Академический Документы
Профессиональный Документы
Культура Документы
Eating Disorders
Загружено:
Wendy Escalante0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров4 страницыEating Disorders
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документEating Disorders
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров4 страницыEating Disorders
Загружено:
Wendy EscalanteEating Disorders
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
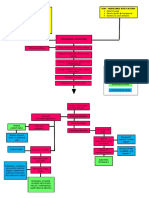
EATING DISORDERS
CATEGORIES OF EATING DISORDERS AND RELATED DISORDERS
Anorexia nervosa Life-threatening eating disorder characterized by the clients refusal or inability to
maintain a minimally normal body weight, intense fear of gaining weight or becoming
fat, significantly disturbed perception of the shape or size of the body, and steadfast
inability or refusal to acknowledge the seriousness of the problem or even that one
exists. They have a body weight that is 85% or less of that expected for their age and
height, have experienced amenorrhea for at least three consecutive cycles, and have a
preoccupation with food and food-related activities.
binge eating and purging Clients with anorexia nervosa can be classified into two subgroups depending on how
they control their weight. Clients with the restricting subtype lose weight primarily
through dieting, fasting, or excessive exercising. Those with the _ and _ subtype
engage regularly in binge eating followed by purging.
*Binge eating Consuming a large amount of food (far greater than most people eat at one time) in a
discrete period of usually 2 hours or less.
*Purging Involves compensatory behaviors designed to eliminate food by means of self-induced
vomiting or misuse of laxatives, enemas, and diuretics. Some clients with anorexia do
not binge but still engage in purging behaviors after ingesting small amounts of food.
anorexia The term_ is actually a misnomer: These clients do not lose their appetites. They still
experience hunger but ignore it and signs of physical weakness and fatigue; they often
believe that if they eat anything, they will not be able to stop eating and will become
fat. Clients with anorexia often are preoccupied with food-related activities such as
grocery shopping, collecting recipes or cookbooks, counting calories, creating fat-free
meals, and cooking family meals. They also may engage in unusual or ritualistic food
behaviors such as refusing to eat around others, cutting food into minute pieces, or not
allowing the food they eat to touch their lips. These behaviors increase their sense of
control
Bulimia nervosa Often simply called bulimia, is an eating disorder characterized by recurrent episodes
(at least twice a week for 3 months) of binge eating followed by inappropriate
compensatory behaviors to avoid weight gain, such as purging, fasting, or excessively
exercising.
Bulimia nervosa Between binges, the client may eat low-calorie foods or fast. Binging or purging
episodes are often precipitated by strong emotions and followed by guilt, remorse,
shame, or self-contempt. Recurrent vomiting destroys tooth enamel, and incidence of
dental caries and ragged or chipped teeth increases in these clients. Dentists are often
the first health care professionals to identify clients with bulimia
rumination disorder, pica, and feeding Related eating disorders usually first diagnosed in infancy and childhood include _
disorder
Binge eating disorder The essential features are recurrent episodes of binge eating; no regular use of
inappropriate compensatory behaviors, such as purging or excessive exercise or abuse
of laxatives; guilt, shame, and disgust about eating behaviors; and marked psychologic
distress. Binge eating disorder frequently affects people over age 35, and it occurs
often in men (Yager, 2008). Individuals are more likely to be overweight or obese,
overweight as children, and teased about their weight at an early age.
Night eating syndrome is characterized by morning anorexia, evening hyperphagia (consuming 50% of daily
calories after the last evening meal), and nighttime awakenings (at least once a night)
to consume snacks. It is associated with life stress, low self-esteem, anxiety,
depression, and adverse reactions to weight loss. Most people with night eating
syndrome are obese. Treatment with SSRI antidepressants has shown positive
effects.
Anorexia and bulimia are both characterized by perfectionism, obsessivecompulsiveness, neuroticism,
negative emotionality, harm avoidance, low self-directedness, low cooperativeness,
and traits associated with avoidant personality disorder. In addition, clients with
bulimia may also exhibit high impulsivity, sensation seeking, novelty seeking, and
traits associated with borderline personality disorder
Such a history may be a factor contributing to problems with intimacy, sexual attractiveness, and low interest in sexual activity. Clients
with eating disorders and a history of sexual abuse also have higher levels of depression and anxiety, lower self-esteem, more
interpersonal problems, and more severe obsessivecompulsive symptoms
ETIOLOGY
-Biologic vulnerability, developmental problems, and family and social influences can turn dieting into an eating disorder
Biologic Factors
-Genetic vulnerability also might result from a particular personality type or a general susceptibility to psychiatric disorders. Or it may
directly involve a dysfunction of the hypothalamus.
-Disruptions of the nuclei of the hypothalamus may produce many of the symptoms of eating disorders. Two sets of nuclei are
particularly important in many aspects of hunger and satiety (satisfaction of appetite): the lateral hypothalamus and the ventromedial
hypothalamus. Deficits in the lateral hypothalamus result in decreased eating and decreased responses to sensory stimuli that are
important to eating. Disruption of the ventromedial hypothalamus leads to excessive eating, weight gain, and decreased responsiveness
to the satiety effects of glucose, which are behaviors seen in bulimia.
-Norepinephrine levels do not rise during starvation, however, because few nutrients are available to metabolize. Therefore, low
norepinephrine levels are seen in clients during periods of restricted food intake. Also, low epinephrine levels are related to the
decreased heart rate and blood pressure seen in clients with anorexia
-Increased levels of the neurotransmitter serotonin and its precursor tryptophan have been linked with increased satiety. Low levels of
serotonin as well as low platelet levels of monoamine oxidase have been found in clients with bulimia and the binge and purge subtype
of anorexia nervosa
DEVELOPMENTAL FACTORS:
-Two essential tasks of adolescence are the struggle to develop autonomy and the establishment of a unique identity. Autonomy,
or exerting control over oneself and the environment, may be difficult in families that are overprotective or in which enmeshment
(lack of clear role boundaries) exists. Such families do not support members efforts to gain independence, and teenagers may feel as
though they have little or no control over their lives. They begin to control their eating through severe dieting and thus gain control
over their weight. Losing weight becomes reinforcing: by continuing to lose, these clients exert control over one aspect of their lives.
Body image disturbance Occurs when there is an extreme discrepancy between ones body image and the
perceptions of others and extreme dissatisfaction with ones body image
PLEASE READ FAMILY INFLUENCES AND SOCIOCULTURAL FACTORS :) PAGE 376-377 AT PSYCHIA BOOK
THANK YOU :)
ANOREXIA NERVOSA
Onset and Clinical Course
-Anorexia nervosa typically begins between 14 and 18 years of age. In the early stages, clients often deny they have a negative body
image or anxiety regarding their appearance. They are very pleased with their ability to control their weight and may express this.
-As the illness progresses, depression and lability in mood become more apparent. As dieting and compulsive behaviors increase,
clients isolate themselves. This social isolation can lead to a basic mistrust of others and even paranoia. Clients may believe their peers
are jealous of their weight loss and may believe that family and health care professionals are trying to make them fat and ugly.
Psychopharmacology Amitriptyline (Elavil) and the antihistamine cyproheptadine (Periactin) in high
doses (up to 28 mg/day) can promote weight gain in inpatients with anorexia
nervosa. Olanzapine (Zyprexa) has been used with success because of its
antipsychotic effect (on bizarre body image distortions) and associated weight
gain. Fluoxetine (Prozac) has some effectiveness in preventing relapse in clients
whose weight has been partially or completely restored; however, close monitoring
is needed because weight loss can be a side effect.
DSM-IV-TR DIAGNOSTIC CRITERIA:
Symptoms of Anorexia Nervosa
*Fear of gaining weight or becoming fat even when severely underweight
*Body image disturbance
*Amenorrhea
*Depressive symptoms such as depressed mood, social withdrawal, irritability, and insomnia *Preoccupation with thoughts of food
*Feelings of ineffectiveness
*Inflexible thinking
*Strong need to control environment
*Limited spontaneity and overly restrained emotional expression
*Complaints of constipation and abdominal pain
BULIMIA
Onset and Clinical Course
-Bulimia nervosa usually begins in late adolescence or early adulthood; 18 or 19 years is the typical age of onset. Binge eating
frequently begins during or after dieting. Between binging and purging episodes, clients may eat restrictively, choosing salads and
other low-calorie foods. This restrictive eating effectively sets them up for the next episode of binging and purging, and the cycle
continues.
-Clients with bulimia are aware that their eating behavior is pathologic and go to great lengths to hide it from others. They may store
food in their cars, desks, or secret locations around the house. They may drive from one fastfood restaurant to another, ordering a
normal amount of food at each but stopping at six places in 1 or 2 hours
DSM-IV-TR DIAGNOSTIC CRITERIA:
Symptoms of Bulimia Nervosa
*Recurrent episodes of binge eating
*Compensatory behavior such as self-induced vomiting, misuse of laxatives, diuretics, enema or other medications, or excessive
exercise
*Self-evaluation overly influenced by body shape and weight
*Usually within normal weight range, possibly underweight or overweight
*Restriction of total calorie consumption between binges, selecting low-calorie foods while avoiding foods perceived to be fattening or
likely to trigger a binge
*Depressive and anxiety symptoms
*Possible substance use involving alcohol or stimulants
*Loss of dental enamel
*Chipped, ragged, or moth-eaten appearance of teeth
*Increased dental caries
*Menstrual irregularities
*Dependence on laxatives
Treatment and Prognosis
* CognitiveBehavioral Therapy Has been found to be the most effective treatment for bulimia. This outpatient
approach often requires a detailed manual to guide treatment. Strategies designed to
change the clients thinking (cognition) and actions (behavior) about food focus on
interrupting the cycle of dieting, binging, and purging and altering dysfunctional
thoughts and beliefs about food, weight, body image, and overall selfconcept
Psychopharmacology
Since the 1980s, several controlled studies have been conducted to evaluate the effectiveness of antidepressants to treat bulimia.
Drugs, such as desipramine (Norpramin), imipramine (Tofranil), amitriptyline (Elavil), nortriptyline (Pamelor), phenelzine
(Nardil), and fluoxetine (Prozac) were prescribed in the same dosages used to treat depression
ASSESSMENT
History
Family members often describe clients with anorexia nervosa as perfectionists with above-average intelligence, achievement oriented,
dependable, eager to please, and seeking approval before their condition began. Parents describe clients as being good, causing us no
trouble until the onset of anorexia. Likewise, clients with bulimia often are focused on pleasing others and avoiding conflict.
General Appearance and Motor Behavior
Clients with anorexia appear slow, lethargic, and fatigued; they may be emaciated, depending on the amount of weight loss. They may
be slow to respond to questions and have difficulty deciding what to say. They are often reluctant to answer questions fully because
they do not want to acknowledge any problem. They often wear loose-fitting clothes in layers, regardless of the weather, both to hide
weight loss and to keep warm (clients with anorexia are generally cold)
Mood and Affect
Clients with eating disorders have labile moods that usually correspond to their eating or dieting behaviors. Avoiding bad or
fattening foods gives them a sense of power and control over their bodies, whereas eating, binging, or purging leads to anxiety,
depression, and feeling out of control. Clients with eating disorders often seem sad, anxious, and worried.
Thought Processes and Content
Clients with eating disorders spend most of the time thinking about dieting, food, and food-related behavior. They are preoccupied
with their attempts to avoid eating or eating bad or wrong foods. Clients cannot think about themselves without thinking about
weight and food. The body image disturbance can be almost delusional; even if clients are severely underweight, they can point to
areas on their buttocks or thighs that are still fat, thereby fueling their need to continue dieting
Sensorium and Intellectual Processes
Generally, clients with eating disorders are alert and oriented; their intellectual functions are intact. The exception is clients with
anorexia who are severely malnourished and showing signs of starvation, such as mild confusion, slowed mental processes, and
difficulty with concentration and attention.
Judgment and Insight
Clients with anorexia have very limited insight and poor judgment about their health status. They do not believe they have a problem;
rather, they believe others are trying to interfere with their ability to lose weight and to achieve the desired body image. Facts about
failing health status are not enough to convince these clients of their true problems. Clients with anorexia continue to restrict food
intake or to engage in purging despite the negative effect on health
Self-Concept
Low self-esteem is prominent in clients with eating disorders. They see themselves only in terms of their ability to control their food
intake and weight. They tend to judge themselves harshly and see themselves as bad if they eat certain foods or fail to lose weight.
Roles and Relationships
Eating disorders interfere with the ability to fulfill roles and to have satisfying relationships. Clients with anorexia may begin to fail at
school, which is in sharp contrast to previously successful academic performance. They withdraw from peers and pay little attention to
friendships. They believe that others will not understand or fear they will begin out-of-control eating with others.
Physiologic and Self-Care Considerations
The health status of clients with eating disorders relates directly to the severity of self-starvation, purging behaviors, or both (see Table
18.2). In addition, clients may exercise excessively, almost to the point of exhaustion, in an effort to control weight. Many clients have
sleep disturbances such as insomnia, reduced sleep time, and earlymorning wakening.
Data Analysis
Nursing diagnoses for clients with eating disorders include the following:
Imbalanced Nutrition: Less Than/More Than Body Requirements
Ineffective Coping
Disturbed Body Image
Chronic Low Self-esteem
Interventions
*Establishing Nutritional Eating Patterns
*Identifying Emotions and Developing Coping Strategies
-Because clients with anorexia have problems with selfawareness, they often have difficulty identifying and expressing feelings
(alexithymia). Therefore, they often express these feelings in terms of somatic complaints such as feeling fat or bloated
*Dealing with Body Image Issues
*Providing Client and Family Education
Self-monitoring Cognitivebehavioral technique designed to help clients with bulimia. It may help
clients to identify behavior patterns and then implement techniques to avoid or to
replace them (Schmidt, 2008). Self-monitoring techniques raise client awareness about
behavior and help them to regain a sense of control. The nurse encourages clients to
keep a diary of all food eaten throughout the day, including binges, and to record
moods, emotions, thoughts, circumstances, and interactions surrounding eating and
binging or purging episodes
CLIENT/FAMILY EDUCATION for Eating Disorders
Client
Basic nutritional needs
Harmful effects of restrictive eating, dieting, and purging
Realistic goals for eating
Acceptance of healthy body image
Family and Friends
Provide emotional support.
Express concern about clients health.
Encourage client to seek professional help.
Avoid talking only about weight, food intake, and calories.
Become informed about eating disorders.
It is not possible for family and friends to force the client to eat. The client needs professional help from a therapist or psychiatrist.
END. GOD BLESS! STUDY WELL! PHIL 4:13 :)
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Degenerative Joint DiseaseДокумент35 страницDegenerative Joint DiseaseWendy EscalanteОценок пока нет
- Fundamentals in NursingДокумент9 страницFundamentals in NursingWendy EscalanteОценок пока нет
- DM No. 2022-0287 Updated Moa and Tor PRDPДокумент8 страницDM No. 2022-0287 Updated Moa and Tor PRDPDRMC Infirmary100% (1)
- Assessment of Kidneys PDFДокумент1 страницаAssessment of Kidneys PDFWendy EscalanteОценок пока нет
- Drug StudyДокумент14 страницDrug StudyWendy EscalanteОценок пока нет
- PATHOДокумент2 страницыPATHOWendy EscalanteОценок пока нет
- NCPДокумент3 страницыNCPWendy EscalanteОценок пока нет
- NCP 2 MiДокумент16 страницNCP 2 MiWendy EscalanteОценок пока нет
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendДокумент2 страницыModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- Nasogastric Tube Management and CareДокумент21 страницаNasogastric Tube Management and CareWendy EscalanteОценок пока нет
- Acid-Ash DietДокумент10 страницAcid-Ash DietWendy Escalante0% (1)
- Concept Map of Carotid Artery DiseaseДокумент2 страницыConcept Map of Carotid Artery DiseaseWendy EscalanteОценок пока нет
- 02 Orig Art 02 PDFДокумент3 страницы02 Orig Art 02 PDFWendy EscalanteОценок пока нет
- Case Presentation: Group 2Документ30 страницCase Presentation: Group 2Wendy EscalanteОценок пока нет
- Caring For The Bedridden PatientДокумент1 страницаCaring For The Bedridden PatientWendy EscalanteОценок пока нет
- Assessment of KidneysДокумент1 страницаAssessment of KidneysWendy EscalanteОценок пока нет
- Concept Map of CKD Gastrointestinal SymptomsДокумент4 страницыConcept Map of CKD Gastrointestinal SymptomsWendy Escalante0% (1)
- At DietДокумент8 страницAt DietWendy EscalanteОценок пока нет
- Brat DietДокумент8 страницBrat DietWendy EscalanteОценок пока нет
- Pediatric NursingДокумент16 страницPediatric NursingWendy Escalante100% (1)
- DM Report1Документ16 страницDM Report1Wendy EscalanteОценок пока нет
- Therapeutic DietДокумент3 страницыTherapeutic DietWendy EscalanteОценок пока нет
- Drug Study FinalДокумент8 страницDrug Study FinalWendy EscalanteОценок пока нет
- FNCP CommunityДокумент4 страницыFNCP CommunityWendy EscalanteОценок пока нет
- Nursing Care For Patient With Neurological DiseaseДокумент8 страницNursing Care For Patient With Neurological DiseaseWendy EscalanteОценок пока нет
- Integrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsДокумент78 страницIntegrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsWendy EscalanteОценок пока нет
- Diabetes MellitusДокумент5 страницDiabetes MellitusWendy EscalanteОценок пока нет
- Antibacterial Activity of Medicinal Plants Against ESKAPE An Up - 2021 - HeliyoДокумент12 страницAntibacterial Activity of Medicinal Plants Against ESKAPE An Up - 2021 - HeliyoTONY VILCHEZ YARIHUAMANОценок пока нет
- Functional Motor AssessmentДокумент5 страницFunctional Motor AssessmentLoren EstefanОценок пока нет
- Professional Development Plan PPT 1Документ10 страницProfessional Development Plan PPT 1api-355484042Оценок пока нет
- Standard Operating Procedures For Environment & Physical HazardДокумент6 страницStandard Operating Procedures For Environment & Physical HazardDr Aynul HoqueОценок пока нет
- Reviewer Micp Midterms 1Документ29 страницReviewer Micp Midterms 1Shiro KagomeОценок пока нет
- Sal Mvlex WebДокумент35 страницSal Mvlex WebCarlos EcosОценок пока нет
- Factors Affecting Sleep: The Quality and Quantity of Sleep AreДокумент3 страницыFactors Affecting Sleep: The Quality and Quantity of Sleep AreBijali sinha100% (3)
- MSF - H Mental Health Guidelines, 9 August 2005Документ140 страницMSF - H Mental Health Guidelines, 9 August 2005Diego Mercado100% (1)
- Niche and Sub-NicheДокумент3 страницыNiche and Sub-NichehoneybeeОценок пока нет
- Mcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyДокумент27 страницMcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyAnonymous kQCQ30Rq5OОценок пока нет
- Republic Act No. 4688Документ1 страницаRepublic Act No. 4688Im MiОценок пока нет
- Food Power For AthletesДокумент3 страницыFood Power For AthletesVegan Future100% (1)
- IbmsbrochureДокумент36 страницIbmsbrochureadipoliachayan52350% (1)
- Physical Restraint Reduction For Older AdultsДокумент11 страницPhysical Restraint Reduction For Older Adultsantariksa tedyОценок пока нет
- ZXXZДокумент6 страницZXXZfei cuaОценок пока нет
- Self Assessment Toolkit-NABH Hosp Standard-2nd EdiДокумент44 страницыSelf Assessment Toolkit-NABH Hosp Standard-2nd Edimadhuri24Оценок пока нет
- ME1410 Wk4 Worksheet 2017 V01Документ1 страницаME1410 Wk4 Worksheet 2017 V01shanesiaОценок пока нет
- Expository Essay by PauДокумент2 страницыExpository Essay by PauStary Larry BumfuzzleОценок пока нет
- Colorectal Management of Postoperative Complications (Complicaciones Gen)Документ13 страницColorectal Management of Postoperative Complications (Complicaciones Gen)Carlos NoronaОценок пока нет
- Vital Signs: Nursing Assessment Techniques ModuleДокумент24 страницыVital Signs: Nursing Assessment Techniques ModuleSHELLAH MARIE MAMAWAGОценок пока нет
- 7724 (11) The Hospital and Pertinent Laws and RegulationsДокумент24 страницы7724 (11) The Hospital and Pertinent Laws and RegulationsnewazОценок пока нет
- Covid-19 Among Neonates: Experience From An Sncu of A Tertiary Care Hospital in Eastern IndiaДокумент4 страницыCovid-19 Among Neonates: Experience From An Sncu of A Tertiary Care Hospital in Eastern IndiaIJAR JOURNALОценок пока нет
- Consolidated Guidelines OnДокумент594 страницыConsolidated Guidelines OnRICHARD EDUARDO FERNANDEZ SAENZОценок пока нет
- Myocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrДокумент23 страницыMyocardial Infarction: Disscused With Head Supervisor: DR - Yassmeen Ahmed of Pathology Department:prof - Dr.Manal El-NemrOmar ShazlyОценок пока нет
- Disaster Nursing Lecture 1Документ11 страницDisaster Nursing Lecture 1Beahtriz GuintoОценок пока нет
- Carmen Best Background InformationДокумент15 страницCarmen Best Background InformationKING 5 NewsОценок пока нет
- Caregiving: A Common or Uncommon ExperienceДокумент13 страницCaregiving: A Common or Uncommon ExperienceANGELОценок пока нет
- The Roots and Branches of Neuromuscular Therapy - NMT CenterДокумент7 страницThe Roots and Branches of Neuromuscular Therapy - NMT CentersalmazzОценок пока нет
- PE 2112 Week 1-19 OedДокумент5 страницPE 2112 Week 1-19 OedEury Marc Suhi-anОценок пока нет