Академический Документы
Профессиональный Документы
Культура Документы
PAPER (ENG) - (Caplan L.) Occlusion of The Vertebral or Basilar Artery - Follow Up Analysis of Some Patients With Benign Outcome
Загружено:
Aldo Hip NaranjoОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
PAPER (ENG) - (Caplan L.) Occlusion of The Vertebral or Basilar Artery - Follow Up Analysis of Some Patients With Benign Outcome
Загружено:
Aldo Hip NaranjoАвторское право:
Доступные форматы
PROLONGED CEREBRAL ISCHEMIA/ATo/a/a 277
models of brain ischemia. Stroke 7: 14-17, 1976 1960
9. Reivich M, Jehle J, Sokoloff L, Kety SK: Measurement of 16. Cantu RC, Ames A, DiGiacinto G, Dixon J: Hypotension: A
regional cerebral blood flow with antipyrine - U C in awake major factor limiting recovery from cerebral ischemia. J Surg
cats. J Appl Physiol 27: 296-300, 1969 Res 9: 525-529, 1969
10. Hossmann K-A, Zimmermann V: Resuscitation of the monkey 17. Heymann C, Bouckert JJ, Jourdan F, Nowak SJG, Farber S:
brain after 1 hour complete ischemia. I. Physiological and Survival and revival of nerve centers following acute anemia.
morphological observations. Brain Res 81: 59-74, 1974 Arch Neurol Psych 38: 304-309, 1937
11. Ponte J, Purves M: The role of the carotid body chemo- 18. Hossmann K-A, Sakaki S, Kimoto K: Cerebral uptake of
receptors and carotid sinus baroreceptors in the control of glucose and oxygen in the cat brain after prolonged ischemia.
cerebral blood vessels. J Physiol 237: 315-340, 1974 Stroke 7: 301-305, 1976
12. Ellis CH, Colville KI: Effect of current intensity on cardiovas- 19. Hossmann, K-A, Sakaki S, Zimmermann V: Cation activities
cular response to transcranial stimulation. Dis Nerv Sys 19: in reversible ischemia of the cat brain. Stroke 8: 77-81, 1976
54-57, 1958 20. Wolin LR, Massopust LC Jr, Taslitz N: Tolerance to arrest of
13. Lind B, Snyder J, Safar P: Total brain ischemia in dogs: cerebral circulation in the rhesus monkey. Exp Neurol 30:
Cerebral physiological and metabolic changes after 15 minutes 103-115, 1971
of circulatory arrest. Resuscitation 4: 97-113, 1976 21. Miller JR, Myers RE: Neurological effects of systemic circula-
14. Weinberger LM, Gibbon MH, Gibbon JH Jr: Temporary tory arrest in the monkey. Neurology (Minneap) 20: 715-724,
arrest of the circulation to the central venous system. Arch 1970
Neurol Psych 43: 615-634, 1940 22. Safar P, Stezoski W, Nemoto EM: Amelioration of brain
15. Brockman SK, Jude JR: The tolerance of the dog brain to total damage after 12 minutes cardiac arrest in dogs. Arch Neurol
arrest of circulation. Bull Johns Hopkins Hosp 106: 74-80, 33: 91-95, 1976
Occlusion of the Vertebral or Basilar Artery
Follow Up Analysis of Some Patients with Benign Outcome
Louis R. CAPLAN, M.D.
S U M M A R Y Ten patients with angiographically verified occlusion of the basilar or vertebral artery have
been followed for an average of 2.75 years. None has developed further ischemia after the initial stroke, and 4
patients survived without any clinical deficit. In occlusive disease of the posterior circulation, the critical period
for deficit acquisition is at the time of occlusion. Extent of the deficit depends on the rapidity of development of
adequate collateral circulation, and the presence of distal embolization at the time of occlusion. Some patients
survive basilar occlusion without permanent deficit.
Stroke Vol 10, No 3, 1979
OCCLUSION of the basilar artery is generally con- circulation. 46 No reference could be found on follow
sidered a very serious event incompatible with normal up of patients with angiographically documented
survival. Kubik and Adams 1 described 18 patients vertebrobasilar occlusive disease.
with brainstem infarction due to occlusion of the The author's files, and those of the Harvard Stroke
basilar artery discovered at postmortem examination Registry,7 were searched for patients meeting the
and emphasized the abrupt onset and frequent fatal following criteria: 1) patients who were examined and
outcome. Marshall2 subsequently pointed out that followed carefully by the author during hospitaliza-
many untreated patients with the clinical picture of tion for acute stroke; 2) technically satisfactory
posterior circulation vascular disease do not develop angiograms taken during the stroke which
serious deficits; however, the underlying vascular documented an occlusion of either a vertebral or the
pathology in this group of clinical patients was un- basilar artery; 3) patients who survived the acute
known. Occlusion of the vertebral artery, the most stroke and had been followed by the author more than
frequent cause of lateral medullary infarction iden- 6 months. The temporal profile of illness and clinical
tified at postmortem examination,3 has usually been outcome in this group of patients gave insights into the
associated with a relatively benign clinical course.4 In- pathogenesis of the clinical deficit and mechanisms of
frequent studies have attempted to correlate the compensation.
severity of the neurological deficit with angio-
graphically verified vascular pathology in the posterior Results
Case Material
From the Department of Neurology, Beth Israel Hospital and Ten patients (8 male, 2 female) from 26-71 years of
Harvard Medical School, Boston, MA.
Reprints: Louis R. Caplan, M.D., Chairman, Department of
age (average 52.2 years) were studied clinically and
Neurology, Michael Reese Hospital, 29th St. and Ellis, Chicago, IL angiographically. Six had occlusion of the basilar
60616. artery (2 proximal and 4 midportion beyond the
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
278 STROKE VOL 10, No 3, MAY-JUNE 1979
AICA branching). Four had an occluded vertebral weeks. In 4 of these 8 patients the clinical deficit fluc-
artery. All basilar occlusion cases had collateral cir- tuated with alteration of position in bed (3 when
culation involving the long circumferential cerebellar elevated, 1 when turned to the left side). Two patients
vessels (PICA, AICA, SCA) with late filling of the left the hospital without neurological abnormalities, 3
distal segment of the basilar artery. Patients with ver- had slight deficits, 4 moderate and 1 severe.
tebral occlusion had a patent contralateral vertebral Follow up ranged from Vi to 6 years (average 2.75
artery and basilar artery. Six patients had transient years). No patient developed a late increase in deficit
ischemic attacks (TIAs) prior to strokes. The time referable to the posterior circulation, and in 6 patients
between the initial TIA and the stroke ranged from 1 clinical deficits improved during the period of follow
week to 1 year (average 15 weeks). The last TIA up. Two patients with a slight deficit upon hospital dis-
always occurred within 1 month of the stroke (5 or 6 charge subsequently returned to normal. Six patients
within 1 week). TIAs were usually multiple (range have been treated with long-term warfarin; 2 patients
1-30, average 11). had temporary anticoagulant treatment (1 heparin for
After onset of stroke, 8 patients had either progres- 2 weeks, 1 warfarin for 6 months). No patient has had
sion of the deficit over a 2 or 3 day period, or had fluc- a new stroke, but 1 patient died of a myocardial in-
tuations of their clinical deficit during the first 2 farction 4 years after his pontine infarction.
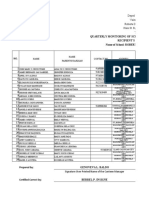
TABLE 1 Vertebrobasilar Occlusion-Deficit Profile
Deficit at Severity of
hospital deficit at Follow up
Age/Sex Onset and course Clinical signs discharge follow up length Angiographic lesion
(Group I)
1. 65, M TIA 1 year before; dysarthna, clumsy slight none 2^yrs. Proximal basilar occlusion
6 TIA's within 2 right arm, inter-
wks., fluctuating mittent INO
deficit 1 week
2. 60, M 5 mos. before-3 left hemiplegia, mod. mod. 6yrs. Midbasilar occlusion
TIA's, 2 mos.- pain in right eye
prolonged TIA,
awakened with
sudden deficit
3. 59, M many TIA's over bilat. VI, R VII, none none 4 yrs. Midbasilar occlusion
wks; fluctuating fluctuating level of beyond AICA
deficit for 2 wks. consciousness
4. 46, M 30 or more TIA's transient quadriplegia none none 2}/2 yrs. Proximal basilar occlusion
over 3 mos., grad. and dysarthria
onset of deficit over
hrs. with fluctuation
for 2 weeks
5. 26, M 4 TIA's in 2 wks; R hemiparesis, L mod. slight l^yrs. Right vertebral occlusion;
sudden deficit ataxia, dysarthria, embolic occlusion of supe-
dysphagia rior cerebellar artery and
narrowing of PCA
6. 71, M TIA 1 week before nystagmus, R VII, R slight none l^yrs. Right vertebral occlusion
sudden deficit ataxia, transient at Cl level
which fluctuated L hemiparesis
for 1 week
(Group II)
7. 44, F Sudden deficit; R Homer's R palatal mod. mod. 3 yrs. Right vertebral artery
later progressing paralysis, diminished occluded intracranially
over 48 hours pain and temp, sensation
R face and L body,
R arm ataxia
8. 58, M 2 abrupt deficits L VI, L ataxia, mod. slight 4 ^ yrs. Left vertebral occlusion
then fluctuated bilateral upgoing toes neck
for one week
9. 38, M sudden deficit with quadriparesis upgoing slight slight 6 mos. Occlusion midbasilar
fluctuation for 2 toes, pseudobulbar artery; no filling of right
weeks vertebral artery
(Group III)
10. 55, M gradual evolution quadriplegia, bilat. severe severe 4 yrs. Midbasilar occlusion
over 72 hours facial and tongue beyond AICA
weakness
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
VERTEBRAL, BASILAR OCCLUSION/Cap/an 279
The patients fitted into 3 different patterns of onset
and course (table). 1) The majority (6) (patients 1-6)
had TIAs prior to stroke. The TIAs were usually mul-
tiple and increased in frequency as the stroke ap-
proached, with 5 of 6 patients having a TIA within a
week of the stroke. The stroke usually began in the
morning on rising, and symptoms and signs of
brainstem, cerebellar and posterior cerebral artery
territory dysfunction fluctuated for a period ranging
between 2 days and 3 weeks. Clinical fluctuations were
very sensitive to postural change. After a period of 2-3
weeks, the clinical deficit stabilized and no further
deterioration occurred. 2) A second group of 3
patients (patients 7-9) had sudden onset deficits with
only minor subsequent fluctuations over a period of
2-3 days. All had unilateral vertebral occlusions
angiographically. 3) One patient (No. 10) had a
progressive course over 3 days without TIAs or
sudden onset.
Illustrative Cases
1. Patient 4
FIGURE 2. Patient 4: Retrograde filling of the basilar
A 46-year-old man with known coronary artery dis- artery (arrow) and superior cerebellar artery from a carotid
ease had 30 or more episodes of vertigo and diplopia injection.
during a 3 month period. He awakened during
December, 1975, with poor hearing and slurred speech
and staggered when he attempted to walk. Recovery a few seconds. He was placed in the Trendelenburg
occurred within hours, but later the same day he position and an intravenous infusion of heparin was
became mute and quadriplegic while awaiting ex- begun. By the next morning, a right internuclear
amination in the office of an otologist. Neurological ophthalmoplegia (INO) and slight left hemiparesis
examination within minutes revealed ocular bobbing remained; by day 7, examination showed return to
and no voluntary or reflex horizontal gaze. There was normal. Angiography revealed occlusion of the prox-
severe facial, palatal and lingual paralysis bilaterally. imal basilar artery; the left posterior inferior
The left limbs were flaccid, but the patient could cerebellar artery (PICA) filled the left superior
feebly lift his right arm and right leg from the bed for cerebellar artery (SCA) by branches coursing over the
cerebellar hemispheres, leading to delayed filling of
the distal basilar artery (figs. 1 and 2). A transient
brief deficit (right INO and left hemiparesis) followed
angiography. During hpspitalization the patient was
treated with intravenous heparin, subsequently
changed to warfarin. He has had no further attacks or
central nervous system deficits in the 2Vi years since
hospitalization. After 1 year, warfarin was discon-
tinued. He has been maintained on dipyridamole 150
mg, aspirin 20 grains and clofibrate 2 gm daily.
2. Patient 1
A 65-year-old male with a remote myocardial in-
farction (20 years) complained of intermittent
claudication of his legs. A year before hospitaliza-
tion, he had a brief episode of dizziness with diplopia.
Two weeks before admission an episode of diplopia
lasted 5 minutes. During the week before hospitaliza-
tion, there were 4 brief spells of dizziness with
diplopia; on one other occasion he suddenly slumped
to the ground without paralysis. An ophthalmologist
whom he consulted discovered weakness of the right
FIGURE I. Patient 4: Vertebral angiogram lateral view. lateral rectus muscle. On the morning of admission in
Filling of the PICA and cerebellar branches of the vertebral December, 1974, he noted dizziness, slurred speech
artery without filling of the basilar artery. and numbness, and weakness of his right limbs. A left
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
380 STROKE VOL 10, No 3, MAY-JUNE 1979
Horner's syndrome, left horizontal rotatory
nystagmus, and right limb ataxia were present on ex-
amination. During the initial 3 weeks of hospitaliza-
tion there was considerable fluctuation of his symp-
toms and signs, often after elevation of his head. On
day 5, transfemoral vertebral angiography demon-
strated complete occlusion of the proximal basilar
artery with reflux from the left vertebfal artery filling
the right vertebral. Both PICAs were opacified. Treat-
ment with intravenous heparin had been instituted
shortly after hospitalization, but had to be stopped on
day 14 when a large retroperitoneal hemorrhage
developed. Upon hospital discharge at 4 weeks, the
patient's only residual neurological deficit was slight
instability of gait. He has had no transient episodes or
strokes during the 7>Vi years since hospitalization and
has been able to return to work in a restaurant. He has
been maintained on aspirin 15 grains daily.
FIGURE 4. Patient 5: Left vertebral injection. Limited
3. Patient 5 retrograde filling of the right vertebral artery and non-filling
of the left superior cerebellar artery. A plaque is seen near
A 26-year-old man had several poorly defined the left posterior cerebral artery orifice.
episodes of dizziness, occasionally accompanied by
weakness of the face or legs. Two weeks later
(January, 1977) he awakened with dizziness and ring- he became unable to walk; his vision was distorted es-
ing in his right ear, and vomited. Later in the morning, pecially to the right; and he could not swallow. Blood
pressure was 145/85. Present on examination were a
left Horner's syndrome, left horizontal rotatory
nystagmus, bifacial weakness, left greater than right,
palatal and lingual weakness with severe dysarthria,
moderate right hemiparesis, clumsiness of the left
hand and increased deep tendon reflexes, right greater
than left. CAT scan was normal. Angiography the
same day revealed occlusion of the right vertebral
artery intracranially. Injection of the left vertebral
artery led to good basilar opacification but nofillingof
the left superior cerebellar artery; a narrowing was ap-
parent at the orifice of the left posterior cerebral
artery (figs. 3 and 4). Treatment with heparin was
begun and was later changed to warfarin.
Several months after the stroke, the patient
developed transient unilateral spells of numbness, first
in his right, then left limbs. These were migratory,
associated with headache, and disappeared after
diphenylhydantoin was begun. The clinical impression
was that the spells were migrainous. In April, 1977, he
developed severe chest pain and an electrocardiogram
revealed an acute myocardial infarction. Coronary
arteriography revealed occlusion of the left anterior
descending coronary artery, but no embolic source
was identified by cardiac catheterization. Blood lipids
were normal. A temporal artery biopsy was normal.
He has had no further neurological symptoms 18
months after his stroke. Residual deficit consisted of
slight slurring of speech and clumsiness of his left arm.
He has been maintained on warfarin.
Discussion
5
FIGURE 3. Patient 5: Right vertebral angiogram revealing Meyer et al. described the angiographicfindingsin
filling of the PICA but no distal vertebral opacification 35 patients with occlusive disease of the posterior cir-
(arrow) culation and emphasized the frequency of abnor-
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
VERTEBRAL, BASILAR OCCLUSION/Cap/an 281
malities in the basilar artery itself. Clinical course and (sometimes after death of cerebral tissue, i.e., stroke)
follow up data were not included in the report, which which is generally resistant to further hemodynamic
excluded "critically ill patients" or those with severe crises. In addition, stabilization of the clot (days to
brainstem infarction. Nonetheless, angiography in 2 weeks) is usually associated with a cessation of late
patients revealed clinically unsuspected complete emboli arising from the region of thrombosis.
occlusion of the basilar artery. Archer and In some patients, e.g., group 3 (patient 10) throm-
Horenstein6 discussed the angiographic findings in 20 bosis may produce a progressive clinical course over
patients with basilar occlusion. Their clinical group days without preceding TIAs. In our experience, in
consisted of patients with severe clinical deficits in patients with progressing stroke due to lacunar infarc-
contrast to Meyer's criteria for selection.3 Fifteen of tion or internal carotid artery occlusion, the prognosis
Archer and Horenstein's patients were stuporous or is poorer than for those patients with TIAs or fluctuat-
comatose at the time of angiography and 2 were ing course. The recovery phase of a TIA or fluctuat-
"locked-in"; 15 patients died, 4 were severely disabled ing thrombotic stroke may be due, at least partially, to
and 1 patient had a moderately severe deficit the presence of adequate collateral circulation.
(hemiparesis). These authors defined the locus of Progressing stroke may indicate poor collateral poten-
occlusion and the pathways of collateral circulation tial, and so a worse prognosis. The single patient in
and sought to correlate the anatomy of the clinical group 3 in this report had the most severe deficit of
deficit with angiographic findings. Caplan and Rosen- any of our 10 patients.
baum4 pointed out the utility of vertebrobasilar Jones, Millikan and Sandok11 described the tem-
angiography in differentiating severe obstructive dis- poral profile of 37 patients with a clinical diagnosis of
ease of the vertebral or basilar artery from "small vertebrobasilar system infarction. None of the
vessel" disease within the posterior circulation, and patients had angiographic definition of the underlying
emphasized the frequent benign outcome of many vascular pathology, but all 10 patients who died had
patients with clinical vertebrobasilar symptoms who occlusion of a vertebral or basilar artery at post-
had no major vascular lesions seen angiographically. mortem examination. Twenty-two of their 37 patients
Caplan and Rosenbaum also pointed out that patients had reached maximum deficit within 24 hours, and
with known basilar occlusion may survive without dis- some other patients progressed over a period of 4
abling neurological sequelae. The present report seeks days. No patient had progression of signs after 1
to extend and explain that finding. week, and there were no known late exacerbations.
The initial period of TIAs, in group 1 patients, Since little data exist concerning the clinical tempo
likely represents diminished flow referable to vascular of angiographically verified vertebrobasilar occlusion,
stenosis. When occlusion of the vertebral or basilar it will be useful to compare the clinical course of our
artery becomes complete, a hemodynamically un- patients with that of patients with known occlusion of
stable situation develops in which collateral circula- the internal carotid artery (a vessel of comparable size
tion must develop quickly or there will occur irreversi- and length). Fourteen patients, personally examined,
ble ischemia of brainstem, cerebellum, or posterior with angiographically documented occlusion of the in-
cerebral territory hemispheral tissue. During this ternal carotid artery were followed an average of 3
period of development of collateral circulation (1-21 years. Eight had TIAs, 2 sudden onset deficits, and 4
days), hemodynamic changes (arrhythmia, bleeding, gradually progressive onset over days. Fluctuations of
or hypotension) and alteration of position may be clinical deficit occurred during the first 2 weeks but the
critical. 8 ' 9 The slight changes in cerebral blood flow patients remained stable thereafter irrespective of
which occur on sitting may be enough in these patients treatment (8 untreated). Two of these patients had late
with marginal vascular compensation to produce (greater than 1 year post-stroke) episodes of
clinical ischemia. Positional ischemia has been limited amaurosis fugax; each, in addition to the carotid
to patients with basilar or bilateral vertebral occlusion occlusion, had severe stenosis of the ipsilateral exter-
and has not been seen in patients with unilateral nal carotid artery and 1 had, in addition, stenosis c{
vertebral occlusion, presumably because of an ade- the ophthalmic artery. No patient developed a late
quate contralateral vertebral supply. As thrombosis permanent or transient central nervous system deficit
occurs, embolization distally within the vertebro- on the side of prior carotid occlusion. Barnett and
basilar system may lead to sudden posterior circula- Aldis12 specifically studied the question of delayed
tion clinical deficit. Embolization distally is the cerebral ischemia distal to occlusion of a major
presumed mechanism of presentation in our group 2 cerebral artery. Of 426 patients, there were only 12 oc-
patients with sudden onset deficits, and in patient 5 currences of subsequent events, 4 within the first 2
with a sudden deficit following TIAs in whom nonfill- weeks (1.9% late occurrence). Of the late occurrences
ing of the left superior cerebellar artery (a clinically 3 were amaurosis fugax alone, 6 were cerebral alone
affected vascular territory) favored an embolic and 3 were amaurosis fugax and cerebral. One patient
mechanism. Embolization in the posterior circulation had common carotid stenosis ipsilateral to an internal
has been documented on postmortem examination by carotid artery occlusion but episodes ceased after
others.10 Meyer et al.6 and Sundt, Whisnant et al.9 complete common carotid artery occlusion. In 3
have also emphasized the role of emboli arising from patients documented hemodynamic changes occurred
proximal vertebrobasilar occlusion. After a period of (2 postural hypotension and 1 ventricular arrhythmia).
several weeks, a stable collateral circulation develops Barnett13 subsequently reported that 25 of 235 patients
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
282 STROKE VOL 10, No 3, MAY-JUNE 1979
enrolled in a cooperative study of antiplatelet aggrega- (weeks or a few months) anticoagulation may be
tion drugs had cerebral ischemia subsequent to known hypothetically useful in preventing embolization or
occlusion. One of these patients had a basilar artery acute extension of the clot. A clinical trial of conserva-
occlusion, and another a bilateral vertebral artery tive medical therapy with short term anticoagulation
occlusion in the neck. Barnett and Aldis12 and or agents which decrease platelet agglutination (e.g.,
Barnett13 expressed the belief that late episodes aspirin, dipyridamole, or sulfinpyrazone) seems
represented embolic material breaking off from the worthy of consideration as opposed to the present
top of the prior occlusion, or, more commonly, em- practice in many centers of long term warfarin
bolization from diseased external or common carotid therapy. Intracranial bypass grafts (e.g., occipital to
collateral supply. In other series of patients with PICA shunts) might be reserved for those unusual
carotid occlusion reported in the literature late patients with documented extensive stenosis of major
episodes occasionally occurred but insufficient details vertebral or basilar vessels with repeated episodes of
were given regarding the nature and locus of the late ischemia unresponsive to conservative treatment.
ischemia.
The patient population reported herein represents a References
selected group of patients with vertebrobasilar disease
all were angiographically studied with documented 1. Kubik CS, Adams RD: Occlusion of the basilar artery a
occlusion of the vertebral or basilar arteries and all clinical and pathological study. Brain 69: 73-121, 1946
survived long enough for follow up. During the same 2. Marshall J: The natural history of transient ischemic cerebro-
vascular attacks. Quart J Med 33: 309-324, 1964
period, 5 patients with angiographically documented 3. Fisher CM, Karnes W, Kubik C: Lateral medullary infarction,
disease died, and 10 patients with severe brainstem in- the pattern of vascular occlusion. J Neuropathol Exp Neurol
farction died without angiography. In addition, our 20: 323-379, 1961
patients' course does not represent the natural course 4. Caplan L, Rosenbaum A: Role of cerebral angiography in
vertebrobasilar occlusive disease. J Neurol Neurosurg
of illness since 8 patients have received temporary or Psychiatry 38: 601-612, 1975
long term anticoagulation. Nevertheless, 2 conclu- 5. Meyer JS, Sheehan S, Bauer R: An arteriographic study of
sions seem warranted from our clinical material: cerebrovascular disease in man. 1. Stenosis and occlusion of the
1) Some patients with occlusion of the basilar vertebrobasilar arterial system. Arch Neurol 2: 27-45, 1960
6. Archer C, Horenstein S: Basilar artery occlusion; clinical and
artery survive with little or no deficit. radiological correlation. Stroke 8: 383-390, 1977
2) In occlusive disease of the posterior circulation, 7. Mohr J, Caplan L, Melski J, et al: The Harvard Cooperative
just as is true in patients with occlusion of the internal Stroke Registry: A prospective registry, Neurology (Minneap)
carotid artery, the critical period for acquisition of a 28: 754-762, 1978
central nervous system deficit is at the time of occlu- 8. Caplan L, Sergay S: Positional cerebral ischemia. J Neurol
Neurosurg Psychiatry 39: 385-391, 1976
sion. The degree of deficit depends primarily on the 9. Sundt T, Whisnant J, Piepgras D, Campbell J, Holman C: In-
development of adequate collateral circulation and the tracranial bypass grafts for vertebrobasilar ischemia. Mayo
presence of distal embolization at the time of occlu- Clin Proc 53: 12-18, 1978
sion. 10. Castaigne P, Lhermitte F, Gautier JC, et al: Arterial occlusion
in vertebrobasilar system: A study of 44 patients with post-
Our data suggest that in the group of patients with mortem data. Brain 96: 133-154, 1973
documented occlusion of the basilar artery a period of 11. Jones HR, Millikan CH, Sandok B: Temporal profile of acute
bedrest in the supine position, with maintenance of vertebrobasilar system infarction. Stroke 9: 109, 1978 (abs)
systemic blood pressure, is important. Occlusion of a 12. Barnett HJM, Aldis E: Delayed cerebral ischemic episodes dis-
vertebral artery, in the presence of a patent con- tal to occlusion of major cerebral arteries. Neurology
(Minneap) 25: 370, 1975
tralateral vertebral artery, usually is associated with a 13. Barnett HJM: Delayed cerebral ischemic episodes distal to
nonprogressive clinical course unless distal emboliza- occlusion of major cerebral arteries. Neurology (Minneap) 28:
tion occurs in the weeks after occlusion. Short term 769-774, 1978
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
Occlusion of the vertebral or basilar artery. Follow up analysis of some patients with benign
outcome.
L R Caplan
Stroke. 1979;10:277-282
doi: 10.1161/01.STR.10.3.277
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 1979 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/10/3/277
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is
available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/
Downloaded from http://stroke.ahajournals.org/ by guest on July 17, 2016
Вам также может понравиться
- PAPER (ENG) - Cardiovascular Risk Profile and Cognitive Function in Young, Middle-Aged, and Elderly SubjectsДокумент14 страницPAPER (ENG) - Cardiovascular Risk Profile and Cognitive Function in Young, Middle-Aged, and Elderly SubjectsAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Coordination of Respiration and Swallowing For Volitional and Reflex Swallows - A Pilot StudyДокумент11 страницPAPER (ENG) - The Coordination of Respiration and Swallowing For Volitional and Reflex Swallows - A Pilot StudyAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Cardiac Disease Increases Risk of Non-Amnestic Mild Cognitive Impairment - Stronger Impact in WomenДокумент17 страницPAPER (ENG) - Cardiac Disease Increases Risk of Non-Amnestic Mild Cognitive Impairment - Stronger Impact in WomenAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - New Subtype of Spinocerebellar Ataxia With Altered Vertical Eye Movements Mapping To Chromosome 1p32Документ9 страницPAPER (ENG) - New Subtype of Spinocerebellar Ataxia With Altered Vertical Eye Movements Mapping To Chromosome 1p32Aldo Hip NaranjoОценок пока нет
- PAPER (ENG) - (Alencar M., Et Al., 2012 BRA) Correlation Between Brain Injury and Dysphagia in Adult Patients With StrokeДокумент9 страницPAPER (ENG) - (Alencar M., Et Al., 2012 BRA) Correlation Between Brain Injury and Dysphagia in Adult Patients With StrokeAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Swallowing Dysfunction in Patients Receiving Prolonged Mechanical VentilationДокумент6 страницPAPER (ENG) - Swallowing Dysfunction in Patients Receiving Prolonged Mechanical VentilationAldo Hip NaranjoОценок пока нет
- Predictors of Cognitive Impairment in An Early Stage Parkinson S Disease CohortДокумент9 страницPredictors of Cognitive Impairment in An Early Stage Parkinson S Disease CohortGeorgiana PrisoschiОценок пока нет
- PAPER (ENG) - Life-Span Cognitive Activity, Neuropathologic Burden, and Cognitive AgingДокумент8 страницPAPER (ENG) - Life-Span Cognitive Activity, Neuropathologic Burden, and Cognitive AgingAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Early Impact of Feeding On Infant Breathing-Swallowing CoordinationДокумент7 страницPAPER (ENG) - The Early Impact of Feeding On Infant Breathing-Swallowing CoordinationAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Safety of FEESST - An Analysis of 500 Consecutive EvaluationsДокумент7 страницPAPER (ENG) - The Safety of FEESST - An Analysis of 500 Consecutive EvaluationsAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Presentation and Management of Laryngeal Cleft - A 10 Years ExperienceДокумент7 страницPAPER (ENG) - The Presentation and Management of Laryngeal Cleft - A 10 Years ExperienceAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Tracheostomy Decannulation and Cough Peak Flows in Patients With Neuromuscular WeaknessДокумент5 страницPAPER (ENG) - Tracheostomy Decannulation and Cough Peak Flows in Patients With Neuromuscular WeaknessAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Dysphagia Outcome and Severity Scale (DOSS Scale)Документ8 страницPAPER (ENG) - The Dysphagia Outcome and Severity Scale (DOSS Scale)Aldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Stimulation of Sucking and Swallowing To Promote Oral Feeding in Premature InfantsДокумент3 страницыPAPER (ENG) - Stimulation of Sucking and Swallowing To Promote Oral Feeding in Premature InfantsAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaДокумент5 страницPAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Accuary of The Modified Evan's Bue Dye Test in Predicting AspirationДокумент5 страницPAPER (ENG) - The Accuary of The Modified Evan's Bue Dye Test in Predicting AspirationAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - New Subtype of Spinocerebellar Ataxia With Altered Vertical Eye Movements Mapping To Chromosome 1p32Документ9 страницPAPER (ENG) - New Subtype of Spinocerebellar Ataxia With Altered Vertical Eye Movements Mapping To Chromosome 1p32Aldo Hip NaranjoОценок пока нет
- PAPER (ENG) - The Early Feeding Skills Assessment For Preterm InfantsДокумент15 страницPAPER (ENG) - The Early Feeding Skills Assessment For Preterm InfantsAldo Hip NaranjoОценок пока нет
- Dysphagia Handicap Index, Development and ValidationДокумент7 страницDysphagia Handicap Index, Development and ValidationWlf OoОценок пока нет
- PAPER (ENG) - Swallowing Disorders in Clinical Practice - Funtional Anatomy, Assessment and Rehabilitation StrategiesДокумент7 страницPAPER (ENG) - Swallowing Disorders in Clinical Practice - Funtional Anatomy, Assessment and Rehabilitation StrategiesAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Pseudodysphagia Due To Omohyoid Muscle SyndromeДокумент6 страницPAPER (ENG) - Pseudodysphagia Due To Omohyoid Muscle SyndromeAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Screening Test For Silent Aspiration at The BedsideДокумент8 страницPAPER (ENG) - Screening Test For Silent Aspiration at The BedsideAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Speech-Language Pathologist-Led Fiberoptic Endoscopic Evaluation of Swallowing Functional Outcomes For Patients After StrokeДокумент6 страницPAPER (ENG) - Speech-Language Pathologist-Led Fiberoptic Endoscopic Evaluation of Swallowing Functional Outcomes For Patients After StrokeAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Mechanics of Sucking - Comparison Between Bottle Feeding and BreastfeedingДокумент8 страницPAPER (ENG) - Mechanics of Sucking - Comparison Between Bottle Feeding and BreastfeedingAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Otolaryngology and Speech Therapy Evaluation in The Assessment of Oropharyngeal Dysphagia - A Combined Protocol ProposalДокумент13 страницPAPER (ENG) - Otolaryngology and Speech Therapy Evaluation in The Assessment of Oropharyngeal Dysphagia - A Combined Protocol ProposalAldo Hip NaranjoОценок пока нет
- PAPER (ENG) - Relevance of Subcortical Stroke in DysphagiaДокумент6 страницPAPER (ENG) - Relevance of Subcortical Stroke in DysphagiaAldo Hip NaranjoОценок пока нет
- 6th Central Pay Commission Salary CalculatorДокумент15 страниц6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- PAPER (ENG) - Predictors of Nutritive Sucking in Preterm InfantsДокумент11 страницPAPER (ENG) - Predictors of Nutritive Sucking in Preterm InfantsAldo Hip NaranjoОценок пока нет
- Measuring Breathing and Swallowing Coordination in Human Infants Using The Kay Elemetrics Swallowing WorkstationДокумент9 страницMeasuring Breathing and Swallowing Coordination in Human Infants Using The Kay Elemetrics Swallowing WorkstationAldo Hip NaranjoОценок пока нет
- Jpts 27 3355Документ3 страницыJpts 27 3355Gabriel GonzalezОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Logic ModelДокумент2 страницыLogic ModelstojannaОценок пока нет
- Aris Wand Brochure (39555 V1)Документ4 страницыAris Wand Brochure (39555 V1)mohitpriyank2003Оценок пока нет
- Visa Application FAQ-SummerДокумент8 страницVisa Application FAQ-SummerCaioAndradeОценок пока нет
- Prof Nik Marzuki Data PDFДокумент3 страницыProf Nik Marzuki Data PDFsue labanОценок пока нет
- Situation Analysis: Children in Bangsamoro Autonomous Region in Muslim MindanaoДокумент335 страницSituation Analysis: Children in Bangsamoro Autonomous Region in Muslim MindanaoTerence YuОценок пока нет
- POCSOДокумент15 страницPOCSOThakur Avnish Singh100% (1)
- Job Contract Agreement Letter PDFДокумент4 страницыJob Contract Agreement Letter PDFQazi Yusuf100% (1)
- Draft Scoping DocumentДокумент10 страницDraft Scoping DocumentJohn N. AllegroОценок пока нет
- ROICAM7 BookletДокумент99 страницROICAM7 BookletPopy HalifahОценок пока нет
- Trastorno de AdaptacionДокумент11 страницTrastorno de AdaptacionEduardo AguilarОценок пока нет
- Outpatient Dental & Clinical - Claim FormДокумент1 страницаOutpatient Dental & Clinical - Claim FormYiki TanОценок пока нет
- FeverДокумент2 страницыFeverMuhammad Jefri LukmanОценок пока нет
- 276) 2010 Cerio - Mechanism Action Clinical Benefits Colloidal Oatmeal Dermatologic PracticeДокумент5 страниц276) 2010 Cerio - Mechanism Action Clinical Benefits Colloidal Oatmeal Dermatologic Practicezebulon78Оценок пока нет
- Evacuation Earthquake PlanДокумент9 страницEvacuation Earthquake PlanShane Giacinth AmarilaОценок пока нет
- MSDS Dross AluminiumДокумент18 страницMSDS Dross AluminiumNurul muzayyanahОценок пока нет
- Clinical Gaze Through The Prism of LiteratureДокумент10 страницClinical Gaze Through The Prism of LiteratureZedarОценок пока нет
- Physical Science - 11 - Q1 - 13 - Use of The Other Ingredients in Cleaning Agents 08082020Документ18 страницPhysical Science - 11 - Q1 - 13 - Use of The Other Ingredients in Cleaning Agents 08082020gwynceОценок пока нет
- HSE Assignment 3 FinalДокумент21 страницаHSE Assignment 3 FinalLuqman HakimОценок пока нет
- School Canteen Feeding Program 2019 2020 K 6 1Документ20 страницSchool Canteen Feeding Program 2019 2020 K 6 1MaryRoseTrinidadОценок пока нет
- Root Caries: A Periodontal Perspective: Review ArticleДокумент21 страницаRoot Caries: A Periodontal Perspective: Review ArticleIlmia AmaliaОценок пока нет
- Therapy General Objective Specific Objective Indication Activities Rationale Dance Therapy 1. Jumping RhythmsДокумент2 страницыTherapy General Objective Specific Objective Indication Activities Rationale Dance Therapy 1. Jumping RhythmsSabrina Porquiado Magañan SNОценок пока нет
- Ekso 1Документ8 страницEkso 1HASANUDDIN STОценок пока нет
- Agama Dan Spiritualitas Dalam Konteks Kesehatan Dan KeperawatanДокумент28 страницAgama Dan Spiritualitas Dalam Konteks Kesehatan Dan KeperawatanSELVI AQILAHОценок пока нет
- Salt Sole Himalayan Salt SolutionДокумент1 страницаSalt Sole Himalayan Salt Solutionwa waОценок пока нет
- Cancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Документ10 страницCancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Pilar AufrastoОценок пока нет
- From The Cocoon To The ButterflyДокумент26 страницFrom The Cocoon To The ButterflyParamita BanerjeeОценок пока нет
- Microbial Content and Diversity Inseveral Tempe From Bogor AreasДокумент9 страницMicrobial Content and Diversity Inseveral Tempe From Bogor AreasCendra KammiОценок пока нет
- Antibiotic Use in Food Animals Worldwide, With A Focus On Africa - Pluses and MinusesДокумент8 страницAntibiotic Use in Food Animals Worldwide, With A Focus On Africa - Pluses and MinusesxubicctОценок пока нет
- Ethiopia - Design Gudeline Final - OromiaДокумент71 страницаEthiopia - Design Gudeline Final - OromiaEphrem Gizachew100% (15)
- Medihuanna Brand GuidelinesДокумент71 страницаMedihuanna Brand GuidelinespuskickОценок пока нет