Sample Questions MJDF Part 1Документ21 страницаSample Questions MJDF Part 1 Sample Questions MJDF Part 1HarkanОценок пока нет
- Periodontal Problems in KidsДокумент49 страницPeriodontal Problems in KidsRaksmey PhanОценок пока нет
- Periodicity DentalGuideДокумент52 страницыPeriodicity DentalGuideSalam BataienehОценок пока нет
- Oral Tuberculosi S: Dr. Ishita Singhal Mds First YearДокумент31 страницаOral Tuberculosi S: Dr. Ishita Singhal Mds First YearDR. ISHITA SINGHALОценок пока нет
- Aapd Guidelines - Restorative DentistryДокумент8 страницAapd Guidelines - Restorative DentistrymahmoudОценок пока нет
- Ans 30 Dec Nbde 1 RQДокумент10 страницAns 30 Dec Nbde 1 RQKandiwapa ShivuteОценок пока нет
- Gingival InflammationДокумент12 страницGingival InflammationdeenmОценок пока нет
- Pregnancy & Oral Health SlidesДокумент32 страницыPregnancy & Oral Health Slidesdikri pangersaОценок пока нет
- Oral and Maxillofacial SurgeryДокумент6 страницOral and Maxillofacial Surgerysunaina chopraОценок пока нет
- Schedule 14 Protected Persons and Convention RefugeesДокумент1 страницаSchedule 14 Protected Persons and Convention RefugeesMaTiullah KhanОценок пока нет
- Oral Path Summary SheetДокумент5 страницOral Path Summary Sheettrangy77Оценок пока нет
- Vika Nbde Part 2 Revised 1Документ3 страницыVika Nbde Part 2 Revised 1luckytung07Оценок пока нет
- Gingival EnlargementДокумент125 страницGingival Enlargementdr_saurabhsinha_165Оценок пока нет
- Dental Considerations-CVS DiseasesДокумент86 страницDental Considerations-CVS Diseasesapi-3704106100% (1)
- 03 MFDS Regulations & Syllabus 2011Документ15 страниц03 MFDS Regulations & Syllabus 2011FarahMohammed1Оценок пока нет
- Community Dental Health Final Flashcards - QuizletДокумент19 страницCommunity Dental Health Final Flashcards - QuizletRMОценок пока нет
- Indications For Removal of TeethДокумент27 страницIndications For Removal of TeethMoh'dMAssufiОценок пока нет
- Systemic Diseases Manifested in The JawsДокумент25 страницSystemic Diseases Manifested in The JawsTeguh Caninus100% (1)
- What Is EBD?Документ7 страницWhat Is EBD?RATHEESH M. S.Оценок пока нет
- Oral Manifestations in Covid19Документ2 страницыOral Manifestations in Covid19La redazione Tp24Оценок пока нет
- Write Your Name On Your Scantron Scoring SheetДокумент8 страницWrite Your Name On Your Scantron Scoring Sheetchakriy9Оценок пока нет
- 1st Course Introductory Course in Paediatric Dentistry&Childhood StagesДокумент29 страниц1st Course Introductory Course in Paediatric Dentistry&Childhood StagesChristosSougkakisОценок пока нет
- NBDE Part 1 RQ FileДокумент132 страницыNBDE Part 1 RQ Filenaumz60% (5)
- ORAL SURGERY FlashcardsДокумент9 страницORAL SURGERY FlashcardsMihika MahandwanОценок пока нет
- 2009 Mid-Term Questions For Oral Pathology 1 Exclude Cyct Questions, Because They Are Not Included in Your Mid ExamДокумент7 страниц2009 Mid-Term Questions For Oral Pathology 1 Exclude Cyct Questions, Because They Are Not Included in Your Mid ExamPrince AhmedОценок пока нет
- Good Morning.: @areebazainabДокумент42 страницыGood Morning.: @areebazainabshabana waniОценок пока нет
- Oral Pathology For The Dental Hygienist 7th Edition Test BankДокумент22 страницыOral Pathology For The Dental Hygienist 7th Edition Test BankDaniel EstibarОценок пока нет
- Syllabus 5k en ExamДокумент2 страницыSyllabus 5k en ExamVagelis RaftopoulosОценок пока нет
- Developmental Disturbances of The Oral Mucosa, Gingiva and TongueДокумент51 страницаDevelopmental Disturbances of The Oral Mucosa, Gingiva and Tonguekavin_sandhu100% (1)
- 1000 Mcqs - MiscellaneousДокумент11 страниц1000 Mcqs - MiscellaneousSelvaArockiamОценок пока нет
- A Guide To Succeeding in The Df1 Interview (Sample Pages Only)Документ15 страницA Guide To Succeeding in The Df1 Interview (Sample Pages Only)jaipald9067% (3)
- Anterior Teeth Ndbe McqsДокумент5 страницAnterior Teeth Ndbe McqsParneetОценок пока нет
- NBDE NotesДокумент2 страницыNBDE NotesAbhay KhannaОценок пока нет
- 2015Документ45 страниц2015jimmyОценок пока нет
- Tongue DisordersДокумент31 страницаTongue DisordersMaphoto Xola0% (1)
- NBDE PART 2::::::::::::::::::: Test Takers Plan 1. EndodonticsДокумент6 страницNBDE PART 2::::::::::::::::::: Test Takers Plan 1. EndodonticsEmma LiamОценок пока нет
- Australian Dental Journal: Rhinosinusitis in Oral Medicine and DentistryДокумент7 страницAustralian Dental Journal: Rhinosinusitis in Oral Medicine and DentistryVishakha SabooОценок пока нет
- Incline PlanesДокумент3 страницыIncline PlanesdigdouwОценок пока нет
- Diagnosis of Metastatic Neoplasms An Immunohistochemical ApproachДокумент9 страницDiagnosis of Metastatic Neoplasms An Immunohistochemical ApproachdesantosalbaОценок пока нет
- Washington: Pride of The Nation: Climate and TransportationДокумент8 страницWashington: Pride of The Nation: Climate and TransportationdesantosalbaОценок пока нет
- A New Lingual Straight-Wire TechniqueДокумент10 страницA New Lingual Straight-Wire TechniquedesantosalbaОценок пока нет
- Effectiveness of Tramadol/paracetamol Compared With Etoricoxib As Postoperative Analgesia in Daycare SurgeryДокумент6 страницEffectiveness of Tramadol/paracetamol Compared With Etoricoxib As Postoperative Analgesia in Daycare SurgerydesantosalbaОценок пока нет
- Census FormatДокумент35 страницCensus Formatkolintang1Оценок пока нет
- TiroideДокумент10 страницTiroideRosália CoutadaОценок пока нет
- Comorbidity GuidelinesДокумент231 страницаComorbidity Guidelinesgavinbuzz100% (1)
- Bacterial MeningitisДокумент2 страницыBacterial MeningitisSpideyPacerОценок пока нет
- Axali, Damatebiti Tipobrivi Sagamocdo Testuri Sekitxvebi Medicinis Fakultetis Iii Kursis Studentebisatvis Mikrobiologia 2-SiДокумент15 страницAxali, Damatebiti Tipobrivi Sagamocdo Testuri Sekitxvebi Medicinis Fakultetis Iii Kursis Studentebisatvis Mikrobiologia 2-SiMKGUОценок пока нет
- Chapter 9: Congenital Constriction Band Syndrome (CCBS)Документ3 страницыChapter 9: Congenital Constriction Band Syndrome (CCBS)Javaid KhanОценок пока нет
- Polyphenols, and Physical PerformanceДокумент7 страницPolyphenols, and Physical PerformancezoliteamlavylitesОценок пока нет
- Somatic Symptom and Related DisordersДокумент31 страницаSomatic Symptom and Related DisordersMarinel June Paler100% (2)
- Mini VET GuideДокумент186 страницMini VET GuideemitibiОценок пока нет
- CEMAT 3 (Pvt. Hosp Booking) Hanbook Version 0Документ47 страницCEMAT 3 (Pvt. Hosp Booking) Hanbook Version 0sourabhОценок пока нет
- Managing Anaphylactic Shock Journal of Modern Pharmacy 2006Документ3 страницыManaging Anaphylactic Shock Journal of Modern Pharmacy 2006Saputro AbdiОценок пока нет
- Gemsical Cap (Menrik Biomerge PVT LTD)Документ3 страницыGemsical Cap (Menrik Biomerge PVT LTD)Nani GangОценок пока нет
- Notices About Filtered ResultsДокумент5 страницNotices About Filtered ResultsJoshua TerceñoОценок пока нет
- 3.muscle TestДокумент10 страниц3.muscle TestSummer PookieОценок пока нет
- Clinical Medical Reviews and Case Reports CMRCR 5 227Документ8 страницClinical Medical Reviews and Case Reports CMRCR 5 227Juan BacelarОценок пока нет
- Carcinoma BreastДокумент47 страницCarcinoma BreastMayank YadavОценок пока нет
- DRUG STUDY Durano Aireen E.Документ4 страницыDRUG STUDY Durano Aireen E.Doneva Lyn MedinaОценок пока нет
- De Novo Histoid Leprosy With Borderline Tuberculoi PDFДокумент5 страницDe Novo Histoid Leprosy With Borderline Tuberculoi PDFNelsi Mellisa DewiОценок пока нет
- Stroke Hemoragic: Sebagai Salah Satu Tugas Mata Kuliah TIK Akademi Keperawatan (Akper) SawerigadingДокумент10 страницStroke Hemoragic: Sebagai Salah Satu Tugas Mata Kuliah TIK Akademi Keperawatan (Akper) SawerigadingMade Serly KrisdayantiОценок пока нет
- Small For Gestational Age: I. Definition/ DescriptionДокумент11 страницSmall For Gestational Age: I. Definition/ Descriptionfaye kimОценок пока нет
- Assaz Predisposing Factors: Advanced Age Gender Ileal Resection/Disease RaceДокумент3 страницыAssaz Predisposing Factors: Advanced Age Gender Ileal Resection/Disease RaceryanОценок пока нет
- Gavage Feeding RepДокумент6 страницGavage Feeding RepEon Provido AlfaroОценок пока нет
- Cirrhosis & Vit KДокумент8 страницCirrhosis & Vit KBagii GonchigОценок пока нет
- Harjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCДокумент7 страницHarjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCSofia PerezОценок пока нет
- Jama Statin and Stroke Prevention SupplementДокумент17 страницJama Statin and Stroke Prevention SupplementMesan KoОценок пока нет
- Soal Prof. BalaДокумент3 страницыSoal Prof. BalaronnyОценок пока нет
- OligodendrogliomaДокумент9 страницOligodendrogliomaroni pahleviОценок пока нет
- Vaginal Discharge GuidelineДокумент4 страницыVaginal Discharge GuidelineGung Bagvs SaputraОценок пока нет
- Autonomic Dysreflexia-Part OneДокумент3 страницыAutonomic Dysreflexia-Part OneManuel BucurОценок пока нет
- Method of Toxicity Test 1Документ59 страницMethod of Toxicity Test 1Widya AnggrainiОценок пока нет
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerОт EverandGut: the new and revised Sunday Times bestsellerРейтинг: 4 из 5 звезд4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingОт EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingРейтинг: 4 из 5 звезд4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningОт EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningРейтинг: 4 из 5 звезд4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsОт EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsРейтинг: 4.5 из 5 звезд4.5/5 (6)