Академический Документы
Профессиональный Документы
Культура Документы
Tof Care Plan
Загружено:
kayal67%(12)67% нашли этот документ полезным (12 голосов)
8K просмотров4 страницыTETROLOGY OF FALLOT CARE PLAN
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документTETROLOGY OF FALLOT CARE PLAN
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
67%(12)67% нашли этот документ полезным (12 голосов)
8K просмотров4 страницыTof Care Plan
Загружено:
kayalTETROLOGY OF FALLOT CARE PLAN
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
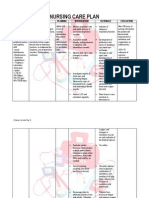
NURSING CARE PLAN
Tetralogy of Fallot
ASSESSMENT NURSING SCIENTIFIC PLANNING RATIONALE IMPLEMENTATION EVALUA-TION
DIAGNOSES ANALYSIS
Cyanosis Risk for Tetralogy fallot After 4 hours of nursing If the patient experience cardiac Assessed and record the vital sign. Objective evaluation:
dyspnea Decreased cardiac results in low intervention the pt, will output he cardiac and respiratory rate Administered cardiac drugs as Baby's condition was
delay in growth output related to oxygenation of have adequate cardiac will increase and bp will decrease. ordered. improved
and development structural blood due to output as evidenced by Cardiac drugs are given to increase Assessed dypsnea,exertion skin
blue anoxia abnormalities of mixing of cardiac rate within the strength of cardiac contractions. color during rest and when active.
attacks the heart. oxygenated and normal range. Indicates hypoxia and increase Avoided allowing the infant to cry
de oxygenated Assess and record the oxygen need. for a long period of time, use soft
blood in the left vital sign. Conserves energy,cross cut nipple nipple when feeding.
ventricle Administer cardiac requires less energy for infant to
through the drugs as ordered. feed.
VSD and Assess
preferential low dypsnea,exertion skin
of both color during rest and
oxygenated and when active.
deoxgenated Avoid allowing the
blood from the infant to cry for a long
ventricles period of time,use soft
through the nipple when feeding
aorta because of
obstruction to
flow through
the pulmonary
valve.
ASSESSMENT NURSING SCIENTIFIC PLANNING RATIONALE IMPLEMENTATION EVALUA-TION
DIAGNOSES ANALYSIS
Objective: Impaired gas Congenital 1. Establish good To gain both trust and Established good trusting Objective evaluation:
exchange related Heart Disease trusting relationship cooperation relationship with the patient the baby condition
-V/S: to altered oxygen refers to a with the patient and was improved
and significant others
supply as
BP:80/50 mmHg evidenced by problem with significant others Monitored respiratory
Indicators of adequacy of
dyspnea, the hearts 2. Monitor respiratory rate/depth, use of accessory
respiratory function or degree of
PR: 124 bpm tachypnea, structure and rate/depth, use of muscles, areas of cyanosis.
compromise and therapy
RR: 28 cpm
tachycardia, and function due to accessory muscles, needs/effectiveness Auscultated breath sounds,
fatigue secondary abnormal heart areas of cyanosis. noting presence or absence
Temp: 37.1 C to Congenital development 3. Auscultate breath Development of atelectasis and and adventitious sounds.
Heart Disease t/c sounds, noting stasis of secretion can impair gas
-with O2 Tetralogy of fallot Before birth. It exchange
can disrupt the
presence or absence Monitored vital signs; note
inhalation @ and adventitious
normal flow of changes in cardiac rhythm.
2lpm via nasal sounds.
blood to the Compensatory changes in vital Compensatory.
cannula as different parts signs and development of Helped with breathing
ordered of the body thus 4. Monitor vital signs; dysrhythmias reflect effects of exercises. Pursed lip
affecting the note changes in impaired gas exchange
-circumoral breathing.
exchange of cardiac rhythm.
cyanosis noted gasses Helps improve oxygen inspiration Elevated head of bed to
Compensatory.
of the lungs moderate or high back rest.
5. Help with breathing
exercises. Pursed lip Helps the lung expand and aids in
breathing. the relaxation of the muscles
6. Elevate head of bed decreasing the oxygen demand of
to moderate or high the body
back rest.
ASSESSMENT NURSING SCIENTIFIC PLANNING RATIONALE IMPLEMENTATION EVALUA-TION
DIAGNOSES ANALYSIS
Objectives: Ineffective tissue Due to 1. Monitor skin colour Cool, blanched, mottled skin Monitored skin colour and Objective evaluation:
perfusion narrowing of and temp. every and cyanosis may indicate temp. every 2hours. the baby condition
-bluish the artery which tissue perfusion was improved
2hours. Assess for Assessed for signs of skin
discoloration on (cardiopulmonary small amount of signs of skin Decrease heart rate and
oxygenated breakdown.
lips noted ) blood pressure may
blood can pass breakdown.
indicateincreased Monitored and documented
-clubbing of Related to through the 2. Monitor and arteriovenousexchange,whic patients vital signs every
finger noted decrease oxygen systemic documented patients h leads to decrease tissue hour..
cellular exchange circulation vital signs every perfusion Kept patient warm
-nasal flaring secondary to
Which the hour.. Warmth aids Elevated lower extremities.
patient 3. Keep patient warm vasodilation,which improve
-use of accessory congenital heart experience Changed position regularly
4. Elevate lower tissue perfusion
disease t/c and inspect skin every shift.
muscle noted difficulty in
extremities. To increase arterial blood
tetralogy of fallot breathing supply and improve tissue
-with capillary 5. Change position
perfusion.
refill time of 3 regularly and inspect To avoid decrease in tissue
seconds skin every shift. perfusion and risk of skin
breakdown.
-with O2 of 2 lpm
via nasal cannula
as ordered
-body weakness
noted(allways on
bed)
Вам также может понравиться
- NCP FORM For TetralogyДокумент3 страницыNCP FORM For TetralogyGraceMelendres100% (3)
- Tetralogy of Fallot Nursing CaseДокумент32 страницыTetralogy of Fallot Nursing CaseUday Kumar50% (2)
- Tetralogy of Fallot NCPДокумент6 страницTetralogy of Fallot NCPHarlene Joyce ReyОценок пока нет
- Tetralogy of Fallot Patient CaseДокумент15 страницTetralogy of Fallot Patient CaseBenjamin Leonzon100% (2)
- Baby fever nursing careДокумент6 страницBaby fever nursing caregopscharanОценок пока нет
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Intervention Rationale EvaluationДокумент1 страницаNovilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Intervention Rationale EvaluationCharina Aubrey100% (3)
- NCP Rheumatic Heart DiseaseДокумент3 страницыNCP Rheumatic Heart DiseaseAdrian Mallar71% (28)
- Nursing Care Plan - EndocarditisДокумент2 страницыNursing Care Plan - EndocarditisJoanna Marie Datahan Estomo100% (12)
- NCP For Nephrotic SyndromeДокумент2 страницыNCP For Nephrotic SyndromeLee Jenny100% (5)
- Pathophysiology and Treatment of Tetralogy of FallotДокумент2 страницыPathophysiology and Treatment of Tetralogy of FallotMark James Melendres100% (12)
- Novilyn C. Pataray BSN - Ii Sickle Cell Anemia: St. Paul College of Ilocos SurДокумент1 страницаNovilyn C. Pataray BSN - Ii Sickle Cell Anemia: St. Paul College of Ilocos SurCharina AubreyОценок пока нет
- NCP HydrocephalusДокумент3 страницыNCP HydrocephalusCazze SunioОценок пока нет
- NCP Hydrocephalus-Delayed Growth and DevelopmentДокумент4 страницыNCP Hydrocephalus-Delayed Growth and DevelopmentCazze Sunio100% (3)
- Proplased Umbilical CordДокумент2 страницыProplased Umbilical Cordkurlstein94% (17)
- Case PresentationДокумент43 страницыCase Presentationkayal100% (1)
- Tetralogy of Fallot OverviewДокумент12 страницTetralogy of Fallot OverviewMaricel Agcaoili GallatoОценок пока нет
- Neonatal Sepsis (NCP)Документ10 страницNeonatal Sepsis (NCP)Lucero Hyacinth100% (1)
- Nursing Care Plan 1Документ4 страницыNursing Care Plan 1Johndelle Banlasan Hernan100% (1)
- NCP Proper 1Документ6 страницNCP Proper 1Noreen PinedaОценок пока нет
- NCPДокумент9 страницNCPTracy Camille EscobarОценок пока нет
- Bronchopneumonia Care PlanДокумент6 страницBronchopneumonia Care PlanAbhijit Soundade0% (1)
- Tetralogy of Fallot Lesson PlanДокумент25 страницTetralogy of Fallot Lesson PlanUday Kumar100% (1)
- pg1-33 of Pneumothorax Case StudyДокумент36 страницpg1-33 of Pneumothorax Case StudyikemasОценок пока нет
- NCP Difficulty of Breathing R/T SecretionДокумент3 страницыNCP Difficulty of Breathing R/T Secretionherscentasiascribd50% (8)
- New Born NCPДокумент8 страницNew Born NCPCarl Vincent Marrion Rejuso100% (1)
- NCP: Gestational HTN - Preeclampsiaeclampsia - Hellp SyndromeДокумент23 страницыNCP: Gestational HTN - Preeclampsiaeclampsia - Hellp SyndromeKath100% (2)
- Tetralogy of FallotДокумент5 страницTetralogy of FallotCharity OaniaОценок пока нет
- Tetralogy of FallotДокумент31 страницаTetralogy of FallotAnditha Namira RS100% (1)
- NCP - Excess Fluid Volume (Aortic Stenosis)Документ3 страницыNCP - Excess Fluid Volume (Aortic Stenosis)Daniel Vergara Arce100% (3)
- NCP - PreeclampsiaДокумент3 страницыNCP - PreeclampsiaRap De la Cruz50% (2)
- Assessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationДокумент10 страницAssessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationApol Pen67% (3)
- NCP RHDДокумент7 страницNCP RHDHenry Roque Tagalag80% (5)
- NCP NicuДокумент3 страницыNCP NicuNoel Telosa100% (1)
- Nursing Diagnosis For AsthmaДокумент6 страницNursing Diagnosis For AsthmaTINAIDA33% (3)
- 1.case Presentation CHDДокумент23 страницы1.case Presentation CHDDHARM MEENA0% (1)
- Ineffective Tissue PerfusionДокумент3 страницыIneffective Tissue PerfusionAngel Hernandez100% (1)
- Cord ProlapseДокумент4 страницыCord ProlapseCleta Escabarte Dehlin100% (1)
- Improving Neonatal Tissue Perfusion for SepsisДокумент2 страницыImproving Neonatal Tissue Perfusion for SepsisNiña Montejo Ealdama100% (1)
- NCP - TBДокумент2 страницыNCP - TBPahw BaluisОценок пока нет
- Monitor for signs of fluid overload: increasing dyspnea, rales, edema, weight gain. Notify physician if presentДокумент3 страницыMonitor for signs of fluid overload: increasing dyspnea, rales, edema, weight gain. Notify physician if presentmakyofrancis20Оценок пока нет
- Nursing Care Plans: Ineffective (Uteroplacental) Tissue PerfusionДокумент2 страницыNursing Care Plans: Ineffective (Uteroplacental) Tissue PerfusionVincent Paul SantosОценок пока нет
- Anthropometric MeasurementsДокумент18 страницAnthropometric MeasurementsJaezee Ramos50% (2)
- Nursing Care Plan Pneumonia With Congenital Heart DiseaseДокумент18 страницNursing Care Plan Pneumonia With Congenital Heart DiseaseKarri Ann Tonel100% (2)
- Pda Case StudyДокумент27 страницPda Case Studykreny10100% (9)
- NCP1 Knowledge DeficitДокумент2 страницыNCP1 Knowledge DeficitNOslipperyslope100% (1)
- Buergers Disease NCPДокумент5 страницBuergers Disease NCPNikko Dela Cruz100% (2)
- MYELOMENINGOCELEДокумент2 страницыMYELOMENINGOCELECass Bartolome50% (2)
- Spina Bifida NCPДокумент3 страницыSpina Bifida NCPCarpz Darpz100% (2)
- Tetralogy of Fallot Case DiscussionДокумент46 страницTetralogy of Fallot Case DiscussionJoe Ha50% (2)
- HyperbilirubinemiaДокумент29 страницHyperbilirubinemiaCham Ingalla Pascion88% (8)
- NCP (Deficient Fluid VolumeДокумент3 страницыNCP (Deficient Fluid VolumeNica RespondoОценок пока нет
- Nursing Care Plan For Acyanotic Heart DiseaseДокумент55 страницNursing Care Plan For Acyanotic Heart DiseaseDeepikaxena John79% (14)
- Defect (VSD) Occurs: Decreased Cardiac Output Related To IndependentДокумент5 страницDefect (VSD) Occurs: Decreased Cardiac Output Related To IndependentPrincess GarciaОценок пока нет
- Kez NCPДокумент12 страницKez NCPShizuka Marycris AmaneОценок пока нет
- CASE SCENARIO and NCPДокумент14 страницCASE SCENARIO and NCPBeverly PagcaliwaganОценок пока нет
- NCPДокумент3 страницыNCPWendy EscalanteОценок пока нет
- NCP Week 6 Nrg301 ValenzonaДокумент3 страницыNCP Week 6 Nrg301 ValenzonaJoshennaОценок пока нет
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveДокумент2 страницыNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanОценок пока нет
- Improve Cardiac Output Through Nursing InterventionsДокумент8 страницImprove Cardiac Output Through Nursing InterventionsJaylord VerazonОценок пока нет
- Nursing Care Plan for a 54-Year-Old Male with Chest Pain and Elevated Cardiac EnzymesДокумент3 страницыNursing Care Plan for a 54-Year-Old Male with Chest Pain and Elevated Cardiac EnzymesDwight DiazОценок пока нет
- Ardy TinitusДокумент4 страницыArdy TinitusArdy SantosoОценок пока нет
- Elder Abuse and Neglect: Brenda Holmes MSN/Ed, RNДокумент25 страницElder Abuse and Neglect: Brenda Holmes MSN/Ed, RNSonia SinghОценок пока нет
- Abdominal TraumaДокумент16 страницAbdominal TraumaBagas SatrioОценок пока нет
- Child Attitude Joward Jllness Scale: EspaňДокумент1 страницаChild Attitude Joward Jllness Scale: EspaňAvinash ToraneОценок пока нет
- RTP RLSSampleUTMCR2CarePlanSnapshotДокумент3 страницыRTP RLSSampleUTMCR2CarePlanSnapshotHendry HuangОценок пока нет
- 84359Документ5 страниц84359Pedro Gouveia100% (1)
- Physical Assessment - General Survey GuideДокумент2 страницыPhysical Assessment - General Survey GuideDanielle TorresОценок пока нет
- Scribe America Final, Emergency DepartmentДокумент41 страницаScribe America Final, Emergency DepartmentJulio CastilloОценок пока нет
- El Médico Inca Conocimiento Empírico y Magia en El Perú Precolombino (En Inglés)Документ28 страницEl Médico Inca Conocimiento Empírico y Magia en El Perú Precolombino (En Inglés)bogotano8Оценок пока нет
- Ineffective Airway ClearanceДокумент2 страницыIneffective Airway ClearanceMaria ArregoitiaОценок пока нет
- 11 Best Herbs For Astral Projection - Insight StateДокумент2 страницы11 Best Herbs For Astral Projection - Insight Stateiamthe100% (1)
- Introduction 2 PDFДокумент178 страницIntroduction 2 PDFSilent StarОценок пока нет
- Transient Ischemic Attack and HomeopathyДокумент32 страницыTransient Ischemic Attack and HomeopathyDr. Rajneesh Kumar Sharma MD HomОценок пока нет
- Medical-Surgical Nursing: (Prepared By: Prof. Rex B. Yangco)Документ12 страницMedical-Surgical Nursing: (Prepared By: Prof. Rex B. Yangco)Leilah Khan100% (1)
- Parakeet RingneckДокумент2 страницыParakeet RingneckAhmer KhanОценок пока нет
- Ill Effects of CrackersДокумент3 страницыIll Effects of Crackersnagpal3Оценок пока нет
- Vital Signs: Learning ObjectivesДокумент35 страницVital Signs: Learning ObjectivesVictoria TamayoОценок пока нет
- Corneal Ulcer - StatPearls - NCBI BookshelfДокумент5 страницCorneal Ulcer - StatPearls - NCBI BookshelfAngel LimОценок пока нет
- The Detection and Measurement of CatatoniaДокумент5 страницThe Detection and Measurement of CatatoniaImon PaulОценок пока нет
- Asma PDFДокумент2 страницыAsma PDFAzizah Hana RОценок пока нет
- Hollamby Mitchell s5001226 Case 1 DtgaДокумент13 страницHollamby Mitchell s5001226 Case 1 Dtgaapi-299009880Оценок пока нет
- Panic Attacks PDFДокумент8 страницPanic Attacks PDFluis_violinosОценок пока нет
- Maintain Acid-Base BalanceДокумент34 страницыMaintain Acid-Base BalanceAnnie GeorgeОценок пока нет
- Calf Protocols Ver4Документ6 страницCalf Protocols Ver4Sadam Irshad100% (1)
- Falun GongДокумент97 страницFalun GongVera GroenОценок пока нет
- Karmic Correlations From Wheel of KnivesДокумент3 страницыKarmic Correlations From Wheel of KnivesBogdanCapsa50% (2)
- Self-Declaration Form - STUDIOДокумент2 страницыSelf-Declaration Form - STUDIOLeticia BikaerОценок пока нет
- SOP 01 Criteria For Donor SelectionДокумент9 страницSOP 01 Criteria For Donor Selectionهشام الشهيميОценок пока нет
- Agbede DanielДокумент18 страницAgbede DanielDaniel AgbedeОценок пока нет
- Assessment of the Musculoskeletal SystemДокумент35 страницAssessment of the Musculoskeletal SystemChristine Joy MolinaОценок пока нет