Академический Документы
Профессиональный Документы
Культура Документы
Hipertensi
Загружено:
yuriikeОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hipertensi
Загружено:
yuriikeАвторское право:
Доступные форматы
1932 EXPERIMENTAL AND THERAPEUTIC MEDICINE 13: 1932-1936, 2017
Abdominal ultrasonography for patients with abdominal
pain as a first-line diagnostic imaging modality
MINORU TOMIZAWA1, FUMINOBU SHINOZAKI2, RUMIKO HASEGAWA3, YOSHINORI SHIRAI3,
YASUFUMI MOTOYOSHI4, TAKAO SUGIYAMA5, SHIGENORI YAMAMOTO6 and NAOKI ISHIGE7
Departments of 1Gastroenterology, 2Radiology, 3Surgery, 4Neurology, 5Rheumatology, 6Pediatrics and
7
Neurosurgery, National Hospital Organization Shimoshizu Hospital, Yotsukaido, Chiba 2840003, Japan
Received August 30, 2015; Accepted January 20, 2017
DOI: 10.3892/etm.2017.4209
Abstract. The utility and limitations of abdominal Introduction
ultrasonography (US) were retrospectively evaluated as
a firstline diagnostic imaging modality in patients with Abdominal pain is one of the most common symptoms
abdominal pain. Hospital records from patients subjected to prompting patients to visit hospitals. Among such individuals,
abdominal US as a firstline diagnostic imaging examination a number of patients have serious diseases and require subse-
at the National Hospital Organization Shimoshizu Hospital quent hospitalization or surgery. Diagnosis may consist of acute
(Yotsukaido, Japan) from April2010 to April2015 were appendicitis, intestinal obstruction and other serious conditions
analyzed. Only those patients who underwent abdominal US such as bowel necrosis and intestinal volvulus(1). Correct
to diagnose abdominal symptoms were included in the present and prompt diagnosis is essential for the appropriate manage-
study. All patients with prior diagnostic imaging examination ment of patients. Diagnosis of patients with abdominal pain is
findings were excluded from the study in order to reduce bias primarily determined by imaging techniques, such as radiog-
of results. The analyzed patients included 39males with an raphy, abdominal ultrasonography (US), computed tomography
average (meanstandard deviation) age of 65.818.8years and (CT) and magnetic resonance imaging (MRI)(2). Among these,
37females with an average age of 53.719.3years. Diagnosis abdominal US is a noninvasive procedure, which is readily
with abdominal US was in agreement with the final diagnosis available at most hospitals even during offhours (weekends,
in 66of the 76patients. Final diagnosis of symptoms by nights and holidays) and may be performed at the bedside(3).
abdominal US was not successful in the remaining 10patients Abdominal US is indispensable for the diagnosis of
who required further investigation. Acute cholangitis, acute diseases in the abdominal cavity in patients with abdominal
cholecystitis, acute pancreatitis, acute appendicitis, colonic symptoms(4,5). In addition, abdominal US is also useful
diverticulitis and spleen rupture were correctly diagnosed. for the diagnosis of solid organ conditions, including acute
Different types of cancer, including colorectal cancer, were also cholangitis, acute cholecystitis and acute pancreatitis(68).
successfully diagnosed. Bile duct cancer and sigmoid colon Abdominal US is also useful in the diagnosis of bowel disease
volvulus could not be diagnosed by abdominal US due to the based on pathological findings(9,10). Diagnostic criteria with
presence of intestinal gas. Abnormal findings were detected abdominal US have been established for acute appendicitis and
using abdominal US, but the diagnosis required additional colonic diverticulitis(1114) and colorectal cancer may be diag-
consultation with gynecologists. Abdominal US was suitable nosed with abdominal US(15). In numerous cases, patients are
for patients with abdominal symptoms. It is recommended that diagnosed by a combination of laboratory data and diagnostic
patients undergo further diagnostic imaging or consultation imaging findings based on symptoms and physical examina-
with gynecologists when large gas bubbles are present or tion. With regards to diagnostic imaging, CT is recommended
gynecological conditions are suspected. as the firstline procedure(16); however, CT is not readily avail-
able during offh at the majority of hospitals. In these cases,
abdominal US is the firstline procedure performed.
On the basis of the aforementioned considerations, the
current study retrospectively analyzed the records of patients
Correspondence to: Dr Minoru Tomizawa, Department of
who underwent abdominal US as a firstline diagnostic
Gastroenterology, National Hospital Organization Shimoshizu
Hospital, 9345Shikawatashi, Yotsukaido, Chiba 2840003, Japan
imaging procedure in order to evaluate its utility and limita-
Email: nihminorcib@umin.ac.jp tions in determining the diagnosis of patients presenting with
abdominal symptoms.
Key words: acute appendicitis, colonic diverticulitis, ovarian
torsion Materials and methods
Patients. Medical records were retrospectively analyzed
for 76patients who were subjected to abdominal US as the
TOMIZAWA etal: US FOR DIAGNOSIS DURING ACUTE ABDOMINAL PAIN 1933
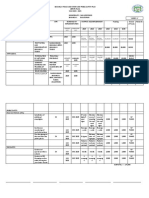
firstline diagnostic imaging modality at the National Hospital Table I. Diseases successfully diagnosed with abdominal
Organization Shimoshizu Hospital (Yotsukaido, Japan) from ultrasonography.
April2010 to April2015. Abdominal US was performed at the
time of consultation or during offhours (weeknights, week- Number Number of
ends and holidays). Recruited patients were restricted to those of offhoura
in which abdominal US was performed as a first diagnostic Diagnosis patients patients
approach in order to evaluate the diagnostic performance
solely from abdominal US without any potentially confounding Acute cholangitis 15 3
information from other diagnostic imaging procedures. Thus, Acute appendicitis 11 9
patients were excluded when abdominal US was performed Acute cholecystitis 7 0
following another diagnostic imaging procedures, such as Acute pancreatitis 7 4
radiography, CT or MRI because the sonographer may have Enteritis 7 4
been informed of the findings obtained. The analyzed patients Colonic diverticulitis 5 3
included 39males with an average (meanstandard deviation) Ileus 2 2
age of 65.818.8years and 37females with an average age of Colorectal cancer 2 1
53.719.3years. Hepatocellular carcinoma 2 0
Patients were hospitalized or referred to a different hospital
Pancreatic cancer 2 0
based on the diagnosis obtained by abdominal US, the results
Bile duct cancer 2 1
of blood examinations, clinical findings or diagnostic imaging
following abdominal US. The National Hospital Organization Bowel perforation 2 2
Shimoshizu Hospital does not have a department of gynecology. Spleen rupture 1 0
Therefore, patients were referred to another hospital for gyne- Upper gastrointestinal bleeding 1 1
cological consultation. The referred hospitals were National Total 66 30
Hospital Organization Chiba Medical Center (Chiba, Japan)
and Seirei Sakura Citizen Hospital (Sakura, Japan). During Weeknights, weekends and holidays.
a
offhours, the management of patients was determined on the
basis of abdominal US and clinical symptoms. The present
study was approved by the Ethics Committee of the National
Hospital Organization Shimoshizu Hospital. It was not consid- diagnosed when abdominal US revealed a swollen pancreas,
ered a clinical trial since abdominal US was performed as a fluid collection and inflammation of adjacent organs. Acute
part of routine clinical practice. Written informed consent for diverticulitis was diagnosed as diverticulum with thickened
inclusion in the study was waived. Patient records/information wall and high echo from the surrounding tissue (Fig.1A)(12).
was anonymized and deidentified prior to analysis. Acute appendicitis was diagnosed as swollen appendix with a
diameter >10mm, and thickened wall (Fig.1B)(13,14).
Abdominal US. Abdominal US was performed by Senior
Fellows of the Japan Society of Ultrasonics in Medicine Results
(Tokyo, Japan; http://www.jsum.or.jp/jsume/index.html)
using a SSA700A US system (Toshiba Medical Systems Successful diagnosis of patients. Initial diagnosis with abdom-
Corporation, Ohtawara, Japan) with a 3.75MHz curvedarray inal US was in agreement with the final diagnosis in 66patients.
probe (PVT375BT; Toshiba Medical Systems Corporation) or For the remaining 10patients, the diagnosis obtained from
an 8.0MHz lineararray probe (PLT805AT; Toshiba Medical abdominal US differed from the final diagnosis. To investigate
Systems Corporation). the performance and limitations of abdominal US, patients
were divided into two groups. The first included patients in
Diagnostic criteria of diseases. Acute cholangitis is defined as whom abdominal US diagnosis agreed with the final diagnosis
inflammation due to the obstruction of a bile duct(6). Findings (TableI) and the other included patients whose initial abdominal
detectable by abdominal US include bile duct dilatation and US diagnosis differed from the final diagnosis (TableII).
evidence of its etiology, such as stricture, stones or stent(6). In
the present study, in the absence of these findings, acute chol- Colorectal cancer and spleen rupture. Solid organ diseases,
angitis was not diagnosed by abdominal US, but was based on including acute cholangitis, acute cholecystitis and acute
a combination of symptoms including systemic inflammation pancreatitis, were correctly diagnosed by abdominal US.
and cholestasis(6). Acute cholecystitis was diagnosed by a Intestinal diseases, including acute appendicitis and colonic
combination of local and systemic signs of inflammation(7). diverticulitis, were also correctly diagnosed. Abdominal
Abdominal US supported the diagnosis with findings of US was useful for the diagnosis of various types of cancer,
distension, wall thickening and sludge in the gallbladder(7). including hepatocellular carcinoma, pancreatic cancer, and
More specifically, the finding of a sonographic Murphy sign colorectal cancer (Fig.2A). Colorectal cancer findings included
was considered the most reliable because it is considered to irregular shaped wall thickening and loss of stratification, also
suggest inflammation of the gallbladder(17). referred to as the pseudokidney sign(15). Critical conditions,
Acute pancreatitis is typically diagnosed as abdominal pain, such as rupture of the spleen, were also successfully diagnosed
elevated serum amylase and swelling of the pancreas by diag- with abdominal US (Fig.2B). Fluid in the abdominal cavity
nostic imaging(18). In the current study, acute pancreatitis was and high echo in the spleen suggested bleeding and damaging
1934 EXPERIMENTAL AND THERAPEUTIC MEDICINE 13: 1932-1936, 2017
Table II. List of misdiagnosed patients and speculated causes of misdiagnosis following abdominal ultrasound.
Patient Age Consultation or
number Gender (years) Final diagnosis Cause of misdiagnosis offhour
1 F 49 Acute cholangitis Bile duct diameter C
within normal range
2 M 69 Bile duct cancer, Bile duct cancer not O
acute cholangitis detected due to gas
3 M 88 Sigmoid colon Difficult to examine due to O
volvulus presence of massive gas bubbles
4 F 87 Acute appendicitis Appendix not detected O
5 M 39 Intestinal anisakiasis Anisakiasis not detected O
6 F 89 Duodena Ulcer Tentatively diagnosed as acute C
cholecystitis due to a positive
sonographic Murphy sign
7 M 53 Spontaneous Nature of ascites not O
hemoperitoneum examined with US
8 F 40 Recurrence of Presence of a huge mass in the O
cervical cancer pelvis of unknown origin
9 F 48 Left ovarian torsion Torsion not diagnosed by US C
10 F 57 Inflammation of uterus Inflammation of the uterus C
not diagnosed
F, female; M, male; O, offhour (weeknights, weekends, and holidays); C, consultation; US, ultrasound.
Figure 2. Colorectal cancer and spleen rupture. (A)A 79yearold female
Figure 1. Acute appendicitis and colonic diverticulitis. (A)A 33yearold
was admitted to hospital with lower abdominal pain. Abdominal ultrasonog-
male was admitted to hospital with right lower abdominal pain. Abdominal
raphy demonstrated a masslike lesion in the sigmoid colon (pseudokidney
ultrasonography demonstrated diverticula with thickened wall containing
sign). The patient was diagnosed with sigmoid colorectal cancer. (B)A
air (arrows). High echo tissue surrounded the diverticulum (*), suggesting an
64yearold male was hospitalized following a rib fracture. The patient had
inflamed mesentery and omentum. The patient was diagnosed with colonic
left upper back pain and was subjected to abdominal ultrasonography. An
diverticulitis. (B)A 34yearold male was admitted to hospital with right
irregularshaped high echo lesion was detected in the spleen (arrow) and
lower abdominal pain. Abdominal ultrasonography indicated a swollen
fluid was observed near the spleen (arrowhead). The patient was diagnosed
appendix with a diameter of 11mm (arrowheads; dotted line). The patient
with spleen rupture.
was diagnosed with acute appendicitis.
suggested the necessity of further management. Two patients
lesions, respectively(19). A total of 30patients were admitted were referred to another hospital for gynecological consulta-
outside of regular working h and were subjected to abdominal tion. All patients described in TableII were appropriately
US. They were correctly diagnosed without being subjected managed, according to their condition.
to CT or other diagnostic imaging procedures. These results One major cause of misdiagnosis was intestinal gas. Gas
clearly indicate that abdominal US is useful for the diagnosis over the site of the disease made the examination difficult to
of patients presenting with abdominal symptoms specifically execute. Gas over the bile duct (patient 2) hindered the detec-
during offhours. tion of bile duct cancer. Gas in the sigmoid colon made the
examination difficult for patient 3.
Unsuccessful diagnosis of patients. TableII summarizes data
from those patients who were misdiagnosed by abdominal Unsuccessful diagnosis of acute appendicitis and duodenal
US and the potential reasons for misdiagnosis. These patients ulcer. A diagnosis of acute appendicitis was hampered
were subjected to additional diagnostic imaging procedures when it was not possible to detect the appendix (patient 4;
and were hospitalized for treatment because their conditions Fig.3A)(20).
TOMIZAWA etal: US FOR DIAGNOSIS DURING ACUTE ABDOMINAL PAIN 1935
abnormal findings in the pelvis, particularly in the ovary and
uterus.
Discussion
The presence of gas bubbles makes abdominal US difficult
to perform(21). Large amounts of gases arise due to perfo-
ration and obstruction of the bowel(22,23). In the current
study, bile duct cancer and sigmoid colon volvulus were not
Figure 3. Misdiagnosis by abdominal ultrasonography. (A)An 87yearold diagnosed using abdominal US due to the presence of intes-
female was admitted to hospital with right lower abdominal pain. The tinal gas. Sigmoid colon volvulus requires prompt diagnosis
patient's abdominal ultrasonography indicated that there was fluid (arrow) followed by surgical or endoscopic treatment(24). An upside
near the terminal ileum and cecum. The appendix was not identified. The
patient was diagnosed with acute appendicitis following further investigation. down Ushaped loop of dilated bowel is a typical radiological
(B)An 89yearold male was referred to the National Hospital Organization finding(25). With regards to abdominal US, findings specific
Shimoshizu Hospital with right upper abdominal pain. An abdominal to sigmoid colon volvulus have not been reported(26).
ultrasound indicated a distended gallbladder. The patient presented with Abdominal US is not, therefore, suitable for the diagnosis
tenderness at the gallbladder, suggesting a sonographic Murphy sign. Wall
thickening of the gallbladder was not conclusive. The patient was diagnosed of sigmoid colon volvulus. It is recommended that patients
with acute cholecystitis. The diagnosis was controversial due to the lack of should be subjected to radiography and CT when sigmoid
evident wall thickening therefore, an upper gastrointestinal endoscopy was colon volvulus is suspected(27).
performed and the patient was subsequently diagnosed with a duodenal ulcer. The diagnosis of acute appendicitis with abdominal US
is challenging when the appendix is unable to be visual-
ized(20). In such cases, a large amount of fluid, phlegmon
and pericecal inflammatory fat changes are clear indications
for the diagnosis of acute appendicitis(20). In the present
study, fluid and high echo tissues were detected (Fig.3A) and
these findings suggested acute appendicitis. However, it was
not possible to exclude the diagnosis of colonic diverticulitis
or peritonitis. It was concluded that acute appendicitis is
difficult to diagnose without the direct observation of the
appendix.
Abdominal US is useful for gynecologists in the diagnosis
Figure 4. Misdiagnosis of gynecological diseases. (A)A 48yearold female of gynecological emergencies(28). Abnormal findings in the
was admitted to hospital with lower abdominal pain. The patient's abdominal
ultrasonography indicated a cystic lesion with sludgelike material (arrow)
pelvis were detected in the current study, although a precise
in the left ovary. The patient was referred for a gynecological consultation at diagnosis was delayed since patients had to be referred to a
different institution and was subsequently diagnosed with left ovary torsion. gynecologist at a different institution for consultation. Among
(B)A 57yearold female was admitted to hospital with lower abdominal pain. patients in the present study, ovarian torsion was the most
The abdominal ultrasonography indicated the presence of fluid (arrowhead)
between the sigmoid colon (*) and the uterus (**). Peristalsis was weakened in
critical condition. Ovarian torsion is diagnosed based on
the sigmoid colon. The patient was referred for a gynecological consultation clinical symptoms, abdominal US, CT, and MRI(29). Color
at a different institution and was subsequently diagnosed with inflammation Doppler US reveals absent or diminished central venous flow
of the uterus. in patients with ovarian torsion(5). However, a diagnosis of
ovarian torsion is difficult to achieve(29). A previous report, in
addition to the results from the patients in the current study, has
A sonographic Murphy sign markedly suggests acute suggested that gynecological diseases are difficult to correctly
cholecystitis when abdominal US findings include disten- diagnose with abdominal US alone(28). It is recommended
sion and wall thickening of the gallbladder(17). Since the that a patient should be promptly referred to a gynecologist if
duodenum is close to the gallbladder, the tenderness perceived an emergency condition is suspected.
in duodenal ulcer may occasionally resemble a sonographic One of the limitations of the present study was the rela-
Murphy sign (patient 6; Fig.3B). tively small number of patients examined. The number of
patients was limited as the study was restricted to patients
Unsuccessful diagnosis of gynecological diseases. A major subjected to abdominal US as the first diagnostic imaging
difficulty in successful diagnosis with abdominal US was the method. The initial aim of the present study was to evaluate
presence of gynecological disorders. It was not difficult to the diagnostic performance of firstline abdominal US for
detect a mass in the pelvis (patient 8) or a cystic lesion in the patients presenting with abdominal symptoms. If information
ovary (patient 9; Fig.4A), however it was difficult to diagnose from the other diagnostic imaging examinations was available
the site or organ of the original lesion, or relative torsion. The prior to abdominal US, this information may have interfere
abdominal US clearly illustrated ascites and weakened peri- with the overall outcome of the abdominal US.
stalsis of the sigmoid colon (patient 10; Fig.4B), but the correct In the present study, performing an abdominal US was
diagnosis required subsequent referral to a gynecologist. Thus, suitable for the correct diagnosis of patients presenting with
these results suggested that patients should be referred for abdominal symptoms. CT is sensitive, but requires exposure
gynecological consultation when the abdominal US indicates to radiation; abdominal US reduces the necessity of CT, and
1936 EXPERIMENTAL AND THERAPEUTIC MEDICINE 13: 1932-1936, 2017
lowers the exposure (30). It is recommended that patients 14. RodgersPM and VermaR: Transabdominal ultrasound for bowel
evaluation. Radiol Clin North Am51: 133148, 2013.
should undergo further diagnostic imaging examinations when 15. TomizawaM, ShinozakiF, HasegawaR, FugoK, ShiraiY,
large gas bubbles are observed(31). It is also recommended IchikiN, SugiyamaT, YamamotoS, SueishiM and YoshidaT:
that patients should be referred to a gynecologist when gyne- Screening ultrasonography is useful for the diagnosis of gastric
and colorectal cancer. Hepatogastroenterology60: 517521, 2013.
cological diseases are suspected. 16. StokerJ, van RandenA, Lamris W and Boermeester MA:
In conclusion, abdominal US was suitable for the diagnosis Imaging patients with acute abdominal pain. Radiology253:
of patients with abdominal symptoms. It is recommended that 3146, 2009.
17. MyrianthefsP, EvodiaE, VlachouI, PetrocheilouG, GavalaA,
further diagnostic imaging be performed for patients with a PappaM, BaltopoulosG and KarakitsosD: Is routine ultrasound
large gas bubbles and that patients be referred to a gynecolo- examination of the gallbladder justified in critical care patients?
gist when gynecological diseases are suspected. Crit Care Res Pract2012: 565617, 2012.
18. WuBU and BanksPA: Clinical management of patients with
acute pancreatitis. Gastroenterology144: 12721281, 2013.
References 19. KornerM, KrtzMM, DegenhartC, PfeiferKJ, ReiserMF and
LinsenmaierU: Current role of emergency US in patients with
1. PaduszynskaK, CelnikA and PomorskiL: Patients subject to major trauma. Radiographics28: 225242, 2008.
surgery due to acute abdominal disorders during the period 20. EsteyA, PoonaiN and LimR: Appendix not seen: The predic-
between 20012004. Pol Przegl Chir84: 488494, 2012. tive value of secondary inflammatory sonographic signs. Pediatr
2. HayesR: Abdominal pain: General imaging strategies. Eur Emerg Care29: 435439, 2013.
Radiol14 (Suppl 4): L123L137, 2004. 21. HoffmannB, NurnbergD and WestergaardMC: Focus on
3. RozyckiGS, CavaRA and TchorzKM: Surgeonperformed abnormal air: Diagnostic ultrasonography for the acute abdomen.
ultrasound imaging in acute surgical disorders. Curr Probl Eur J Emerg Med19: 284291, 2012.
Surg38: 141212, 2001. 22. GrassiR, RomanoS, PintoA and RomanoL: Gastroduodenal
4. PuylaertJB, van der ZantFM and RijkeAM: Sonography perforations: Conventional plain film, US and CT findings in 166
and the acute abdomen: Practical considerations. AJR Am J consecutive patients. Eur J Radiol50: 3036, 2004.
Roentgenol168: 179186, 1997. 23. HuclT: Acute GI obstr uction. Best Pract Res Clin
5. BirnbaumBA and JeffreyRB Jr: CT and sonographic evalua- Gastroenterol27: 691707, 2013.
tion of acute right lower quadrant abdominal pain. AJR Am J 24. YeoHL and LeeSW: Colorectal emergencies: Review and
Roentgenol170: 361371, 1998. controversies in the management of large bowel obstruction.
6. KiriyamaS, TakadaT, StrasbergSM, SolomkinJS, MayumiT, JGastrointest Surg17: 20072012, 2013.
PittHA, GoumaDJ, GardenOJ, BchlerMW, YokoeM,etal: 25. JamesB and KellyB: The abdominal radiograph. Ulster Med
New diagnostic criteria and severity assessment of acute chol- J82: 179187, 2013.
angitis in revised Tokyo Guidelines. JHepatobiliary Pancreat 26. LimJH, KoYT, LeeDH, LeeHW and LimJW: Determining the
Sci19: 548556, 2012. site and causes of colonic obstruction with sonography. AJR Am
7. YokoeM, TakadaT, StrasbergSM, SolomkinJS, MayumiT, J Roentgenol163: 11131117, 1994.
GomiH, PittHA, GoumaDJ, GardenOJ, BchlerMW,etal: 27. GingoldD and MurrellZ: Management of colonic volvulus. Clin
New diagnostic criteria and severity assessment of acute chole- Colon Rectal Surg25: 236244, 2012.
cystitis in revised Tokyo Guidelines. JHepatobiliary Pancreat 28. PopowskiT, HuchonC, FathallahK, FalissardB, DumontA and
Sci19: 578585, 2012. FauconnierA: Impact of accreditation training for residents on
8. ScaglioneM, CascianiE, PintoA, AndreoliC, De VargasM and sonographic quality in gynecologic emergencies. JUltrasound
GualdiGF: Imaging assessment of acute pancreatitis: A review. Med34: 829835, 2015.
Semin Ultrasound CT MR29: 322340, 2008. 29. GerscovichEO, CorwinMT, SekhonS, RunnerGJ and
9. MaturenKE, WasnikAP, KamayaA, DillmanJR, KazaRK, GandourEdwards RF: Sonographic appearance of adnexal
PandyaA and MaheshwaryRK: Ultrasound imaging of bowel torsion, correlation with other imaging modalities, and clinical
pathology: Technique and keys to diagnosis in the acute abdomen. history. Ultrasound Q30: 4955, 2014.
AJR Am J Roentgenol197: W1067W1075, 2011. 30. LamerisW, van RandenA, van EsHW, van HeesewijkJP,
10. PuylaertJB: Ultrasound of acute GI tract conditions. Eur van RamshorstB, BoumaWH, ten HoveW, van LeeuwenMS,
Radiol11: 18671877, 2001. van KeulenEM, DijkgraafMG,etal: Imaging strategies for
11. KarulM, BerlinerC, KellerS, TsuiTY and YamamuraJ: Imaging detection of urgent conditions in patients with acute abdominal
of appendicitis in adults. Rofo186: 551558, 2014. pain: Diagnostic accuracy study. BMJ338: b2431, 2009.
12. PuylaertJB: Ultrasound of colon diverticulitis. Dig Dis30: 31. FarinaR, CatalanoO, StavoloC, SandomenicoF, PetrilloA and
5659, 2012. RomanoL: Emergency radiology. Radiol Med120: 7384, 2015.
13. OomsHW, KoumansRK, Ho Kang YouPJ and PuylaertJB:
Ultrasonography in the diagnosis of acute appendicitis. Br
JSurg78: 315318, 1991.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Efficacy and Safety of Sunscreen Use For The Prevention of Skin Cancer CMAJДокумент1 страницаThe Efficacy and Safety of Sunscreen Use For The Prevention of Skin Cancer CMAJyuriikeОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- J. Nutr. 2006 Charlton 295S 8SДокумент4 страницыJ. Nutr. 2006 Charlton 295S 8SyuriikeОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Amitriptilin in Tension Type HeadacheДокумент6 страницAmitriptilin in Tension Type HeadacheyuriikeОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Daftar Pustaka: Infect 78: 90-92Документ5 страницDaftar Pustaka: Infect 78: 90-92yuriikeОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Acute Hepatitis C: Prospects and Challenges: EditorialДокумент3 страницыAcute Hepatitis C: Prospects and Challenges: EditorialyuriikeОценок пока нет
- 151 291 1 PBДокумент9 страниц151 291 1 PByuriikeОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Oxidative Stress and Benefits of Antioxidant Agents in Acute and Chronic HepatitisДокумент8 страницOxidative Stress and Benefits of Antioxidant Agents in Acute and Chronic HepatitisyuriikeОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Cefotaxime Clinical Pathway Effectiveness in Preventing Surgical Site InfectionДокумент8 страницCefotaxime Clinical Pathway Effectiveness in Preventing Surgical Site InfectionyuriikeОценок пока нет
- Activation of Trigeminovascular SystemДокумент3 страницыActivation of Trigeminovascular SystemyuriikeОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Ultrasound Findings in Critical Care Patients: The "Liver Sign" and Other Abnormal Abdominal Air Patterns PDFДокумент7 страницUltrasound Findings in Critical Care Patients: The "Liver Sign" and Other Abnormal Abdominal Air Patterns PDFyuriikeОценок пока нет
- PR DR SantyДокумент10 страницPR DR SantyyuriikeОценок пока нет
- Daftar Pustaka: Infect 78: 90-92Документ5 страницDaftar Pustaka: Infect 78: 90-92yuriikeОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Jurnal Radio Edit 3Документ33 страницыJurnal Radio Edit 3yuriikeОценок пока нет
- HypertensionДокумент6 страницHypertensionyuriikeОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- 3 s2.0 B9781416056829502109Документ2 страницы3 s2.0 B9781416056829502109yuriikeОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- HJKHДокумент10 страницHJKHyuriikeОценок пока нет
- 3 s2.0 B9781416056829502109Документ2 страницы3 s2.0 B9781416056829502109yuriikeОценок пока нет
- 3 s2.0 B9780323321082000299Документ43 страницы3 s2.0 B9780323321082000299yuriikeОценок пока нет
- Bioreactor For Air Pollution ControlДокумент6 страницBioreactor For Air Pollution Controlscarmathor90Оценок пока нет
- GP Series Portable Generator: Owner's ManualДокумент48 страницGP Series Portable Generator: Owner's ManualWilliam Medina CondorОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Corn Genetics and Chi Square AnalysisДокумент2 страницыCorn Genetics and Chi Square AnalysisBonifacius Budi NugrohoОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Preparation of Salts (Multiple Choice) QPДокумент8 страницPreparation of Salts (Multiple Choice) QPkhalil rehmanОценок пока нет
- CASE Study PTBДокумент53 страницыCASE Study PTBmeleanaquino94% (16)
- Personal and Group Trainer Juan Carlos GonzalezДокумент2 страницыPersonal and Group Trainer Juan Carlos GonzalezDidier G PeñuelaОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Chronic Pain GuidelinesДокумент56 страницChronic Pain GuidelinesOporadhBiggan100% (1)
- Kathrein Antenna Dual BandДокумент4 страницыKathrein Antenna Dual BandAmine AchrafОценок пока нет
- EIM GRADE 9 10 Q4 Module 1b - National Electrical Code NEC Provisions in Installing Wiring Devices - GFCI. - FinalДокумент23 страницыEIM GRADE 9 10 Q4 Module 1b - National Electrical Code NEC Provisions in Installing Wiring Devices - GFCI. - FinalTitser Ramca100% (3)
- Lazzaro Spallanzani ExperimentДокумент14 страницLazzaro Spallanzani ExperimentWiwi Pratiwi100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Strategies and Tactics for Collecting on Overdue AccountsДокумент9 страницStrategies and Tactics for Collecting on Overdue AccountsAkii WingОценок пока нет
- 1 6Документ58 страниц1 6Emiliano.Armando Aguilera.Vázquez100% (1)
- Being ProfessionalДокумент3 страницыBeing ProfessionalPutra SyahrezaОценок пока нет
- (Distracted Subjects) CHAPTER 2. Reading The Language of Distraction - Hamlet, Macbeth, King LearДокумент23 страницы(Distracted Subjects) CHAPTER 2. Reading The Language of Distraction - Hamlet, Macbeth, King LearLCAP ConsultingОценок пока нет
- MIDWIFE1115ra Tugue e PDFДокумент9 страницMIDWIFE1115ra Tugue e PDFPhilBoardResultsОценок пока нет
- Asian Organized CrimeДокумент17 страницAsian Organized CrimeMagr EscaОценок пока нет
- Penyakit Palpebra Dan AdneksaДокумент39 страницPenyakit Palpebra Dan AdneksaayucicuОценок пока нет
- 2016 Ruptured Pseudoaneurysm of The Middle Meningeal ArteryДокумент5 страниц2016 Ruptured Pseudoaneurysm of The Middle Meningeal ArteryJulio Cesar Velasco CastroОценок пока нет
- Sem-V Principle of Taxation Law PDFДокумент3 страницыSem-V Principle of Taxation Law PDFAnantHimanshuEkkaОценок пока нет
- DaloДокумент2 страницыDalojosua tuisawauОценок пока нет
- SureFlo RДокумент2 страницыSureFlo RKen NgОценок пока нет
- Working at Height ProcedureДокумент11 страницWorking at Height ProcedureAniekan AkpaidiokОценок пока нет
- Microeconomics 5th Edition Hubbard Solutions Manual 1Документ23 страницыMicroeconomics 5th Edition Hubbard Solutions Manual 1christina100% (48)
- KPI and Supplier Performance Scorecard ToolДокумент7 страницKPI and Supplier Performance Scorecard ToolJayant Kumar JhaОценок пока нет
- Bio23 LindenДокумент34 страницыBio23 LindenDjamal ToeОценок пока нет
- Literature Review On Female InfertilityДокумент7 страницLiterature Review On Female Infertilityea68afje100% (1)
- 16 Point Msds Format As Per ISO-DIS11014 PDFДокумент8 страниц16 Point Msds Format As Per ISO-DIS11014 PDFAntony JebarajОценок пока нет
- SinogramДокумент2 страницыSinogramNguyễn Thành CôngОценок пока нет
- Acute Atelectasis Prevention & TreatmentДокумент9 страницAcute Atelectasis Prevention & TreatmentmetabolismeproteinОценок пока нет
- Barangay Peace and Order and Public Safety Plan Bpops Annex AДокумент3 страницыBarangay Peace and Order and Public Safety Plan Bpops Annex AImee CorreaОценок пока нет