Академический Документы
Профессиональный Документы
Культура Документы
Pharmacology Handout
Загружено:
Mark Elben Teodoro100%(1)100% нашли этот документ полезным (1 голос)
266 просмотров5 страницPharmacology Handout
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документPharmacology Handout
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
100%(1)100% нашли этот документ полезным (1 голос)
266 просмотров5 страницPharmacology Handout
Загружено:
Mark Elben TeodoroPharmacology Handout
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
PHARMACOLOGY AMPHETAMINES
increase the release of catecholamines
JOHN J. TEODORO PTRP, RN (NE from stored sites in nere terminals)
Block the re-uptake of dopamine & NE
Analgesics
following release into the synapse, &
1. NARCOTIC AGONISTS
inhibit the action of MAO
2. NARCOTIC PARTIAL AGONISTS; NARCOTIC
Increase stimulating effect on cerebral
ANTAGONISTS
cortex & RAS
3. NON-STEROIDAL ANTI-
DOXAPRAM (DOPRAM)
INFLAMMATORY
METHYLPHEMDATE Hcl (Ritalin)
4. MISCELLANEOUS ANALGESIC AGENTS
PEMOLINE (Cylert)
CAFFEIN
Anxiolytics
Librium watch for signs of leukopenia,
Anticholinergic med
hypotension
Equanil metabolizes extensively in the liver &
benztropine mesylate (Cogentin), biperiden
interferes w/ liver function tests.
HCl (Akineton) Trihexyphenidyl HCl (Artane),
- decreases PT if on coumadin
scopolamine, atropine
Atarax - does not cause tolerance & can be
*Block cholinergic receptors in the CNS,
used
thereby suppressing
temporarily when other anti-
acetylcholine activity
anxiety
*A/R: blurred vision, dry mouth & secretions,
agents have been abused
urinary retention,
Serax useful for treating elderly clients. Does
constipation, restlessness & confusion
not rely on liver for metabolism
*Client to have regular eye check up for
increase in IOP
Anticonvulsants
*Avoid aspirin, caffeine, smoking & ROH to
BARBITURATES
decrease gastric
*treat grandmal seizures ; tonic-clonic
acidity
seizure
BENZODIAZEPINES
CARDIAC DRUGS
*diazepam is DOC for Rx of STATUS
EPILIPTICUS
Beta adrenergic Blockers
*clorazepate is use w/ other
*Inhibit response to beta-adrenergic
antiepileptic agents to control partial seizures
stimulation
HYDANTOINS
*Block release of epi & NE thus decreasing HR
*Used to depress abnormal neuronal
& BP
charges & prevent spread of seizures
*Used for angina, dysrhythmias, prevention of
*also used to treat dysrhythmias
MI & glaucoma
*A/R: gingival hyperplasia, alopecia,
*A/R: bradycardia, hypotension, weakness &
hyperglycemia, blood dyscracias
fatigue
*Seizure precaution & dental hygiene
*Hold if BP & HR not within parameters
*Give IV with normal saline & never
prescribed by MD
with dextrose
*Not to D/C meds abruptlyrebound HPN,
tachycardia, angina
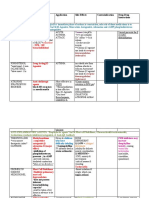
CNS STIMULANTS
*Early signs of hypoglycemia such as
tachycardia & nervousness can be masked by
these drugsmonitor blood sugar
BETA- BLOCKING AGENTS anesthetics to promote prolonged anesthetic
BETA1 ADRENERGIC ( CARDIO SELECTIVE) action by
BLOCKING AGENTS decreased blood flow to area
-acebutolol (Sectral) Adrenergic Agonist
-atenolol (Tenormin, Atenol, isoproterenol (Isuprel)
Premorphine) *Stimulates beta receptors & used for cardiac
-metoprolol (apo-metoprolol, betaloc) stimulation &
BETA1 & 2 ADRENERGIC (nonselective) bronchodilation
BLOCKING AGENTS norepinephrine (Levophed)
-nadolol (corgard) *Stimulates heart in cardiac arrest
-pindolol (visken) *Vasoconstricts & increases BP during
-propranolol( inderal, novopranol) hypotension & shock
-timolol (blocadren, betin, temserin) *A/R: tachycardia, angina, restlessness
*If extravasation occurs, infiltrate with normal
Calcium channel blocker saline &
verapamil (Calan, Isoptin), nifedipine phentolamine (Regitine)
(Procardia) Antianginal meds
felodipine (Plendil), diltiazem (Cardizem) NITRATES
*Decrease cardiac contractility by relaxing nitroglycerin (Nitrostat, Nitrolingual)
smooth muscle nitroglycerin ointment 2% (Nitrol, Transderm-
and the workload of the heartthus Nitro)
decreasing need for O2 *Produce vasodilation & improved myocardial
*Promote vasodilation of coronary & O2 consumption
peripheral vessels *C/I in client with severe hypotension
*A/R: bradycardia, hypotension, dizziness & *A/R: H/A, orthostatic hypotension, dizziness,
lightheadedness weakness & faintness
*Instruct client how to take HR & to inform SUBLINGUAL:
MD if dizziness *Offer sips of H2O since dryness may inhibit
Persists absorption
*Leave under tongue until fully absorbed, not
Adrenergic agonist swallowed
dobutamine (Dobutrex) *Take 1 tab for pain ff q5 mins for a total of 3
*Increases myocardial force & C.O. through doses. If pain not relieved in 15 minutes, seek
beta receptors MD help.. may indicate MI
stimulation *Stinging/burning feeling means tablet is fresh
*Used in clients with CHF TOPICAL
dopamine (Intropin) *Remove ointment from previous dose, rotate
*Increases BP & C.O. & increases renal outflow sites & avoid
through its touching ointment & hairy areas
action on alpha & beta receptors *Squeeze ribbon into prescribed length on
*Treat mild renal failure due to decreased C.O. applicator paper
epinephrine (adrenalin) *Sites: chest, back, abdomen, upper arm &
*Cardiac stimulation during cardiac arrest, anterior thigh
bronchodilation TRANSDERMAL PATCH
asthma & allergy, mydriasis *Apply patch to hairless area, using new patch
*Promotes vasoconstriction when combined & different
with local site every day
*Remove patch after 12-14 hours, allowing 10- *Used for thrombosis, pulmonary embolism &
12 patch- MI
free hours daily to prevent tolerance *C/I in active bleeding except in disseminated
*Stand away from microwave ovens intravascular
Digitalis coagulation (DIC), bleeding disorders, ulcers
DIGITALIS TOXICITY *A/R: hemorrhage, hematuria, epistaxis,
* loss of apetite, nausea, extreme ecchymosis,
fatigue, weakness of the arms & legs, bleeding gums, thrombocytopenia
psychiatric disturbances (nightmares, heparin Na (Liquaemin Na)
agitation, listlessness, or hallucination) or *Prevents thrombin from converting
visual disturbances ( hazy, or blurred vision, fibrinogen to fibrin
difficulty reading & green color) *Prevents thromboembolism
N.I. *Therapeutic dose does not dissolve clots, but
1. Take APICAL PULSE 1 full minute prevents
*dont give for Adult <60/min; new thrombus formation
child < 90 bts/min *Blood levels: normal APTT is 20-36 seconds;
*monitor potassium level maintain APTT is 1.5-2.5 times normal; APTT
specially diuretics therapy should be measured q 4-6H during
digoxin (Lanoxin) initial therapy & then daily
*Inhibit sodium-potassium pump
*positive inotropic action heparin Na
*negative chronotropic action *Monitor clotting time; normal is 8-15
*A/R: anorexia, N/V, visual disturbances minutes; maintain
*Monitor serum therapeutic level 0.5-2.0 clotting time 15-20 minutes
ng/ml; increased *Observe for signs of bleeding
risk of toxicity in clients with hypokalemia *Inject SQ into the abdomen with 25-28g at 90
*Used for CHF, atrial tachycardia, atrial degrees
fibrillation & flutter angle; dont aspirate or rub injection site
*Increase K+ rich food: fresh & dried fruits, *Antidote is protamine SO4
fruit juices, warfarin Na (Coumadin)
vegetables & potatoes *Decreases prothrombin activity & prevents
*Monitor HR & hold if below 60 & above 100 the use of vitamin K by the liver
(adults) *Used for long-term anticoagulation
*Antidote: digoxin immune FAB (Digibind) *Prolongs clotting time & monitor PT
*Life threatening toxicity: ventricular (prothrombin time)
tachycardia, fibrillation, severe sinus *Used mainly to prevent thromboembolitic
bradycardia conditions such
*80% DIGOXIN excreted by kidneys; half life is as thrombophlebitis, pulmonary embolism,
36-120H embolism
*90% DIGITOXIN metabolized by liver; half life caused by heart valve damage, atrial
is 120-210H fibrillation & MI
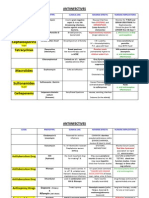
Anticoagulants *Given 2-3 months after an MI to prevent DVT
*Prevent the extension & formation of clots by warfarin Na (Coumadin)
inhibiting *Average PT is 9.6 to 11.8 seconds & normal
factors in the clotting cascade & decreasing INR is 1.3-2.0
blood Goal is to raise the INR to 2 to 3
coagulability *Observe for signs of bleeding
*Antidote: Vitamin K (AquaMEPHYTON)
THROMBOLYTIC MEDS Antacids and Mucousal Lining protectives
*Monitor for bleeding, hypotension &
tachycardia *react with gastric acid to produce neutral
*Avoid injections; apply pressure to puncture salts or salts of low
site for 20-30 minutes acidity
*Handle clients minimally & let clients use *inactivate pepsin and enhance mucosal
electric razors & brush teeth gently protection but do not coal ulcer to protect
*Antidote: aminocaproic acid (Amicar) from acid & pepsin
*used for patients with PUD & GRF
Respiratory Drugs (gastroesophageal reflex disease)
*antacid tablets should be chewed and
Bronchodilator followed with glass of H2O or milk
* Used for allergic rhinitis, acute *administer 1 hour apart from other meds to
bronchospasm, acute & chronic asthma, minimize the chance of drug interactions
bronchitis, COPD, emphysema
Caution with clients with glaucoma & sucralfate (Carafate)
HPN *creates a protective barrier against acid &
* A/R: palpitations, tachycardia, nervousness, pepsin
tremors, restlessness & HA *given po & on an empty stomach
Give RTC to maintain therapeutic *A/R: constipation, impede absorption of
blood level warfarin Na,
* Avoid caffeine products phenytoin, theophylline, digoxin & some
antibiotics
ANTIHISTAMINES administer 2 hours apart from these meds
astemizole (Hismanal), diphenylhydramine magnesium hydroxide (Milk of Magnesia)
(Benadryl) *rapid acting & A/R is diarrhea
loratadine (Claritin) *usually combined with aluminum hydroxide
*Histamine antagonists or H1 blockers; to counter diarrhea
compete with histamine (MAALOX)
for receptor sites preventing histamine aluminum hydroxide (Amphojel, Alu-cap)
response thus *slow acting & A/R: constipation
constricting smooth muscles *with significant Na contentcaution in clients
*Decrease nasopharyngeal secretions & with HPN &
decreases itching which heart failure; reduce effect of tetracyclines,
causes sneezing warfarin Na &
*Used for common colds, rhinitis, urticaria, digoxin
nausea & vomiting, *reduce phosphate absorption
motion sickness & sleep aid
*CNS depressant with ROH, narcotics, calcium carbonate (Tums)
barbiturates & sedatives *rapid acting & A/R: constipation
*Caution with COPD clients & Benadryl C/I in sodium bicarbonate
clients with *rapid onset
glaucoma *A/R: liberates CO2 & increases intra-
*A/R: dizziness, dry mouth, blurred vision abdominal pressure
causing flatulence, caution in clients with HPN
& heart
GIT DRUGS failure, systemic alkalosis in clients with renal
failure
H2 RECEPTOR ANTAGONIST
*suppress secretion of gastric acid
*indicated for PUD & heart burn & for GRF
disease
cimetidine (Tagamet)
*taken on an empty stomach
*administered 1 hour apart from antacids
*crosses the blood-brain barrier & may cause
mental confusion, agitation, anxiety &
disorientation
*dosages of these meds are reduced when
taken together:
warfarin Na, phenytoin, theophyllin &
lidocaine
ranitidine (Zantac)
*not affected by food
*S/E are uncommon & does not cross blood-
brain barrier
Вам также может понравиться
- Pharmacology SlidesДокумент114 страницPharmacology Slidesbrandon15000100% (9)
- NCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsОт EverandNCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsОценок пока нет
- UWORLDNCLEXreview2021 Watermarked PDFДокумент100 страницUWORLDNCLEXreview2021 Watermarked PDFashley100% (1)
- Pharma 12Документ16 страницPharma 12Mary Roan RonatoОценок пока нет
- Antidiarrheal DrugsДокумент4 страницыAntidiarrheal DrugsNadhirah ZulkifliОценок пока нет
- Drug Outline: Autonomic Nervous System Drug Class Drug OtherДокумент4 страницыDrug Outline: Autonomic Nervous System Drug Class Drug OtherCess Lagera YbanezОценок пока нет
- Pharmacology - Section 23 - Antibiotics 2Документ5 страницPharmacology - Section 23 - Antibiotics 2Pathalee ThalpavilaОценок пока нет
- NCLEX Review: Pharmacology Charlene Natale, BSN, RNДокумент43 страницыNCLEX Review: Pharmacology Charlene Natale, BSN, RNMenly Susada100% (1)
- PharmacologyДокумент3 страницыPharmacologyMohd Afiq AizuddinОценок пока нет
- Cardio Q&aДокумент147 страницCardio Q&aHoney Lyn AlebioОценок пока нет
- Cardiovascular System Drugs - Active Stack® Pharmacology Flash Cards - Study Materials - My ATIДокумент1 страницаCardiovascular System Drugs - Active Stack® Pharmacology Flash Cards - Study Materials - My ATIAntonette Joy SolinapОценок пока нет
- PharmacologyДокумент9 страницPharmacologyRPh Krishna Chandra JagritОценок пока нет
- Cholinergic Pharmacology - Drug TableДокумент2 страницыCholinergic Pharmacology - Drug TableFОценок пока нет
- Pharmacology FirecrackerДокумент37 страницPharmacology FirecrackerRehan Usman100% (1)
- Suffixes and PrefixesДокумент2 страницыSuffixes and PrefixesBeckyОценок пока нет
- Drugs SummaryДокумент23 страницыDrugs Summaryapi-3832811100% (1)
- PharmacyДокумент16 страницPharmacyJow RamosОценок пока нет
- Pharm Phlash PDFДокумент207 страницPharm Phlash PDFAdiShine100% (1)
- Angina Pharmacology YeahДокумент16 страницAngina Pharmacology YeahMuhammad AfifuddinОценок пока нет
- Family Names of DrugsДокумент1 страницаFamily Names of DrugsangelОценок пока нет
- 12 Points To Answering Pharmacology Questions PDFДокумент2 страницы12 Points To Answering Pharmacology Questions PDFbsebi763271Оценок пока нет
- Head and NeckkkkkkДокумент7 страницHead and NeckkkkkkJoey A. RumbaoaОценок пока нет
- Pharm Chapter 2 and 3 Study GuideДокумент10 страницPharm Chapter 2 and 3 Study GuideamkОценок пока нет
- Pharmacodynamics 4Документ28 страницPharmacodynamics 4علي المحترفОценок пока нет
- Pall CareДокумент81 страницаPall Careडा. सत्यदेव त्यागी आर्यОценок пока нет
- Table of Sedative, Hypnotic, AntianxietyДокумент4 страницыTable of Sedative, Hypnotic, AntianxietyirfanzukriОценок пока нет
- Pharmacology Important Things To RememberДокумент5 страницPharmacology Important Things To RememberHydie100% (1)
- Classification of Drugs PDFДокумент15 страницClassification of Drugs PDFmuhammad ihtisham ul hassanОценок пока нет
- Anti-Infective Pharmacology ReviewerДокумент5 страницAnti-Infective Pharmacology ReviewerArianne Pearl PrimeroОценок пока нет
- Antidepressants: Depression Is One The Most Treatable Mental IllnessДокумент40 страницAntidepressants: Depression Is One The Most Treatable Mental IllnessMohammed AbdullahОценок пока нет
- Pharmacology A ReviewДокумент15 страницPharmacology A ReviewKathrynne MendozaОценок пока нет
- Drug Name Mechanism Application Side Effects Contraindication Drug-Drug InteractionsДокумент3 страницыDrug Name Mechanism Application Side Effects Contraindication Drug-Drug Interactionsazhar hussinОценок пока нет
- Suffixes and PrefixesДокумент2 страницыSuffixes and PrefixesNiksОценок пока нет
- NCMA216.PHARMA Drugs Acting On The Endocrine SystemДокумент71 страницаNCMA216.PHARMA Drugs Acting On The Endocrine SystemKhams TolentinoОценок пока нет
- Remembering Medication ClassificationsДокумент2 страницыRemembering Medication ClassificationsGVHHОценок пока нет
- Printed Material Module 7 Gastrointestinal System Drugs - PDFДокумент45 страницPrinted Material Module 7 Gastrointestinal System Drugs - PDFShang MacarayonОценок пока нет
- Pharm 2013Документ13 страницPharm 2013Shae Thomas100% (6)
- Chapter 1 - The Nursing Process and Drug TherapyДокумент3 страницыChapter 1 - The Nursing Process and Drug TherapyHaleyОценок пока нет
- Drugs Used in TuberculosisДокумент27 страницDrugs Used in Tuberculosisapi-3705123Оценок пока нет
- Introduction To Nursing PharmacologyДокумент6 страницIntroduction To Nursing PharmacologyArun Roa DanielОценок пока нет
- Pharm Exam ReviewДокумент13 страницPharm Exam ReviewAshleyОценок пока нет
- GIT DrugsДокумент180 страницGIT DrugsMaria Linevel Balderamos Dalida100% (1)
- Pharmacology Notes #1Документ2 страницыPharmacology Notes #1JUSTINE ALLYSA MAY CASTILLOОценок пока нет
- Medication DilutionДокумент23 страницыMedication DilutionamgdanielaОценок пока нет
- Fluid Overload Student PagesДокумент4 страницыFluid Overload Student PagesJess OswaldОценок пока нет
- Antihypertensive Cheat SheetДокумент2 страницыAntihypertensive Cheat SheetRigley GarmanОценок пока нет
- Pharmacology CNS DrugsДокумент15 страницPharmacology CNS DrugsM Youssif Elkady100% (1)
- Introduction To Cns PharmacologyДокумент66 страницIntroduction To Cns PharmacologyYazan Emad Salem100% (1)
- Common Drugs and AntidotesДокумент2 страницыCommon Drugs and AntidotesreynoldОценок пока нет
- Drug Card Solu-MEDROLДокумент2 страницыDrug Card Solu-MEDROLBenОценок пока нет
- Labs 1.19 ABG AnalysisДокумент1 страницаLabs 1.19 ABG AnalysisMonica GonzalezОценок пока нет
- Antiarrhythmic Drugs Classification (Vaughan Williams)Документ8 страницAntiarrhythmic Drugs Classification (Vaughan Williams)ana100% (1)
- ATI Flash Cards 05, Medications Affecting The Nervous SystemДокумент110 страницATI Flash Cards 05, Medications Affecting The Nervous SystemGiovanni MictilОценок пока нет
- Pharmacology Notes (Chapter 20 and 21)Документ2 страницыPharmacology Notes (Chapter 20 and 21)graycorypОценок пока нет
- Drug KenalogДокумент1 страницаDrug KenalogSrkocherОценок пока нет
- Northern Ireland Management of Infection Guidelines For Primary and Community Care 2016Документ48 страницNorthern Ireland Management of Infection Guidelines For Primary and Community Care 2016dreneavalentinstefanОценок пока нет
- Pain Med ChartsДокумент4 страницыPain Med ChartsNursingSchoolNotesОценок пока нет
- Drug Names - Stems, Prefixes, Roots and Suffixes - NCLEX MasteryДокумент5 страницDrug Names - Stems, Prefixes, Roots and Suffixes - NCLEX MasteryMarcel YoungОценок пока нет
- Antiinfectives Drug TableДокумент5 страницAntiinfectives Drug Tablecdp1587100% (3)
- HANDOUT1Документ6 страницHANDOUT1Mark Elben TeodoroОценок пока нет
- Or Nursing 2Документ4 страницыOr Nursing 2Mark Elben TeodoroОценок пока нет
- Or NursingДокумент6 страницOr NursingMark Elben TeodoroОценок пока нет
- RN HealsДокумент2 страницыRN HealsMark Elben TeodoroОценок пока нет
- Test Bank For General Organic and Biochemistry An Applied Approach 2nd Edition ArmstrongДокумент15 страницTest Bank For General Organic and Biochemistry An Applied Approach 2nd Edition Armstrongrowancong0f3pОценок пока нет
- DR Erwin Sukandi, SPPD, K-KV BelumДокумент47 страницDR Erwin Sukandi, SPPD, K-KV BelumrajaalfatihОценок пока нет
- Side Effects of Calcium Channel Blockers: R. Patterson RussellДокумент3 страницыSide Effects of Calcium Channel Blockers: R. Patterson RussellLivia GudacОценок пока нет
- 2018.docx Version 1Документ92 страницы2018.docx Version 1Afsal Ur FriendОценок пока нет
- Complications of Thoracic SurgeryДокумент45 страницComplications of Thoracic SurgeryAlin ToaderОценок пока нет
- Nuclear Stress Test Instructions 1Документ2 страницыNuclear Stress Test Instructions 1Maria EdelОценок пока нет
- Guaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsДокумент2 страницыGuaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsAmberОценок пока нет
- Tacrolimus Ointment Is Used To Treat The Symptoms of EczemaДокумент2 страницыTacrolimus Ointment Is Used To Treat The Symptoms of EczemaSharan SahotaОценок пока нет
- Drugs Affecting Blood PressureДокумент54 страницыDrugs Affecting Blood PressureJeremy VivitОценок пока нет
- Cardiac DripsДокумент7 страницCardiac DripsCeara MillasОценок пока нет
- MCQ On Cardiology IДокумент84 страницыMCQ On Cardiology IHarsh Oak50% (2)
- Diltiazem - ProfileДокумент14 страницDiltiazem - Profileumamaheswararao4Оценок пока нет
- Cardiovascular PharmacologyДокумент77 страницCardiovascular PharmacologyDhruva PatelОценок пока нет
- Practice Exam 1 HESIДокумент10 страницPractice Exam 1 HESIdinkinspdd50% (2)
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreДокумент112 страницOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYC100% (2)
- DRUG INDEX CompiledДокумент24 страницыDRUG INDEX Compiledahmad aliОценок пока нет
- New Question for MoH Prometric Exam تمДокумент7 страницNew Question for MoH Prometric Exam تمsundus951100% (1)
- 0905 (1) When Cardiovascular Medications Become ToxinsДокумент20 страниц0905 (1) When Cardiovascular Medications Become ToxinsjojoleroОценок пока нет
- ACLS DrugsДокумент16 страницACLS Drugstostc100% (2)
- Reflective Journal 1Документ3 страницыReflective Journal 1api-380537580Оценок пока нет
- Cardiac Drug FunctionДокумент2 страницыCardiac Drug FunctionShanda Rieder KozickiОценок пока нет
- 2017 Medical Pharmacology Practice Exam 4Документ6 страниц2017 Medical Pharmacology Practice Exam 4Franklin garryОценок пока нет
- MCQs For Prometric Examination PDFДокумент155 страницMCQs For Prometric Examination PDFYacine Tarik AizelОценок пока нет
- Cardiovascular Agent: Prof. Clement Belvis RN, RM, MPHДокумент86 страницCardiovascular Agent: Prof. Clement Belvis RN, RM, MPHEimhie Lee CasiОценок пока нет
- Lesson 1 Cardiac Glycosides, Antianginals, and Antidysrhythmics - AntiarrhythmmicsДокумент40 страницLesson 1 Cardiac Glycosides, Antianginals, and Antidysrhythmics - AntiarrhythmmicsXiamen Magsino NolascoОценок пока нет
- Herbesser StrokeДокумент15 страницHerbesser StrokePrincess MiraОценок пока нет
- Guaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsДокумент2 страницыGuaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsCarl LeeОценок пока нет
- DRUGS Initial StockДокумент163 страницыDRUGS Initial StockdeasyОценок пока нет
- Cardialgia. Chronic Coronary DiseaseДокумент75 страницCardialgia. Chronic Coronary DiseaseВиктория ПашаеваОценок пока нет
- SDL Obat EmergencyДокумент26 страницSDL Obat EmergencyfarhantunichiaОценок пока нет
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassОт EverandTroubled: A Memoir of Foster Care, Family, and Social ClassРейтинг: 4.5 из 5 звезд4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingОт EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingРейтинг: 4 из 5 звезд4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (253)