Академический Документы
Профессиональный Документы
Культура Документы
Ne W Engl and Journal Medicine
Загружено:
hanifahrafaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ne W Engl and Journal Medicine
Загружено:
hanifahrafaАвторское право:
Доступные форматы
new england
The
journal of medicine
established in 1812 august 25 , 2005 vol. 353 no. 8
A Comparison of Medical Management with Misoprostol
and Surgical Management for Early Pregnancy Failure
Jun Zhang, Ph.D., M.D., Jerry M. Gilles, M.D., Kurt Barnhart, M.D., Mitchell D. Creinin, M.D.,
Carolyn Westhoff, M.D., and Margaret M. Frederick, Ph.D., for the National Institute of Child Health
and Human Development (NICHD) Management of Early Pregnancy Failure Trial*
abstract
background
Misoprostol is increasingly used to treat women who have a failed pregnancy in the From the National Institute of Child Health
first trimester. We assessed the efficacy, safety, and acceptability of this treatment in a and Human Development, Bethesda, Md.
(J.Z.); the University of Miami, Miami
large, randomized trial. (J.M.G.); the University of Pennsylvania,
Philadelphia (K.B.); the University of Pitts-
methods burgh, Pittsburgh (M.D.C.); Columbia Uni-
versity, New York (C.W.); and Clinical Tri-
A total of 652 women with a first-trimester pregnancy failure (anembryonic gestation, als and Surveys Corporation, Baltimore
embryonic or fetal death, or incomplete or inevitable spontaneous abortion) were (M.M.F.). Address reprint requests to Dr.
randomly assigned to receive 800 g of misoprostol vaginally or to undergo vacuum Zhang at the Epidemiology Branch,
NICHD, NIH, Bldg. 6100, Rm. 7B03, Be-
aspiration (standard of care) in a 3:1 ratio. The misoprostol group received treatment thesda, MD 20892, or at zhangj@mail.
on day 1, a second dose on day 3 if expulsion was incomplete, and vacuum aspiration on nih.gov.
day 8 if expulsion was still incomplete. Surgical treatment (for the misoprostol group)
*Participants in the NICHD Management
or repeated aspiration (for the vacuum-aspiration group) within 30 days after the initial of Early Pregnancy Failure Trial are listed
treatment constituted treatment failure. in the Appendix.
N Engl J Med 2005;353:761-9.
results Copyright 2005 Massachusetts Medical Society.
Of the 491 women assigned to receive misoprostol, 71 percent had complete expulsion
by day 3 and 84 percent by day 8 (95 percent confidence interval, 81 to 87 percent).
Treatment failed in 16 percent of the misoprostol group and 3 percent of the surgical
group (absolute difference, 12 percent; 95 percent confidence interval, 9 to 16 percent)
by day 30. Hemorrhage or endometritis requiring hospitalization was rare (1 percent
or less in each group), with no significant differences between the groups. In the miso-
prostol group, 78 percent of the women stated that they would use misoprostol again if
the need arose and 83 percent stated that they would recommend it to others.
conclusions
Treatment of early pregnancy failure with 800 g of misoprostol vaginally is a safe and
acceptable approach, with a success rate of approximately 84 percent.
n engl j med 353;8 www.nejm.org august 25, 2005 761
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
an ultrasound examination demonstrating an em-
e arly pregnancy failure occurs in
15 percent of clinically recognized preg-
nancies.1 The most common types of early
pregnancy failure include spontaneous abortion,
anembryonic gestation, and embryonic or fetal
bryonic pole or crownrump length between 5 and
40 mm without cardiac activity,8 an anembryonic
gestational sac with a mean diameter between 16
and 45 mm,9 growth of the gestational sac by less
death. Approximately one in four women will have than 2 mm over a five-day period or less than 3 mm
an early pregnancy failure during her lifetime.1 For over a seven-day period,10 or an increase in human
most of the 20th century, dilatation and curettage chorionic gonadotropin levels of less than 15 per-
was the commonly accepted approach to early preg- cent over a two-day period, with a yolk sac visual-
nancy failure. This practice can be traced back to ized by ultrasound examination. Women who had
the late 19th and early 20th centuries, when illegally an incomplete or inevitable abortion were also in-
induced abortions commonly resulted in hemor- cluded. Incomplete spontaneous abortion was de-
rhage and sepsis.2 With the legalization of abor- fined as the passage of some products of concep-
tion and the availability of antibiotics, these prob- tion, with the residual anteroposterior endometrial
lems have become rare. In more recent years, the lining exceeding 30 mm on transvaginal ultraso-
medical community began to question whether im- nography and a uterine size indicating less than 13
mediate evacuation by surgical intervention was weeks of gestation. This cut-off was based on evi-
necessary for uncomplicated cases of early preg- dence from prior studies of women treated with
nancy failure.3,4 misoprostol for medical abortion11 or early preg-
Expectant management is clearly an option for nancy failure.12 Inevitable abortion was defined as
incomplete spontaneous abortion, but the success an intrauterine gestational sac of less than 45 mm
rate with the use of this approach for embryonic or or embryonic pole of less than 40 mm and an inter-
fetal death or anembryonic gestation is suboptimal nal cervical os that was open to digital examination
(ranging from 25 to 76 percent).5,6 The interval to with active vaginal bleeding. Women were excluded
spontaneous expulsion is unpredictable, and it may if they had anemia (hemoglobin level below 9.5 g per
take a month. The uncertainty and anxiety, along deciliter), had hemodynamic instability, had a his-
with the sadness resulting from pregnancy loss, tory of a clotting disorder or were using anticoagu-
often make expectant management less appealing lants (not including aspirin), were allergic to pros-
to patients. taglandins or nonsteroidal antiinflammatory drugs,
Medical management with misoprostol for early or had previously undergone a surgical or medical
pregnancy failure appears to offer more prompt abortion that was either self-induced or induced by
evacuation of the uterus and has become an increas- other physicians during the current pregnancy. All
ingly popular alternative.7 However, the efficacy, subjects provided written informed consent.
safety, and acceptability of this approach have yet At enrollment, the medical history, hemoglobin
to be established in a large, randomized trial. We level, and Rh-antigen status were assessed and a
conducted a multicenter randomized trial compar- physical examination was performed. Using a cen-
ing misoprostol treatment with vacuum aspiration, tralized, computer-automated telephone response
the current standard of care, for early pregnancy system, we randomly assigned eligible subjects to
failure. either medical or surgical management in a 3:1 ratio
(i.e., approximately 75 percent of the subjects were
methods assigned to receive medical management and 25
percent to receive surgical treatment). Randomiza-
This randomized trial was approved by the institu- tion was stratified according to the study site and
tional review boards of the National Institute of the type of pregnancy failure (anembryonic gesta-
Child Health and Human Development, Columbia tion or fetal death vs. incomplete or inevitable spon-
University, the University of Miami, the University taneous abortion) and used randomly permuted
of Pennsylvania, the University of Pittsburgh, and blocks. The day of randomization was considered
Clinical Trials and Surveys Corporation. Patients study day 1.
who sought medical care for possible early preg- Surgical management typically consisted of
nancy failure at the four university settings from manual vacuum aspiration in an outpatient setting
March 2002 to March 2004 were screened. Women at Columbia University and the University of Pitts-
who had an anembryonic gestation or embryonic burgh and electric vacuum aspiration in an oper-
or fetal death were eligible for inclusion if they had ating room at the University of Miami and the
762 n engl j med 353;8 www.nejm.org august 25 , 2005
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
misoprostol for early pregnancy failure
University of Pennsylvania. The aspiration was per- study as a noninferiority trial. Success was defined
formed by a study investigator or by a resident phy- a priori as complete uterine evacuation without the
sician who was supervised by an investigator. All need for vacuum aspiration in the medical-manage-
women were contacted by telephone on day 8 to in- ment group or a repeated aspiration in the surgi-
quire about any symptoms, medications, or emer- cal-management group within 30 days after initial
gency visits to the hospital after the treatment. treatment. On the basis of clinical judgment, we de-
Women returned for a follow-up visit on day 15 cided that, for medical treatment to be considered
(range, day 13 to day 18). a reasonable alternative to surgery, it should be suc-
Although randomized trials have not identified cessful in at least 80 percent of the women; since
the optimal dose of misoprostol, 800 g given vag- prior data suggested a success rate of 98 percent for
inally was the most commonly tested regimen.7 surgical intervention,14 we selected an absolute dif-
Thus, for the women assigned to medical treatment ference of 18 percent as the maximal acceptable
in our study, four 200-g tablets (800 g) of miso- difference between the two treatment groups to in-
prostol (Cytotec, Searle) were inserted into the pos- dicate noninferiority. We used a one-sided test of
terior fornix through a speculum. These women equivalence with a significance level of 0.05. A total
returned on day 3 (range, day 2 to day 5). If expul- of 620 subjects were needed for the study to achieve
sion of the products of conception was not com- a statistical power of 80 percent.15
plete (that is, a gestational sac was still visualized We first compared the baseline characteristics
or the endometrial lining was greater than 30 mm and the success rate according to clinical site in the
on transvaginal ultrasonography), a second 800-g two groups, using the chi-square test (or Fishers
dose of misoprostol was administered vaginally. On exact test) and Students t-test for categorical and
day 8 (range, day 6 to day 10), if the expulsion of continuous variables, respectively. All these analy-
products of conception was still not complete, vac- ses were done with the use of SAS software. In ad-
uum aspiration was offered. The women returned dition, we calculated 95 percent confidence inter-
for a follow-up visit on day 15. vals for differences in success rates with the use of
The women were given 30 tablets of ibuprofen StatXact software.16 According to the protocol, the
(200 mg) and 20 tablets of codeine (30 mg) for pain data and safety monitoring committee conducted
and were instructed to use ibuprofen primarily and one interim analysis after half the subjects had been
the narcotic as needed. They also received a struc- recruited. No early termination occurred.
tured diary in which to record side effects, medica-
tions, and emergency calls or visits to the hospital, results
and they were instructed to take their temperature
daily for two weeks. Pain intensity was recorded on A total of 652 women were enrolled: 491 were ran-
a 10-cm visual-analogue scale, with higher numbers domly assigned to receive misoprostol, and 161 to
indicating greater pain.13 At each follow-up visit, undergo vacuum aspiration (Fig. 1). Overall, em-
transvaginal ultrasonography was performed, and bryonic or fetal death was diagnosed in 58 percent
the clinical investigator performed a physical exam-of the women, an anembryonic gestation was diag-
ination, conducted an interview, and collected the nosed in 36 percent, and an incomplete or inevita-
diary pages. In addition, at the day 15 visit, hemo-ble abortion was diagnosed in 6 percent. The aver-
globin was measured and each woman completed age gestational age was 7.6 weeks. There were no
a questionnaire assessing the acceptability of the significant differences in demographic characteris-
treatment and the quality of life. A telephone inter-
tics at enrollment between the two groups (Table 1).
view was conducted on day 30 (range, day 25 to day Almost all the women who were assigned to medi-
35) to determine whether any woman underwent cal management received misoprostol immediately
additional treatment. Women with symptoms po- after randomization. In contrast, 63 percent of the
tentially related to the study treatment were fol- women who were assigned to surgical management
lowed until the symptoms resolved. received the treatment on the day of randomiza-
tion, 28 percent did so one day after randomization,
statistical analysis and 9 percent did so two or more days after random-
Recognizing that the success rate of medical treat- ization, owing to the need to wait for an operating
ment was unlikely to exceed that of surgical treat- room. Surgical treatment was manual vacuum aspi-
ment for early pregnancy failure,7 we designed the ration in 57 percent of the women and electric aspi-
n engl j med 353;8 www.nejm.org august 25, 2005 763
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
652 Women enrolled
491 Assigned to misoprostol 161 Assigned to vacuum aspiration
490 Eligible 159 Eligible
487 Received misoprostol 155 Underwent aspiration 2 Ineligible (did not
1 Ineligible (received
2 Had expulsion 3 Had expulsion meet ultrasonographic
methotrexate before
before misoprostol before aspiration criteria)
enrollment)
1 Withdrew after 1 Withdrew after
randomization randomization
Successful in 412 Failed in 76
1 Dose in 346 1 Dose in 32 No follow-up Successful in 143 Failed in 5 No follow-up
2 Doses in 64 2 Doses in 43 for 2 for 11
0 Doses in 2 0 Doses in 1
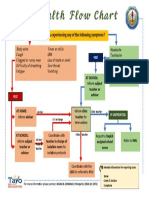
Figure 1. Randomization, Treatment, and Outcomes.
ration in 43 percent. The efficacy of these treatments tween groups of 6 percentage points. Our study de-
did not vary significantly among the four clinical fined success a priori as the absence of the need for
centers (Table 2). vacuum aspiration for any reason within 30 days
The success rates of the treatments are presented after the initial treatment with misoprostol. Four
in Table 3. Of the women who completed the trial women (all from the misoprostol group), however,
according to the protocol, 84 percent (95 percent underwent vacuum aspiration after day 30 for heavy
confidence interval, 81 to 87 percent) were suc- bleeding or persistent bleeding.
cessfully treated with misoprostol and 97 percent In the misoprostol group, the expulsion of prod-
(95 percent confidence interval, 94 to 100 percent) ucts of conception was complete after one dose in
were successfully treated with vacuum aspiration. 71 percent of the women (346 of 490). Among
The absolute difference in success rates between the those who received a second dose, this approach
two treatments was 12 percentage points (95 per- was successful by day 8 in 60 percent (64 of 107),
cent confidence interval, 9 to 16 percent). for an overall success rate of 84 percent by day 8.
To assess the potential effect of losses to follow- The success rate varied among the subtypes of early
up, we performed secondary analyses assessing pregnancy failure; women with an anembryonic
success rates on the basis of various assumptions. gestation had a lower rate of success by day 8 than
Assuming that women who did not return for fol- did the other groups combined (P=0.02). There
low-up had all been successfully treated yielded an was no significant relationship in either treatment
absolute difference in success rates between treat- group between the gestational age at the time of
ments of 12 percentage points. Assuming that treat- the treatment and the success rate (P=0.67 for the
ment had failed in all women who did not complete misoprostol group and P=0.30 for the surgical
follow-up resulted in an absolute difference be- group) (Table 3).
764 n engl j med 353;8 www.nejm.org august 25 , 2005
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
misoprostol for early pregnancy failure
Table 1. Characteristics of the Study Population at Enrollment.*
Characteristic Misoprostol (N=491) Vacuum Aspiration (N=161)
Age yr 29.87.2 30.97.3
Race or ethnic group no. (%)
Non-Hispanic white 114 (23) 32 (20)
Non-Hispanic black 149 (30) 48 (30)
Hispanic 202 (41) 69 (43)
Asian or other 26 (5) 12 (7)
Education no. (%)
Less than high-school graduate 116 (24) 33 (20)
High-school graduate 143 (29) 43 (27)
Attended college 232 (47) 85 (53)
No. of previous pregnancies no. (%)
0 116 (24) 31 (19)
1 128 (26) 49 (30)
2 247 (50) 81 (50)
Planned pregnancy no. (%) 165 (34) 56 (35)
Best estimate of gestational age wk 7.61.5 7.61.4
Low abdominal pain in previous 24 hr no. (%) 298 (61) 86 (53)
Vaginal bleeding in previous 24 hr no. (%) 318 (65) 101 (63)
Type of pregnancy failure no. (%)
Embryonic or fetal death 282 (57) 96 (60)
Anembryonic gestation 179 (36) 56 (35)
Incomplete spontaneous abortion 19 (4) 3 (2)
Inevitable abortion 11 (2) 6 (4)
Hemoglobin g/dl 12.81.0 12.81.0
* Plusminus values are means SD. There were no significant differences between groups.
Race or ethnic group was self-reported.
Hemorrhage and pelvic infection were rare after cent, P=0.09). A decrease in hemoglobin of at least
either treatment (1 percent or less); the rates of these 3 g per deciliter occurred more frequently in the
complications did not differ significantly between misoprostol group than in the vacuum-aspiration
groups (Table 4). The incidence of fever (tempera- group (5 percent vs. 1 percent, P=0.04). Women
ture, 38.0C [100.4F] or greater) was also similar who received misoprostol were also more likely to
in the two groups. Among 13 women in the miso- report nausea, vomiting, abdominal pain, and more
prostol group who had fever, 2 visited the hospital severe pain. Nonetheless, 83 percent of women
and 1 received antibiotic therapy. Among six women stated that they would probably or absolutely rec-
in the surgical group who had fever, three visited ommend misoprostol treatment to their family and
the hospital and two received antibiotic therapy. No friends, and 78 percent stated that they would prob-
maternal sepsis occurred. The frequency of emer- ably or absolutely use it again should similar circum-
gency visits to the hospital during the first 24 hours stances occur in the future. The acceptability of treat-
after treatment was similar in the medical and sur- ment did not differ significantly between groups.
gical groups (3 percent and 2 percent, respectively; Furthermore, among 190 women who had under-
P=0.59). gone vacuum aspiration in previous pregnancies but
The percentage of women who made unsched- who received misoprostol during the current preg-
uled visits to the hospital was slightly but not sig- nancy, 80 percent stated that they would recom-
nificantly higher in the misoprostol group than in mend misoprostol treatment and 73 percent stated
the vacuum-aspiration group (23 percent vs. 17 per- that they would use misoprostol again if needed.
n engl j med 353;8 www.nejm.org august 25, 2005 765
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
Table 2. Results According to Clinical Site.
Site Misoprostol Vacuum Aspiration
No. of Success Failure No Follow-up P No. of Success Failure No Follow-up P
Women* (N=412) (N=76) (N=2) Value Women (N=143) (N=5) (N=11) Value
no. of women (%) no. of women (%)
Columbia University 101 82 (81) 17 (17) 2 (2) 0.17 33 29 (88) 1 (3) 3 (9) 0.79
University of Miami 166 143 (86) 23 (14) 0 53 49 (92) 2 (4) 2 (4)
University of Pennsylvania 113 97 (86) 16 (14) 0 37 34 (92) 0 3 (8)
University of Pittsburgh 110 90 (82) 20 (18) 0 36 31 (86) 2 (6) 3 (8)
* One patient was ineligible.
P values are for the comparison among the four groups.
Two patients were ineligible.
Table 3. Efficacy of the Treatments.
Vacuum Absolute
Variable Misoprostol Aspiration Difference
% (no./total no.) %
Success by day 30
Data on women lost to follow-up treated as missing 84 (412/488) 97 (143/148) 12
Outcome among women lost to follow-up considered a success 84 (414/490) 97 (154/159) 12
Outcome among women lost to follow-up considered a failure 84 (412/490) 90 (143/159) 6
Success after 0 or 1 dose of misoprostol by day 30 71 (348/488)
Success by day 3 71 (347/490)
Success by day 8 84 (414/490)
Success by day 15 85 (417/490) 90 (143/159) 5
Embryonic or fetal death 88 (244/278)
Anembryonic gestation 81 (142/176)
Incomplete or inevitable abortion 93 (28/30)
Success rate according to timing of treatment
5 Wk of gestation 67 (6/9) 100 (2/2)
6 Wk of gestation 82 (93/114) 91 (31/34)
7 Wk of gestation 84 (115/137) 100 (41/41)
8 Wk of gestation 85 (90/106) 100 (36/36)
9 Wk of gestation 88 (67/76) 91 (20/22)
10 Wk of gestation 88 (21/24) 100 (8/8)
11 Wk of gestation 94 (15/16) 100 (1/1)
12 Wk of gestation 83 (5/6) 100 (3/3)
cent). The risks of hemorrhage and pelvic infection
discussion
were very low, and the side effects were tolerable.
Our study indicates that treatment of early pregnan- Misoprostol treatment was acceptable to most
cy failure with 800 g of misoprostol vaginally, with women.
the dose repeated after 48 hours when necessary, is The efficacy of misoprostol treatment for early
efficacious. The success rate by day 30 was 84 per- pregnancy failure has varied greatly (ranging from
cent (95 percent confidence interval, 81 to 87 per- 13 to 100 percent) in previous retrospective and
766 n engl j med 353;8 www.nejm.org august 25 , 2005
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
misoprostol for early pregnancy failure
Table 4. Adverse Events and Acceptability of Medical and Surgical Treatment of Early Pregnancy Failure.*
Variable Misoprostol Vacuum Aspiration P Value
Adverse event
Hemorrhage requiring hospitalization with or without blood trans- 1 (5/488) 1 (1/148) 1.0
fusion % (no./total no.)
Hospitalization for endometritis % (no./total no.) <1 (2/488) 0 (0/148) 1.0
Fever (temperature 38.0C [100.4F]) % (no./total no.) 3 (13/477) 4 (6/148) 0.41
Emergency visit to hospital within 24 hr after treatment 3 (15/488) 2 (3/148) 0.59
% (no./total no.)
Unscheduled hospital visits % (no. of visits/total no. of patients) 23 (114/488) 17 (25/148) 0.09
Change in hemoglobin between day 1 and day 15 g/dl 0.651.10 0.180.89 <0.001
Decrease in hemoglobin 2 g/dl % (no./total no.) 9 (38/421) 4 (5/134) 0.05
Decrease in hemoglobin 3 g/dl % (no./total no.) 5 (19/421) 1 (1/134) 0.04
Nausea % (no./total no.) 53 (250/472) 29 (41/141) <0.001
Vomiting % (no./total no.) 20 (96/475) 7 (10/142) <0.001
Diarrhea % (no./total no.) 24 (113/473) 10 (14/142) <0.001
Abdominal pain % (no./total no.) 99 (473/476) 95 (134/141) <0.001
Pain-severity score 5.72.4 3.22.4 <0.001
Acceptability % (no./total no.)
Would probably or absolutely recommend this procedure 83 (379/456) 83 (125/150) 0.95
Would probably or absolutely use this treatment again 78 (357/456) 75 (112/150) 0.36
* Plusminus values are means SD.
The chi-square test (or Fishers exact test) was used for categorical variables, and Students t-test was used for continu-
ous variables.
A woman could have had multiple unscheduled visits.
Hemoglobin analyses included four women who received a blood transfusion. Values were available for 421 women in
the misoprostol group and 134 women in the vacuum-aspiration group.
This symptom was reported in a womans diary within 48 hours after the treatment.
A 10-cm visual-analogue scale was used to record the severity of pain. Scores could range from 0 (no pain) to 10 (worst
pain ever). Scores were available for 476 women in the misoprostol group and 141 women in the vacuum-aspiration
group.
prospective studies.7 This variation may be attribut- tion. However, by using a second dose if expulsion
able to small sample sizes, the type of pregnancy is incomplete, a similarly high success rate can be
failure (anembryonic gestation and embryonic or achieved in the latter group of women. We waited
fetal death vs. incomplete abortion), the dose of mi- 48 hours between doses in an attempt to allow suf-
soprostol, and the criteria used to define success. ficient time for the initial dose to be effective while
Studies of misoprostol to date have used a sin- acknowledging the desire for prompt uterine evac-
gle dose (ranging from 400 to 800 g), two or three uation; the majority of the women in our study re-
consecutive doses given 2 to 4 hours apart (with a ported satisfaction with this approach.
total dose of 600 to 1800 g within 24 hours), or an Some previous studies have used an endometrial
initial dose (ranging from 400 to 800 g) that could thickness of 15 mm as assessed by transvaginal ul-
be repeated 24 to 48 hours later if needed.7 We trasonography as a cut-off for success.17 However,
found that an 800-g dose of misoprostol adminis- increasing evidence from women who have had a
tered vaginally was sufficient in the majority of spontaneous abortion18 or a medical abortion11,12
women, with side effects that were tolerable to most or received medical treatment for early pregnancy
women. We also found that women with an incom- failure19 suggested that such a cut-off may be too
plete or inevitable spontaneous abortion were more stringent. In our study, almost all women with an
likely to have complete expulsion after one dose of endometrial thickness of greater than 15 mm but
misoprostol than were women with embryonic or less than 30 mm after misoprostol treatment com-
fetal death or women with an anembryonic gesta- pleted expulsion spontaneously and uneventfully.
n engl j med 353;8 www.nejm.org august 25, 2005 767
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
In findings consistent with those of previous utable to our use of a relatively stringent definition
studies, our trial demonstrated that complications of incomplete abortion (an endometrial thickness
with misoprostol treatment occur at a rate of less of 30 mm, as compared with one of 15 mm in pre-
than 1 in 70 treated patients. In the misoprostol vious studies). In addition, women who were hav-
group, 3 percent of women reported an emergency ing active, heavy bleeding when they presented to
visit within 24 hours after treatment (a rate not sig- the hospital were ineligible, since they had a medi-
nificantly different from that in the surgical group), cal indication for emergency vacuum aspiration.
and one woman (0.2 percent) required emergency Thus, women who had an anembryonic gestation
vacuum aspiration within 24 hours. Our experience, or embryonic or fetal death were overrepresented in
in accordance with that in other literature on medi- our study population. Furthermore, we studied
cal abortion,20 suggests that hospitalizing patients only vaginal administration of misoprostol. Previ-
for the misoprostol treatment is unnecessary. As ous randomized trials have indicated that the effi-
long as clear instructions for monitoring bleeding cacy of misoprostol is similar whether it is admin-
and infection are given to women and emergency istered vaginally or orally, whereas the incidence of
service is readily accessible, self-administration of nausea, vomiting, and diarrhea was higher when the
misoprostol at home could increase the conve- agent was administered orally.21-23 It is not known
nience and privacy and further reduce the cost. Pre- whether 800 g of misoprostol represents the low-
vious data have clearly demonstrated that women est effective dose for all subtypes of early pregnancy
can comfortably insert pills into the vagina at failure.
home.20 In summary, our study shows that treatment of
Our trial was large and involved a 30-day follow- early pregnancy failure with 800 g of misoprostol
up period. The vast majority of patients recovered vaginally, with the dose repeated after 48 hours
satisfactorily in two weeks, but a small number re- when necessary, is efficacious and safe. The risks of
quired surgical evacuation even after one month. hemorrhage and pelvic infection are similar to those
In addition, tissue was often seen in the cervical os with vacuum aspiration, and the side effects are
of women who came for an emergency visit and tolerable. Misoprostol treatment is an acceptable al-
sometimes at the follow-up visit; it was removed in ternative to surgical management for most women.
many cases with ring forceps without further treat- Funded by contracts (N01-HD-1-3321, N01-HD-3322, N01-HD-
3323, N01-HD-3324, and N01-HD-3325) with the National Insti-
ment. It is uncertain whether tissue in the os simply tute of Child Health and Human Development, National Institutes
reflects the normal process of expulsion or wheth- of Health.
er its presence intensifies and prolongs bleeding. Drs. Creinin and Westhoff report having served as consultants to
Pfizer, which now owns Searle. Dr. Westhoff reports having received
Our study included relatively few women with grant support from Pfizer.
an incomplete or inevitable abortion. This is attrib-
ap p e n d i x
The following persons and institutions participated in the NICHD Management of Early Pregnancy Failure Trial: NICHD J. Zhang, T.
Nansel; Columbia University C. Westhoff, A. Davis, C. Robilotto; University of Miami J. Gilles, M. Diro, F. Doyle, N. Vazquez; University of
Pennsylvania K. Barnhart, J. Hollander, T. Bader, K. Timbers, A. Hummel, L. Martino; University of Pittsburgh M. Creinin, B. Harwood,
R. Guido, L. Reid; Clinical Trials and Surveys Corporation M. Frederick, X.K. Huang; Data and Safety Monitoring Committee P. Coney (chair),
J.M. Alvir, P.D. Blumenthal, B. Littman, T. MacKay.
refer enc es
1. Alberman E. Spontaneous abortions: plete spontaneous abortion? Am J Obstet management concepts. Obstet Gynecol
epidemiology. In: Stabile I, Grudzinskas G, Gynecol 1998;179:1279-82. Surv 2001;56:105-13.
Chard T, eds. Spontaneous abortion: diag- 5. Jurkovic D, Ross JA, Nicolaides KH. 8. Goldstein SR. Significance of cardiac ac-
nosis and treatment. London: Springer- Expectant management of missed miscar- tivity on endovaginal ultrasound in very early
Verlag, 1992:19-20. riage. Br J Obstet Gynaecol 1998;105:670- embryos. Obstet Gynecol 1992;80:670-2.
2. Hertig AT, Livingstone RG. Spontane- 1. 9. Rowling SE, Coleman BG, Langer JE,
ous, threatened, and habitual abortion: their 6. Luise C, Jermy K, May C, Costello G, Arger PH, Nisenbaum HL, Horii SC. First
pathogenesis and treatment. N Engl J Med Collins WP, Bourne TH. Outcome of expect- trimester US parameters of failed pregnan-
1944;230:797-806. ant management of spontaneous first tri- cy. Radiology 1997;203:211-7.
3. Macrow P, Elstein M. Managing miscar- mester miscarriage: observational study. 10. Nyberg DA, Mack LA, Laing FC, Patten
riage medically. BMJ 1993;306:876. BMJ 2002;324:873-5. RM. Distinguishing normal from abnormal
4. Ballagh SA, Harris HA, Demasio K. Is 7. Creinin MD, Schwartz JL, Guido RS, Py- gestational sac growth in early pregnancy.
curettage needed for uncomplicated incom- mar HC. Early pregnancy failure current J Ultrasound Med 1987;6:23-7.
768 n engl j med 353;8 www.nejm.org august 25 , 2005
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
misoprostol for early pregnancy failure
11. Harwood B, Meckstroth KR, Mishell Cambridge, Mass.: Cytel Software Corpora- efficacy, acceptability and future directions.
DR, Jain JK. Serum beta-human chorionic tion, 2000:428-35. Am J Obstet Gynecol 2000;183:Suppl 2:S44-
gonadotropin levels and endometrial thick- 17. Graziosi GCM, Mol BWJ, Reuwer PJH, S53.
ness after medical abortion. Contraception Drogtrop A, Bruinse HW. Misoprostol ver- 21. Pang MW, Lee TS, Chung TKH. Incom-
2001;63:255-6. sus curettage in women with early pregnan- plete miscarriage: a randomized controlled
12. Creinin MD, Harwood B, Guido RS, Fox cy failure after initial expectant manage- trial comparing oral with vaginal misopros-
MC, Zhang J. Endometrial thickness after ment: a randomized trial. Hum Reprod tol for medical evacuation. Hum Reprod
misoprostol use for early pregnancy failure. 2004;19:1894-9. 2001;16:2283-7.
Int J Gynaecol Obstet 2004;86:22-6. 18. Fox MC, Creinin MD, Meyn LA, Murthy 22. Tang OS, Lau WNT, Ng EHY, Lee SWH,
13. Revill SI, Robinson JO, Rosen M, Hogg AS, Harwood B. Ultrasound appearance of Ho PC. A prospective randomized study to
MIJ. The reliability of a linear analogue for the endometrium after medical abortion. compare the use of repeated doses of vagi-
evaluating pain. Anaesthesia 1976;31:1191- Contraception 2004;70:261. abstract. nal with sublingual misoprostol in the man-
8. 19. Luise C, Kermy K, Collons WP, Bourne agement of first trimester silent miscarriag-
14. Grimes DA, Cates WC Jr. Complications TH. Expectant management of incomplete, es. Hum Reprod 2003;18:176-81.
from legally-induced abortion: a review. Ob- spontaneous first-trimester miscarriage: 23. Honkanen H, Piaggio G, Hertzen H, et
stet Gynecol Surv 1979;34:177-91. outcome according to initial ultrasound cri- al. WHO multinational study of three miso-
15. Makuch R, Simon R. Sample size re- teria and value of follow-up visits. Ultra- prostol regimens after mifepristone for ear-
quirements for evaluating a conservative sound Obstet Gynecol 2002;19:580-2. ly medical abortion. BJOG 2004;111:715-
therapy. Cancer Treat Rep 1978;62:1037-40. 20. Newhall EP, Winikoff B. Abortion with 25.
16. StatXact 4 for Windows: users manual. mifepristone and misoprostol: regimens, Copyright 2005 Massachusetts Medical Society.
physician-journalist
The Journal is seeking a physician with substantial reporting
experience to write occasional articles on timely topics in medicine
and society for the Perspective section. Send curriculum vitae and
writing samples to Perspective Editor, New England Journal of Medicine,
10 Shattuck St., Boston, MA 02115, or at writer@nejm.org.
n engl j med 353;8 www.nejm.org august 25, 2005 769
The New England Journal of Medicine
Downloaded from nejm.org by hengki permana on June 29, 2014. For personal use only. No other uses without permission.
Copyright 2005 Massachusetts Medical Society. All rights reserved.
Вам также может понравиться
- A Randomized Trial of Misoprostol Compared With Manual Vacuum Aspiration For Incomplete AbortionДокумент8 страницA Randomized Trial of Misoprostol Compared With Manual Vacuum Aspiration For Incomplete AbortionElena ZepedaОценок пока нет
- Ultrasound in Obstet Gyne - 2021 - Fernlund - Reproductive Outcome After Early Miscarriage Comparing Vaginal MisoprostolДокумент7 страницUltrasound in Obstet Gyne - 2021 - Fernlund - Reproductive Outcome After Early Miscarriage Comparing Vaginal MisoprostolPutu Gede WidyatamaОценок пока нет
- Progesterone and The Risk of Preterm Birth Among Women With A Short CervixДокумент8 страницProgesterone and The Risk of Preterm Birth Among Women With A Short Cervixangela_karenina_1Оценок пока нет
- Linical Ounds Management Options For Women With Midtrimester Fetal Loss: A Case ReportДокумент4 страницыLinical Ounds Management Options For Women With Midtrimester Fetal Loss: A Case ReportGianna RamosОценок пока нет
- Ectopic Pregnancy: Clinical PracticeДокумент9 страницEctopic Pregnancy: Clinical PracticeNurul WulandariОценок пока нет
- Mifepristone and Misoprostol For Early Pregnancy Failure: A Cohort AnalysisДокумент6 страницMifepristone and Misoprostol For Early Pregnancy Failure: A Cohort AnalysisBobby SetiawanОценок пока нет
- IJGO Incomp BlumДокумент0 страницIJGO Incomp BlumTrigunawangantengОценок пока нет
- Mifepristone Antagonization With Progesterone To Prevent Medical AbortionДокумент8 страницMifepristone Antagonization With Progesterone To Prevent Medical Abortionนีล ไบรอันОценок пока нет
- Minimal Stimulation IVF Vs Conventional IVFДокумент8 страницMinimal Stimulation IVF Vs Conventional IVFpolygoneОценок пока нет
- ANESTHESIOLOGY (R) 2016 - Refresher Course Lecture Summaries副本(被拖移)Документ9 страницANESTHESIOLOGY (R) 2016 - Refresher Course Lecture Summaries副本(被拖移)Han biaoОценок пока нет
- Document GelmezogluДокумент7 страницDocument GelmezogluMonica Salas LaverianoОценок пока нет
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesДокумент8 страницAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyОценок пока нет
- Ijwh 5 811Документ8 страницIjwh 5 811Anonymous ORleRrОценок пока нет
- First Trimester BleedingДокумент9 страницFirst Trimester BleedingarmandokinОценок пока нет
- Legrado Obstetrico 2013Документ24 страницыLegrado Obstetrico 2013HOSPITAL BOSAОценок пока нет
- Endometrial Carcinoma - Can Fertility Be Preserved?: T. LevyДокумент6 страницEndometrial Carcinoma - Can Fertility Be Preserved?: T. Levyrashid793Оценок пока нет
- Nama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071Документ11 страницNama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071shalsaОценок пока нет
- Nejme2032499 PDFДокумент2 страницыNejme2032499 PDFBladimir CentenoОценок пока нет
- Comparative Study For Efficacy of Termination in First Trimester Pregnancy Using Misoprostol and MifepristoneДокумент9 страницComparative Study For Efficacy of Termination in First Trimester Pregnancy Using Misoprostol and MifepristonePeertechz Publications Inc.Оценок пока нет
- Grossman-Sep15-Continuing Pregnancy After MifepristoneДокумент6 страницGrossman-Sep15-Continuing Pregnancy After MifepristoneEdward Andres-AnsahОценок пока нет
- Midwifery Triage of First Trimester Bleeding: Susan A. Krause,, and Barbara W. GravesДокумент12 страницMidwifery Triage of First Trimester Bleeding: Susan A. Krause,, and Barbara W. GravesRival Risvaldi RusliОценок пока нет
- Oracle IДокумент10 страницOracle Imaxis4xОценок пока нет
- 04 Shehla20Noor 20PREVALANCE20OF20PRROM20AND20ITS20OUTCOMEДокумент5 страниц04 Shehla20Noor 20PREVALANCE20OF20PRROM20AND20ITS20OUTCOMEMirachel AugustОценок пока нет
- 1 s2.0 S1110569015300042 MainДокумент5 страниц1 s2.0 S1110569015300042 MainAzam alausyОценок пока нет
- Merced 2019Документ14 страницMerced 2019Vanessa CarinoОценок пока нет
- Journal Gyn KETДокумент8 страницJournal Gyn KETImaylani S. SitanggangОценок пока нет
- Thesis On Ectopic Pregnancy in IndiaДокумент7 страницThesis On Ectopic Pregnancy in Indiaynwtcpwff100% (2)
- Medical Management of Incomplete Abortion Using Pervaginal Misoprostol in Chittagong Medical College HospitalДокумент7 страницMedical Management of Incomplete Abortion Using Pervaginal Misoprostol in Chittagong Medical College HospitalBadhon Chandra SarkarОценок пока нет
- Impact of Oligohydramnios On Maternal and PerinataДокумент6 страницImpact of Oligohydramnios On Maternal and PerinataDiana SchlittlerОценок пока нет
- BMJ Outcome of Expectante Management 873.fullДокумент3 страницыBMJ Outcome of Expectante Management 873.fulljuçara bittemcurtОценок пока нет
- Induction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationДокумент6 страницInduction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationFebrinata MahadikaОценок пока нет
- Breast Cancer During Pregnancy A Literature ReviewДокумент7 страницBreast Cancer During Pregnancy A Literature ReviewafmabreouxqmrcОценок пока нет
- Blighted Ovum: A Case ReportДокумент2 страницыBlighted Ovum: A Case Reportakhmad ikhwanОценок пока нет
- A Randomized Trial of Progesterone in Women With Bleeding in Early PregnancyДокумент10 страницA Randomized Trial of Progesterone in Women With Bleeding in Early PregnancyAmpry LoyraОценок пока нет
- Anticoncepcion PostpartoДокумент14 страницAnticoncepcion PostpartomarialecifuentesbОценок пока нет
- Ectopic Pregnancy ThesisДокумент8 страницEctopic Pregnancy ThesisWriteMyPaperCollegeSingapore100% (2)
- Pituitary Tumors: A Clinical CasebookОт EverandPituitary Tumors: A Clinical CasebookLisa B. NachtigallОценок пока нет
- Practice Bulletin Summary: Multifetal Gestations: Twin, Triplet, and Higher-Order Multifetal PregnanciesДокумент3 страницыPractice Bulletin Summary: Multifetal Gestations: Twin, Triplet, and Higher-Order Multifetal PregnancieselmerОценок пока нет
- New England Journal Medicine: The ofДокумент10 страницNew England Journal Medicine: The ofTiffany Rachma PutriОценок пока нет
- Comparison of Misoprostol and Manual Vacuum Aspiration For The Treatment of Incomplete AbortionДокумент5 страницComparison of Misoprostol and Manual Vacuum Aspiration For The Treatment of Incomplete AbortionShofi Dhia AiniОценок пока нет
- Ectopic Pregnancy: A ReviewДокумент13 страницEctopic Pregnancy: A ReviewDinorah MarcelaОценок пока нет
- 57 Andrews2003 PDFДокумент9 страниц57 Andrews2003 PDFangela_karenina_1Оценок пока нет
- 57 Andrews2003 PDFДокумент9 страниц57 Andrews2003 PDFangela_karenina_1Оценок пока нет
- Adjunctive Azithromycin Prophylaxis For Cesarean DeliveryДокумент11 страницAdjunctive Azithromycin Prophylaxis For Cesarean DeliveryrizkiОценок пока нет
- Best Practice & Research Clinical Obstetrics and GynaecologyДокумент12 страницBest Practice & Research Clinical Obstetrics and GynaecologyGrit WingsОценок пока нет
- 976 FullДокумент6 страниц976 FullazifadewiatasyaОценок пока нет
- MALE SEXUAL DYSFUNCTION HarrisonsДокумент7 страницMALE SEXUAL DYSFUNCTION HarrisonsDan Angelo TemplonuevoОценок пока нет
- European Journal of Obstetrics & Gynecology and Reproductive BiologyДокумент3 страницыEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyFahmi Nur SuwandiОценок пока нет
- Csii-Pregnancy in Patients With Mechanical Prosthetic ValvesДокумент6 страницCsii-Pregnancy in Patients With Mechanical Prosthetic Valvesapi-205989841Оценок пока нет
- 1 s2.0 S0020729209615502 Main PDFДокумент1 страница1 s2.0 S0020729209615502 Main PDFPaula UrsuОценок пока нет
- BJOG 2014 GBS Và PROMДокумент10 страницBJOG 2014 GBS Và PROMHòa HồОценок пока нет
- 2013 Chakraborty Outcome of Prelabor Rupture of MembranesДокумент6 страниц2013 Chakraborty Outcome of Prelabor Rupture of MembranesRayhan AlatasОценок пока нет
- Ab 26Документ14 страницAb 26AdelaKalstumAdiibahОценок пока нет
- Pennant Et Al-2016-BJOG - An International Journal of Obstetrics & Gynaecology FichaДокумент8 страницPennant Et Al-2016-BJOG - An International Journal of Obstetrics & Gynaecology Fichaoctavio davilaОценок пока нет
- Article - Infertility Endometriosis PDFДокумент5 страницArticle - Infertility Endometriosis PDFFertility Talks Dr.Tabassum KhanОценок пока нет
- Disparities in The Management of Ectopic Pregnancy: GynecologyДокумент10 страницDisparities in The Management of Ectopic Pregnancy: GynecologysuisОценок пока нет
- Ojog 2013020415273326Документ6 страницOjog 2013020415273326Achmad Safi'iОценок пока нет
- Ijerph 19 08340 PDFДокумент9 страницIjerph 19 08340 PDFShree PatelОценок пока нет
- Pi Is 0020729212003736Документ4 страницыPi Is 0020729212003736Jhon Alexander OrmazaОценок пока нет
- OB - 02 - Outcomes of Multifetal ReductionДокумент6 страницOB - 02 - Outcomes of Multifetal Reductionram4a5Оценок пока нет
- Serenity PrayerДокумент1 страницаSerenity PrayerhanifahrafaОценок пока нет
- 1471 2369 14 154 PDFДокумент10 страниц1471 2369 14 154 PDFhanifahrafaОценок пока нет
- Diastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseaseДокумент6 страницDiastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseasehanifahrafaОценок пока нет
- 1471 2369 14 191 PDFДокумент9 страниц1471 2369 14 191 PDFhanifahrafaОценок пока нет
- Association of Anaemia in Primary Care Patients With Chronic Kidney Disease: Cross Sectional Study of Quality Improvement in Chronic Kidney Disease (QICKD) Trial DataДокумент9 страницAssociation of Anaemia in Primary Care Patients With Chronic Kidney Disease: Cross Sectional Study of Quality Improvement in Chronic Kidney Disease (QICKD) Trial DatahanifahrafaОценок пока нет
- Renal Function, Calcium Regulation, and Time To Hospitalization of Patients With Chronic Kidney DiseaseДокумент10 страницRenal Function, Calcium Regulation, and Time To Hospitalization of Patients With Chronic Kidney DiseasehanifahrafaОценок пока нет
- Toefl PredictionДокумент25 страницToefl PredictionhanifahrafaОценок пока нет
- Critical Appraisal (Descriptive)Документ14 страницCritical Appraisal (Descriptive)hanifahrafa100% (1)
- Dialog Present Continous TenseДокумент2 страницыDialog Present Continous TenseMessy100% (1)
- Nasogastric Gastrostomy Tube Feedling Guidelines v1.4Документ45 страницNasogastric Gastrostomy Tube Feedling Guidelines v1.4bandarascbОценок пока нет
- Histotechnologist, ImmunohistochemistДокумент3 страницыHistotechnologist, Immunohistochemistapi-78178945Оценок пока нет
- ProRoot MTA BrochureДокумент12 страницProRoot MTA BrochureAdela FechetaОценок пока нет
- 10th Monthly Compliance Report On Parkland Memorial HospitalДокумент92 страницы10th Monthly Compliance Report On Parkland Memorial HospitalmilesmoffeitОценок пока нет
- LaQshya Quality Improvement Cycles Resource MaterialДокумент344 страницыLaQshya Quality Improvement Cycles Resource Materialkparasher100% (1)
- Regional Epidemiology Surveillance and Disaster Response UnitДокумент3 страницыRegional Epidemiology Surveillance and Disaster Response UnitthecutealОценок пока нет
- PlagueДокумент31 страницаPlaguelulondon1Оценок пока нет
- Health Flow ChartДокумент1 страницаHealth Flow ChartAlex Cainoy JrОценок пока нет
- Characteristics of Healthcare ProviderДокумент2 страницыCharacteristics of Healthcare ProviderFlora Arcenal100% (1)
- Drug AbuseДокумент38 страницDrug AbuseARIF-UR-REHMAN100% (4)
- CataractДокумент52 страницыCataracttammycristobalmd100% (4)
- Adaptive Immunity: Yanne Pradwi EfendiДокумент25 страницAdaptive Immunity: Yanne Pradwi EfendiMelissa Indah SariОценок пока нет
- Quantum Techniques Client ManualДокумент42 страницыQuantum Techniques Client ManualVeres Beatrix100% (4)
- Flare-Ups After Endodontic Treatment: A Meta-Analysis of LiteratureДокумент5 страницFlare-Ups After Endodontic Treatment: A Meta-Analysis of LiteratureDr.O.R.GANESAMURTHIОценок пока нет
- EclampsiaДокумент14 страницEclampsiaUmi PulunganОценок пока нет
- Use of The Childhood Autism Rating Scale CARS For PDFДокумент10 страницUse of The Childhood Autism Rating Scale CARS For PDFmahwishmahmood 444Оценок пока нет
- MCQ April 2015Документ15 страницMCQ April 2015Sylphana Astharica LawalataОценок пока нет
- LDN Information PackДокумент17 страницLDN Information PackkindheartedОценок пока нет
- Summer Eyetalk BrochureДокумент4 страницыSummer Eyetalk BrochureRey EspinuevaОценок пока нет
- Concepts of DiseaseДокумент55 страницConcepts of DiseaseKailash NagarОценок пока нет
- Emotion Code-Body Code Consent AgreementДокумент1 страницаEmotion Code-Body Code Consent Agreementapi-75991446100% (1)
- DownloadДокумент27 страницDownloadKHAIRUNNISA FADILAОценок пока нет
- Good Bye To AllergyДокумент7 страницGood Bye To Allergykuldip1951Оценок пока нет
- Sleep Physiology and Disorders in Aging and DementiaДокумент17 страницSleep Physiology and Disorders in Aging and DementiaJúlio EmanoelОценок пока нет
- 2015 Revised American Thyroid Association Guidelines For The Management of Medullary Thyroid CarcinomaДокумент44 страницы2015 Revised American Thyroid Association Guidelines For The Management of Medullary Thyroid CarcinomaBeni BolngОценок пока нет
- Maxicare List of PhysiciansДокумент3 952 страницыMaxicare List of PhysiciansEdrian Boado75% (4)
- Acute Pancreatitis Maria Coats v2Документ35 страницAcute Pancreatitis Maria Coats v2Henry MauricioОценок пока нет
- DapusДокумент3 страницыDapusYosi oktarinaОценок пока нет
- Psychiatry 136 Q&AДокумент37 страницPsychiatry 136 Q&AManushi HenadeeraОценок пока нет