Академический Документы
Профессиональный Документы
Культура Документы
A Comparison of African-Caribbean and White European Young Adults
Загружено:
Santiago SainАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A Comparison of African-Caribbean and White European Young Adults
Загружено:
Santiago SainАвторское право:
Доступные форматы
International Journal of Social
Psychiatry
http://isp.sagepub.com/
A Comparison of African-Caribbean and White European Young Adults'
Conceptions of Schizophrenia Symptoms and the Diagnostic Label
L. Stone and W.M.L. Finlay
Int J Soc Psychiatry 2008 54: 242
DOI: 10.1177/0020764008089616
The online version of this article can be found at:
http://isp.sagepub.com/content/54/3/242
Published by:
http://www.sagepublications.com
Additional services and information for International Journal of Social Psychiatry can be found at:
Email Alerts: http://isp.sagepub.com/cgi/alerts
Subscriptions: http://isp.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://isp.sagepub.com/content/54/3/242.refs.html
>> Version of Record - May 9, 2008
What is This?
Downloaded from isp.sagepub.com at UNC on September 26, 2014
A COMPARISON OF AFRICAN-CARIBBEAN AND WHITE EUROPEAN
YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA
SYMPTOMS AND THE DIAGNOSTIC LABEL
L. STONE & W.M.L. FINLAY
ABSTRACT
Background: Discrepancies in the experiences of different ethnic groups in mental
health services exist, such as in the persistently higher rates of schizophrenia
diagnosis found among the African-Caribbean population compared to the white
European population in the UK. Some hypotheses consider whether this is due to
greater stigmatizing attitudes to mental illness in the African-Caribbean community,
leading individuals to avoid treatment-seeking and an increased incidence
of schizophrenia. This study aimed to investigate recognition and evaluation
of schizophrenic symptoms across African-Caribbean and white European
individuals.
Method: One hundred and twenty eight adult students from London colleges com-
pleted a questionnaire assessing stigma beliefs, evaluation of symptoms as mental
illness and help-seeking beliefs, in response to symptom vignettes.
Results and Discussion: African-Caribbean participants indicated less stigmat-
izing beliefs towards both the symptoms and diagnostic label of schizophrenia
compared to the white European participants. White European participants were
more likely to label vignettes as implying mental illness and also more likely to
recommend professional health treatment. These results are inconsistent with a
hypothesis that on average African-Caribbean people stigmatize schizophrenia
more than white European people. While white European participants beliefs
were more likely to follow a western model of mental illness, African-Caribbean
participants were more likely to have alternative beliefs. The influence of racial
discrimination, mental illness knowledge and societal structures are discussed.
Key words: beliefs, schizophrenia, African-Caribbean, White-European, diagnostic
label, cross-cultural
INTRODUCTION
There have been calls for greater understanding of cultural issues within mental health services
over recent years (e.g. Halsey & Patel, 2003; Patel et al., 2000) as well as recommendations to
make services both culturally sensitive and accessible for ethnic minorities (Bhugra, 1997; Dana,
1998; Department of Health (DoH), 2005). Studies have often reported differences in rates of
International Journal of Social Psychiatry. Copyright 2008 SAGE Publications (Los Angeles, London, New Delhi
and Singapore) www.sagepublications.com Vol 54(3): 242261 DOI: 10.1177/0020764008089616
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 243
schizophrenia between minority and majority ethnic groups (Eaton & Harrison, 2000; King, Coker,
Leavey et al., 1994), and there is repeated evidence that there are higher rates of schizophrenia
diagnosis and symptoms among African-Caribbean people compared to people from other ethnic
groups (Bennett & Dennis, 2000; Bhugra, Leff, Mallett, Der, Corridan & Rudge, 1997; Dein,
1997; Fearon, Kirkbride, Morgan, Dazzan, Morgan et al., 2006; Harrison, Glazebrook, Brewin,
Cantwell, Dalkin et al., 1997; King, Nazroo, Weich, McKenzie, Bhui et al., 2005). In contrast, rates
of psychosis in the Caribbean are equivalent to those of the white population in Britain (Hickling
& Rodgers-Johnson, 1995). Further, there is evidence that compared to white people, black people
are more likely: (i) to be admitted into care on the basis of perceptions of threat to others; (ii) to
enter care through the police rather than via a psychiatrist; (iii) to be less satisfied with their primary
care service; (iv) and to have other differences in experience of services, such as being treated with
higher doses of medication and less likely to receive psychological therapies (Bhugra, Harding &
Lippett, 2004; Bhugra, Hilwig, Mallett, Corridan, Leff et al., 2000; Mind, 2002).
Explanations of different rates across groups
Several theories have been proposed to account for different rates of schizophrenia across groups,
ranging from genetic and biological accounts to those highlighting psychological and social aspects.
Theories incorporating psychosocial issues include explanations focusing on socio-economic
status (SES) (McKenzie, Van Os, Fahy, Jones, Harvey, Toone et al., 1995; Modood & Berthoud,
1997; Van Os, Fahy, Bebbington, Jones, Wilkins, Sham et al., 1994) and racism (Boydell, Van
Os, McKenzie, Allardyce, Goel, McCreadie & Murray, 2001; DoH, 2003; DoH, 2005; Hickling
& Hutchinson, 1999; Sashidharan, 2001). However, no one theory seems able to fully account for
differences in rates.
There appears to be consensus in the literature that a core schizophrenic syndrome exists
across several cultures (Jablensky, Sartorius, Ernberg, Anker, Korten et al., 1992). It is therefore
argued that psychosocial variables, including ones own and others understanding of and response
to symptoms, influence differences in course and outcome (Jarvis, 1998). The better outcome of
schizophrenia in certain developing countries may be due to these psychosocial factors, such as
more benign social responses (Lefley, 1990).
Angel and Thoits (1987) propose a theoretical framework for understanding the impact of culture
on symptom interpretation consisting of the following stages: (i) noticing changes; (ii) evaluating
and labelling changes; (iii) acting on changes. This framework acknowledges that cultures may
differ not only in what is perceived as illness, but also the appropriate response to that illness,
including treatment, social and personal responses (e.g. Fernando, 1988; Kirmayer, 1989). Thus,
when symptoms of schizophrenia are recognized, association with psychopathology or stigma may
not necessarily follow (Fabrega, 1991a; Littlewood, 2001). Littlewood states: There is evidence
that the popular understanding of mental illness, and thus the social response, may determine the
actual prognosis of severe mental illness, independently of any recourse to medical treatment
(2001, p. 1). The study described in this paper investigates differences between groups in their
understanding, attitudes (particularly stigmatizing responses) and treatment recommendations
when presented with the symptoms and diagnostic label of schizophrenia.
The role of stigma
Research has suggested that the effects of psychiatric stigma include depleted self-esteem, persistent
depression, unemployment, low income, and expectations and experience of social rejection
Downloaded from isp.sagepub.com at UNC on September 26, 2014
244 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
(Barker, Lavender & Morant, 2001; Knight, Wykes & Hayward, 2003; Link, 1987; Link,
Struening, Rahav, Phelan & Nuttbrock, 1997; although see Camp, Finlay & Lyons, 2002, for a
contrary argument regarding self-esteem). These effects may contribute to symptoms of anxiety,
depression and paranoia, as well as everyday conditions that hinder goals of recovery (such as
social reintegration Wahl, 1999). The stigma of receiving a psychiatric label may therefore act
as a stressor, worsening psychiatric symptoms or obstructing recovery.
Labelling may produce positive as well as negative effects. Angermeyer and Matschinger (1996)
compared beliefs about identical vignettes with or without the diagnostic label schizophrenia.
Participants responding to a label were more likely to suggest biological causes, were less likely to
link it to personal deficits and responsibility, and were more likely to assume a poorer prognosis.
The authors argued that while assigning less personal responsibility reduced blame and might there-
fore facilitate engagement with medical treatment, it might also lead to a more fatalistic attitude,
which could hinder coping efforts.
Stigma may prevent acceptance that symptoms exist or are part of mental illness (Kendell,
2001) and may act as a continual threat interfering with self-disclosure (Crisp, 2001). Furthermore,
having a high expectation of being stigmatized (stigma consciousness) can lead to negative and
critical interpersonal experiences (Pinel, 1999), which may have a strong effect on disclosure and
acceptance of help. The stigma associated with mental health institutions alone may contribute to
difficulties with engagement.
Stigma beliefs may be particularly significant in accounting for variability in the experience of
schizophrenia between African-Caribbean and white European people (Russell, 2002). Littlewood
(2001) reports that ethnic minority groups are commonly thought to be more likely to stigmatize
mental illness than white European groups, leading to later recourse to treatment and then higher
rates of sectioning. Jarvis (1998) suggests there may be a tendency for West Indian families to
severely stigmatize mental illness and then avoid contact with psychiatric services until crisis
point. However, there does not appear to be any clear data on this, and Littlewood (2001) states
that increased stigma beliefs have not actually been demonstrated.
Insight
Some research has considered how poorer insight may affect individuals engagement with
psychiatric services. In a study of inpatients case notes, significantly more black Caribbean indi-
viduals were judged to lack insight compared to white British individuals (Johnson & Orrell, 1996).
It was argued that differences between the psychiatrists and patients models of mental illness or
its treatment might contribute to problems with communication and treatment management within
mental health services. Perkins and Moodley (1993) asked African-Caribbean and white inpatients
to categorize their problems (most had a schizophrenia diagnosis) as psychiatric, physical/social,
or not problems at all. A significant difference was that none of the white patients denied having
problems, while responses of African-Caribbean patients were roughly equally spread across
categories. African-Caribbean patients were also more likely to have been subject to compulsory
admission. It is possible that African-Caribbean patients might have a broader range of ways to
explain their problems, explanations that were not sufficiently tapped in this study; for example,
finding oneself in hospital may more clearly indicate psychiatric or physical problems to white
patients than to African-Caribbean patients, whose experience of being forcibly placed in an
institution may have different connotations (more associated with racial oppression). Insight has
now come to be understood as a socio-cultural process, involving normative social and cultural
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 245
concepts (Saravanan, Jacob, Prince, Bhugra & David, 2004). Its assessment in comparison to local
and cultural standards is thought to be vital to reduce stigma and allow engagement with treatment
models (Saravanan, Bhugra, Prince & Jacob, 2005).
Conceptions of mental illness and treatment
Some studies conducted in the US have examined differences between black and white people in
conceptions of mental illness and treatment recommendations. Hall and Tucker (1985) reported
more misconceptions regarding mental illness among black people, but it is not entirely clear what
misconceptions refers to. Although race was not related to help-seeking attitudes, having fewer
misconceptions of mental illness was significantly related to positive help-seeking attitudes across
all individuals. Conversely, an investigation of black and white American undergraduates beliefs
regarding different mental illnesses, including schizophrenia, revealed no differences in beliefs about
the normality or severity of descriptions (Millet, Sullivan, Schwebel & Myers, 1996). However,
spiritual factors were more prevalent in black Americans beliefs about treatment and cause.
Alvidrez (1999) found that African Americans reported significantly higher stigma ratings con-
cerning mental health problems compared to a Latino group; were significantly less likely than
European-Americans to visit mental health services; and had significantly higher levels of belief
that certain health problems should not be discussed outside the family. Most recently, a survey
of 151 US students found that persons from minority ethnic groups were less likely to support
prejudicial attitudes (Corrigan, Edwards, Green, Diwan & Penn, 2001). However, ethnicity was
only divided into white and non-white, and there were only 33 non-white participants. The
authors acknowledged that future research is needed to validate these findings.
In the UK, Pote and Orrell (2002) asked 191 participants from five broad ethnic groups in Britain
to rate whether they thought schizophrenia symptom vignettes described a mental illness. African-
Caribbean individuals were less likely than others to regard unusual thought content as a sign of
mental illness. However, it is difficult to generalize from this study as there were only 10 people
in the African-Caribbean group, and the educational level of the participants was high (39% had
a university degree or higher). Education has been found to influence attitudes to mental illness
(Furnham & Murao, 1999).
Differences in beliefs about diagnosis and treatment are also pertinent. Leong and Zachar (1999)
found that socially restrictive views of mental illness (e.g. dangerousness) were associated with
negative attitudes towards help-seeking among white undergraduates (see also Furnham & Murao,
1999). Others have argued that while fear of social stigma may prevent seeking professional
treatment, beliefs about the effectiveness of alternatives, such as religious and cultural support,
may also lead to low treatment-seeking (Cinnirella & Loewenthal, 1999).
Schnittker, Freese and Powell (2000) directly examined beliefs in a large sample (n = 1444) and
found that compared to white Americans, African Americans tended to reject the idea that mental
illness is caused by either genetics or poor family upbringing, and held generally negative attitudes
towards mental health services. Schnittker et al. (2000) suggest that African Americans react against
such stigmatizing explanations due to their experience of similar arguments about genetics and
family being used in racial discrimination.
Differences between groups may exist, then, in the degree to which schizophrenia or its symptoms
are stigmatized, the extent to which symptoms are recognized as indicating mental illness, and
what sort of help is recommended for these symptoms. While epidemiological surveys across
ethnic groups have been conducted, the beliefs that African-Caribbean and white European people
Downloaded from isp.sagepub.com at UNC on September 26, 2014
246 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
in Britain hold about schizophrenia and its treatment have not been specifically or systematically
investigated. This research addresses the following questions.
Are there differences between African-Caribbean groups and white European groups in:
(i) stigmatizing attitudes towards a person with the diagnostic label of schizophrenia?
(ii) treatment recommendations for a person exhibiting individual symptoms of
schizophrenia?
(iii) the extent to which individual symptoms are believed to indicate the presence of mental
illness?
METHOD
Participants
This initial sample consisted of 179 people from various ethnic groups. Participants for this study
were recruited from three further education colleges and one adult education centre in London. No
students were recruited from universities. Their student populations were ethnically diverse, aged
16 and over, and mostly without higher (university level) education. Additional participants were
recruited from a college outside London to ensure that the sample was balanced across ethnicity,
age, gender and educational level. Participants were recruited from a variety of BTEC and A-level
classes, including IT, modern languages, physical and social science subjects.
This research was aimed at comparing white European and African-Caribbean people, therefore
participants from other ethnic groups were excluded from the final sample analyzed. Since previous
research has found that educational attainment affects attitudes to mental illness (Pote & Orrell,
2002), the range of educational levels in the final sample was limited to secondary education and
below. The purpose of this was to make the black and white groups as similar as possible, and to
reduce the number of individuals with formal education about mental illness in this way the survey
strived to assess lay beliefs. Those with missing data, for example regarding age or sex, were still
included. The final sample consisted of 128 individuals (see Table 1).
Information about the final sample of participants by ethnic group is provided in Table 2. Although
there were more women than men in all, gender proportions did not differ significantly by ethnic
group (2 (1, n = 121) = 0.288, p = 0.591). Similarly, there was no difference in the proportion
of people with differing educational backgrounds across ethnic groups (2 (1, n = 105) = 4.483,
p = 0.106). MannWhitney U-tests (non-parametric statistics) were used to compare age and years
in the UK as these variables were not normally distributed. Age ranged from 16 to 59 years, and did
not differ significantly by ethnic group (z (69,50) = 1508, p = 0.235). There was a significant differ-
ence between the two ethnic groups in how long individuals had lived in the UK (z (66,47) = 681,
p = 0.000), with the white European group having longer residence.
Procedure
A researcher visited classes and students were asked to complete the Social Perceptions Questionnaire
(SPQ) either before classes started or during study breaks. The researcher introduced the research,
invited students to take part, and then gave a questionnaire pack consisting of the questionnaire,
a debrief sheet, an information sheet and consent form to each member of the group. The ques-
tionnaire also asked for demographic details, in which participants were asked to define their
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 247
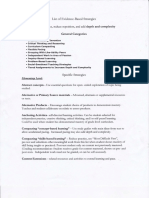
Table 1
Demographic information
Initial sample Final sample
Number of individuals (n) 179 128
Sex
Female 106 (59.2%) 76 (59.4%)
Male 66 (36.9%) 46 (35.9%)
Mean age (SD) 24.5 (10.4) 22.8 (9.87)
Ethnicity
Asian 6 (3.4%) 0
Black/African-Caribbean 81 (45.3%) 76 (59.4%)
Chinese 1 (0.6%) 0
Mixed 13 (7.3%) 0
White/European 76 (42.5%) 50 (39.1%)
Mean years lived in the UK (SD) 17.6 (13.1) 15.2 (12.0)
Highest educational qualification
Current course (need info about what level this was) 30 (16.8%) 28 (21.9%)
GCSE 52 (29.1%) 47 (36.7%)
A level 34 (19.0%) 30 (23.4%)
Degree 25 (14.0%) 0
Higher degree 8 (4.5%) 0
Table 2
Demographic information in the final sample
African-Caribbean White-European
Sex
Male 25 (35.2%) 20 (40.0%)
Female 46 (64.8%) 30 (60.0%)
Mean age (SD) 21.5 (7.3) 24.7 (12.5)
Highest educational level
Current 20 (28.2%) 8 (16%)
GCSE 22 (31.0%) 25 (50%)
A level 18 (25.4%) 12 (24%)
Mean years lived in the UK 10.2 (8.5) 22.0 (13.0)
ethnicity in terms of the categories used in the 2001 census (CRE, 2001). Students who declined
participation could return the questionnaire pack uncompleted. The researcher remained on site
in order to answer questions and collect back questionnaires. In most cases, questionnaires were
completed in the presence of the researcher. Three were returned later and six individuals decided
not to participate and returned their packs uncompleted.
Instruments
Although public opinion surveys regarding attitudes to mental health exist, there does not appear
to be agreement over an instrument to measure stigma (Byrne, 2001). Previous studies examining
stigmatizing attitudes have mostly used questionnaires consisting of statements about mental illness
Downloaded from isp.sagepub.com at UNC on September 26, 2014
248 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
which respondents must rate on Likert scales (e.g. Opinions about Mental Illness Questionnaire
(Cohen & Struening, 1962) as used in Corrigan et al., 2001; Beliefs About Mental Illness scale (Hirai
& Clum, 2000); Community Attitudes towards Mental Illness (Taylor & Dear, 1981)). Alternatively,
studies have employed interviews using vignettes describing particular mental illnesses and have
asked respondents about cause, understanding and treatment (e.g. Angermeyer et al., 2003; Link,
Phelan, Bresnahan, Stueve & Pescosolido, 1999; Millet et al., 1996; Schnittker, Freese & Powell,
2000). While all these questionnaires have acceptable reliability and validity, they do not tackle
stigmatizing attitudes about symptoms of schizophrenia specifically. Therefore, for this study, the
SPQ was developed. It included unlabelled symptom vignettes and a separate vignette containing
the diagnostic label of schizophrenia. By presenting symptom vignettes rather than a case, the
aim was to identify bottom-up what signs are recognized as schizophrenia, what the attitudinal
response to these is, and what action is recommended. In terms of Angel and Thoits model (1987),
this corresponds to first, second and third order categorization of affective change that is attending
to/ignoring (or recognizing), evaluating, and acting on symptoms, respectively.
The SPQ is based on questionnaires previously used to survey beliefs about mental illness. It
consists of seven vignettes: four describe symptoms of schizophrenia, two describe unusual non-
symptom behaviours not classified as psychiatrically pathological, and one describes a diagnosis of
schizophrenia (see Table 3). The symptom and non-symptom vignettes were taken from the pool of
vignettes used by Pote and Orrell (2002) in their study on perceptions of schizophrenia (in which
eight schizophrenia symptom, eight depression symptom and six non-symptom vignettes were
used in total). These symptom vignettes had been developed from well-documented psychiatric
scales (McEvoy, Schooler, Friedman, Steingard & Allen, 1993).
Four symptom vignettes were chosen primarily to focus the investigation on the core signs
indicating schizophrenia. Positive symptoms characteristically associated with schizophrenia include
hallucination, suspicion and unusual thought content, while characteristic negative symptoms
include social withdrawal and blunted affect (Harvey, Davidson, White, Keefe et al., 1996). Similar
impairments associated with auditory uncertainty, deviant perception, ideas of reference, and
disordered thought may also be characteristic within the subjective experience of schizophrenia
(Mass, 2000). Secondly these vignettes appeared to discriminate most between ethnic groups in
Pote and Orrells (2002) study.
Non-symptom vignettes (extraversion, affectionate) were included as a comparison, as well as
to monitor social desirability effects. A schizophrenia-label vignette was devised, presenting a
characteristic experience of receiving a diagnosis of schizophrenia. All vignettes were designed to
be similar in style and length.
Four versions of the questionnaire were used to monitor possible effects of order. Since analysis
revealed no effect of order, this factor was omitted from the analysis below. However, the diagnosis
vignette was always last to prevent biasing participants responses. For each vignette, participants
were asked to assume that the experiences had occurred for at least two weeks (in line with
diagnostic criteria), and then rate their agreement with six statements describing stereotypical and
stigmatizing attitudinal responses towards mental illness. These measured negative social status/
social distance (two items), dangerousness (one item), trustworthiness (one item), abnormality (one
item) and curability (one item) see Table 4. These items were developed on the basis of factors
repeatedly shown to be significant components and indicators of stigmatizing beliefs in the literature
(e.g. Furnham & Murao, 1999; Hirai & Clum, 2000; Link et al., 1997; Taylor & Dear, 1981).
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 249
Table 3
Vignettes used in SPQ
Symptom vignettes
1. Anhedonia/Asociality
He does not find much interesting. Things that had previously been attractive or stimulating to him just do not
seem to matter any more. He does not go out with others much. It just does not seem worth the effort or trouble.
Not much is fun. Not much is exciting. It is simpler just to stay at home and take things easy by himself.
2. Suspiciousness
It became very clear to him that something was definitely going on. They had singled him out and they meant to
cause him trouble. Some very powerful people intended to harm him, and these people left clues everywhere in
order to threaten and worry him. He had to be very cautious because these people seemed to know an incredible
amount about him. Perhaps they were secretly monitoring him.
3. Unusual thought content
He had some very surprising experiences. People seemed able to know his thoughts. He would just think about
a topic and, next thing, they would broadcast that very topic over the radio or the TV. People on the street would
signal that they knew what he was thinking. Sometimes signals appeared in things he was reading that showed how
much they knew about him. Sometimes these people would put their thoughts into his mind. That felt strange.
4. Hallucinatory behaviour
He began to notice people talking about him. At first he was not sure who it was talking or why they talked about
him. People talked about him in many different places and he gradually became used to it. Sometimes at night
they would be outside the window of the next flat. Sometimes it was almost like telepathy. Sometimes they said
very nasty things.
Filler vignettes
5. Extraversion
He is always the first person to speak in a group. Sometimes he can talk for 10 minutes without giving others a
chance to say their point of view. When people do interrupt he will often say a critical comment which silences
them. He does things spontaneously, in reaction to what is going on around him, and may not think them through
beforehand.
6. Affectionate
He is very affectionate, and likes most people he meets. On meeting a friend or someone he has only met on a
couple of occasions he will hug them and kiss them on the cheek. He will talk to others in a very loving manner, and
always shows his feelings. He is often expressive with his hands when talking and will touch others frequently.
Label vignette
7. Schizophrenia diagnosis
He had not been well for some time. He went to the hospital with a relative to see a doctor. The doctor who saw
him was a psychiatrist. The doctor told him he had schizophrenia. He would be in hospital for a while and start
taking medication to help him. A nurse came to talk to him. When he got back home, the nurse continued to visit
him to make sure he was okay.
In order to overcome social desirability tendencies, participants were not asked about their own
stigmatizing attitudes, but about their perceptions of community stigma.
A further statement, that The description implies this person has a mental illness was also
included (providing a replication of Pote and Orrells investigation of perceptions of schizophrenia).
For all seven of these items, participants were asked to rate their agreement on a five-point Likert
scale from strongly disagree to strongly agree.
Two open-ended questions were also asked to obtain participants views about need for help: (1)
Does this indicate any need for help or treatment?; (2) If so, what kind of help or treatment?
Downloaded from isp.sagepub.com at UNC on September 26, 2014
250 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
Table 4
SPQ stigma statements
Negative social status
Most people would not willingly accept this person as a close friend.
Most people would be reluctant to have this person as a boyfriend.
Dangerousness
Most people would be afraid this person may harm others.
Trustworthiness
Most people would believe this person to be trustworthy.
Abnormality
Most people would think that virtually anybody could be like this.
Curability
Most people would believe this person was going through a temporary state which they would emerge from.
RESULTS
Reliability
Total stigma scores were computed by summing all six stigma items per vignette (with items
reverse-scored as appropriate), and so had a possible range of 636. Higher scores indicated greater
(i.e. more negative) stigma beliefs. Reliability analysis (Cronbachs ) was undertaken for all items
relating to stigma and revealed satisfactory internal consistency ( = 0.71).
Responses to the questions about treatment were content analyzed. The categories that emerged
were professional health (e.g. talk to a counsellor, see a doctor); professional non-health (e.g. call
the police); other support (e.g. talk to family or friends); unclear (e.g. get help); and none (i.e. no
help is needed). A second researcher inspected a sample of questionnaires. Inter-rater reliability
assessed by Cohens Kappa (Robson, 1993) was good (K = 0.78).
Content validity
Both the vignettes and response items for the questionnaire were developed from previous studies.
Just as previous studies employed vignettes and items about cause and treatment for different mental
illnesses (e.g. Angermeyer, Beck & Matschinger, 2003; Schnittker, Freese & Powell, 2000), this
study used items from questionnaires probing stigmatizing attitudes to the vignettes. The vignettes
had been found to be reliable and valid in previous studies (Pote & Orrell, 2000; McEvoy et al.,
1993), and the four used here were chosen to correspond to the content of core schizophrenia
symptoms as discussed in the literature. The stigma items corresponded to negative social status,
dangerousness, abnormality and curability, which have frequently emerged in the literature as
organizing factors in peoples conceptions of mental illness. The questionnaire was piloted on a
small group of students; following this, some wording was changed to clarify items and certain
vignettes were made more similar in terms of length and style.
Content validity can further be demonstrated by a factor analysis, which revealed that items loaded
onto two factors relating to the themes of social rejection (negative social status, dangerousness
and trustworthiness items) and setting apart from others (abnormality and curability items), which
are emphasized throughout the literature (Link et al., 1997). Analysis of data according to the social
rejection factor was carried out, and revealed almost identical results to that when a total stigma
score was used. Given this, the analysis based on total stigma scores is presented in this paper.
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 251
In order to provide some indication of the validity of the vignettes, a repeated-measures
analysis of variance (ANOVA) was used to compare mental illness labelling scores for the
diagnosis, symptom and filler vignettes: a significant difference between scores was found for
the total sample (F(2,109) = 94.703, p = 0.000, 2 = 0.635). The diagnosis vignette was rated as
more indicative of mental illness, followed by the symptom vignettes, with the filler vignettes
rated as least indicative.
Stigma
A multivariate analysis of variance (MANOVA) was carried out to examine differences in stigma
beliefs between the two groups. Table 5 shows the total stigma scores for the different vignettes
by ethnic group. Sex was included as an independent variable as previous studies have indicated
sex differences in attitudes to mental illness (e.g. Leong & Zachar, 1999; Corrigan et al., 2001).
Analysis revealed a significant difference in total stigma scores between black and white participants
(F(7,88) = 2.663, p = 0.015, 2 = 0.175). There was no significant effect of sex (F(7,88) = 0.591, p = 0.761,
2 = 0.045), or any significant interaction effect (F(7,88) = 0.947, p = 0.475, 2 = 0.070).
A series of ANOVA tests (see Table 5) revealed that white European participants had significantly
higher total stigma scores (indicating more negative attitudes) than African-Caribbean participants
on hallucination, suspiciousness, thought content and diagnosis vignettes. Conversely, African-
Caribbean participants had significantly higher total stigma scores than white European participants
on the affectionate filler vignette. There were no other significant differences.
Analysis of the data as a whole using a repeated-measures ANOVA was conducted to compare
total stigma scores for the different symptom, filler, and diagnosis vignettes. This revealed a
significant difference between vignettes (F(6,97) = 15.271, p = 0.000, 2 = 0.486). Paired t-tests then
allowed comparisons of all vignettes with the diagnosis vignette. Total stigma scores were lower for
each symptom and filler vignettes compared to the diagnosis vignette, with significant differences
for anhedonia (t (110) = 4.661, p = 0.000), thought content (t (113) = 2.050, p = 0.043) and
affectionate (t (114) = 7.967, p = 0.000) vignettes.
Treatment beliefs
Participants decisions about whether a vignette required treatment were examined across
groups using a series of 2 analyses. There were significant differences in the proportion of
Table 5
Mean total stigma scores
Mean scores (SD) African- White-European F p
Caribbean (two-tailed)
Total stigma
Hallucination 18.44 (3.30) 20.07 (4.08) 4.050 0.047*
Suspiciousness 17.67 (3.19) 20.30 (3.81) 12.295 0.001**
Anhedonia 17.27 (3.31) 17.83 (2.50) 0.564 0.455
Thought content 18.06 (3.03) 19.87 (3.86) 7.642 0.007**
Diagnosis 18.65 (3.65) 20.52 (3.63) 6.557 0.012*
Extraversion 19.25 (3.03) 18.98 (2.62) 0.142 0.707
Affectionate 16.04 (3.21) 14.76 (2.57) 3.427 0.067
* p < 0.05 ** p < 0.01
Downloaded from isp.sagepub.com at UNC on September 26, 2014
252 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
African-Caribbean and white European participants responding yes or no to some form of help
or treatment for several vignettes see Table 6. For hallucination and thought content descriptions,
a significantly greater proportion of the white European group recommended some help-seeking.
The reverse appeared to occur for the extraversion and affectionate vignettes.
Since we were predominantly concerned with proportions of participants suggesting treatment
from a health professional, the categories of non-health professional, other support and unclear
were merged into an other help category. Table 7 shows the proportion of responses for each
vignette (except diagnosis, as treatment was already part of the vignette itself) within each ethnic
group. Initial 2 analyses showed that there were significant differences between proportions of
participants responses across ethnic groups for hallucination, suspiciousness, thought content,
and affectionate vignettes.
Further follow-up 2 analyses allowed specific comparisons of response categories for these four
vignettes. A significantly greater proportion of white European participants than African-Caribbean
participants recommended professional health treatment compared to no treatment for hallucination
(2 (1, n = 87) = 10.000, p = 0.002), suspiciousness (2 (1, n = 71) = 7.870, p = 0.05) and thought
content (2 (1, n = 92) = 6.840, p = 0.009) vignettes. For the suspiciousness vignette, a further
significant difference was found in the higher proportion of African-Caribbean recommendations
for other types of help compared to professional health help (2 (1, n = 69) = 6.462, p = 0.011). On
inspection of individual questionnaires, this seemed to reflect the tendency for African-Caribbean
individuals to advise consultation with the police about the experiences (professional non-health).
There was no significant difference across groups for the anhedonia vignette. Interestingly, in the
affectionate filler vignette more African-Caribbean individuals appeared to indicate some form of
Table 6
Treatment beliefs
African- White- 2 DF p
Caribbean European (two-tailed)
Hallucination
Yes 39 37 7.88 1 0.005**
No 34 10
Suspiciousness
Yes 38 31 2.18 1 0.140
No 31 14
Anhedonia
Yes 36 29 0.868 1 0.352
No 32 18
Thought content
Yes 22 26 5.03 1 0.025*
No 41 20
Extraversion
Yes 24 8 4.16 1 0.041*
No 45 38
Affectionate
Yes 9 0 6.41 1 0.011*
No 54 41
* p < 0.05 ** p < 0.01
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 253
Table 7
Types of help suggested
African-Caribbean White-European 2 DF p
(two-tailed)
Hallucination
Professional health 19 24 9.99 2 0.007**
Other help 20 13
None 34 10
Suspiciousness
Professional health 9 17 9.48 2 0.009**
Other help 29 14
None 31 14
Anhedonia
Professional health 18 19 2.81 2 0.246
Other help 18 9
None 32 18
Thought content
Professional health 12 19 7.01 2 0.030*
Other help 10 20
None 41 45
Extraversion
Professional health 8 2 4.90 2 0.086
Other help 17 6
None 44 38
Affectionate
Professional health 4 0 6.41 2 0.041*
Other help 5 0
None 54 41
help than white European individuals. A comparison of numbers recommending other help and
no help approached significance (2 (1, n = 100) = 3.66, p = 0.056). However, this is difficult to
evaluate as there were no white European responses in the health or other help categories, which
meant that numbers were insufficient for reliable analyses.
Labelling symptoms as mental illness
Table 8 shows the mean labelling scores for each vignette across the two groups. A MANOVA
examined differences in whether symptoms were perceived as mental illness and indicated that
ethnicity was significant in contributing to variance in labelling scores (F(7,96) = 5.254, p = 0.000,
2 = 0.277), while neither sex alone (F(7,96) = 1.064, p = 0.393, 2 = 0.072) nor an ethnicitysex
interaction (F(7,96) = 0.561, p = 0.786, 2 = 0.039) were significant. Further analysis revealed that
participants in the white European group had significantly higher labelling scores (indicating
labelling as mental illness) for the hallucination, suspiciousness, thought content, and diagnosis
vignettes.
Further analyses
Some exploratory analyses were also undertaken. These showed significant positive correlations
between labelling and total stigma scores for six of the seven vignettes (r = 0.2610.479, p < 0.01),
Downloaded from isp.sagepub.com at UNC on September 26, 2014
254 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
Table 8
Mean labelling scores indicating labelling of mental illness in vignettes
Mean scores (SD) African-Caribbean White-European F p
(two-tailed)
Hallucination 2.74 (1.28) 3.54 (1.20) 11.595 0.001**
Suspiciousness 2.33 (1.18) 3.19 (1.25) 12.260 0.001**
Anhedonia 2.38 (1.11) 2.66 (1.04) 0.853 0.358
Thought content 2.56 (1.19) 3.33 (1.06) 9.743 0.002**
Diagnosis 3.39 (1.37) 4.25 (0.84) 14.088 0.000**
Extraversion 2.28 (1.08) 2.04 (0.80) 1.435 0.234
Affectionate 1.97 (1.06) 1.88 (0.82) 0.191 0.663
* p < 0.05 ** p < 0.01
the exception being the extraversion vignette (r = 0.095, ns). MANOVAs were also conducted to
compare the labelling and stigma scores of individuals who recommended treatment and those
who did not for each symptom vignette (hallucination (F(2,110) = 27.333, p = 0.000, 2 = 0.332),
suspiciousness (F(2,109) = 9.225, p = 0.000, 2 = 0.145), anhedonia (F(2,107) = 6.504, p = 0.002,
2 = 0.108), thought content (F(2,105) = 45.320, p = 0.000, 2 = 0.463), extraversion (F(2,105) = 7.359,
p = 0.001, 2 = 0.123), and affectionate (F(2,97) = 17.969, p = 0.000, 2 = 0.270) vignettes). This
revealed a significant difference between these groups on all vignettes. Specific investigation of
these differences using a series of ANOVAs showed that those who did recommend treatment
had significantly higher labelling scores and significantly higher stigma scores than those who
did not recommend treatment across all vignettes (the only exception being the total stigma score
differences for the anhedonia vignette).
DISCUSSION
Before discussing the results, we wish to make it clear that our intention is not to reify the notion
of race, nor to suggest that the groups we have compared are homogeneous. They are not, and we
need to be aware of the tendency when presenting such comparisons to suggest that small differ-
ences in means between groups represent some essential difference. We recognize that black and
white people merge, there are not distinct social categories and the differences we find are only
small differences in tendency compared to the large degree of overlap in response between the two
groups. There is more similarity in every comparison we have made than there is difference.
Our data indicated that, on average, African-Caribbean individuals viewed the schizophrenia
diagnosis and three of the four symptoms as less socially stigmatizing than white European indi-
viduals. The findings are in line with previous research that found lower prejudicial attitudes to
mental illness among ethnic minority groups (Corrigan et al., 2001). The results are inconsistent
with the hypothesis discussed by some authors (Jarvis, 1998; Littlewood, 2001) that African-
Caribbean people stigmatize people with schizophrenia more than white European people. It is
also inconsistent with the American research that has indicated either no difference between black
and white participants in beliefs about the normality of schizophrenia (Millet et al., 1996), or
greater stigma (Alvidrez, 1999) and more stereotypical views among black Americans (Hall &
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 255
Tucker, 1985). This may reflect different patterns of beliefs among black and white people in the
US compared to the UK, or the fact that these studies used different methodologies and investigated
more general beliefs about mental illness, including causal attributions and the effectiveness of
different treatments.
White European participants were, on average, more likely than African-Caribbean participants
to suggest seeking help for symptoms, and more likely to recommend this from a health profes-
sional. This supports previous findings that African-Caribbean individuals are less likely to visit
mental health services than other groups (Alvidrez, 1999), and may consider other factors important
in treatment (Millet et al., 1996).
African-Caribbeans were significantly less likely than white Europeans to label the symptom
vignettes as mental illness. This is consistent with some previous research (e.g. Pote & Orrell,
2002) and suggests a slightly different profile to African-Caribbean peoples understandings of
schizophrenia symptoms compared to white European people. Interestingly, African-Caribbean
people were also significantly less likely than the white European people to agree that the diagnosis
itself implied mental illness.
We may speculate how the results relate to Angel and Thoits (1987) model of symptom inter-
pretation, which delineates stages of recognition, labelling and evaluation, and finally action.
White European participants appear, on average, to recognize descriptions of symptoms somewhat
differently to African-Caribbean participants (i.e. more often in terms of mental illness). Given
the prevailing notion of psychiatric stigma in western society (Porter, 2001), this may have led
to evaluations associated with social stigma, associated beliefs coherent with a western medical
or psychological model of mental illness, and finally action in terms of help-seeking from the
health sector.
African-Caribbean people appeared to perceive descriptions of symptoms as different to
fillers. However, our findings indicate that some individuals of African-Caribbean origin have an
understanding of mental illness encompassing an alternative way of labelling, evaluating and con-
sidering action (or treatment), which appears to contrast with a western psychiatric understanding.
One particular symptom vignette, suspiciousness, may provide an illustration of this. In this
example, African-Caribbean individuals on average showed less stigmatizing attitudes and less
agreement that this implied mental illness. They were more likely to recommend help from non-
health professionals, often the police. This echoes Jarviss (1998) observations that within African-
Caribbean communities, family and friends of a person with schizophrenia often turn to the police
when a crisis develops. One could tentatively propose that personal experiences of discrimination
may predispose African-Caribbean people to view suspiciousness as a quite realistic reaction,
particularly in response to racism. In this case, a different set of processes means recommending
help from the police would be reasonable.
Some potential explanations can cautiously be offered (although this research did not address
these explicitly). Schnittker et al. (2000) note that even when explanations of social problems do not
explicitly cite race, they may be widely understood as having potentially powerful racial implications,
and African-Caribbean individuals may be particularly aware of such implications. African-
Caribbean and white European people may therefore not perceive schizophrenia so differently,
but African-Caribbean people may be more cautious about invoking negative social meanings be-
cause similar attitudes have been used to stigmatize them on the basis of their ethnicity in the past.
Another contributory factor could be a greater emphasis on the individual and independence in
western/white European society (see Fabrega, 1991b), resulting in a tendency towards individual
Downloaded from isp.sagepub.com at UNC on September 26, 2014
256 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
blame and social marginalization. In African developing countries, societal responses are perceived
as less excluding and placing emphasis on networks of people rather than on individuals (Lefley,
1990). These more socially inclusive responses may be present in varying degrees in African-
Caribbean communities in the UK, and be seen in the current African-Caribbean sample.
It is particularly striking that African-Caribbean participants were significantly less likely to rate
the diagnosis of schizophrenia as mental illness. Thus, despite reading that a psychiatrist had
diagnosed schizophrenia, African-Caribbean individuals nevertheless did not agree that this implied
mental illness. Two explanations appear possible. First, this may indicate underlying distrust of
psychiatric opinion, which may be based on negative experiences with health professionals or any
institutions predominantly seen as white. This is consistent with the theory that the first point of
reference for initial decisions about symptoms is the immediate local community (Angel & Thoits,
1987). This possibility is supported by a recent report that acknowledged institutional racism within
the UK National Health Service (Carvel, 2004).
Alternatively, it may suggest that the African-Caribbean group was less familiar with the term
schizophrenia than the white European group. However, it is important not to assume that know-
ledge automatically weakens stigma beliefs. For example, among Japanese communities, rather than
being related to social inclusion (possibly indicated in this study), lack of knowledge about mental
illness appears to be associated with taboo and social criticism (Furnham & Murao, 1999).
In line with modified labelling theory, overall responses to symptoms, such as anhedonia and
unusual thought content, were significantly less stigmatizing than to the diagnosis vignette. How-
ever, no differences between perceptions of the diagnosis and either hallucination or suspiciousness
were found. It seems that hallucination and suspiciousness symptoms may have had particularly
powerful stigma connotations, to some degree separately of the label of schizophrenia. Thus while
psychiatric labelling is stigmatizing, other aspects of the experience of mental illness, such as the
meaning of particular symptoms, appear to also contribute to stigma.
In considering the raised incidence of schizophrenia diagnoses in African-Caribbean people in
the UK, this study found no evidence that it is related to increased stigmatization of mental illness
or its symptoms. The opposite was true. White participants thought that there was more stigma than
black participants. It may be that if symptoms of schizophrenia are not seen as either stigmatizing
or as an illness condition requiring action, people do not present to services until exacerbation of
symptoms occurs. At this point, more extreme measures may be invoked to manage the symptoms,
followed by all the consequences that are found in the data on African-Caribbeans harsh experiences
in mental health services (e.g. involvement of the police). Previous discussions regarding extended
social networks, which may tolerate and contain symptoms until such time when behavioural
disturbance reaches crisis point (Jarvis, 1998), reinforce this possibility. This does not, of course,
negate the importance of other factors such as racism, which are likely to be relevant to groups
different experiences of mental health services. It is particularly important to consider such issues,
given research that shows there is a marked excess of victimization experiences in those suffering
with psychosis (Bebbington et al., 2004).
White European individuals were more likely to recognize core symptoms of schizophrenia in
accordance with the framework that mental health professionals would adopt. One would imagine
that recognizing symptoms in this way would very much facilitate passage through mental health
systems for the individuals themselves, or if they were supporting a family member in accessing
treatment. It may be easier for them to engage in a medical framework and use psychiatric termin-
ology. On being assessed for psychological therapies, it may also be easier for a psychologist to
identify white European clients mental health-related cognitions.
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 257
There are some methodological issues that might affect the interpretation of the results.
It was hoped that asking for views about the majority populations stigmatizing attitudes would tap
wider group beliefs and enable more honest responses. However, it is not clear whether participants
answered with attitudes of their own community, or the majority (white European) community.
Further, this study does not provide specific data concerning self-stigma, that is stigmatizing atti-
tudes one holds about ones own experiences. Treatment-seeking beliefs may operate differently in
relationship to both self-stigma and the stigmatizing attitudes of wider, different communities. In
addition, this study provided only a limited sample of symptoms of schizophrenia and additional
vignettes may be required for a fuller representation of the schizophrenic condition.
Our sample consisted of student subjects, who are a select group and thus may not be representative
of the wider population, thus creating potential problems in generalizing the findings. Although
several participant factors were considered, it was not possible to incorporate the influence of
others, such as knowledge or experience of mental illness, or years lived in the UK. There was a
significant difference between the groups in how long they had lived in the UK. This might indicate
that differences between ethnic groups were more to do with there having been more people in the
African-Caribbean group who had grown up in a different country, and more in the white group
who had grown up in the UK. Our categories also meant that people from quite different cultural
backgrounds were grouped together. For example, white European could include people of both
Western and Eastern European origin, and African-Caribbean could include people of both African
and Caribbean origin. Thus considering other factors, such as religion and country of origin, may
enhance our knowledge of which variables are key.
Clearly reducing the stigma associated with schizophrenia is desirable to improve the lives of
those with the condition. But paradoxically, stigmatizing attitudes may also exert pressure on indi-
viduals to maintain engagement with services (e.g. through the actions of significant others).
Individuals with good mental health literacy seem to hold higher stigma beliefs and they appear
more likely to recommend medical treatment for schizophrenia (Lauber et al., 2005), which
could mean that they would also be more willing to take up treatment. Certainly, exploratory
analyses of this research did suggest that those recommending treatment gave significantly greater
social stigma responses. This suggests that providing education about mental illness, which may
facilitate the process of engaging someone in the early stages of schizophrenic breakdown with
services, might also raise social stigma (Angermeyer et al., 2003). This is consistent with evidence
that biological attributional beliefs about schizophrenia are associated with increased stigma
(Dietrich et al., 2004).
Engaging with those who may benefit from mental health services, such as family and friends of
a person experiencing schizophrenia as well as the person themselves, also means engaging with
their different beliefs. Some projects have been developed that reach out to communities within
their own framework of understanding and engage them on this level (e.g. Cares of Life project,
Nketia & Peters, 2004). Given that health services are not always seen as appropriate help for
symptoms of schizophrenia by different ethnic groups, joining with other services e.g. churches,
leisure and voluntary projects may provide opportunities for people to view health services as an
equally valid and useful means of help.
In terms of adapting services, recognition of the fact that African-Caribbean individuals may, on
average, be more likely to have non-medical understandings of symptoms and psychiatric terms,
may help clinicians consider how to be more flexible in the therapeutic and service models used,
and how to lead clients through services that are informed by medical philosophies. If it is difficult
Downloaded from isp.sagepub.com at UNC on September 26, 2014
258 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
for people to trust medical opinion, consultation from allied health professionals about how to offer
alternative frameworks of opinion may be useful. The challenge of negotiating trust with people
who may have had a very real history of discrimination, which is then complicated by symptoms
of schizophrenia, must be realized. As this research suggests, a joint understanding when using
psychiatric terms such as schizophrenia and mental illness is needed. Without this it is possible
that clients from African-Caribbean backgrounds may see what is offered as inappropriate or
punitive, leading to loss of engagement or negative attitudes to services.
ACKNOWLEDGEMENTS
Our thanks go to the students and tutors of South Bank University, and Morley, Lewisham, Southwark
and Farnham Colleges, for their participation in and support of this piece of research.
REFERENCES
Alvidrez, J. (1999) Ethnic variations in mental health attitudes and service use among low-income African American,
Latina, and European American young women. Community Mental Health Journal, 35(6), 515530.
Angel, R. & Thoits, P. (1987) The impact of culture on the cognitive structure of illness. Culture, Medicine &
Psychiatry, 11, 465494.
Angermeyer, M.C., Beck, M. & Matschinger, H. (2003) Determinants of the publics preference for social distance
from people with schizophrenia. Canadian Journal of Psychiatry, 48(10), 663668.
Angermeyer, M.C. & Matschinger, H. (1996) The effect of diagnostic labelling on the lay theory regarding schizo-
phrenic disorders. Social Psychiatry and Psychiatric Epidemiology, 31, 316320.
Barker, S., Lavender, T. & Morant, N. (2001) Client and family narratives on schizophrenia. Journal of Mental
Health, 10(2), 199212.
Bebbington, P.E., Bhugra, D., Brugha, T., Singleton, N., Farrell, M., Jenkins, R., Lewis, G. & Meltzer, H. (2004)
Psychosis, victimization and childhood disadvantage. British Journal of Psychiatry, 185, 220226.
Bennett, E. & Dennis, M. (2000) Adult mental health module. In Clinical Psychology, Race & Culture: A manual for
trainers (eds N. Patel, E. Bennett, M. Dennis, N. Dosanjh, A. Mahtani, A. Miller & Z. Nadirshaw). Leicester:
BPS Books.
Bhugra, D. (1997) Setting up services: cross-cultural issues. International Journal of Social Psychiatry, 3, 1628.
Bhugra, D., Leff, J., Mallett, R., Der, G., Corridan, B. & Rudge, S. (1997) Incidence and outcome of schizophrenia
in Whites, African-Caribbeans and Asians in London. Psychological Medicine, 27, 791798.
Bhugra, D., Harding, C. & Lippett, R. (2004) Pathways into care and satisfaction with primary care for black patients
in South London. Journal of Mental Health, 13(2), 171183
Boydell, J., Van Os, J., McKenzie, K., Allardyce, J., Goel, R., McCreadie, R.G. & Murray, R.M. (2001) Incidence
of schizophrenia in ethnic minorities in London: ecological study into interactions with environment. British
Medical Journal, 323, 14.
Byrne, P. (2001) Psychiatric stigma. British Journal of Psychiatry, 178, 281284.
Camp, D.L., Finlay, W.M.L. & Lyons, E. (2002) Is low self-esteem an inevitable consequence of stigma? An example
from women with chronic mental health problems. Social Science & Medicine, 55(5), 823834.
Carvel, J. (2004). Abscess of NHS racism exposed. The Guardian, 6 February, pp. 1, 4.
Cinnirella, M. & Loewenthal, K.M. (1999) Religious and ethnic group influences on beliefs about mental illness:
a qualitative interview study. British Journal of Medical Psychology, 72, 505524.
Corrigan, P.W., Edwards, A.B., Green, A., Diwan, S.L. & Penn, D.L. (2001) Prejudice, social distance, and familiarity
with mental illness. Schizophrenia Bulletin, 27, 219225.
CRE: Commission for Racial Equality (2003) Ethnic monitoring categories for England and Wales. At: www.cre.
gov.uk/gdpract/em_cat_ew.html.
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 259
Crisp, A.H. (ed) (2001) Every family in the land understanding prejudice and discrimination against people with
mental illness. London: Royal Society of Medicine Press Ltd.
Dana, R.H. (1998) Understanding cultural identity in intervention and assessment. London: SAGE.
Dein, S. (1997) Mental health in a multi-ethnic society. British Medical Journal, 315, 473476.
Department of Health (2003) Inside Outside Improving mental health services for black and minority ethnic com-
munities in England. London: National Institute for Mental Health in England.
Department of Health (2005) Delivering race equality in mental health care: An action plan for reform inside and
outside services and the Governments response to the Independent inquiry into the death of David Bennett.
London: National Institute for Mental Health in England.
Dietrich, S., Beck, M., Bujantugs, B., Kenzine, D., Matschinger, H. & Angermeyer, M.C. (2004) The relationship
between public causal beliefs and social distance toward mentally ill people. Australian & New Zealand Journal
of Psychiatry, 38(5), 348354.
Eaton, W. & Harrison, G. (2000) Ethnic disadvantage and schizophrenia: the psychosocial basis of schizophrenia.
Acta Psychiatrica Scandinavica, 102 Supp 407, 3843.
Fabrega, H. (1991a) Psychiatric stigma in non-western societies. Comprehensive Psychiatry, 32, 534551.
Fabrega, H. (1991b) The culture and history of psychiatric stigma in early modern and modern western societies: a
review of recent literature. Comprehensive Psychiatry, 32, 97119.
Fearon, P., Kirkbride, J.B., Morgan, C., Dazzan, P., Morgan, K., Lloyd, T., Hutchinson, G., Tarrant, J., Fung, W.L.A.,
Holloway, J., Mallett, R., Harrison, G., Leff, J., Jones, P.B. & Murray, R.M. (2006) Incidence of schizophrenia
and other psychoses in ethnic minority groups: results from the MRC AESOP Study. Psychological Medicine,
36, 15411550.
Fernando, S. (1988) Race and Culture in Psychiatry. London: Croom Helm.
Furnham, A. & Murao, M. (1999) A cross-cultural comparison of British and Japanese lay theories of schizophrenia.
International Journal of Social Psychiatry, 46(1), 420.
Hall, L.E. & Tucker, C.M. (1985) Relationships between ethnicity, conceptions of mental illness, and attitudes
associated with seeking psychological help. Psychological Reports, 57, 907916.
Halsey, R. & Patel, M. (2003) Perils of race and culture for clinical psychology trainees: the missionary position in
the 21st century. Clinical Psychology, 28, 2932.
Harrison, G., Glazebrook, C., Brewin, J., Cantwell, R., Dalkin, T., Fox, R., Jones, P. & Medley, I. (1997) Increased
incidence of psychotic disorders in migrants from the Caribbean to the United Kingdom. Psychological
Medicine, 27, 799806.
Harvey, P.D., Davidson, M., White, L., Keefe, R.S.E., Hirschowitz, R.C.M. & Davis, K.L. (1996) Empirical evaluation
of the factorial structure of clinical symptoms in schizophrenia: effects of typical neuroleptics on the Brief
Psychiatric Rating Scale. Biological Psychiatry, 40(8), 755760.
Hickling, F.W. & Hutchinson, G. (1999) Roast breadfruit psychosis: disturbed racial identification in African-
Caribbeans. Psychiatric Bulletin, 23, 132134.
Hickling, F.W. & Rodgers-Johnson, P. (1995) The incidence of first contact schizophrenia in Jamaica. British Journal
of Psychiatry, 167, 193196.
Hirai, M. & Clum, G.A. (2000) Development, reliability, and validity of the Beliefs Toward Mental Illness scale.
Journal of Psychopathology & Behavioral Assessment, 22(3), 221236.
Jarvis, E. (1998) Schizophrenia in British immigrants: recent findings, issues and implications. Transcultural
Psychiatry, 35(1), 3974.
Jablensky, A., Sartorius, N., Ernberg, G., Anker, M., Korten, A., Cooper, J.E., Kay, R. & Bertelsen, A. (1992)
Schizophrenia: manifestations, incidence and course in different cultures: a World Health Organization ten-
country study. Psychological Medicine, Monograph Supplement 20.
Johnson, S. & Orrell, M. (1996) Insight, psychosis and ethnicity: a case-note study. Psychological Medicine, 26,
10811084.
Kendell, R.E. (2001) Why stigma matters. In Every family in the land understanding prejudice and discrimination
against people with mental illness (ed A.H. Crisp). London: Royal Society of Medicine Press Ltd.
King, M., Coker, E., Leavey, G., et al. (1994) Incidence of psychotic illness in London: comparison of ethnic groups.
British Medical Journal, 309, 11151119.
King, M., Nazroo, J., Weich, S., McKenzie, K., Bhui, K., Karlson, S., Stansfeld, S., Tyrer, P., Blanchard, M., Lloyd,
K., McManus, S., Sprostan, K. & Erens, B. (2005) Psychotic symptoms in the general population of England.
Downloaded from isp.sagepub.com at UNC on September 26, 2014
260 INTERNATIONAL JOURNAL OF SOCIAL PSYCHIATRY 54(3)
A comparison of ethnic groups (The EMPIRIC study). Social Psychiatry & Psychiatric Epidemiology, 40,
375381.
Kirmayer, L.J. (1989) Cultural variations in the response to psychiatric disorders and emotional distress. Social
Science & Medicine, 29(3), 327339.
Knight, M.T.D., Wykes, T. & Hayward, P. (2003) People dont understand: An investigation of stigma in schizophrenia
using Interpretative Phenomenological Analysis (IPA). Journal of Mental Health, 12(3), 209222.
Lauber, C., Carols, N. & Wulf, R. (2005) Lay beliefs about treatments for people with mental illness and their im-
plications for antistigma strategies. Canadian Journal of Psychiatry, 50(12), 745752.
Lefley, H.P. (1990) Culture and chronic mental illness. Hospital and Community Psychiatry, 41(3), 277286.
Leong, F.T.L. & Zachar, P. (1999) Gender and opinions about mental illness as predictors of attitudes toward seeking
professional psychological help. British Journal of Guidance & Counselling, 27(1), 123132.
Link, B.G., J.C. Phelan, M. Bresnahan, A. Stueve, and B.A. Pescosolido. (1999). Public conceptions of mental illness:
Labels, causes, dangerousness and social distace. American Journal of Public Health, 89, 13281333.
Link, B.G. (1987) Understanding labelling effects in the area of mental disorders: an assessment of the effects of
expectations of rejection. American Sociological Review, 52, 96112.
Link, B.G., Struening, E.L., Rahav, M., Phelan, J.C. & Nuttbrock, L. (1997) On stigma and its consequences: evidence
from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health
and Social Behaviour, 38, 177190.
Littlewood, R. (2001) The history of stigmatization of the mentally ill cultural and national aspects of stigmatization.
In Every family in the land understanding prejudice and discrimination against people with mental illness
(ed A.H. Crisp). London: Royal Society of Medicine Press Ltd.
Mass, R. (2000) Characteristic subjective experiences of schizophrenia. Schizophrenia Bulletin, 26(4), 921931.
McEvoy, J.P., Schooler, N.R., Friedman, E., Steingard, S. & Allen, M. (1993) Use of psychopathology vignettes by
patients with schizophrenia or schizoaffective disorder and by mental health professionals to judge patients
insight. American Journal of Psychiatry, 150, 16491653.
McKenzie, K., Van Os, J., Fahy, T., Jones, P., Harvey, I., Toone B., et al. (1995) Psychosis with good prognosis in
Afro-Caribbean people now living in the United Kingdom. British Medical Journal, 311, 13251328.
Millet, P.E., Sullivan, B.F., Schwebel, A.I. & Myers, L.J. (1996) Black Americans and White Americans views of
the etiology and treatment of mental health problems. Community Mental Health Journal, 32(3), 235242.
Mind (2002) The African Caribbean community and mental health in Britain A Factsheet. At: www.mind.org.
uk/Information/Factsheets/Diversity.
Modood, T. & Berthoud, R. (1997) Ethnic Minorities in Britain Diversity and Disadvantage. London: Policy
Studies Institute.
Nketia, A. & Peters, F. (2004) Cares of Life project. Presentation at South Thames (Salomons Centre) Clinical
Psychology Training Course on Delivering culturally competent clinical practice and service provision, 14
June 2004.
Patel, N., Bennett, E., Dennis, M., Dosanjh, N., Mahtani, A., Miller, A. & Nadirshaw, Z. (eds) (2000) Clinical
Psychology, Race & Culture: A manual for trainers. Leicester: BPS Books.
Perkins, R.E. & Moodley, P. (1993) Perception of problems in psychiatric inpatients: denial, race and service usage.
Social Psychiatry and Psychiatric Epidemiology, 28, 189193.
Pinel, E.C. (1999) Stigma Consciousness: The psychological legacy of social stereotypes. Journal of Personality and
Social Psychology, 76(1), 114128.
Porter, R. (2001) The history of stigmatization of the mentally ill is mental illness inevitably stigmatizing? In Every
family in the land understanding prejudice and discrimination against people with mental illness (ed A.H.
Crisp). London: Royal Society of Medicine Press Ltd.
Pote, H.L. & Orrell, M.W. (2002) Perceptions of schizophrenia in multi-cultural Britain. Ethnicity & Health, 7(1),
720.
Robson, C. (1993) Real world research. Oxford: Blackwell.
Russell, M. (2002) A Psychosocial Construction of Psychosis: evidence from the British African-Caribbean population.
Norwich: Social Work Monographs.
Saravanan, D., David, A.S., Bhugra, D., Prince, M. & Jacob, A.S. (2005). Insight in people with psychosis: The
influence of culture. International Review of Psychiatry, 17(2): 8387.
Saravanan, B., Jacob, K.S., Prince, M., Bhugra, D. & David, A.S. (2004). Culture and Insight Revisited. British
Journal of Psychiatry, 184, 107109.
Sashidharan, S.P. (2001) Institutional Racism in British Psychiatry. Psychiatric Bulletin, 25, 244247.
Downloaded from isp.sagepub.com at UNC on September 26, 2014
STONE & FINLAY: YOUNG ADULTS CONCEPTIONS OF SCHIZOPHRENIA SYMPTOMS 261
Schnittker, J., Freese, J. & Powell, B. (2000) Nature, Nurture, Neither, Nor: Black-White differences in beliefs about
the causes and appropriate treatment of mental illness. Social Forces, 78(3), 11011130.
Taylor, S.M. & Dear, M.J. (1981) Scaling community attitudes toward the mentally ill. Schizophrenia Bulletin, 7(2),
225240.
Van Os, J., Fahy, T., Bebbington, P., Jones, P., Wilkins, S., Sham, P., et al. (1994) The influence of life events on the
subsequent course of psychotic illness. Psychological Medicine, 24, 503513.
Wahl, O.F. (1999) Mental health consumers experience of stigma. Schizophrenia Bulletin, 25(3), 467478.
L. Stone, Clinical Psychologist, Clinical Psychology Service, West Middlesex University Hospital.
W.M.L. Finlay, Senior Lecturer, Psychology Department, Surrey University.
Correspondence to: lydsgstone@hotmail.com
Downloaded from isp.sagepub.com at UNC on September 26, 2014
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- AphasiaДокумент208 страницAphasiaErika Velásquez100% (4)
- AphasiaДокумент208 страницAphasiaErika Velásquez100% (4)
- Employee Evaluation Form SummaryДокумент3 страницыEmployee Evaluation Form SummaryRahmatur RizalОценок пока нет
- Evaluating Psychological Burnout of Sports CoachesДокумент23 страницыEvaluating Psychological Burnout of Sports Coachesteto0% (1)
- Balkan Peninsula - 29-30 - 10 - 2018 - Proceedings PDFДокумент264 страницыBalkan Peninsula - 29-30 - 10 - 2018 - Proceedings PDFDean Djordjevic100% (1)
- Internal Verifier Training StandardДокумент22 страницыInternal Verifier Training StandardGanesh GanyОценок пока нет
- ReconstructionismДокумент32 страницыReconstructionismKristine Vergara Masola100% (1)
- Biol Res Nurs 2014 Leutwyler 23 30Документ9 страницBiol Res Nurs 2014 Leutwyler 23 30Santiago SainОценок пока нет
- Issues and Perspectives in Designing Clinical Trials For Negative Symptoms in Schizophrenia 2013 Schizophrenia ResearchДокумент13 страницIssues and Perspectives in Designing Clinical Trials For Negative Symptoms in Schizophrenia 2013 Schizophrenia ResearchSantiago SainОценок пока нет
- Issues and Perspectives in Designing Clinical Trials For Negative Symptoms in Schizophrenia - 2013 - Schizophrenia Research PDFДокумент6 страницIssues and Perspectives in Designing Clinical Trials For Negative Symptoms in Schizophrenia - 2013 - Schizophrenia Research PDFSantiago SainОценок пока нет
- Reviewing The Dossociative SymptomДокумент6 страницReviewing The Dossociative SymptomSantiago SainОценок пока нет
- Cognitive Task Performance and Symptoms Contribute To Personality Abnormalities in First Hospitalized Schizophrenia 2014 Journal of Psychiatric ResearДокумент9 страницCognitive Task Performance and Symptoms Contribute To Personality Abnormalities in First Hospitalized Schizophrenia 2014 Journal of Psychiatric ResearSantiago SainОценок пока нет
- Impact of Primary Negative Symptoms On Functional Outcomes in Schizophrenia 2014 European PsychiatryДокумент7 страницImpact of Primary Negative Symptoms On Functional Outcomes in Schizophrenia 2014 European PsychiatrySantiago SainОценок пока нет
- Hallucinations and Negative Symptoms Differentially Revealed by Frontal and Temporal Responses To Speech in Schizophrenia 2014 Schizophrenia ResearchДокумент6 страницHallucinations and Negative Symptoms Differentially Revealed by Frontal and Temporal Responses To Speech in Schizophrenia 2014 Schizophrenia ResearchSantiago SainОценок пока нет
- Empathy Depressive Symptoms and Social Functioning Among Individuals With Schizophrenia 2014 Psychiatry ResearchДокумент8 страницEmpathy Depressive Symptoms and Social Functioning Among Individuals With Schizophrenia 2014 Psychiatry ResearchSantiago SainОценок пока нет
- Psychopathology and Personality in Parents - SteinhausenДокумент9 страницPsychopathology and Personality in Parents - SteinhausenSantiago SainОценок пока нет
- 2006 Achievement Goals and Discrete Achievement Emotions - A TheoreticalДокумент15 страниц2006 Achievement Goals and Discrete Achievement Emotions - A TheoreticalSantiago SainОценок пока нет
- Job Advertisment 31082022638290828893059775Документ2 страницыJob Advertisment 31082022638290828893059775ZAIN SAJJAD AWANОценок пока нет
- Canada National Archives - McLuhanДокумент509 страницCanada National Archives - McLuhanDavo Lo Schiavo100% (1)
- The Stag - Issue 15Документ40 страницThe Stag - Issue 15The StagОценок пока нет
- Scholarship EssayДокумент3 страницыScholarship Essayapi-543527872Оценок пока нет
- San Rafael, Zaragoza, Nueva Ecija Junior High SchoolДокумент55 страницSan Rafael, Zaragoza, Nueva Ecija Junior High SchoolNica Mae SiblagОценок пока нет
- Dheeraj ResultДокумент2 страницыDheeraj ResultShweta JhaОценок пока нет
- HOMEROOM GUIDANCE LEARNER'S DEVELOPMENT ASSESSMENT (Junior hIGH SCHOOL)Документ2 страницыHOMEROOM GUIDANCE LEARNER'S DEVELOPMENT ASSESSMENT (Junior hIGH SCHOOL)Krizza Mae De LeonОценок пока нет
- Marder Materialsanalysis1Документ11 страницMarder Materialsanalysis1api-454914624Оценок пока нет
- Rizal's 19th Century Philippines: Reform, Education and Rising NationalismДокумент1 страницаRizal's 19th Century Philippines: Reform, Education and Rising NationalismBeatriz ArevaloОценок пока нет
- Fisica Basica Buffa y Wilson V41neДокумент4 страницыFisica Basica Buffa y Wilson V41neLiv Margunn Gutierrez HuancaОценок пока нет
- Computational Skills Topics and Sample Questions: MSU Mathematics Placement TestДокумент4 страницыComputational Skills Topics and Sample Questions: MSU Mathematics Placement TesteltytanОценок пока нет
- ICTv3 Implementation GuideДокумент98 страницICTv3 Implementation Guiderhendrax2398Оценок пока нет
- MCQ With Solution - The Story of Village Palampur - EdurevДокумент10 страницMCQ With Solution - The Story of Village Palampur - EdurevMadhusudan M60% (5)
- India EconomyДокумент216 страницIndia EconomyKishore PotnuruОценок пока нет
- Prezi PresentationДокумент2 страницыPrezi Presentationapi-481626601Оценок пока нет
- Observation Field Notes FormДокумент6 страницObservation Field Notes Formapi-240909170Оценок пока нет
- Constructivism & Integrative Plan Grade 2Документ8 страницConstructivism & Integrative Plan Grade 2CyrelOcfemiaОценок пока нет
- Differentiation StrategiesДокумент3 страницыDifferentiation Strategiesapi-315341156Оценок пока нет
- MUL 1010 Doiron F15Документ14 страницMUL 1010 Doiron F15Bob CrossОценок пока нет
- Department of Education: Attendance Sheet For ParticipantsДокумент2 страницыDepartment of Education: Attendance Sheet For ParticipantsVinMarОценок пока нет
- On Some Lessons From The Assembly LineДокумент2 страницыOn Some Lessons From The Assembly LineArindom56% (9)
- Daily Lesson Plan/LogДокумент7 страницDaily Lesson Plan/LogMyla RicamaraОценок пока нет
- Axact RespondsДокумент3 страницыAxact Respondsthe fifth estateОценок пока нет
- AP Reading List Essays & TextsДокумент6 страницAP Reading List Essays & TextsJamySam999Оценок пока нет
- Shs Answer Sheet Template For Pr1 Module 10Документ4 страницыShs Answer Sheet Template For Pr1 Module 10sheran ballesterosОценок пока нет