Академический Документы
Профессиональный Документы
Культура Документы
Parkinson
Загружено:
EricsonMitraАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Parkinson
Загружено:
EricsonMitraАвторское право:
Доступные форматы
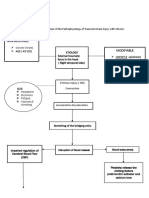
Parkinsons Disease Assessment and Diagnostic Methods
Parkinsons disease is a slowly progressive degenerative Patients history and presence of two of the four cardinal
neurologic disorder affecting the brain centers that are manifestations: tremor, rigidity, bradykinesia, and postural
responsible for control and regulation of movement. The changes.
degenerative or idiopathic form of Parkinsons disease is the Positron emission tomography (PET) and single photon
most common; there is also a secondary form with a known or emission computed tomography (SPECT) scanning have
suspected cause. The cause of the disease is mostly unknown been helpful in understanding the disease and advancing
but research suggests several causative factors (eg, genetics, treatment.
atherosclerosis, viral infections, head trauma). The disease Medical history, presenting symptoms, neurologic
usually first appears in the fifth decade of life and is the fourth examination, and response to pharmacologic management
most common neurodegenerative disease. are carefully evaluated when making the diagnosis.
Pathophysiology Medical Management
Parkinsons disease is associated with decreased levels of Goal of treatment is to control symptoms and maintain functional
dopamine resulting from destruction of pigmented neuronal cells independence; no approach prevents disease progression.
in the substantia nigra in the basal ganglia region of the brain.
The loss of dopamine stores in this area of the brain results in Pharmacologic Therapy
more excitatory neurotransmitters than inhibitory neuro- Levodopa (Larodopa) is the most effective agent and the
transmitters, leading to an imbalance that affects voluntary mainstay of treatment.
movement. Cellular degeneration causes impairment of the Anticholinergic agents (eg, trihexyphenidyl HCl [Artane],
extrapyramidal tracts that control semiautomatic functions and benztropine mesylate [Cogentin]) to control tremor and
coordinated movements; motor cells of the motor cortex and the rigidity.
pyramidal tracts are not affected. Amantadine hydrochloride (Symmetrel), an antiviral agent, to
reduce rigidity, tremor, and bradykinesia.
Clinical Manifestations Dopamine agonists (eg, pergolide [Permax], bromocriptine
The cardinal signs of Parkinsons disease are tremor, rigidity, mesylate [Parlodel]), ropinirole, and pramipexole are used to
bradykinesia (abnormally slow movements), and postural postpone the initiation of carbidopa and levodopa therapy.
instability. Monoamine oxidase inhibitors (MAOIs) (eg, selegiline
Resting tremors: a slow, unilateral turning of the forearm and [Eldepryl], rasagiline [Azilect]) to inhibit dopamine
hand and a pill-rolling motion of the thumb against the breakdown.
fingers; tremor at rest and increasing with concentration and Catechol-O-methyltransferase (COMT) inhibitors (eg,
anxiety. entacapone [Comtan], tolcapone [Tasmar]) to reduce motor
Resistance to passive limb movement characterizes muscle fluctuation.
rigidity; passive movement may cause the limb to move in Antidepressant drugs (eg, amitriptyline HCl [Elavil]).
jerky increments (lead-pipe or cog-wheel movements); Antihistamine drugs (eg, diphenhydramine [Benadryl]) to
stiffness of the arms, legs, face, and posture are common; allay tremors.
involuntary stiffness of passive extremity increases when
another extremity is engaged in voluntary active movement. Surgical Management
Impaired movement: Bradykinesia includes difficulty in Surgery to destroy a part of the thalamus (stereotactic
initiating, maintaining, and performing motor activities. thalamotomy and pallidotomy) to interrupt nerve pathways
Loss of postural reflexes, shuffling gait, loss of balance and alleviate tremor or rigidity.
(difficulty pivoting); postural and gait problems place the Transplantation of neural cells from fetal tissue of human or
patient at increased risk for falls. animal source to reestablish normal dopamine release.
Deep brain stimulation with pacemakerlike brain implants to
Other Characteristics block nerve pathways in the brain that cause tremors.
Autonomic symptoms that include excessive and
uncontrolled sweating, paroxysmal flushing, orthostatic Nursing Diagnoses
hypotension, gastric and urinary retention, constipation, and Impaired physical mobility related to muscle rigidity and
sexual dysfunction. motor weakness
Psychiatric changes may include depression, dementia, Self-care deficits (eating, drinking, dressing, hygiene, and
delirium, and hallucinations; psychiatric manifestations may toileting) related to tremor and motor disturbance
include personality changes, psychosis, and acute Constipation related to medication and reduced activity
confusion. Imbalanced nutrition: less than body requirements related to
Auditory and visual hallucinations may occur. tremor, slowness in eating, difficulty in chewing and
Hypokinesia (abnormally diminished movement) is common. swallowing
As dexterity declines, micrographia (small handwriting) Impaired verbal communication related to decreased speech
develops. volume, slowness of speech, inability to move facial muscles
Masklike facial expression. Ineffective coping related to depression and dysfunction due
Dysphonia (soft, slurred, low-pitched, and less audible to disease progression
speech).
Other nursing diagnoses may include sleep pattern
Stages of Parkinsons Disease disturbances, deficient knowledge, risk for injury, risk for activity
intolerance, disturbed thought processes, and compromised
I. Unilateral flexion of upper extremities
family coping.
II. Shuffling gait
III. Progressive difficulty in ambulating
IV. Progressive weakness
V. Disability = last stage
Nursing Interventions Provide continuous encouragement and reassurance.
Assist and encourage patient to set achievable goals.
Improving Mobility Encourage patient to carry out daily tasks to retain
Help patient plan progressive program of daily exercise to independence.
increase muscle strength, improve coordination and
dexterity, reduce muscular rigidity, and prevent contractures.
Encourage exercises for joint mobility (eg, stationary bike,
walking).
Instruct in stretching and range-of-motion exercises to
increase joint flexibility. Prepared by:
Encourage postural exercises to counter the tendency of the
head and neck to be drawn forward and down. Teach patient ERICSON C. MITRA
to walk erect, watch the horizon, use a wide-based gait, BSN IV Student
swing arms with walking, walk heel-toe, and practice
marching to music. Also encourage breathing exercises
while walking and frequent rest periods to prevent fatigue or
frustration.
Advise patient that warm baths and massage help relax
muscles.
Enhancing Self-Care Activities
Encourage, teach, and support patient during activities of
daily living.
Modify environment to compensate for functional disabilities;
adaptive devices may be useful.
Enlist assistance of an occupational therapist as indicated.
Improving Bowel Elimination
Establish a regular bowel routine.
Increase fluid intake; eat foods with moderate fiber content.
Provide raised toilet seat for easier toilet use.
Improving Swallowing and Nutrition
Promote swallowing and prevent aspiration by having patient
sit in upright position during meals.
Provide semisolid diet with thick liquids that are easier to
swallow.
Teach patient to place the food on the tongue, close the lips
and teeth, lift the tongue up and then back, and swallow;
encourage patient to chew first on one side of the mouth and
then on the other.
Remind patient to hold head upright and to make a conscious
effort to swallow to control buildup of saliva.
Monitor patients weight on a weekly basis.
Provide supplementary feeding and, as disease progresses,
tube feedings.
Consult a dietitian regarding patients nutritional needs.
Encouraging Use of Assistive Devices
An occupational therapist can assist in identifying
appropriate adaptive devices.
Useful devices may include an electric warming tray that
keeps food hot and allows the patient to rest during the
prolonged time that it may take to eat; special utensils; a
plate that is stabilized, a nonspill cup, and eating utensils.
Improving Communication
Remind patient to face the listener, speak slowly and
deliberately, and exaggerate pronunciation of words; a small
electronic amplifier is helpful if the patient has difficulty being
heard.
Instruct patient to speak in short sentences and take a few
breaths before speaking.
Enlist a speech therapist to assist the patient.
Supporting Coping Abilities
Encourage faithful adherence to exercise and walking
program; point out activities that are being maintained
through active participation.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- NCP NANDA: Nursing Diagnosis and Interventions for Urinary Tract InfectionДокумент4 страницыNCP NANDA: Nursing Diagnosis and Interventions for Urinary Tract InfectionEricsonMitra0% (2)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Print 01Документ11 страницPrint 01EricsonMitraОценок пока нет
- APA CitationДокумент79 страницAPA CitationEricsonMitraОценок пока нет
- PBLДокумент3 страницыPBLEricsonMitraОценок пока нет
- PMRДокумент6 страницPMREricsonMitraОценок пока нет
- PMRДокумент6 страницPMREricsonMitraОценок пока нет
- CAP TableДокумент2 страницыCAP TableEricsonMitraОценок пока нет
- How Nursing Leadership Styles Can Impact Patient Outcomes and Organizational Performance - Bradley University OnlineДокумент7 страницHow Nursing Leadership Styles Can Impact Patient Outcomes and Organizational Performance - Bradley University OnlineEricsonMitraОценок пока нет
- TITLE SchizoДокумент3 страницыTITLE SchizoEricsonMitraОценок пока нет
- PPP TbiiiДокумент3 страницыPPP TbiiiEricsonMitraОценок пока нет
- Top 10 Rom-Com Anime List (Best Recommendations)Документ23 страницыTop 10 Rom-Com Anime List (Best Recommendations)EricsonMitraОценок пока нет
- Top 10 Rom-Com Anime List (Best Recommendations)Документ23 страницыTop 10 Rom-Com Anime List (Best Recommendations)EricsonMitraОценок пока нет
- Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMDДокумент5 страницUses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMDEricsonMitraОценок пока нет
- Approval Sheet MitrДокумент2 страницыApproval Sheet MitrEricsonMitraОценок пока нет
- ACME Sales NumbersДокумент7 страницACME Sales NumbersCENTARBEOTCHОценок пока нет
- ACME Quote-Word 2003Документ4 страницыACME Quote-Word 2003Mutmainnah AGОценок пока нет
- NCP Fever: Read Books, Audiobooks, and More Scribd, IncДокумент10 страницNCP Fever: Read Books, Audiobooks, and More Scribd, IncEricsonMitraОценок пока нет
- Deficient Fluid Volume - Nursing Diagnosis & Care PlanДокумент9 страницDeficient Fluid Volume - Nursing Diagnosis & Care PlanEricsonMitraОценок пока нет
- 11 Core CompetenciesДокумент20 страниц11 Core CompetenciesEricsonMitraОценок пока нет
- 7 Gastroenteritis Nursing Care PlansДокумент9 страниц7 Gastroenteritis Nursing Care PlansEricsonMitraОценок пока нет
- Interpersonal RelationsДокумент51 страницаInterpersonal RelationsWaqas Aslam KhanОценок пока нет
- Code of Ethics For NursesДокумент11 страницCode of Ethics For NursesPaul Andrew TugahanОценок пока нет
- 30 Nursing Life Hacks You Probably Didn't Know About - Page 2 of 2 - NurseslabsДокумент5 страниц30 Nursing Life Hacks You Probably Didn't Know About - Page 2 of 2 - NurseslabsEricsonMitraОценок пока нет
- Phil HealthДокумент118 страницPhil HealthEllaineCuiОценок пока нет
- Skin PrepДокумент13 страницSkin PrepEricsonMitraОценок пока нет
- Oral Health ProgramДокумент4 страницыOral Health ProgramEricsonMitraОценок пока нет
- Aruba Alambag ncm417Документ12 страницAruba Alambag ncm417EricsonMitraОценок пока нет
- DisasterДокумент16 страницDisasterEricsonMitraОценок пока нет
- Disaster NursingДокумент16 страницDisaster NursingEricsonMitraОценок пока нет
- Mental and Behavioral Dysfunction in Movement Disorders - M. Bedard, Et Al., (Humana, 2003) WW PDFДокумент580 страницMental and Behavioral Dysfunction in Movement Disorders - M. Bedard, Et Al., (Humana, 2003) WW PDFTommi Jitaru100% (1)
- Clinical Features and Diagnosis of Dementia With Lewy Bodies - FarlowДокумент12 страницClinical Features and Diagnosis of Dementia With Lewy Bodies - FarlowRafael Aramburú Umbert100% (1)
- Difficult Topics of Mrcp-1Документ134 страницыDifficult Topics of Mrcp-1Khalil AhrariОценок пока нет
- Deep Brain StimДокумент6 страницDeep Brain StimGayathri BhatОценок пока нет
- Biology Investigatory Project Class 12thДокумент20 страницBiology Investigatory Project Class 12thsupercelldarshil100% (1)
- Dementia Conversion DisordersДокумент28 страницDementia Conversion DisordersAYO NELSON100% (1)
- Timed Up and Go TestДокумент6 страницTimed Up and Go TestcamilaОценок пока нет
- Parkinson's DiseaseДокумент11 страницParkinson's DiseaseZA IDОценок пока нет
- Presentation FinalДокумент26 страницPresentation FinalDr THOMAS KINGSLEY MDОценок пока нет
- Drugs For Parkinson's Disease: Pharmacist'S Letter / Prescriber'S LetterДокумент4 страницыDrugs For Parkinson's Disease: Pharmacist'S Letter / Prescriber'S Letteranon_84599888Оценок пока нет
- Parkinsonism A General Motor Disability PDFДокумент9 страницParkinsonism A General Motor Disability PDFRishabh SinghОценок пока нет
- Cardiovascular Autonomic Dysfunction in Parkinson's DiseaseДокумент7 страницCardiovascular Autonomic Dysfunction in Parkinson's DiseaseCocosul Cocosului CocosaruluiОценок пока нет
- Parkinson's DiseaseДокумент3 страницыParkinson's DiseaseRachelle Ann E. De FelixОценок пока нет
- Parkinsons DiseaseДокумент8 страницParkinsons Diseaseapi-509210933Оценок пока нет
- LEGACY TO HOMOEOPATHS... DR. PRAFULL VIJAYAKAR'S INSIGHTSДокумент814 страницLEGACY TO HOMOEOPATHS... DR. PRAFULL VIJAYAKAR'S INSIGHTSParag Sharma100% (2)
- Annotatedparkinsonbibliography SharonДокумент5 страницAnnotatedparkinsonbibliography Sharonapi-304810226Оценок пока нет
- 100 Item MEDICAL SURGICAL Nursing ExaminationДокумент15 страниц100 Item MEDICAL SURGICAL Nursing Examinationalexis_borjОценок пока нет
- KNGF Guideline For Physical Therapy in Patients With ParkinsДокумент89 страницKNGF Guideline For Physical Therapy in Patients With ParkinsSrđan ŠarenacОценок пока нет
- R24: IFH Studies ListДокумент5 страницR24: IFH Studies ListDinesh MendheОценок пока нет
- Memory MaximizerДокумент202 страницыMemory MaximizerGanga SinghОценок пока нет
- Prof BSP-Akinetic Rigid Synd - PDДокумент139 страницProf BSP-Akinetic Rigid Synd - PDSavitha BasriОценок пока нет
- Biology Investigatory Project: Topic: Parkinson'S DiseaseДокумент18 страницBiology Investigatory Project: Topic: Parkinson'S DiseaseAneesh MoosaОценок пока нет
- Shackshop - Hydrogen WaterДокумент13 страницShackshop - Hydrogen WaterHeinrich Nel100% (2)
- Vol 22.4 - Movement Disorders.2016Документ304 страницыVol 22.4 - Movement Disorders.2016paslaru danОценок пока нет
- 9 Multiple SeclrosisДокумент38 страниц9 Multiple SeclrosisAhmed aljumailiОценок пока нет
- Vivir Con ParkinsonДокумент22 страницыVivir Con ParkinsonAlexis Muñoz TrincadoОценок пока нет
- Chatterbox Edition 142 - June July 2023Документ44 страницыChatterbox Edition 142 - June July 2023Christine JonesОценок пока нет
- Early Detection of Parkinson's Disease Using Deep Learning and Machine LearningДокумент12 страницEarly Detection of Parkinson's Disease Using Deep Learning and Machine LearningPraveenОценок пока нет
- Chapter 13: Antiparkinsonian DrugsДокумент5 страницChapter 13: Antiparkinsonian DrugsKT100% (1)
- First AidДокумент52 страницыFirst Aidapi-351099966Оценок пока нет