Академический Документы
Профессиональный Документы
Культура Документы
Notes Jun 6, 2014 Obstetrics and Gynecology Part 8
Загружено:
Diwakesh C BАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Notes Jun 6, 2014 Obstetrics and Gynecology Part 8
Загружено:
Diwakesh C BАвторское право:
Доступные форматы
Cancer cervix
Bimodal distribution
1st peak in 3-4 decade, more common here
2nd peak in 6-7 decade
Most common Ca in Indian women
Most common histology
Squamous cell Ca, 70%
Adenocarcinoma, 30%
Risk factors:
Early age at first intercourse
Early age at first child birth
Multiparity
Multiple sexual partners
Low socio economic status
Presence of STD's
Presence of pr invasive lesions
Controversial risk factors
OCP's increase the risk but only after 5 years of use
They are more related to adenocarcinoma
Cigarette smoking: only for squamous cell Ca
No relation to early menarche and late menopause
Family history has no relation
Causative agent
HPV
DNA virus
High risk: 16,18,31,33,35,45,52,58
Low risk: 6,11
Type 16,18 account for 70%
More sensitive is 16, squamous Ca and 18 is more specific,
adenocarcinoma
What type of cells are infected by HPV
Basal epithelial cells aka basal stem cells
What viral proteins are responsible for malignant transformation
E6,7
For DNS replication: E1,2
Characteristic Histopathological finding
Koilocytosis, perinuclear halo due to cytoplasmic clearing
6,11 cause condylomata accuminata
Juvenile papillomatosis in the baby
HPV vaccines
Inactivated capsid proteins
Are mandatory/ should be given to HIV positive women
Annual screening in HIV positive women
CI in pregnancy
HPV vaccine protects only against 16,18 as others may be present
so the screening should continue after vaccination
Ideal age is 11-12 years of age
But can be given anytime between 9-26 years
Penile, anal, oral other than cervical, vaginal and vulval cancers
Thus given to boys as well
Gardasil: 16,18,6,11
Can be given to boys also
0,2 and 6 months
Cervirix
More ecacious than gardasil
16,18
0,1 and 6 months
No booster required for both
Both given IM
Protection rate is 70% as 16,18 cause 70% Ca
Most common side eect is the pain at the site of injection
Other is Syncopal attack, thus should be accompanied and
observation time of 15 min
One liners
Most common or the first presenting complaint: irregular vaginal
bleeding
Most specific complaint: post coital bleeding
Most common route of spread: lymphatic spread
Q. Pt with h/o post coital bleeding, next step is PAPS
Q. H/o post coital bleeding, 3x4 cm mass on anterior lip of cervix:
do a punch biopsy
Most common cause of death: uremia secondary to renal failure
Most common LN is obturator LN
Sentinel lymph nodes are para cervical
Risk of involvement of ovaries in Ca cervix: <1%
Thus ovaries are spared during Sx
Staging of cervical Ca
This is a clinical staging
Done by the gynecologist
Certain investigations can not be used to change the staging:
USG, CT, MRI, PET
The only thing for which CT is approved is to look for hydroureter
All kind of scopies are allowed
Cystoscopy, hysteroscopy, colposcopy etc
Stage 1
A: microscopic
B: macroscopic
A1: <3 mm in depth and <7 in horizontal spread
A2:<3-5 and <7
B1:<4
B2:>4
??
Stage 2
Upper 2/3 of vagina involved
A: without parametrium
B: with parametrium
A1:<4
A2>4
Parametrium is connective tissue surrounding the cervix
Stage 3
Lower 1/3 vagina involved
A: not reaching the lateral pelvic wall
B: reaching the lateral pelvic wall with or without lower 1/3 vagina
involvement
Clues indicating lateral pelvic wall reached
Presence of hydroureter or hydronephrosis
Lower limb edema
Pain radiating down the leg
Stage 4
A: involvement of bladder and rectum
B: distant metastasis
Bullous edema of bladder mucosa indicates lymphatics are
involved, it does not change the stage
Inguinal LN are considered distant metastasis for cervical Ca
Treatment
Upto stage 2A, primary modality of treatment is surgery
>=2B, primary modality is chemo radiation
Stage 1A1: 3 options
Hysterectomy
Therapeutic Conization
Radical trachelectomy
If family is complete, hysterectomy done ka type 1 hysterectomy
aka Simple extra fascial hysterectomy
If child bearing is desired aka fertility preserving surgeries
Conization
Radical trachelectomy
Look for lymphvascular space invasion LVSI
If absent, conization
If present, radical trachelectomy
Radical trachelectomy
Fertility preserving surgery
Can be done in stage 1A1, 1A2, 1B1 if size less than 2 cm
Structures removed: cervix, parametrium, pelvic LN, small part of
vagina
Cerclage between uterus and vagina
Delivery done by CS
Stage 1A2
Werthiem's hysterectomy aka type 2 hysterectomy aka modified
radical hysterectomy
Along with this pelvic lymph adenectomy also done
Stage 1B1, 1B2, 2A
Surgery done is Meig's hysterectomy aka type 3 hysterectomy aka
radical hysterectomy
Pelvic lymph adenectomy also done
And
Para aortic LN sampling
Inoperable stages
>= 2B
Primary modality is chemo radiation
Both chemo and RT are given together
Chemotherapy:
Cisplatin aka radiation sensitizer
Can be also used
5 FU
Radiotherapy
Initially divided into
External beam RT or brachytherapy which means intracavitary RT
If both have to be given
EBRT followed by brachytherapy
EBRT can be either given to only pelvis
Or pelvis and abdomen: extended field RT
Indication is positive para aortic LN
Pelvis EBRT
25 fractions over 5 weeks
Each fraction has a dose of 1.8-2 gy
Thus total dose is 40-50 gy
Abdomen EBRT
25 fractions over 5 weeks
Dose is 1-1.2 gy per fraction
Thus total is 25-30 gy
Radio isotope used is Caesium Cs
Brachytherapy
Given two 2 points A and B
Location of point A
Two cm lateral tottering canal, corresponds to para cervical LN and
to ureter
Radiation dose at A is 8000 centigy
Point B
3 cm lateral to point A and 3 cm above external Os
Thus 5 cm from uterine canal
Corresponds to obturator LN
Dose is 6000 centigy
American brachytherapy society criteria
Point A divided into early and advanced stage
Early: 80-85 gy
Advanced:85-90 gy
Point B or lateral pelvic wall
Early:50-55 gy
Advanced:55-60 gy
Radio isotopes for brachytherapy
Low dose therapy: Caesium
High dose therapy: Iridium
Boundaries of pelvis
Upper border: disc space between L4-5 vertebra
Lateral border: 2 cm lateral to bony canal
Inferior border: lower margin of obturator foramen
When Abdomen radiated
Only the upper border changes
Disc space between T12-L1
Pelvic lymphadenectomy
Internal iliac
External iliac
Obturator
Pre sacral
Common iliac
Indications for post operative RT( Adjuvant)
Indications
Positive LN
Involvement of parametria
Positive margins
Recurrent cervical Cancer
Treatment depends on the primary modality
If first Sx was done, give RT
If primary modality was radiation, surgery can be done
Total pelvic exenteration
Dierence between type 2 and type 3 hysterectomy
Type 2
Medial half of parametrium is removed
Uterosacral and Mackenrodt ligaments are cut midway
Uterine artery is ligated after it gives the uretric branch
<1 cm of vagina is removed
Type 3
All the parametrium is removed
Uterosacral and Mackerodt are cut at their insertion
Uterine artery is ligated at its origin from the internal iliac
More than 2 cm vagina is removed
TAH
Total abdominal hysterectomy
Uterus and cervix are removed
If only uterus is removed: subtotal hysterectomy
TAH+ BSO: pan hysterectomy
Ovarian Cancer
No universal screening
Uncommon
No specific sign and symptoms
Adenexal mass
If benign or malignant
Benign
Seen in reproductive age group
Usually unilateral
History of pain
Cystic consistency on examination
Malignant
Seen in extremes of age
Bilateral
Usually no pain
Variable consistency
USG
High risk features suggestive of malignancy
Solid component
Thick septae (2-3 mm)
Presence of papillary projections
Ascites
Enlarged LN and matted bowel loops
Doppler
Increased vascularity is high risk
Resistive index
Pulsatility index
Both are low and suggest high vascularity
Indications for Sx Mx of masses
Any high risk feature on USG
Raised CA-125 in a post menopausal woman
Normal value is <35 IU
Ovarian mass >7 cm suggestive of malignancy
Adenexal mass >10 cm
Any mass that presents with acute abdomen: torsion and rupture
When the diagnosis is not confirmed
Pregnancy: except for CA-125 as physiologically rises
Rapid enlarging mass also requires Sx intervention
Ovarian mass in reproductive age women
Management depends on size of mass
3-5 cm: wait and watch
5-7 cm: serial USG at 6 weeks interval
CA-125 is not done as first line investigation in reproductive age
group because there are many benign and malignant conditions
when it is raised
Benign:
Menses
Pregnancy
PID
Endometriosis
Genital TB
Fibroid uterus
Any abdominal itis
Malignant conditions
Breast Ca
Colon Ca
Lung Ca
Pancreatic Ca
Ovarian Ca
Endometrial Ca
Important investigation in post menopausal women
OCP's are not routinely to be given for ovarian masses
As they do not aect the current mass but prevent future masses
Ovarian Cancer
Risk factors
Two pathophysiologies
More the number of ovulatory cycles, more the risk
Increased estrogen content
1. Early menarche
2. Late menopause
3. Nulliparous
4. Obesity
5. Polycystic ovarian syndrome
6. HRT
7. BRCA 1-2 and HNPCC
8. Smoking: risk factor for Mucinous cancers
Protective factors
Multi parity
Breast feeding
Use of OCP's
Salpingectomy, tubal ligation and hysterectomy: prevent ascending
mitogens
Most common type are
Epithelial ovarian Ca
90-95% of all ovarian Ca
Most commonly BL
Serous cystadenocarcinoma, 70%
Mucinous, 10%
Endometroid, 10%
Clear cell
Brenners
Mostly present in post menopausal age group, 6-7th decade
Vague abdominal symptoms
N/V, altered bowel habits, gastritis, Ascites, anorexia
Present in late stages
Highest mortality rate amongst gynecological malignancies
Most are sporadic
Mucinous have some characteristics
Remain confined to ovaries for a long time
Can attain large sizes upto 20 cms
CA-125 levels is not much raised
Asso with pseudomyxoma peritoneii
What % of epithelial Ca are familial: only 10%
Seen in women carrying mutations in BRCA 1-2 and HNPCC
With BRCA 1:35-45%
BRCA 2:25%
HNPCC:15%
Familial occur a decade earlier
Peak in 4-5th decade
Risk increases after 35 years of age every year
Thus screening done in ???
Screening done annually
CA-125 and TVS
Started at 35 years of age
Prophylactic BL BSO done ideally at 35 years of age of as soon as
family is complete
Second line agents for prevention if Sx declined
OCP's
But breast Ca and Peritoneal Carcinomatosis can still occur after
BSO
By what % is breast Ca reduced by prophylactic BSO:50%
Borderline epithelial
Also show epithelial hyperplasia, mitotic figures, abnormal shapes
and size
But do not show stromal invasion
Also occur a decade earlier
They metastatize late
Remain confined to ovary for a long time, thus late spread
Prognosis is better
It's a Histopathological diagnosis
Managed by Conservative Sx
Germ cell tumors of the ovary
Account for 5% of ovarian tumors
Dysgerminoma
Mature teratoma
Immature teratoma
Embryonal cell Ca
Endodermal sinus tumor/ yolk cell tumor
Choriocarcinoma
Mixed
Tend to be unilateral
Peak is between 10-30, usually 10-20 years of age
Vague abdominal complaints
Acute abdomen
Precocious puberty
Thus diagnosed early
Tumor markers
Alpha feto protein
HCG
They metastasize late
Managed by conservative Sx
Sex cord tumors
Least common
Granulosa cell tumors
Theca cell tumors
Fibroma- thecoma group
Sertoli leydig tumors
Sertoli tumors
Can be seen at any age but most common is peri menopausal
Vague abdominal complaints
Along with
Abnormal uterine bleeding, if producing estrogen
Virilization, if producing testosterone
No asso to the BRCA genes
Metastasis is rare
Risk of second malignancy: endometrial cancers
One liners
Specific cell types:
1. Signet ring cells: Krukenberg's tumor
It is a metastasis to ovary
Most common primary is stomach Ca
Always BL
Shape of ovary is always maintained
2. Psamomma bodies: serous Ca
3. Call Exner: granulosa cell
4. Wallthard cell: brenners
5. Reinke's crystal: leydig/ Hilus
6. Schiller Duvall: EST
7. Rokitansky protuberance: dermoid
Tumor markers
Serous cystadenoma : cA125
HE4 , human Epididymal protein 4
LDH : dysgerminoma,
It also secretes HCG, placental alkaline phosphatase
Embryonal cell Ca: HCG, AFP
Endodermal sinus: AFP, LDH
ChorioCa: HCG
Mucinous adenocarcinoma : CEA
Granulosa cell tumor: inhibin
Dermoid and fibroma don't release any tumor marker
Most common ovarian Ca: serous cystadenocarcinoma
Most common ovarian tumor: serous cystadenoma
Most common ovarian tumor in pregnancy: dermoid
Most common ovarian Ca in pregnancy: dysgerminoma
Radiosensitive: dysgerminoma, it is moderately radio sensitive
Which germ cell tumor is BL: dysgerminoma
Risk of BL is 10-15% as high as 20%
Risk of BL in dermoid is upto 10%
Dermoid is always benign
Risk of malignancy is 0.2-2%
If it occurs, it is squamous cell Ca
Most rapidly growing tumor: endodermal sinus tumor
Which germ cell tumor has best prognosis: dysgerminoma
Worst prognosis: endodermal sinus tumor
It presents as acute abdomen as rapidly growing
Which tumor involves opposite ovary by metastasis: granulosa cell
tumor
Dysgerminoma frequently occurs with another tumor,
Gonadoblastoma
Which tumor has highest risk of torsion: dermoid
Meig's syndrome
Ovarian Fibroma, Ascites, pleural eusion( more common on the rt
side)
Pseudo Meig's : any other tumor other than fibroma with same
other findings
Male counterpart of dysgerminoma: seminoma
Staging
It's a surgical staging
Stage 1
A: unilateral ovary involved
B: bilateral ovary involved
C: a or B with any of the following
Tumor in the surface
Ruptured capsule
Malignant Ascites
Stage 2
A: involvement of uterus and FT
B: any other structure in pelvis
C: any of the following with A and B
Tumor in the surface
Ruptured capsule
Malignant Ascites
Stage 3
A: microscopic peritoneal deposits
B: macroscopic, but less than 2 cm
C1: macroscopic but more than 2 cms
C2: any positive LN, can be pelvic, para aortic, inguinal
Stage 4
Distant metastasis or tumor in the liver parenchyma
Stage 3 and 4 are called Advanced stage disease
Вам также может понравиться
- Detailed Instructions For Candidates Attending Personality Test Board in Respect of Combined Medical Services Examination, 2017Документ2 страницыDetailed Instructions For Candidates Attending Personality Test Board in Respect of Combined Medical Services Examination, 2017Diwakesh C BОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Genetics: MedpgnotesДокумент19 страницGenetics: MedpgnotesDiwakesh C BОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Chin 200524139Документ1 страницаChin 200524139Diwakesh C BОценок пока нет
- Case Proforma Final, SurgeryДокумент37 страницCase Proforma Final, SurgeryDiwakesh C B100% (4)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- 3 PDFДокумент62 страницы3 PDFDiwakesh C BОценок пока нет
- 2 Medicine MCQs NephrologyДокумент3 страницы2 Medicine MCQs NephrologyDiwakesh C BОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- 1 Medicine MCQs - CNSДокумент10 страниц1 Medicine MCQs - CNSDiwakesh C B80% (5)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Neet PG Mock 4Документ65 страницNeet PG Mock 4Diwakesh C B100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- 5 Medicine MCQs - RheumatologyДокумент11 страниц5 Medicine MCQs - RheumatologyDiwakesh C B100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- ALL INDIA 2005 (AIPGE 2005 January, Answers, Explanation and Notes)Документ97 страницALL INDIA 2005 (AIPGE 2005 January, Answers, Explanation and Notes)Diwakesh C BОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Notes Jun 30, 2014 Anatomy Part 1Документ37 страницNotes Jun 30, 2014 Anatomy Part 1Diwakesh C BОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Karnataka BankДокумент6 страницKarnataka BankS Vivek BhatОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Dragon Ball AbrigedДокумент8 страницDragon Ball AbrigedAlexander SusmanОценок пока нет
- CS 124/LINGUIST 180 From Languages To Information: Conversational AgentsДокумент58 страницCS 124/LINGUIST 180 From Languages To Information: Conversational AgentsamanОценок пока нет
- End of Semester Student SurveyДокумент2 страницыEnd of Semester Student SurveyJoaquinОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Parts Catalog: TJ053E-AS50Документ14 страницParts Catalog: TJ053E-AS50Andre FilipeОценок пока нет
- Topic 6Документ6 страницTopic 6Conchito Galan Jr IIОценок пока нет
- Chapter 6 Bone Tissue 2304Документ37 страницChapter 6 Bone Tissue 2304Sav Oli100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Group 2 Lesson 2 DramaДокумент38 страницGroup 2 Lesson 2 DramaMar ClarkОценок пока нет
- English HL P1 Nov 2019Документ12 страницEnglish HL P1 Nov 2019Khathutshelo KharivheОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Kolehiyo NG Lungsod NG Lipa: College of Teacher EducationДокумент3 страницыKolehiyo NG Lungsod NG Lipa: College of Teacher EducationPrincess LopezОценок пока нет
- New Kanban System DesignДокумент4 страницыNew Kanban System DesignJebin GeorgeОценок пока нет
- Full Download Test Bank For Health Psychology Well Being in A Diverse World 4th by Gurung PDF Full ChapterДокумент36 страницFull Download Test Bank For Health Psychology Well Being in A Diverse World 4th by Gurung PDF Full Chapterbiscuitunwist20bsg4100% (18)
- Intro To Law CasesДокумент23 страницыIntro To Law Casesharuhime08Оценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Tesmec Catalogue TmeДокумент208 страницTesmec Catalogue TmeDidier solanoОценок пока нет
- FAMILYДокумент3 страницыFAMILYJenecel ZanoriaОценок пока нет
- Concordia: The Lutheran Confessions - ExcerptsДокумент39 страницConcordia: The Lutheran Confessions - ExcerptsConcordia Publishing House28% (25)
- Kumar-2011-In Vitro Plant Propagation A ReviewДокумент13 страницKumar-2011-In Vitro Plant Propagation A ReviewJuanmanuelОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- PS4 ListДокумент67 страницPS4 ListAnonymous yNw1VyHОценок пока нет
- Astm D1895 17Документ4 страницыAstm D1895 17Sonia Goncalves100% (1)
- Pda Teachers GuideДокумент2 страницыPda Teachers Guidepeasyeasy100% (2)
- Kutune ShirkaДокумент11 страницKutune ShirkaAnonymous CabWGmQwОценок пока нет
- Digestive System LabsheetДокумент4 страницыDigestive System LabsheetKATHLEEN MAE HERMOОценок пока нет
- Photo Essay (Lyka)Документ2 страницыPhoto Essay (Lyka)Lyka LadonОценок пока нет
- Approach To A Case of ScoliosisДокумент54 страницыApproach To A Case of ScoliosisJocuri KosoОценок пока нет
- E Tech SLHT QTR 2 Week 1Документ11 страницE Tech SLHT QTR 2 Week 1Vie Boldios Roche100% (1)
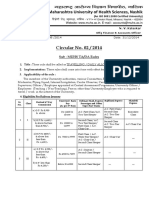
- Circular No 02 2014 TA DA 010115 PDFДокумент10 страницCircular No 02 2014 TA DA 010115 PDFsachin sonawane100% (1)
- Information: Republic of The Philippines Regional Trial Court 8 Judicial Region Branch VIДокумент2 страницыInformation: Republic of The Philippines Regional Trial Court 8 Judicial Region Branch VIlossesaboundОценок пока нет
- Finding Neverland Study GuideДокумент7 страницFinding Neverland Study GuideDean MoranОценок пока нет
- BCG-How To Address HR Challenges in Recession PDFДокумент16 страницBCG-How To Address HR Challenges in Recession PDFAnkit SinghalОценок пока нет
- DE1734859 Central Maharashtra Feb'18Документ39 страницDE1734859 Central Maharashtra Feb'18Adesh NaharОценок пока нет