Академический Документы
Профессиональный Документы
Культура Документы
Pain Modulation
Загружено:
smartie_chaiАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pain Modulation
Загружено:
smartie_chaiАвторское право:
Доступные форматы
Pain Modulation
Pain modulation means pain perception variability which is influenced by:
Endogenous mechanism
Exogenous mechanism
Pain modulation can be discussed under following headings:
Spinal modulation of pain input
Gate theory of pain
Supra spinal modulation
Role of periaqueductal grey (PAG) matter
Role of Nucleus Raphe Magnus (NRM)
Pain modulation by use of Opioid neurotransmitters eg: endorphin, enkaphalin
Dynorphin.
The gate theory of pain control:
Special neurons located in the grey matter of the spinal cord (the dorsal horn of
spinal cord SGR) form the gate through which pain impulses must pass to reach
brain.
Three variables control this gate:
A-Delta fibres (fast pain). (Strongest)
C- fibres (slow pain).
A-Beta fibres (light touch).
Pain Gate Theory
This gate has the ability to block the signals from the A-delta and C fibres
preventing them from reaching the brain.
Gate opened or closed by 3 factors:
1.Activity in the pain fibres - opens the gate.
2.Activity in other sensory nerves - closes the gate.
3.Messages from the brain.
The gate theory of pain control (Cont.)
Mechanism:
Impulses coming along type C pain fibers cause the release of substance P
from these fibers and tend to open the gate.
While impulses coming along A fibers tend to keep the gate closed by
process of presynaptic inhibition of C fibers and postsynaptic inhibition of
secondary neurons in dorsal horn.
o If impulses in the C and A-Delta Fibres are stronger than the A-beta
Fibres the gate opens.
o If impulses in the A-beta Fibres are stronger than the C and A-Delta
Fibres the gate closes.
A-delta fibres are always stronger!
Explanation
Gate Control Theory:
Having learnt this from practical experience, shaking/rubbing an injured area results
in a decreased amount of pain, have you ever wondered why?
The theory behind this is the gate control of pain which states: Pain is a function of
the balance between the information travelling into the spinal cord through large
(touch, pressure, vibration) nerve fibres [carrying non-nociceptive information] and
information travelling into the spinal cord through thin (pain) nerve fibres [carrying
nociceptive information]. If the relative amount of activity is greater in large
nerve fibres, there should be little or no pain. However, if there is more
activity in small nerve fibres, then there will be pain.
Lets go through this theory in steps:
1) Both thin (pain) and large (touch, pressure, vibration) nerve fibres carry information
from site of injury to 2 destinations.
2) The 2 destinations are:
(a) dorsal horn of spinal cord; transmission cells that carry pain signals up to the
brain and
(b) inhibitory interneurons that impede transmission cells activity.
3) When both nerve fibres are active transmission cells are excited
4) Activity in thin fibres inhibitory cells are impeded; allowing transmission cells to
fire
5) Activity in large fibres inhibitory cells excited; inhibiting transmission cell activity
6) Hence, the more large nerve fibres activated in comparison to thin ones, the less pain
is felt.
7) So, WITHOUT any stimulation: both large and thin nerve fibres are quite and the
inhibitory interneurons BLOCKS the signal in the projection neuron (that connects to
the brain); gate is CLOSED; NO PAIN
8) With NON-PAINFUL stimulation: large nerve fibres are activated; activating the
projecting neuron AND activating the inhibitory interneurons (which now blocks the
signal in the projection neuron that connects to the brain); gate is CLOSED; NO PAIN
9) With PAINFUL stimulation: thin nerve fibres become more active, activating the
projection neuron AND BLOCKING the inhibitory interneurons; pain signal is NOT
BLOCKED; gate is OPEN; PAIN!
10) So this is the explanation behind skin rubbing, shaking the painful part,
transcutaneous electrical stimulation & acupuncture; to STIMULATE
mechanoreceptors that ACTIVATE neurons of dorsal column large fibres, allowing
them to TAKE OVER the thin fibres activity.
The gate theory of pain control (Cont.)
- So is that what controls the gate only?
No, there is also control by HIGHER CENTRES called control triggers
- How do these centres control the gate?
Via specialised nerve impulses that arise in the brain, inhibitory and excitatory
nerve signals travel down and influence the gate sensitising it to either C or A- fibres.
Supra spinal modulation (Special pain control analgesic system)
This is a specific system that blocks pain transmission in CNS. Its major constituents
are, so what areas of the brain are responsible for pain REDUCTION?
Periaqueductal Gray (PAG) in midbrain
Nucleus raphe magnus (NRM) in upper medulla
Periventricular nucleus in hypothalamus, near 3rd ventricle
Pain inhibitory complex (PIC) in dorsal horn of spinal cord:
- It consists of multiple short encephalinergic neurons that terminate on
central endings of pain conducting afferent fibers
- When stimulated the released encephalin cause pre & postsynaptic inhibition
of pain transmission i.e it prevents the release of substance P from pain nerve
endings.
Analgesia occurs as follows:
Periaqueductal grey area receives neuronal inputs from thalamus, hypothalamus,
cerebral cortex.
PAG projects neurons containing aspartate & glutamate that stimulate raph magnus
nucleus (RMN)
RMN projects serotoninergic neurons, this in addition to noradrenergic neurons project
from adjacent medulla to dorsal horn. They block pain signals by activating PIC.
1 2
7 6 5
Opiod receptor modulation:
What are opioid peptides?
Opioid peptides are morphine-like substances present in body.
They are natural analgesic substances that act by binding to opiate receptors in
analgesic system and dorsal horn of SC on central ending of pain
conducting pain fibers.
Mechanism of opiod neurotransmitter action:
Endorphin: Neurons using endorphin or enkaphalin are found in PAG where
they inhibit GABAnergic interneurons that normally suppress the anti-
nociceptor neurons
Enkephalin: It is used by interneurons in lamina II responsible for inhibiting
the lamina I nocioceptor-specific spinothalamic neurons
Dynorphin: In hypothalamus, PAG, reticular formation, and dorsal horn.
Endogenous morphin: In terminals forming synapses with neuron having -
opioid receptors in pain modulating pathways.
Opioid Antagonist: Naloxone
Used to reverse opioid overdose
Displaces receptor-bound opioids
Good for overcoming respiratory and CV depression
Different Pain sensations:
Hyperalgesia Excessive Pain
Allodynia Pain caused by any other sensation e.g. touch will cause
pain.
Muscular Pain Less blood flow in the muscles (ischemia).
Causalgia Burning pain
Stress induced analgesia Mild degree of pain is not felt if the other part of the body
has excessive pain.
Its a well known phenomenon seen when the soldier is
wounded in battle field but feels no pain until the battle is
over. The cause is not known may be it is similar to Gate
control hypothesis.
Phantom pain Pain felt in an amputated part long after amputation was
done.
Thalamic Syndrome Obstruction of the thalmogeniculate branch of the
posterior cerebral artery Affects posterior thalamic nuclei.
Prolonged severe pain.
Trigeminal neuralgia It is excruciating intermittent pain by stimulation of trigger
area in the face e.g. Washing of face, combing hair, blast of
air on face. It results from compression of trigeminal nerve
root by blood vessels
Chronic pain Chronic pain can be considered as bad pain because it
persist long after injury and is often refractory to pain
killers.
Chronic pain caused by nerve injury is called neuropathic
pain.
Neuropathic pain Caused by the damage to peripheral nerve.
The distal cut end develops a scar tissue forming rounded
ball (neuroma) which is sensitive to pressure.
Repeated activation causes continuous pain.
Examples post herpetic neuralgia and diabetic neuropathy.
Sites and mechanisms of pain relief:
Block production of inflammatory mediators.e.g. Aspirin & nonsteroidal
antiinflammatories.
Sympathectomy can be useful.
Exogenously administration of opoid like drugs.
Electrical stimulation of the dorsal column can alleviate pain originating below
site of stimulation.
Selective activation of large diameter afferent fibers by transcutaneous electrical
nerve stimulation.
Stimulation of brainstem sites or administration of drugs which can modify
serotoninergic or adrenergic neurons e.g. antidepressants.
Test your knowledge for both pain lectures 6+29:
1- Pain is:
a) Unconscious activity caused by a harmful stimulus
b) Any unpleasant sensation with/without tissue damage
c) Neural process of processing noxious stimuli
d) Any unpleasant sensation associated with tissue damage whether or
not individual is aware of
2- Natural mechanisms of pain relief are:
a) Gate control and electrical stimulation
b) Gate control
c) Gate control and pain analgesic system
d) No natural mechanism
3- Radiating pain is usually ____ in origin:
a) Visceral
b) Muscular
c) Facial
d) Neuropathic
4- 46 y/o female presenting with severe facial pain upon strange
stimuli such as applying her everyday make-up, what is the most
probable diagnosis and whats its explanation?
a) Thalamic syndrome; damage of thalamus
b) Trigeminal neuralgia; congenital defect in cranial nerve 5
c) Trigeminal neuralgia; compression of cranial nerve 5
d) Herpes zoster
5- All are true except:
a) Activity in thin fibres lead to impedance of inhibitory cells
b) Activity in large fibres lead to impedance of inhibitory cells
c) Thin fibres carry pain impulses
d) Activity in both fibres cause excitement in transmission cells
6- All are responsible for pain reduction except:
a) Post thalamic nuclei
b) Periaqueductal gray
c) Nucleus raphe magnus
d) Periventricular nucleus
7- All are true regarding encephalin except:
a) Prevents release of substance P
b) Pre and postsynaptic inhibition of pain transmission
c) Stimulated by noradrenergic neurons
d) Released from ventral horn
8- NSAIDs analgesic effect is conducted by:
a) Blocking nerve endings
b) Inhibit release of inflammatory mediators
c) A placebo effect only
d) Block transfer of signals at spinal level
9- Regarding referred pain:
a) Appendicitis pain is referred to umbilical area
b) Kidney stone pain is referred to suprapubic area
c) Fractured radius pain is referred to finger tips
d) Angina pain is referred to umbilical area
10- Neuralgia is:
a) Pain following nerve damage
b) Shrinkage of acute nerve endings
c) Cannot be treated surgically
d) Only seen in amputees
11- Phantom limb phenomenon is:
a) Only seen in amputees
b) May be encountered in post cancer breast surgery
c) Done due to inability of brain to reorganise the surgical event
d) Cannot be treated
Answers:
1) B
2) C
3) A
4) C
5) B
6) A
7) D
8) B
9) A
10) A
11) B
Вам также может понравиться
- Pain PhysiologyДокумент51 страницаPain Physiologyvladex77100% (1)
- Pain PathwayДокумент17 страницPain PathwaySalsabila Al-BasheerОценок пока нет
- Pain and Pain Gate Control MechanismДокумент17 страницPain and Pain Gate Control MechanismKapil LakhwaraОценок пока нет
- Nerve of The Lower Limb Edited LagiДокумент159 страницNerve of The Lower Limb Edited Lagifathizu100% (1)
- Local AnaesthesiaДокумент4 страницыLocal AnaesthesiaFaria Islam JuhiОценок пока нет
- 15 CerebrumДокумент32 страницы15 CerebrumMédecin Adrian TGОценок пока нет
- 3-Ascending Tracts of Spinal CordДокумент28 страниц3-Ascending Tracts of Spinal Cordmuhammad altaf100% (2)
- 4 NCV1Документ100 страниц4 NCV1sridharОценок пока нет
- Practical Skills On PalpationДокумент6 страницPractical Skills On PalpationsudersonОценок пока нет
- Cerebellar Function Tests: Experiment 29: Md-1C Group 5Документ42 страницыCerebellar Function Tests: Experiment 29: Md-1C Group 5Verlette Roselle Aguisanda LizardoОценок пока нет
- Brachial Plexus InjuryДокумент21 страницаBrachial Plexus InjurySemi IqbalОценок пока нет
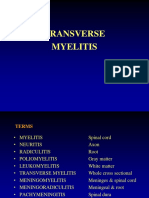
- Transverse MyelitisДокумент19 страницTransverse MyelitisAnonymous YHQmN8a01100% (1)
- Phantom Limbs and Plastic BrainДокумент19 страницPhantom Limbs and Plastic BrainZinneRah RahManОценок пока нет
- Clinical Guidelines For The Physiotherapy Management of Females Aged 16-65 With Stress Urinary IncontinenceДокумент72 страницыClinical Guidelines For The Physiotherapy Management of Females Aged 16-65 With Stress Urinary IncontinenceAndré RodriguesОценок пока нет
- Tuberculosis of Bones and JointsДокумент19 страницTuberculosis of Bones and JointsreinОценок пока нет
- Interactions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionОт EverandInteractions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionОценок пока нет
- Role of Physio in Neurological Disorders.Документ17 страницRole of Physio in Neurological Disorders.Maheen AnwaarОценок пока нет
- Upper Extremities Ortho SG3Документ119 страницUpper Extremities Ortho SG3Nuhu Bankwhot100% (1)
- Muscle Tone PhysiologyДокумент5 страницMuscle Tone PhysiologyfatimaОценок пока нет
- Peripheral Nerve InjuriesДокумент12 страницPeripheral Nerve InjuriesJiggs LimОценок пока нет
- Brachial Plexus PowerpointДокумент32 страницыBrachial Plexus PowerpointZulkarnain Syamsuri100% (1)
- 21-Spinal Cord TractsДокумент23 страницы21-Spinal Cord TractsALFAHRUL CAHYADIОценок пока нет
- Internal CapsuleДокумент25 страницInternal CapsuleMadan KumarОценок пока нет
- Spinal StabilizationДокумент32 страницыSpinal StabilizationLakshita PrajapatiОценок пока нет
- Spinal Cord LesionsДокумент110 страницSpinal Cord Lesionsgtaha80100% (1)
- Brain Areas - Location and FunctionДокумент12 страницBrain Areas - Location and FunctionMattGilmoreОценок пока нет
- Dysphagia ManagementДокумент21 страницаDysphagia ManagementSooraj A. O.100% (1)
- Gait Phases Kinetics Kinema TicsДокумент36 страницGait Phases Kinetics Kinema Ticsjonrocks100% (1)
- Anatomi PelvisДокумент44 страницыAnatomi Pelvisari naОценок пока нет
- RS2480 Amputation 2018Документ49 страницRS2480 Amputation 2018Hung Sarah100% (1)
- ASIA Impairment ScaleДокумент10 страницASIA Impairment Scaleazimahzainal211Оценок пока нет
- Mulligan Concept IFI Kudus, 29 Oktober 2017-1Документ84 страницыMulligan Concept IFI Kudus, 29 Oktober 2017-1Ilham Sii Pendekar Biru100% (1)
- Cerebellum: Principally Because Electrical Excitation of The CerebellumДокумент42 страницыCerebellum: Principally Because Electrical Excitation of The Cerebellumdr_mksinhaОценок пока нет
- Cranial NervesДокумент16 страницCranial Nervesapi-302547403100% (1)
- Nerve Pathways - Functions, Lesions and AdhesionsДокумент33 страницыNerve Pathways - Functions, Lesions and Adhesionshajra habibОценок пока нет
- Claw HandДокумент54 страницыClaw HandArum MaharaniОценок пока нет
- Complications of Bed RestДокумент51 страницаComplications of Bed Restsuderson100% (1)
- Dermatomes & Myotomes PDFДокумент4 страницыDermatomes & Myotomes PDFsridhar_physio0% (1)
- BPT 3rd Year-Pt in Ortho ConditionsДокумент5 страницBPT 3rd Year-Pt in Ortho Conditionsvenkata ramakrishnaiahОценок пока нет
- Muscles and Their VAN Supply and FunctionДокумент8 страницMuscles and Their VAN Supply and FunctionVinothini Siva100% (1)
- HeliotherapyДокумент20 страницHeliotherapyDodo JuniorОценок пока нет
- New Techniques in Physical TherapyДокумент61 страницаNew Techniques in Physical TherapyMohamed Magdy El MeligieОценок пока нет
- Sensory SystemДокумент13 страницSensory SystemFazira EkmaОценок пока нет
- Upper Limb Orthosis - Dr. Bhaskarananda KumarДокумент33 страницыUpper Limb Orthosis - Dr. Bhaskarananda KumarsudiptomukherjeeОценок пока нет
- Functional Areas of Cerebral CortexДокумент3 страницыFunctional Areas of Cerebral CortexMatet MonjeОценок пока нет
- Hip ExaminationДокумент84 страницыHip ExaminationDeepak KumarОценок пока нет
- Lung SurgeriesДокумент43 страницыLung SurgeriesSereinОценок пока нет
- Fractures of The Upper LimbДокумент3 страницыFractures of The Upper LimbJim Jose AntonyОценок пока нет
- Brain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFДокумент7 страницBrain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFBennat RajОценок пока нет
- Biomechanics of Peripheral and Spinal Nerve RootsДокумент86 страницBiomechanics of Peripheral and Spinal Nerve RootsJawad HassanОценок пока нет
- Physiotherapy Questions and AnswersДокумент4 страницыPhysiotherapy Questions and AnswersRonak PatelОценок пока нет
- Basics of Electrotherapy 2nd PDFДокумент175 страницBasics of Electrotherapy 2nd PDFPraneetha NouduriОценок пока нет
- Joint Mobilization What Is Joint Mobilization?Документ6 страницJoint Mobilization What Is Joint Mobilization?taravindnagarajОценок пока нет
- Splinting For Peripheral Nerve Injuries-PPT (2023)Документ49 страницSplinting For Peripheral Nerve Injuries-PPT (2023)KarisiОценок пока нет
- Anatomy Physiology of Hip JointДокумент6 страницAnatomy Physiology of Hip JointSundaraBharathiОценок пока нет
- Sherin Seminar 1 Combined Movements AssessmentДокумент47 страницSherin Seminar 1 Combined Movements AssessmentANKITA SHETTYОценок пока нет
- Examination of The Hip Joint - RP's Ortho NotesДокумент5 страницExamination of The Hip Joint - RP's Ortho NotesSabari NathОценок пока нет
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsРейтинг: 4 из 5 звезд4/5 (2)
- Validation of Lam Assessment of Employment Readiness (C-LASER) For Chinese Injured WorkersДокумент10 страницValidation of Lam Assessment of Employment Readiness (C-LASER) For Chinese Injured Workerssmartie_chaiОценок пока нет
- Assessing Readiness To Work From A Stages of Change Perspective: Implications For Return To WorkДокумент12 страницAssessing Readiness To Work From A Stages of Change Perspective: Implications For Return To Worksmartie_chaiОценок пока нет
- BLS ExamДокумент9 страницBLS ExamEdwin Delos Reyes Abu100% (3)
- Free First Breakthrough Cryptocurrency Mining Using Phone - "Pi Network App" (Next Bitcoin) (Golden Opportunity To Be Pioneer For Cryptocurrency To Become Rich, Multi-Millionaire and Financial Free)Документ2 страницыFree First Breakthrough Cryptocurrency Mining Using Phone - "Pi Network App" (Next Bitcoin) (Golden Opportunity To Be Pioneer For Cryptocurrency To Become Rich, Multi-Millionaire and Financial Free)smartie_chaiОценок пока нет
- Validation of Lam Assessment of Employment Readiness (C-LASER) For Chinese Injured WorkersДокумент10 страницValidation of Lam Assessment of Employment Readiness (C-LASER) For Chinese Injured Workerssmartie_chaiОценок пока нет
- Assessing Readiness To Work From A Stages of Change Perspective: Implications For Return To WorkДокумент12 страницAssessing Readiness To Work From A Stages of Change Perspective: Implications For Return To Worksmartie_chaiОценок пока нет
- Stoke Fall PrecautionДокумент31 страницаStoke Fall Precautionsmartie_chai100% (1)
- Hip SurveillanceДокумент1 страницаHip Surveillancesmartie_chai100% (1)
- SeizureДокумент11 страницSeizuresmartie_chai100% (1)
- 2010 Spasticity MechanismsДокумент10 страниц2010 Spasticity Mechanismsachsyaf arfanОценок пока нет
- Elaine Owen - Prosthetic International 254.fullДокумент17 страницElaine Owen - Prosthetic International 254.fullsmartie_chaiОценок пока нет
- Predictor of Post Stroke SpasticityДокумент8 страницPredictor of Post Stroke Spasticitysmartie_chaiОценок пока нет
- Elaine Owen - Prosthetic International 254.fullДокумент17 страницElaine Owen - Prosthetic International 254.fullsmartie_chaiОценок пока нет
- Aequanimitas Tribute To TJ DanarajДокумент181 страницаAequanimitas Tribute To TJ DanarajchuhuaОценок пока нет
- The 2015 BLS ACLS Guidelines ENA PDFДокумент36 страницThe 2015 BLS ACLS Guidelines ENA PDFsmartie_chaiОценок пока нет
- Barthel IndexДокумент2 страницыBarthel Indexgania100% (1)
- Anatomy of The LegДокумент57 страницAnatomy of The Legsmartie_chaiОценок пока нет
- Updated 10-16-14 Quick Reference Guide Digital Npuap Epuap Pppia 16oct2014Документ75 страницUpdated 10-16-14 Quick Reference Guide Digital Npuap Epuap Pppia 16oct2014Anonymous kZQet6QA100% (1)
- Range of Joint Motion Evaluation Chart OK PDFДокумент2 страницыRange of Joint Motion Evaluation Chart OK PDFcesamav100% (4)
- Rehab Goal Setting SMARTДокумент5 страницRehab Goal Setting SMARTsmartie_chaiОценок пока нет
- Good Muscle For Gait Cycle Podiatric - GAIT - ANAL PDFДокумент20 страницGood Muscle For Gait Cycle Podiatric - GAIT - ANAL PDFsmartie_chaiОценок пока нет
- Kinesio CKTT BrochureДокумент1 страницаKinesio CKTT Brochuresmartie_chaiОценок пока нет
- 2015 ACLS Guideline Update InfographicДокумент1 страница2015 ACLS Guideline Update Infographiccmalpicac1Оценок пока нет
- Special Tests LeДокумент9 страницSpecial Tests Lenurasyikah0% (1)
- CPG Management of Type 2 Diabetes Mellitus (5th Edition) Special AFES Congress EditionДокумент141 страницаCPG Management of Type 2 Diabetes Mellitus (5th Edition) Special AFES Congress Editionkhangsiean89100% (1)
- 4th Edition of Clinical Practice Guidelines Management of Dyslipidemia 2011Документ88 страниц4th Edition of Clinical Practice Guidelines Management of Dyslipidemia 2011Farah Aishah HamdanОценок пока нет
- Stroke in PregnancyДокумент24 страницыStroke in Pregnancysmartie_chaiОценок пока нет
- Key Sensory PointsДокумент6 страницKey Sensory PointsJose Maria Dominguez RoldanОценок пока нет
- Range of Joint Motion Evaluation Chart OK PDFДокумент2 страницыRange of Joint Motion Evaluation Chart OK PDFcesamav100% (4)
- Choose The Correct Answer by Crossing A, B, or C (Pilihlah Jawaban Yang Benar Dengan MemberДокумент3 страницыChoose The Correct Answer by Crossing A, B, or C (Pilihlah Jawaban Yang Benar Dengan MemberJufriОценок пока нет
- Addendum PDFДокумент2 страницыAddendum PDFIbaiMitxelenaSanchezОценок пока нет
- Education-and-Life-in-Europe - Life and Works of RizalДокумент3 страницыEducation-and-Life-in-Europe - Life and Works of Rizal202202345Оценок пока нет
- Research Papers Harvard Business SchoolДокумент8 страницResearch Papers Harvard Business Schoolyquyxsund100% (1)
- List of Holidays 2019Документ1 страницаList of Holidays 2019abhishek ranaОценок пока нет
- Iris Sofía Tobar Quilachamín - Classwork - 16-09-2022Документ4 страницыIris Sofía Tobar Quilachamín - Classwork - 16-09-2022IRIS SOFIA TOBAR QUILACHAMINОценок пока нет
- SANTHOSH RAJ DISSERTATION Presentation1Документ11 страницSANTHOSH RAJ DISSERTATION Presentation1santhosh rajОценок пока нет
- Forge Innovation Handbook Submission TemplateДокумент17 страницForge Innovation Handbook Submission Templateakil murugesanОценок пока нет
- May 11-Smart LeadersДокумент28 страницMay 11-Smart LeaderstinmaungtheinОценок пока нет
- Prosthetic Aspects of Dental Implants - IIДокумент73 страницыProsthetic Aspects of Dental Implants - IIKomal TalrejaОценок пока нет
- Gonzales v. Court of Appeals, G.R. No. L-37453, (May 25, 1979), 179 PHIL 149-177)Документ21 страницаGonzales v. Court of Appeals, G.R. No. L-37453, (May 25, 1979), 179 PHIL 149-177)yasuren2Оценок пока нет
- Unit 1 Revision PDFДокумент2 страницыUnit 1 Revision PDFИлья ЕвстюнинОценок пока нет
- PLM V6R2011x System RequirementsДокумент46 страницPLM V6R2011x System RequirementsAnthonio MJОценок пока нет
- Study of Indian Wrist Watch Industry and Repositioning Strategy of Titan WatchesДокумент60 страницStudy of Indian Wrist Watch Industry and Repositioning Strategy of Titan WatchesVinay SurendraОценок пока нет
- Infographic Group Output GROUP 2Документ2 страницыInfographic Group Output GROUP 2Arlene Culagbang GuitguitinОценок пока нет
- Cable GlandДокумент25 страницCable Glandfernando.magalhaesmowОценок пока нет
- Farm Gate TasmaniaДокумент20 страницFarm Gate TasmaniaplouffrОценок пока нет
- NLP - Neuro-Linguistic Programming Free Theory Training Guide, NLP Definitions and PrinciplesДокумент11 страницNLP - Neuro-Linguistic Programming Free Theory Training Guide, NLP Definitions and PrinciplesyacapinburgosОценок пока нет
- ALA - Application Guide 2023Документ3 страницыALA - Application Guide 2023Safidiniaina Lahatra RasamoelinaОценок пока нет
- SSD Term 3Документ52 страницыSSD Term 3anne_barltropОценок пока нет
- Painter Gary Woo - Oct 19 Talk by Yolanda Garfias WooДокумент2 страницыPainter Gary Woo - Oct 19 Talk by Yolanda Garfias WooChinese Historical Society of America MuseumОценок пока нет
- Bennett Et Al 2019 Towards A Sustainable and Equitable Blue EconomyДокумент3 страницыBennett Et Al 2019 Towards A Sustainable and Equitable Blue Economynaomi 23Оценок пока нет
- Kangar 1 31/12/21Документ4 страницыKangar 1 31/12/21TENGKU IRSALINA SYAHIRAH BINTI TENGKU MUHAIRI KTNОценок пока нет
- Eris User ManualДокумент8 страницEris User ManualcasaleiroОценок пока нет
- Fogarty HardwickДокумент35 страницFogarty HardwickBen KellerОценок пока нет
- Datasheet PIC1650Документ7 страницDatasheet PIC1650Vinicius BaconОценок пока нет
- GSRTCДокумент1 страницаGSRTCAditya PatelОценок пока нет
- A Day in The Life of A Scrum MasterДокумент4 страницыA Day in The Life of A Scrum MasterZahid MehmoodОценок пока нет
- The List of Official United States National SymbolsДокумент3 страницыThe List of Official United States National SymbolsВікторія АтаманюкОценок пока нет
- DharmakirtiДокумент7 страницDharmakirtialephfirmino1Оценок пока нет