Академический Документы
Профессиональный Документы
Культура Документы
Community Acquired Pneumonia
Загружено:
Daniel Puentes SánchezАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Community Acquired Pneumonia
Загружено:
Daniel Puentes SánchezАвторское право:
Доступные форматы
Annals of Internal Medicine
In the Clinic
Community-Acquired
Pneumonia Prevention
C
ommunity-acquired pneumonia (CAP) can
vary from a mild outpatient illness to a more Diagnosis
severe disease requiring hospital admission
and, at times, intensive care. CAP is the eighth lead-
ing cause of death, along with inuenza, and is the Treatment
leading cause of death from infectious diseases in
persons in the United States older than 65 years. The
key management decisions related to CAP are rec- Patient Information
ognition and treatment in a timely and effective
manner, dening the appropriate site of care (home,
hospital, or intensive care unit [ICU]), and ensuring
effective prevention. Health careassociated pneu-
monia (HCAP), or pneumonia in persons in contact
with such health care environments as nursing
homes and chronic hemodialysis centers or persons
recently discharged from the hospital, can be
caused by multidrug-resistant (MDR) organisms.
Whether HCAP is best classied as a form of
community-acquired or hospital-acquired pneumo-
nia is controversial.
The CME quiz is available at www.annals.org/intheclinic.aspx. Complete the quiz to earn up to 1.5 CME
credits.
Physician Writer CME Objective: To review current evidence for prevention, diagnosis, treatment, and practice
Michael S. Niederman, MD improvement of community-acquired pneumonia.
Funding Source: American College of Physicians.
Disclosures: Dr. Niederman, ACP Contributing Author, reports personal fees from Pzer,
personal fees from Thermo Fisher Scientic, grants and personal fees from Merck/Bayer, and
personal fees from Cempra outside the submitted work.
In the Clinic does not necessarily represent ofcial ACP clinical policy. For ACP clinical
guidelines, please go to https://www.acponline.org/clinical_information/guidelines/.
With the assistance of additional physician writers, the editors of Annals of Internal Medicine
develop In the Clinic using MKSAP and other resources of the American College of Physicians.
2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
Prevention
Who is at increased risk for age, with a special effort to re-
CAP? view risk factors in persons older
Persons with comorbid illness than 50 years. High-risk individu-
and the elderly are at increased als who should be vaccinated
risk for pneumonia and for hav- include persons living in special
ing a more complex course. In environments (long-term care
2006, there were nearly 1.3 mil- facilities), Alaskan natives or
lion hospitalizations for pneumo- American Indians, and/or those
nia in the United States, and 57% who have any of the following
were in persons older than 65 conditions: chronic heart disease
years (1). Comorbid illnesses that (congestive heart failure, cardio-
are associated with an increased myopathy but not hypertension),
incidence of CAP include respira- chronic lung disease (COPD but
tory disease, such as chronic ob- not asthma), diabetes mellitus,
structive pulmonary disease alcoholism, chronic liver disease,
(COPD); cardiovascular disease; cigarette smoking, cerebrospinal
diabetes mellitus; and chronic uid leaks, cochlear implants,
liver disease. Other at-risk popu- functional or anatomical asplenia
lations include those with HIV (including sickle cell disease),
infection and other forms of im- and immune-suppressing condi-
mune suppression, as well as tions (including HIV infection;
persons who have chronic kidney congenital or acquired immune
disease and those who have had deciencies; chronic renal failure;
splenectomy. nephrotic syndrome; other im-
mune suppression, including re-
Cigarette smoking and alcohol ceipt of long-term corticoste-
abuse also often result in severe roids; and cancer, including
forms of CAP. Cigarette smoking multiple myeloma, leukemia,
is a risk factor for bacteremic lymphoma, and Hodgkin
pneumococcal infection (2). disease).
Other common illnesses in per-
sons with CAP include cancer The 13-valent conjugate vaccine
and any neurologic illness that (PCV-13) and the 23-valent poly-
predisposes to aspiration, includ- saccharide vaccine (PPS-23) are
ing seizures. Immunization with the 2 licensed adult pneumococ-
pneumococcal vaccine in high- cal vaccines available. All adults
risk individuals and with inuenza should receive PCV-13 in series
vaccine in at-risk patients during with PPS-23. However, the timing
inuenza season is benecial for of immunization varies by age
preventing CAP and many of its and the presence of high-risk
complications. conditions. Because PCV-13 is
more immunogenic, it should
Who should receive pneumo- generally be given rst, when
coccal vaccination and when vaccination is indicated, to all
should they receive it? individuals who were not previ-
All individuals aged 65 years and ously immunized, and followed
1. American Lung Associa-
tion. Trends in pneumonia older and other high-risk persons 6 12 months later by PPS-23 (to
and inuenza and pneu- should receive pneumococcal add additional strain coverage).
monia morbidity and
mortality; 2010. vaccination. For persons without Immune-compromised patients
2. Nuorti JP, Butler JC, Farley
MM, et al. Cigarette smok-
high-risk conditions, vaccination younger than 65 years should
ing and invasive pneumo- should be given at age 65 years. receive PPS-23 only 8 weeks after
coccal disease. Active
Bacterial Core Surveillance Patients with risk factors should PCV-13. Persons who have previ-
Team. N Engl J Med. be vaccinated when the risk is ously received PPS-23 should
2000;342:681-9. [PMID:
10706897] rst identied, irrespective of receive a dose of PCV-13 at least
2015 American College of Physicians ITC2 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
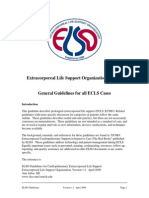
Figure. Recommended pneumococcal vaccine schedule and intervals, by age, health condition, and other risks.
No health condition Chronic Smoker or Immunocompromising Anatomical or Cerebrospinal fluid
or other risk health resident of condition functional asplenia leak or cochlear
condition* long-term implant
care facility
PCV13 PCV13
8 weeks
8 weeks
PPSV23 PPSV23
Adults aged
5 years
1964 years
1 year 5 years PPSV23
Adults aged
65 years
PCV13 5 years
612 months
PPSV23
The dashed line represents the interval between the two PPSV23 doses. PCV13# = 13-valent pneumococcal conjugate vaccine; PPSV23# =
23-valent pneumococcal polysaccharide vaccine.
* Immunocompromising conditions are dened as congenital or acquired immunodeciency (including B- or T-lymphocyte deciency, com-
plement deciencies, and phagocytic disorders excluding chronic granulomatous disease), HIV infection, chronic renal failure, nephrotic
syndrome, leukemia, lymphoma, Hodgkin disease, generalized malignancy, multiple myeloma, solid organ transplant, and iatrogenic immu-
nosuppression (including long-term systemic corticosteroids and radiation therapy).
Anatomical or functional asplenia is dened as sickle cell disease and other hemoglobinopathies, congenital or acquired asplenia, splenic
dysfunction, and splenectomy.
Chronic health conditions are dened as chronic heart disease (including congestive heart failure and cardiomyopathies, excluding hyper-
tension), chronic lung disease (including chronic obstructive lung disease, emphysema, and asthma), chronic liver disease (including cirrhosis),
chronic alcoholism, or diabetes mellitus.
Administer PPSV23 as soon as possible if the 6- to 12-month time window has passed. Reproduced from Reference 3.
1 year after the most recent vac- Although concerns have been
cination. For those with immune- raised about adverse reactions in
compromising conditions, a sec- patients who receive repeated
ond dose of PPS-23 should be vaccination, in 1 study fewer than
given 5 years after the rst dose. 1% of patients who received at
For those who received either 1 least 3 pneumococcal vaccina-
or 2 doses of PPS-23 before 65 tions had an adverse reaction,
years of age, a repeated dose and no reaction was severe, even
should be given at 65 years of when vaccination was repeated
age or older, provided that 5 in less than 6 years (4). Vaccina-
years have passed since the prior tion reduces the frequency of
dose. Although PCV-13 is gener- bacteremic pneumonia in
ally given before PPS-23, current healthy, immune-competent 3. Kim DK, Bridges CB, Harri-
man KH, et al. Advisory
vaccine recommendations allow adults. Not all randomized, con- Committee on Immuniza-
PPS-23 to be given rst in per- trolled trials (RCTs) have found tion Practices Recom-
mended Immunization
sons younger than 65 years who reductions in the frequency of Schedule for Adults Aged
have chronic health conditions bacteremic pneumonia in adults 19 and Older: United
States, 2015. Ann Intern
but are not immune-suppressed with chronic illness, although Med 2015;162:214-23.
PMID: 25654609]
and have not had splenectomy case control studies report 4. Walker FJ, Singleton RJ,
(3) (Figure). reductions from 56% 81%. Bulkow LR, et al. Reactions
after 3 or more doses of
pneumococcal polysaccha-
Pneumococcal vaccination In a double-blind RCT of 84 496 adults older ride vaccine in adults in
should be considered for anyone Alaska. Clin Infect Dis.
than 65 years, PCV-13 prevented both bactere- 2005;40:1730-5. [PMID:
hospitalized for a medical illness. mic and nonbacteremic, vaccine strainspecic 15909258]
6 October 2015 Annals of Internal Medicine In the Clinic ITC3 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
pneumococcal pneumonia and vaccine-type which some patients believe
invasive pneumococcal pneumonia; however, themselves to be allergic) that
it did not prevent all-cause CAP (5). are present in the inactivated
In an RCT of 1006 nursing home residents in vaccine or the live attenuated
Japan, PPS-23 signicantly reduced the fre- nasal vaccine. Live attenuated
quency and mortality of pneumococcal pneu- vaccine can be given intranasally
monia, as well as the frequency but not the to healthy, nonpregnant adults
mortality of all-cause pneumonia (6). up to age 49 years. It should not
be given to health care workers
The efcacy of pneumococcal
who are in contact with (and able
vaccine has not been established
to transmit the virus to) severely
in patients with sickle cell dis-
ease, chronic renal failure, immu- immune-compromised patients
5. Bonten MJM, Huijts SM,
noglobulin deciency, Hodgkin or to those with immunosuppres-
Bolkenbaas M, et al. Poly-
saccharide Conjugate disease, lymphoma, leukemia, or sion and chronic medical condi-
Vaccine Against Pneumo-
multiple myeloma. Use of the tions. A high-dose inuenza vac-
coccal Pneumonia in
Adults. N Engl J Med. 7-valent conjugate vaccine in cine (4 times the standard dose)
2015;372:1114-1125. is available for individuals older
[PMID:25785969] children led to herd immunity for
6. Maruyama T, Taguchi O,
older adults who live with immu- than 65 years. In 1 randomized
Niederman MS, et al.
Efcacy of 23-valent pneu- nized children, but necrotizing trial, this vaccine led to a higher
mococcal vaccine in pre-
pneumonia caused by nonvac- antibody response and better
venting pneumonia and
improving survival in cine strains may be more com- protection against laboratory-
nursing home residents:
double blind, randomised mon in children who receive this conrmed inuenza in persons
and placebo controlled
vaccine (7). older than 65 years than in those
trial. BMJ. 2010;340:
c1004. [PMID: 20211953] who received the standard inu-
7. Bender JM, Ampofo K, What is the role of inuenza enza vaccine (8).
Korgenski K, et al. Pneu-
mococcal necrotizing vaccination in the prevention
pneumonia in Utah: does of CAP and its complications? In a meta-analysis of 20 studies, inuenza vac-
serotype matter? Clin
Infect Dis. 2008;46:1346- All patients at increased risk for cine was shown to reduce pneumonia by 53%,
52. [PMID: 18419434]
inuenza complications and such hospitalization by 50%, and mortality by 68%
8. DiazGranados CA, Dun-
ning AJ, Kimmel M, et al. persons as health care workers (9). In addition, observational studies suggest
Efcacy of high-dose ver- that inuenza vaccine can reduce all-cause
sus standard-dose inu- who are more likely to transmit
enza vaccine in older mortality during inuenza season by 27%
the infection to high-risk patients
adults. N Engl J Med. 54% as well as being cost-effective due to its
2014;371:635-648. (immune-suppressed, elderly, ability to reduce hospitalization rates for con-
[PMID: 25119609]
9. Gross PA, Hermogenes and those with chronic medical gestive heart failure and pneumonia in elderly
AW, Sacks HS, et al. The illness), should be immunized persons (10). However, recent analyses ques-
efcacy of inuenza vac-
cine in elderly persons. A yearly. Adults aged 18 49 years tion these benets, noting that few RCTs have
meta-analysis and review
of the literature. Ann In-
can receive recombinant inu- been conducted in these populations and that
tern Med. 1995;123:518- enza vaccine, which does not selection bias may lead to vaccination of
27. [PMID: 7661497]
10. Nichol KL, Margolis KL, contain the egg proteins (to healthier persons (11, 12).
Wuorenma J, et al. The
efcacy and cost effec-
tiveness of vaccination
against inuenza among Prevention... Persons at risk for CAP and its complications should be
elderly persons living in offered pneumococcal and inuenza vaccination at the doses and fre-
the community. N Engl J
Med. 1994;331:778-84. quencies described here. In nonvaccinated individuals in whom pneu-
[PMID: 8065407] mococcal vaccine is indicated, give PCV-13 rst followed by PPS-23
11. Centers for Medicare &
Medicaid Services. Hos-
6 12 months later in immune-competent persons but after only 8 weeks
pital Quality Initiative in immune-suppressed patients. For persons who have previously re-
Overview. Accessed at ceived PPS-23, give 1 dose of PCV-13 at least 1 year after the prior im-
www.cms.hhs.gov
/HospitalQualityInits munization. Repeat PPS-23 vaccination after 5 years in persons older
/Downloads/Hospital- than 65 years who received the previous (1 or 2) doses before age 65
overview.pdf on 24 Au-
gust 2009.
years, and after 5 years at any age in immune-suppressed patients. In-
12. Nelson JC, Jackson ML, uenza vaccine should be offered yearly to at-risk persons, including
Weiss NS, Jackson LA. health care workers, with consideration of the high-dose vaccine in per-
New strategies are
needed to improve the sons older than 65 years. Patients hospitalized with a medical illness
accuracy of inuenza should be considered for both of these vaccines.
vaccine effectiveness
estimates among se-
niors. J Clin Epidemiol.
2009;62:687-94. [PMID:
19124221]
CLINICAL BOTTOM LINE
2015 American College of Physicians ITC4 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
Diagnosis
Which symptoms should lead present for longer periods in el-
clinicians to consider CAP? derly persons.
Pneumonia usually presents with Which organisms cause CAP?
both respiratory and systemic
The most commonly identied
symptoms, particularly in young
bacterial pathogens for CAP are
patients and immune-competent
Streptococcus pneumoniae
persons. It should be suspected
(pneumococcus); Haemophilus
when the patient has cough, pu-
rulent sputum, pleuritic chest inuenzae; and atypical patho-
pain, dyspnea, chills, fever, night gens, such as Mycoplasma pneu-
sweats, and weight loss. Fever moniae, Chlamydophila pneu-
and chills have a sensitivity of moniae, and Legionella. Patients
50% 85% but may be absent in older than 65 years and those
elderly persons. Dyspnea has a with alcoholism, noninvasive dis-
sensitivity of 70% for the diagno- ease, antibiotic therapy within 3
sis of CAP, whereas purulent spu- months, multiple medical comor-
tum has a sensitivity of only 50%. bid conditions, exposure to chil-
Hemoptysis suggests necrotizing dren in a day care center, or im-
infection, such as lung abscess, munosuppressive illness are
tuberculosis, or gram-negative more likely to have drug-resistant
pneumonia. Many older patients pneumococcus (DRSP) than
and those with chronic illness other patients (Table).
have a weaker immune response,
and the disease may go unrecog- A cohort study of 3339 patients with invasive
pneumococcal infection found that if the pa-
nized because the patient has
tient had received penicillin, macrolide, uoro-
only nonrespiratory symptoms.
quinolone, or trimethoprimsulfamethoxazole
These symptoms include confu- therapy 3 months before the onset of bactere-
sion, weakness, lethargy, falling, mia, the organism was more likely to be resis-
poor oral intake, and decompen- tant to the antibiotic recently received (13).
sation of a chronic illness (for ex-
ample, congestive heart failure). Viruses can also cause CAP, and
Most patients with CAP present 1 recent study found viruses in
with an acute illness 12 days in 18% of all patients who had
duration, but symptoms may be paired serologies. The most com-
Table. Modifying Factors That Increase the Risk for Infection With Specic
Pathogens
Organism Risk Factor
Penicillin-resistant and Age >65 years
drug-resistant pneumococci -lactam therapy within the past 3 months
Alcoholism
Immune-suppressive illness (including therapy with
corticosteroids)
Multiple medical comorbid conditions
Exposure to a child in a day care center
Enteric gram-negative bacteria Residence in a nursing home
Underlying cardiopulmonary disease
Multiple medical comorbid conditions
Recent antibiotic therapy
Pseudomonas aeruginosa Structural lung disease (bronchiectasis) 13. Toronto Invasive Bacterial
Corticosteroid therapy (prednisone, >10 mg/d) Disease Network. Predict-
Broad-spectrum antibiotic therapy for >7 d in the ing antimicrobial resis-
past month tance in invasive pneu-
Malnutrition mococcal infections. Clin
Infect Dis. 2005;40:
1288-97. [PMID:
15825031]
6 October 2015 Annals of Internal Medicine In the Clinic ITC5 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
mon viral organisms were inu- those with poor functional status,
enza and parainuenza virus, fol- severe illness, recent antibiotic
lowed by respiratory syncytial therapy, and recent hospitaliza-
virus and adenovirus. Viruses are tion (18). Methicillin-resistant S.
also common in patients with se- aureus (MRSA) can occur in pa-
vere CAP, especially with the ad- tients with HCAP and in previ-
vent of molecular diagnostic ously healthy persons after inu-
methods. In a study of 198 ICU enza, particularly in the form of a
patients with CAP or HCAP, vi- severe, bilateral, necrotizing in-
ruses were present in 72, using fection (19, 20).
real-time polymerase chain reac-
14. Choi SH, Hong SB, Ko What is the role of history and
GB, et al. Viral infection tion (PCR) testing or shell vial cul-
in patients with severe physical examination in the
pneumonia requiring tures of either bronchoalveolar
intensive care unit ad- lavage or nasal swabs. Rhinovi-
diagnosis of CAP?
mission. Am J Respir Crit
rus, parainuenza, inuenza, and History and physical examination
Care Med. 2012;186:
325-32. [PMID: respiratory syncytial virus were are valuable for suggesting the
22700859]
15. Wiemken T, Peyrani P, most common (14). In another presence of pneumonia, predict-
Bryant K, et al. Incidence
study of 468 ICU patients, viruses ing the cause, and helping to de-
of respiratory viruses in
patients with were present in 23% of adults, ne severity. The history can
community-acquired
using PCR testing of nasopharyn- identify risk factors for HCAP,
pneumonia admitted to
the intensive care unit:
geal swabs (15). Gram-negative such as hospitalization or antibi-
results from the Severe
Inuenza Pneumonia bacteria have been found in up otic therapy in the past 90 days,
Surveillance (SIPS) proj- residence in a long-term care
ect. Eur J Clin Microbiol to 10% of patients with CAP (al-
facility, long-term dialysis, outpa-
Infect Dis. 2013;32:705- though some of these patients
10. [PMID: 23274861] tient wound care, or home infu-
16. Arancibia F, Bauer TT, are now classied as having
Ewig S, et al. sion therapy. It can also identify
Community-acquired HCAP), particularly those with a
patients who might have a less
pneumonia due to gram- history of chronic cardiopulmo-
negative bacteria and common cause of pneumonia,
pseudomonas aerugi- nary disease, residence in a nurs-
nosa: incidence, risk, and such as bird (Chlamydia psittaci,
ing home, multiple medical co-
prognosis. Arch Intern Cryptococcus neoformans) or bat
Med. 2002;162:1849- morbid conditions, recent
58. [PMID: 12196083] (Histoplasma capsulatum) expo-
17. El-Solh AA, Pietrantoni C, antibiotic therapy, renal insuf-
sure or travel to the southwestern
Bhat A, et al. Microbiol- ciency, chronic liver disease, dia-
ogy of severe aspiration United States (endemic fungi,
pneumonia in institu- betes, or active cancer (16). Pseu-
tionalized elderly. Am J such as coccidioidomycosis). In
domonas aeruginosa should be
Respir Crit Care Med. addition to fever, dyspnea,
2003;167:1650-4. considered in persons with bron-
[PMID: 12689848] cough, and pleuritic chest pain,
18. Maruyama T, Fujisawa T, chiectasis, recent hospitalization,
symptoms can include confusion,
Okuno M, et al. A new or recent antibiotic therapy. Al-
strategy for health care- weakness, falling, lethargy, re-
associated pneumonia: a though anaerobic organisms
2-year prospective multi- duced oral intake, or deteriora-
should be considered when aspi-
center cohort study using tion due to a chronic illness (such
risk factors for multidrug- ration is a possibility (for exam-
resistant pathogens to as congestive heart failure).
select initial empiric ple, in elderly patients with neu-
therapy. Clin Infect Dis. rologic or swallowing disorders),
2013;57:373-83. [PMID: Clinical examination ndings
23999080] in 1 study the most common or- suggestive of pneumonia include
19. Carratala J, Mykietiuk A,
Fernandez-Sabe N, et al. ganisms identied in persons at fever or hypothermia, tachypnea,
Health care-associated risk for aspiration were gram- crackles, bronchial breath sounds
pneumonia requiring
hospital admission: negative bacteria (17). Klebsiella on auscultation, and pleural effu-
epidemiology, antibiotic
therapy, and clinical
pneumoniae has been reported sion. Specic ndings that are
outcomes. Arch Intern in patients with alcoholism. Al- associated with a poor outcome
Med. 2007;167:1393-9.
[PMID: 17620533] though some studies suggest include a respiratory rate greater
20. Infectious Diseases Soci- that HCAP pathogens are more than 30 breaths/min, diastolic
ety of America. Infectious
Diseases Society of Amer- similar to those in hospital- blood pressure less than 60 mm
ica/American Thoracic
Society consensus guide-
acquired pneumonia than to Hg, systolic blood pressure less
lines on the manage- those in CAP, not all studies con- than 90 mm Hg, heart rate
ment of community-
acquired pneumonia in rm these ndings. Patients with greater than 125 beats/min, and
adults. Clin Infect Dis. HCAP who are most at risk for temperature less than 35 C or
2007;44 Suppl 2:S27-
72. [PMID: 17278083] drug-resistant organisms are greater than 40 C. An elderly
2015 American College of Physicians ITC6 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
person with CAP may present present even in the absence of a
with nonrespiratory symptoms radiographic inltrate if the pa-
and ndings because of an im- tient has a convincing history
paired immune and inammatory and focal physical ndings; a fol-
response. low-up radiograph may show an
inltrate. Interobserver variability
When should clinicians use
in chest radiographic interpreta-
chest radiography?
tion was shown in 1 study that
A chest radiograph should be
compared the readings of
obtained in all patients with clini-
at least 2 radiologists. Positive
cal features suggesting CAP to
agreement (59%) was less fre-
dene the presence of parenchy-
quent than negative agreement
mal lung infection and to identify
(94%) (23).
certain pneumonia complica-
tions. Clinical diagnosis of pneu- What is the role of other
monia is often inaccurate and has laboratory tests?
an overall sensitivity ranging For outpatients, perform pulse
from 70%90% and a specicity oximetry to assess oxygenation.
ranging from 40%70% (20, 21). No other tests are needed. For
Elderly and immunosuppressed inpatients, additional testing is
patients can have radiographic done to dene disease severity
evidence of pneumonia without and identify the cause. Measure
clear-cut clinical features. In 1 pulse oximetry in all patients and
study, measurement of serum arterial blood gases in those sus-
procalcitonin levels added to pected of having carbon dioxide
physical examination data in- retention. Even with extensive di-
creased the predictive value of agnostic testing, a specic cause is
an abnormal chest radiograph (22). found in fewer than half of all pa-
When history (cough, fever, dyspnea, pleuritic tients. Sputum should be collected
pain) and physical examination ndings (focal for Gram stain and culture before
crackles, temperature 38 C) were used to therapy is started in patients sus-
predict the presence of radiographic pneumo- pected of being infected with a
nia in a study of 129 patients with lower respi- drug-resistant or unusual patho-
ratory tract infection (26 with pneumonia), no gen, but evaluation of sputum
combination of ndings was highly accurate. should be done only if it is of good
The positive predictive value of each nding quality and processed rapidly.
varied from 17% 43% (21).
Rapid diagnostic testing of respira-
It is especially important to have tory secretions with molecular
a chest radiograph if the diagno- methods (such as PCR) is now be- 21. Graffelman AW, le Cessie
sis is questionable or if pleural coming widely available, although S, Knuistingh Neven A,
et al. Can history and
effusion, lung abscess, necrotiz- their value for patient manage- exam alone reliably
ing pneumonia, or multilobar ment is uncertain because they predict pneumonia?
J Fam Pract. 2007;56:
illness is suspected. Radiographs may be too sensitive and unable to 465-70. [PMID:
17543257]
can specically aid patient man- distinguish colonization from infec- 22. Muller B, Harbarth S,
agement if ndings of severe ill- tion. In patients with severe pneu- Stolz D, et al. Diagnostic
and prognostic accuracy
ness are present (bilateral, multi- monia, 2 sets of blood cultures of clinical and laboratory
should be collected and urine parameters in
lobar, or rapidly expanding community-acquired
inltrates), but patterns only tested for Legionella and pneumo- pneumonia. BMC Infect
Dis. 2007;7:10. [PMID:
rarely suggest a specic diagno- coccal antigens. Limit blood cul- 17335562]
sis or cause (e.g., tuberculosis, P. tures to patients with severe ill- 23. Hopstaken RM, Witbraad
T, van Engelshoven JM,
jiroveci). If pleural effusion is ness; these cultures are positive in Dinant GJ. Inter-observer
variation in the interpre-
present, conrmation should be only 10%20% of all patients with tation of chest radio-
obtained with a decubitus lm, CAP. In low-risk patients (without graphs for pneumonia in
community-acquired
thoracic ultrasonography, or severe illness), the incidence of lower respiratory tract
computed tomography. Pneumo- false-positive results may exceed infections. Clin Radiol.
2004;59:743-52. [PMID:
nia should be assumed to be the incidence of true-positive re- 15262550]
6 October 2015 Annals of Internal Medicine In the Clinic ITC7 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
sults (20, 24). Culture an endotra- role in the routine management
cheal aspirate in patients who are of CAP is not dened. Serum
intubated and mechanically levels of procalcitonin identify
ventilated. patients who can benet from
antibiotic therapy; levels are ele-
A study of 13 043 Medicare patients identied the
vated with bacterial and Legion-
following predictors of true-positive results on blood
ella infection, but not always with
culture: no previous receipt of antibiotics, underlying
liver disease, systolic blood pressure <90 mm Hg, other atypical pathogen infec-
temperature <35 C or >40 C, pulse >125/min, tion, and not with viral infection.
blood urea nitrogen levels >10.71 mmol/L (30 mg/ Serial measurements of procalci-
dL), serum sodium levels <130 mmol, and leuko- tonin levels may help guide when
cyte count <5 or >20 109 cells/L. The diagnostic to stop antibiotic therapy (26).
yield of blood cultures increased in patients with 1 or
more of the above predictors and in those who had A randomized trial of 302 patients with CAP
not received antibiotics before blood collection (24). compared patients managed by usual care
with those managed by an algorithm recom-
Do not perform serologic tests mending antibiotics and the duration of ther-
for viruses and atypical patho- apy. The algorithm was based on serial mea-
gens because they require con- surement of procalcitonin levels using the
valescent titers 6 8 weeks after highly sensitive Kryptor assay. Procalcitonin
the initial test to identify infec- levels were measured on admission and after
tion. Rapid diagnostic tests that 6 24 hours, 4 days, 6 days, and 8 days. The
can evaluate for viral pathogens procalcitonin-guided group had signicantly
fewer antibiotic prescriptions on admission
on nasopharyngeal swabs, such
and less antibiotic use, and the duration of
as rapid antigen testing, direct therapy was reduced from 12 to 5 days with
uorescent antibody, or PCR, are similar clinical success (27). Measurement of
available. However, the role of serum procalcitonin, using the Kryptor assay at
these tests in managing patients the time of admission, has been shown in 4
with CAP and in guiding antibi- randomized studies (of both single-center and
24. Metersky ML, Ma A, otic selection are not yet estab- multicenter design) to reduce antibiotic use. In
Bratzler DW, Houck PM.
Predicting bacteremia in lished, although some studies these studies, antibiotic therapy was discour-
patients with have shown that they may reduce aged when the procalcitonin level was <0.25
community-acquired
pneumonia. Am J Respir unnecessary antibiotic use and g/L, with no adverse effects on mortality (26).
Crit Care Med. 2004;
169:342-7. [PMID:
increase antiviral use, especially What other disorders should
14630621] when results are positive for inu- clinicians consider in patients
25. van der Eerden MM,
Vlaspolder F, de Graaff enza. Regardless, establishing a
suspected of having CAP?
CS, et al. Comparison specic cause is usually not nec-
between pathogen di- If the patient does not respond to
rected antibiotic treat- essary because empirical therapy
ment and empirical empirical therapy after 48 72
broad spectrum antibi-
is effective. For example, when
hours, consider the possibility of
otic treatment in patients pathogen-directed treatment
with community ac- a virus or an unusual bacterial
quired pneumonia: a was compared with empirical
prospective randomised pathogens, such as Mycobacte-
treatment using a broad-spec-
study. Thorax. 2005;60: rium tuberculosis (which may be
672-8. [PMID: trum antibiotic, the 2 groups did
16061709] masked by a partial response to
26. Upadhyay S, Niederman not signicantly differ in the
empirical quinolone therapy of
MS. Biomarkers: what is length of hospital stay, 30-day
their benet in the iden- CAP) or endemic fungi (histoplas-
tication of infection, mortality, clinical failure, or reso-
severity assessment, and mosis, coccidioidomycosis, blas-
management of
lution of fever (25).
community-acquired
tomycosis). Also consider non-
pneumonia? Infect Dis Measurement of serum levels of infectious possibilities, such as
Clin North Am. 2013
27:19-31. [PMID: C-reactive protein or procalci- bronchiolitis obliterans with or-
3398863] tonin may be helpful to dene ganizing pneumonia, pulmonary
27. Christ-Crain M, Stolz D,
Bingisser R, et al. Procal- which patients have bacterial vasculitis, hypersensitivity pneu-
citonin guidance of anti-
biotic therapy in
pneumonia, to decide whether to monitis, interstitial diseases, lung
community-acquired start antibiotic therapy, to deter- cancer, lymphangitic carcinoma,
pneumonia: a random-
ized trial. Am J Respir mine prognosis, and to provide bronchoalveolar cell carcinoma,
Crit Care Med. 2006; supportive information in the lymphoma, and congestive heart
174:84-93. [PMID:
16603606] site-of-care decision, but their failure. If the patient's condition de-
2015 American College of Physicians ITC8 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
teriorates after an initial response to patients do not respond to initial tomycosis), Pasteurella multo-
therapy, consider pulmonary em- empirical therapy. An infectious cida, Bacillus anthracis,
bolus; antibiotic-induced colitis; and disease specialist can help iden- Actinomyces Israeli, Francisella
the pneumonia complications of tify infectious complications of tularensis (tularemia), Yersinia
empyema, meningitis, and pneumonia and unusual infec- pestis (plague), or Chlamydia
endocarditis. tions, such as Coxiella burnetii (Q psittaci (psittacosis). A pulmo-
fever), Burkholderia pseudomallei nary specialist can help identify
When should clinicians (melioidosis), Mycobacterium inammatory lung disease and
consider specialty consultation tuberculosis (which may be pulmonary embolus and per-
for diagnosis, and which types masked by a partial response to form bronchoscopy and trans-
of specialists should they consult? empirical quinolone therapy of bronchial biopsy. A surgeon can
Consultation is most valuable to CAP) , endemic fungi (histoplas- perform thoracoscopic or open
clarify diagnostic questions when mosis, coccidioidomycosis, blas- lung biopsy.
Diagnosis... History is particularly valuable for dening risk factors for
specic pathogens, and physical ndings help dene disease severity.
Clinical ndings are less dramatic in elderly persons. Conrm the diag-
nosis of CAP with a chest radiograph, although this test is not always
denitive early in the course of illness. Laboratory testing has limited
value; however, it can be used in conjunction with other data to dene
severity and to identify systemic and respiratory complications. Diag-
nosing specic pathogens early is less useful because most initial ther-
apy is empirical. If the patient does not respond to initial therapy, con-
sult specialists and consider bronchoscopy and lung biopsy for a
denitive diagnosis.
CLINICAL BOTTOM LINE
Treatment
How should clinicians the hospital. The BTS rule has patients who had low levels of procalcitonin had
determine whether a patient been condensed into the CURB- low mortality, regardless of PSI class or number
with CAP requires outpatient, 65, which is based on the pres- of CURB-65 points (29).
inpatient, or ICU care? ence of Confusion, blood Urea Current guidelines support ICU
Many site-of-care decisions can nitrogen >7.0 mmol/L (19.6 mg/ care if the patient needs assisted
be facilitated with the pneumonia dL), Respiratory rate 30 ventilation, has septic shock re-
severity index (PSI) or the British breaths/min, systolic Blood pres- quiring vasopressors, or has at
Thoracic Society (BTS) rule. sure <90 mm Hg or diastolic least 3 of the following: respira-
These tools predict risk for death. blood pressure <60 mm Hg, and tory rate 30 breaths/min, PaO2/
Patients at high risk are generally age 65 years. Patients with at FiO2 ratio 250, multilobar inl-
managed in the hospital, and least 2 of these criteria are usu- trates, confusion or
those at highest risk are man- ally admitted to the hospital, disorientation, blood urea nitro-
aged in the ICU. The PSI straties whereas those with at least 3 gen 7.1 mmol/L (20 mg/dL),
patients into 5 categories by us- criteria are considered for ICU leukocyte count <4 109 cells/L,
ing a scoring system based on admission (20, 28, 29). platelet count <100 109
patient age, comorbid illness, cells/L, temperature lower than
physical examination ndings, One prospective study of 3181 patients seen
36 C, and hypotension requir-
and laboratory data. In general, in 32 emergency departments compared the
ing aggressive uid resuscitation
PSI with the CURB and CURB-65 criteria and
patients in classes I and II are (20). One study found that leu-
found that both approaches accurately identi-
treated as outpatients, those in ed low-risk patients. CURB-65 was better for kopenia, thrombocytopenia, and
class III have the site-of-care deci- predicting mortality in high-risk patients (28). In hypothermia were each present
sion based on careful clinical as- another prospective study of 1651 patients, mea- in <5% of all patients; further,
sessment, and those in classes IV surement of serum procalcitonin levels supple- omitting these criteria and re-
and V are generally admitted to mented data obtained by prognostic scoring, and placing them with acidosis sim-
6 October 2015 Annals of Internal Medicine In the Clinic ITC9 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
plied the prediction of need for doxime, or cefuroxime) with a
ICU admission without a loss of macrolide or doxycycline. If the
accuracy (30). patient has received an antibiotic
in the past 3 months, avoid using
What is the role of nondrug
an antibiotic of the same class.
therapies?
In outpatients, nondrug therapy How long should outpatients
should focus on encouraging continue antibiotic treatment?
oral hydration. For hospitalized The duration of therapy should
patients, nondrug therapies in- be based on the patient's clinical
clude intravenous hydration and response, severity of illness, and
oxygen for hypoxemia. Chest probable pathogen. Outpatients
physiotherapy has not been with mild-to-moderate CAP can
widely studied, but it has been be treated for as few as 5 days if
shown to improve the outcome clinical response is good, there
of patients with pneumonia who has been no fever for 48 to 72
have more than 30 mL/d of spu- hours, and there are no signs of
tum and impaired clearance of extrapulmonary infection. Azi-
secretions (31). A meta-analysis thromycin has such a long half-
of 6 randomized trials in 434 pa- life that therapy for 1 or 3 days
tients evaluated the following 4 may be effective.
types of chest physiotherapy:
conventional chest physiotherapy, A meta-analysis of 15 RCT studying mild-to-
active cycle breathing, osteopathic moderate CAP found that therapy for 7 days or
fewer was as effective as longer therapy with
manipulation, and positive expira-
regard to clinical failure, mortality, adverse
tory pressure. No method reduced events, and bacteriologic eradication. The trials
28. Aujesky D, Auble TE,
mortality, whereas osteopathic compared only monotherapies, and 13 of the
Yealy DM, et al. Prospec- manipulation and positive expira- short-duration trials used azithromycin, uoro-
tive comparison of three
validated prediction rules tory pressure reduced the duration quinolones, or ketolides, which provide cover-
for prognosis in of hospital stay by 2.02 and 1.4 age for both pneumococcus and atypical
community-acquired
pneumonia. Am J Med. days, respectively (32). In the se- pathogens. Only 2 short-duration trials used
2005;118:384-92. verely ill ICU patient, nondrug -lactam monotherapy (33).
[PMID: 15808136]
29. Huang DT, Weissfeld LA, therapy can include noninvasive How should clinicians follow
Kellum JA, et al. Risk
ventilatory support and mechani-
prediction with procalci- patients during outpatient
tonin and clinical rules in cal ventilation for those with respi-
community-acquired treatment?
pneumonia. Ann Emerg ratory failure.
Med. 2008;52:48-58. Up to 10% of patients initially
[PMID: 18342993] Which antibiotics should be managed at home do not re-
30. Salih W, Schembri S,
Chalmers JD. Simplica- prescribed for outpatients? spond to outpatient therapy and
tion of the IDSA/ATS
criteria for severe CAP For patients with no cardiopul- require hospitalization. To iden-
using meta-analysis and monary disease and no factors tify these patients early, the phy-
observational data. Eur
Respir J 2014;43:842- that increase risk for infection sician and patient should agree
851. [PMID: 24114960]
31. Graham WG, Bradley DA.
with DRSP or enteric gram- on a plan to monitor the re-
Efcacy of chest physio- negative bacteria (Table), pre- sponse to therapy. Ask patients
therapy and intermittent
positive-pressure breath- scribe a macrolide (azithromycin, to measure their temperature
ing in the resolution of clarithromycin, or erythromycin) orally every 8 hours and to report
pneumonia. N Engl J
Med. 1978;299:624-7. or doxycycline (Appendix Table, if it exceeds 38.3 C (101 F) or
[PMID: 355879]
32. Yang M, Yan Y, Yin X,
available at www.annals.org). For does not decrease below 37.2 C
et al. Chest physiother- outpatients who have cardiopul- (99 F) after 48 hours. Encourage
apy for pneumonia in
adults. Cochrane Data- monary disease or factors that patients to drink at least 1 to 2
base Syst Rev. 2013 Feb
28;2:CD006338.
increase the risk for infection with quarts of liquid daily and to report
33. Li JZ, Winston LG, Moore DRSP or enteric gram-negative if they cannot achieve this goal.
DH, Bent S. Efcacy of
short-course antibiotic bacteria, prescribe an antipneu- Instruct patients to report symp-
regimens for mococcal quinolone (levooxacin toms of chest pain, severe or in-
community-acquired
pneumonia: a meta- or moxioxacin) or a combination creasing shortness of breath, or
analysis. Am J Med.
2007;120:783-90.
of a -lactam (amoxicillin, 3 g/d; lethargy. Encourage patients to
[PMID: 17765048] amoxicillin clavulanate, cefpo- take their antibiotics on schedule
2015 American College of Physicians ITC10 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
and to continue taking them even DRSP or gram-negative bacteria
after they begin feeling better and (20, 36), very few such patients
until they have taken all of them. are hospitalized, and this is not a
commonly used approach. Most 34. Meehan TP, Fine MJ,
If the response to therapy is satis- hospitalized patients not in the Krumholz HM, et al.
Quality of care, process,
factory, ask the patient to return ICU have cardiopulmonary dis- and outcomes in elderly
for an examination in 10 14 days. ease or factors that increase the
patients with pneumo-
nia. JAMA. 1997;278:
Give pneumococcal and inu- risk for DRSP or gram-negative 2080-4. [PMID:
9403422]
enza vaccinations at the outpa- bacteria, and they should receive 35. Kanwar M, Brar N,
tient visit if they have not previ- an intravenous or oral quinolone
Khatib R, Fakih MG.
Misdiagnosis of
ously been given. Obtain a (levooxacin, 750 mg/d, when community-acquired
repeated chest radiograph no renal function is normal, or moxi-
pneumonia and inappro-
priate utilization of anti-
sooner than 1 month after start- oxacin, 400 mg/d) or the combi- biotics: side effects of the
4-h antibiotic administra-
ing pneumonia therapy to screen nation of a -lactam (cefotaxime, tion rule. Chest. 2007;
for nonresolution of inltrates, ceftriaxone, ampicillinsulbac-
131:1865-9. [PMID:
17400668]
which could be due to lung can- tam, or high-dose ampicillin, but 36. Feldman RB, RhewDC,
cer, inammatory disease, or an Wong JY, et al. Azithro-
not cefuroxime) with a macrolide mycin monotherapy for
unusual infection (20). Assess the or doxycycline (20). The addition patients hospitalized
with community-
patient's overall health and look of a macrolide to a -lactam has acquired pneumonia: a
for decompensated comorbid been associated with reduced
31/2-year experience
from a veterans affairs
illness to attempt to prevent fu- mortality and hospital stay (37), hospital. Arch Intern
ture episodes of pneumonia. Med. 2003;163:1718-
even for bacteremic pneumococ- 26. [PMID: 12885688]
37. Martnez JA, Horcajada
When patients require cal pneumonia (37). In contrast, JP, Almela M, et al. Addi-
hospitalization, how soon after in a randomized trial of 580 tion of a macrolide to a
beta-lactam-based empir-
admission should antibiotics be immune-competent patients, ical antibiotic regimen is
started, and which antibiotics -lactam monotherapy was not associated with lower
in-hospital mortality for
inferior to a -lactammacrolide patients with bacteremic
should patients receive if they pneumococcal pneumo-
combination in patients with nia. Clin Infect Dis. 2003;
do not need ICU care?
moderately severe CAP. How- 36:389-95. [PMID:
Patients should receive initial an- ever, patients with atypical
12567294]
38. Garin N, Genne D, Car-
tibiotic therapy as soon as possi- pathogens and those in PSI class ballo S, et al. -Lactam
ble after the diagnosis is estab- monotherapy vs
IV had delayed clinical stability -lactam-macrolide
lished and before they leave the with -lactam monotherapy when
combination treatment
in moderately severe
emergency department. Al-
compared with those receiving community-acquired
though therapy within 4 hours of pneumonia: a random-
combination therapy (38). In an- ized noninferiority trial.
arrival to the hospital has been JAMA Intern Med 2014;
other trial of admitted patients 174:1894-1901. [PMID:
associated with reduced mortal-
with nonsevere CAP, -lactam 25286173]
ity in some studies, undue em- 39. Postma DF, van Werk-
monotherapy was equivalent to a hoven CH, van Elden LJ,
phasis on early therapy can lead
-lactammacrolide combination et al; CAP-START Study
to unnecessary use of antibiotics Group. Antibiotic treat-
for 30 day mortality (which was ment strategies for
and associated complications
<10%) (39). Specic -lactams, community-acquired
pneumonia in adults.
(11, 34). In 1 study, the nal diag-
such as ceftriaxone and cefo- N Engl J Med 2015;372:
nosis of pneumonia in patients 13121323.[PMID:
taxime, are preferred if DRSP is 25830421]
suspected of having pneumonia 40. Lujan M, Gallego M,
suspected because they are ef-
in the emergency department Fontanals D, Mariscal D,
fective at mean inhibitory con- Rello J. Prospective ob-
decreased from 75.9% to 58.9% servational study of bac-
centrations up to 2 mg/L (40). teremic pneumococcal
after the initiation of a program
However, 1 study showed in- pneumonia: Effect of
to give more patients antibiotics discordant therapy on
creased mortality when cefu- mortality. Crit Care Med.
within 4 hours of arrival in the 2004;32:625-31. [PMID:
roxime was used in patients with
emergency department (35). 15090938]
bacteremic DRSP (41). 41. International Pneumo-
coccal Study Group. An
Although guidelines recommend One international study of 4337 hospitalized international prospective
study of pneumococcal
that hospitalized patients who patients with CAP showed that approximately bacteremia: correlation
are not in the ICU receive intrave- 20% had evidence of atypical pathogen infec- with in vitro resistance,
antibiotics administered,
nous azithromycin if they have no tion and that therapy directed against these or- and clinical outcome.
cardiopulmonary disease and no Clin Infect Dis. 2003;37:
ganisms decreased the time to clinical stabil- 230-7. [PMID:
factors that increase the risk for ity, length of stay, and both total and CAP- 12856216]
6 October 2015 Annals of Internal Medicine In the Clinic ITC11 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
related mortality (42). However, another study olone effective against P.
of 2209 hospitalized Medicare patients with aeruginosa (ciprooxacin or high-
bacteremic pneumonia found that therapy di- dose levooxacin). Alternatively,
rected at atypical pathogens reduced 30-day treat patients with risk factors
mortality and 30-day readmission rate, but the with an intravenous, antipseudo-
benets occurred only with macrolides and not
monal -lactam combined with
42. Community-Acquired with uoroquinolones (43).
Pneumonia Organization an aminoglycoside (amikacin,
(CAPO) Investigators. A
worldwide perspective of For patients with HCAP admitted to gentamicin, or tobramycin) plus
atypical pathogens in the hospital but not the ICU, antibi- either an intravenous macrolide
community-acquired
pneumonia. Am J Respir otic choice should be individualized (azithromycin or erythromycin) or
Crit Care Med. 2007;
175:1086-93. [PMID:
based on risk factors for MDR patho- intravenous antipneumococcal
17332485] gens. A CAP regimen is effective for quinolone (levooxacin or moxi-
43. Metersky ML, Ma A,
Houck PM, Bratzler DW. most patients, but therapy directed oxacin). In studies of patients
Antibiotics for bacteremic at multidrug-resistant, gram- admitted to the ICU with severe
pneumonia: improved
outcomes with macro- negative bacteria and MRSA may be CAP, mortality was reduced
lides but not uoro- when combination therapy was
quinolones. Chest. 2007;
needed for patients with nonsevere
131:466-73. [PMID: pneumonia and at least 2 MDR risk used; monotherapy, even with a
17296649]
44. Sligl WI, Asadi L, Eurich factors (recent hospitalization, recent quinolone, was not as effective.
DT, et al. Macrolides and antibiotics, poor functional status,
mortality in critically ill A meta-analysis of 28 observational studies, involv-
patients with immune suppression) or severe
community-acquired ing nearly 10 000 critically ill patients found that
pneumonia: a systematic
pneumonia with at least 1 MDR risk macrolide use (generally in a combination regimen)
review and meta- factor. Therapy for HCAP in patients was associated with an 18% reduction in mortality
analysis. Crit Care Med
2014;42:420-432. at risk for MDR pathogens usually compared with nonmacrolide regimens and that a
[PMID:24158175] requires dual pseudomonal therapy
45. International Pneumo- -lactammacrolide combination had a trend to-
coccal Study Group. plus therapy directed at MRSA. ward reduced mortality compared with a -lactam
Combination antibiotic
therapy lowers mortality quinolone regimen (44). In patients with bacteremic
among severely ill pa- A prospective study of 321 HCAP patients showed pneumococcal pneumonia and critical illness, stud-
tients with pneumococcal that with the use of an algorithm, 93% received ap- ies have found that mortality was lower with combi-
bacteremia. Am J Respir
Crit Care Med. 2004;
propriate therapy, but this was achieved with only nation therapy than with monotherapy (45).
170:440-4. [PMID: 53% requiring broad-spectrum empirical therapy
15184200]
46. Micek ST, Dunne M,
(18). The algorithm stratied patients on the basis of If community-acquired MRSA is sus-
Kollef MH. Pleuropulmo- severity of illness (admission to the ICU or not) and pected, add either linezolid alone or
nary complications of
Panton-Valentine
the presence of other risk factors for MDR pathogens consider vancomycin combined
leukocidin-positive (recent antibiotic therapy, recent hospitalization, with clindamycin, because both of
community-acquired poor functional status, and immune suppression).
methicillin-resistant these regimens are antibacterial and
Staphylococcus aureus: Patients with nonsevere illness and at least 2 MDR
importance of treatment risk factors, or those with severe illness and at least 1
inhibit production of bacterial toxins.
with antimicrobials inhib-
MDR risk factor, were treated empirically with broad- Vancomycin alone is antibacterial
iting exotoxin produc-
tion. Chest. 2005;128: spectrum, multidrug therapy, whereas all others re- but cannot inhibit toxin production
2732-8. [PMID:
16236949] ceived CAP regimens. Through use of this approach, (46). These regimens are recom-
47. Salluh JI, Verdeal JC, mortality was 13.7%. mended, even though the organ-
Mello GW, et al. Cortisol
levels in patients with isms are often sensitive in vitro to
severe community- Which antibiotics should be given
trimethoprimsulfamethoxazole and
acquired pneumonia.
Intensive Care Med.
to patients admitted to the ICU? quinolones.
2006;32:595-8. [PMID: No patient in the ICU should re-
16552616] What are the other components
48. Salluh JI, Povoa P, ceive empirical monotherapy.
Soares M, et al. The role Assess these patients for risk fac- of ICU care for CAP?
of corticosteroids in se-
vere community- tors for P. aeruginosa. Treat those Hydration should be ensured and
acquired pneumonia: a
systematic review. Crit
without risk factors with intrave- supplemental oxygen and chest
Care. 2008;12:R76. nous ceftriaxone or cefotaxime physiotherapy should be consid-
[PMID: 18547407]
49. Torres A, Sibiila O, Ferrer plus either azithromycin or a ered. However, the main determina-
M, et al. Effect of cortico- quinolone, such as levooxacin tion is whether ventilatory support
steroids on treatment
failure among hospital- or moxioxacin. Treat patients for respiratory failure is needed. In-
ized patients with severe
community-acquired
who have risk factors with an in- tubation and mechanical ventilation
pneumonia and high travenous, antipseudomonal are required in patients who have
inammatory response:
a randomized clinical -lactam (cefepime, piperacillin oxygen saturation less than 90% on
trial.JAMA 2015;313: tazobactam, imipenem, mero- maximal mask oxygen, inability to
677-686. [PMID:
25688779] penem) plus an intravenous quin- clear secretions, inability to protect
2015 American College of Physicians ITC12 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
the airway, or hypercarbia. If the pa- can be made as early as 2448 nary consultation should be re-
tient has only hypoxemia or hyper- hours after admission and is made quested if pleural effusion is docu-
carbia and is alert and cooperative, by day 3 in up to half of all patients. mented and help is needed with a
it may be possible to use noninva- Changing to oral therapy can be decision regarding thoracentesis.
sive positive pressure ventilation. done safely even if pneumococcal Pulmonary or thoracic surgical con-
This therapy may be associated with bacteremia has been documented, sultation is appropriate for place-
fewer complications than endotra- although these patients may take ment of a chest tube if a compli-
cheal intubationincluding longer to respond. Longer durations cated parapneumonic effusion or
ventilator-associated pneumonia of therapy are usually needed for empyema is found on thoracente-
but if it is used, the clinician must patients infected with P. aeruginosa sis, because early therapy can re-
ensure that the patient can expecto- or S. aureus and for those with ex- duce hospital stay and avoid com-
rate any respiratory secretions. Con- trapulmonary complications, such as plications. A thoracic surgeon can
sider systemic corticosteroids, espe- empyema or meningitis, but should also perform surgical decortication
cially if relative adrenal insufciency be individualized to specic patient for advanced and loculated pleural
is suspected, or if a patient with situations. Select an oral regimen effusion and empyema. Cardiology
pneumococcal pneumonia has as- that covers all organisms isolated in consultation may be needed if
sociated meningitis. Routine use of blood or sputum cultures and re- complications of cardiac ischemia
systemic corticosteroids in severe ects the intravenous therapy. For arise or in cases of congestive heart
CAP is not recommended, but pa- some patients, this means a -lac- failure. In a study of 170 patients
tients with severe illness and high tammacrolide combination or quin- with pneumococcal pneumonia,
levels of systemic inammation may olone monotherapy. Patients who 19.4% had at least 1 major cardiac
benet from adjunctive systemic have responded to a -lactammac- event, including 12 with acute myo-
corticosteroids. Because many pa- rolide combination can be contin- cardial infarction, 8 with new-onset
tients with severe CAP also have ued on macrolide monotherapy atrial brillation or ventricular tachy-
systemic sepsis, consider aggressive unless cultures justify dual therapy. cardia, and 13 with newly diag-
hydration, vasopressors, and mea- nosed or worsening heart failure
surement of serum lactate. To facilitate a switch to oral therapy, hospitals should without other cardiac complica-
consider using a standing order set supplemented
tions. Patients with cardiac events
In 1 study of 40 patients with severe CAP when by prospective case management. In a cohort study,
each patient was managed in 3 successive periods
had a signicantly higher mortality
random serum cortisol levels were measured
in the rst 72 hours, 65% of patients met cri- with conventional therapy, a guideline-based order rate (27.3% vs. 8.8%) (51).
teria for adrenal insufciency and 63% of the set supported by prospective case management that When can inpatients be
19 patients with CAP and septic shock also had provided feedback to clinicians, and a guideline-
discharged from the hospital?
adrenal insufciency (47). In 4 studies, includ- based order set alone. Time to clinical stability was
ing randomized trials, evidence was inconsis- similar in all 3 periods, but prospective case man- Patients can be discharged once a
tent for a benet from routine corticosteroid agement led to the greatest reductions in the time to switch to oral therapy is made and
therapy; however, if the patient required corti- oral antibiotics, time from oral therapy to discharge, coexisting medical conditions are
costeroids for another reason (such as underly- and overall length of stay (50). under control. No benet for con-
ing COPD), they seemed to cause no harm tinued hospital observation has
(48). A multicenter RCT of severe CAP com- When should a consultation be
been proven. In 1 study, two thirds
pared 61 patients given 0.5 mg/kg methyl- requested for hospital patients, of clinically stable patients were
prednisolone every 12 hours for 5 days with and which types of specialists or observed while receiving oral ther-
59 patients given placebo. All patients had se- subspecialists should be apy before discharge, and no dete-
vere CAP and a C-reactive protein level greater consulted? rioration occurred during this pe-
than 150 mg/L on admission. The group
An infectious disease or pulmonary riod (52). Another study compared
treated with corticosteroids had less treatment
failure, with no difference in mortality (49). consultation is appropriate if there patients who remained in the hos-
are questions about the selection of pital for 1 day after the switch from
When can clinicians switch initial antibiotic therapy or when the intravenous to oral therapy with
hospitalized patients from patient does not respond to initial those discharged on the day of the
intravenous to oral antibiotics? therapy. A pulmonary or critical care switch. The study excluded patients
A switch from intravenous to oral physician should be consulted for with complicated pneumonia,
antibiotics is indicated once the patients with severe illness to decide those who were not eligible to be
symptoms of cough, sputum pro- about using vasopressors, deter- switched to oral therapy, and those
duction, and dyspnea improve; the mine the appropriate site of care, with lengths of stay less than 3 days
patient is afebrile on 2 occasions 8 decide about the need for ventila- or more than 7 days. There were no
hours apart; and he or she is able to tory support, and to aid in managing differences in mortality or 14-day
receive oral medications. This switch the mechanical ventilator. Pulmo- readmission rate (53). Therapy may
6 October 2015 Annals of Internal Medicine In the Clinic ITC13 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
need to be continued after dis- enza vaccinations; avoid smoking
charge, but the total duration of cigarettes; and receive optimal ther-
therapy is usually 57 days. apy for comorbid illnesses, such as
What are the indications for congestive heart failure and COPD.
In addition, careful evaluation is
follow-up chest radiography?
needed for medical conditions that
Patients hospitalized for pneumonia
could predispose to recurrent infec-
do not need a routine chest radio-
graph before discharge, but those tion. One study found new comor-
who do not reach clinical stability bid conditions in 6% of patients with
and those who deteriorate despite CAP, including diabetes mellitus,
therapy require an aggressive evalu- cancer, COPD, and HIV infection
50. Fishbane S, Niederman
MS, Daly C, et al. The ation, including an early follow-up (55). The patient should be evalu-
impact of standardized
chest radiograph. If the patient has a ated for aspiration risk factors. If
order sets and intensive
clinical case manage- good clinical response to therapy, a pneumonia recurs in the same loca-
ment on outcomes in
community-acquired chest radiograph should not be re- tion, consideration should be given
pneumonia. Arch Intern peated any earlier than 46 weeks to the possibility of bronchiectasis,
Med. 2007;167:1664-9.
[PMID: 17698690] after initial therapy. Radiographic aspirated foreign body, or endo-
51. Musher DM, Rueda AM,
Kaka AS, Mapara SM.
resolution usually lags behind clini- bronchial obstruction. If the patient
The association between cal resolution by about 68 weeks, has recurrent pneumonia or pneu-
pneumococcal pneumo-
nia and acute cardiac but early improvement is usually monia with an unusual pathogen,
events. Clin Infect Dis. substantial. In a prospective study of immune deciency may be present.
2007;45:158-65. [PMID:
17578773] patients aged 70 years or older,
52. Rhew DC, Hackner D,
58% had a clear chest radiograph The 30-day readmission rate for
Henderson L, Ellrodt AG,
Weingarten SR. The after 3 weeks, but it took 12 weeks CAP patients varied from 16.8%
clinical benet of in-
hospital observation in until at least 75% had radiographic 20.1% in a review of 12 studies
low-risk pneumonia resolution of CAP. Predictors of slow (56). Pneumonia itself was the
patients after conversion
from parenteral to oral resolution included a high comor- cause of readmission in only
antimicrobial therapy.
Chest. 1998;113:142-6.
bidity index, bacteremia, multilobar 17.9%29.4% of patients; how-
[PMID: 9440581] involvement, and infection with en- ever, other common causes were
53. Nathan RV, Rhew DC,
Murray C, et al. In- teric gram-negative bacteria (54). exacerbations of congestive
hospital observation after
antibiotic switch in pneu- How can patients prevent heart failure or COPD. Patients
monia: a national evalu-
ation. Am J Med. 2006; recurrent CAP? with HCAP have a higher risk for
119:512.e1-7. [PMID: readmission than patients with
16750965]
Patients with CAP should be up-to-
54. El Solh AA, Aquilina AT, date with pneumococcal and inu- CAP (57).
Gunen H, Ramadan F.
Radiographic resolution
of community-acquired
bacterial pneumonia in
the elderly. J Am Geriatr Treatment... The most important clinical decisions in the treatment of CAP
Soc. 2004;52:224-9.
[PMID: 14728631] include determining the site of care (outpatient, hospital, or ICU), selecting
55. Falguera M, Martn M, antibiotic therapy, delivering supportive care (oxygen, hydration), and deter-
Ruiz-Gonzalez A, Pifarre
R, Garca M. Community- mining the need for ventilatory support. Antibiotic therapy differs for outpa-
acquired pneumonia as tients, inpatients, and those in the ICU. However, all patients should receive
the initial manifestation timely empirical therapy directed at pneumococcus, atypical pathogens, and
of serious underlying
diseases. Am J Med. other organisms when they have risk factors for those organisms. The PSI and
2005;118:378-83. the CURB-65 aid decisions about the site of care. Patients should be managed
[PMID: 15808135]
56. Prescott HC, Sjoding in the ICU if they require ventilatory or vasopressor support or close observa-
MW, Iwashyna TJ. Diag- tion. Consultation should take place in cases of severe disease and when pa-
noses of early and late tients do not respond to initial therapy or have complications. Inpatients can
readmissions after hospi-
talization for pneumonia. be transitioned to oral antibiotics after treatment response occurs and they are
A systematic review. Ann clinically stable, after which the patient can be discharged and managed on an
Am Thor Soc. 2014;11:
1091-100. [PMID: outpatient basis. Routine follow-up chest radiography should be delayed for
25079245] 46 weeks if the patient is responding well to therapy. During follow-up, pa-
57. Shorr AF, Zilberberg MD, tients should be monitored for undiagnosed or ineffectively managed comor-
Reichley R, et al. Read-
mission following hospi- bid illness, up-to-date on pneumococcal and inuenza vaccinations, and en-
talization for pneumonia: couraged to avoid cigarette smoking.
the impact of pneumo-
nia type and its implica-
tion for hospitals. Clin
Infect Dis. 2013;57:362-
367. [PMID:23677872]
CLINICAL BOTTOM LINE
2015 American College of Physicians ITC14 In the Clinic Annals of Internal Medicine 6 October 2015
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
Practice Improvement
What measures of pneumonia January 2015, data collection on
care are regularly collected and these measures was suspended
publicly reported? because compliance was high
In the past, the Center for Medi- and continued monitoring and
public reporting were not be-
care & Medicaid Services (CMS)
lieved to be valuable. The quality
and the Joint Commission have
measures recommended by pro-
endorsed a set of core mea-
fessional organizations are being
sures for CAP, which focused on
reevaluated, as are the guide-
vaccination, smoking cessation, lines for the treatment of CAP.
antibiotic choice, timing of ther- The CMS will continue to monitor
apy, and doing blood cultures on all-cause mortality rates for pa-
critically ill patients before the tients with CAP, and they will
start of antibiotics. The perfor- monitor, and tie future reim-
mance of individual hospitals in bursement rates to, 30-day
achieving these measures had readmission rates for these
been publicly reported. As of 1 patients.
In the Clinic
Tool Kit
Patient Information
www.nlm.nih.gov/medlineplus/ency/article/000145
.htm
NIH MedLine Plus.
www.cdc.gov/pneumococcal/clinicians/diagnosis
-medical-mgmt.html
IntheClinic
Centers for Disease Control and Prevention.
http://familydoctor.org/familydoctor/en/diseases
-conditions/pneumonia.html
Community-Acquired http://umm.edu/health/medical/ency/articles
Pneumonia /pneumonia-adults-community-acquired
Patient resources in English.
http://umm.edu/health/medical/spanishency/articles
/neumonia-en-adultos-extrahospitalaria
Patient resources in Spanish.
Guidelines
https://www.thoracic.org/statements/resources/mtpi
/idsaats-cap.pdf
https://www.brit-thoracic.org.uk/guidelines-and
-quality-standards/community-acquired-pneumonia
-in-adults-guideline/
Medical guidelines for clinical practice for the diagnosis
and treatment of community-acquired pneumonia.
6 October 2015 Annals of Internal Medicine In the Clinic ITC15 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
WHAT YOU SHOULD In the Clinic
Annals of Internal Medicine
KNOW ABOUT
COMMUNITY-ACQUIRED
PNEUMONIA
What Is Pneumonia?
Pneumonia is a serious infection of the lungs.
Community-acquired pneumonia is a type of
pneumonia that you develop outside of a hospi-
tal or nursing home. It is most commonly caused
by bacteria, but viruses can also cause it. Risk
factors for pneumonia include:
Being 65 years or older
Eating a poor diet
Drinking alcohol
Smoking cigarettes
Having inuenza (the u)
Having a weakened immune system, such as
from old age or a serious disease, like HIV or
cancer
Having periods of time where you lost Drink lots of uids to make sure you stay hydrated.
consciousness, such as from anesthesia, Your doctor may prescribe medicines for
drinking too much, drug use, stroke, and cough and to reduce fever. Feeling tired and
seizure coughing may last for up to a month or longer
before going away.
What Are the Warning Signs of Most patients are treated at home, but some
Pneumonia? who are very ill or who have a greater risk for
complications may have to stay in the hospital.
Long-lasting cough, which can sometimes If you have to stay in the hospital, doctors will
bring up mucus monitor your heart and breathing rates,
Feeling cold and shaky oxygen levels, and temperature. You may also
Fever be given uids and medicines through your
Patient Information
Shortness of breath veins (intravenously).
Chest pains
Feeling tired and weak Questions for My Doctor
Am I contagious?
How Is Pneumonia Diagnosed? What can I do to help relieve my symptoms?
Your doctor will ask you questions about your Why do I still feel so tired?
symptoms and give you a physical How can I prevent another episode of
examination. He or she will listen to your lungs pneumonia?
and heart and check your temperature. Should I be treated at home or in the hospital?
Your doctor will usually order a chest X-ray to When can I start my normal activities again?
see how much your lungs are affected. When can I go back to work?
Your doctor may also order tests of the sputum
(mucous brought up with coughing) and urine to Bottom Line
learn what type of bacteria is causing the Pneumonia is a serious infection of the lungs.
pneumonia. A blood test can show if the infection It is most commonly caused by bacteria.
has spread from the lungs to the blood. Symptoms include shortness of breath,
coughing, chest pains, high fever, and feeling
How Is Pneumonia Treated? cold and shaky.
If your pneumonia is caused by bacteria, your Treatment usually includes antibiotic
doctor will prescribe antibiotics. Your medicines, medicines for cough and fever,
symptoms usually start to go away within a few drinking lots of uids, and rest.
days of starting treatment. It is important to Some people may need to stay in the hospital
nish all of your antibiotics, even if you are if the infection is more serious or if pneumonia
feeling better. does not go away.
For More Information
Medline Plus
www.nlm.nih.gov/medlineplus/ency/article/000145.htm
American Lung Association
www.lung.org/lung-disease/pneumonia/symptoms-diagnosisand
.html
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
Appendix Table. Drug Treatment for Community-Acquired Pneumonia
Agent Mechanism of Action Dosage Benets Side Effects Notes
Antibiotics for Bacteriostatic; binds 600 mg PO or IV q12h Penetrates well into the Myelosuppression Drug interactions may lead
community-acquired to 50 S ribosomal lung and is active particularly to serotonin syndrome.
MRSA subunit to inhibit against MRSA thrombocytopenia, Do not use with tricyclic
Linezolid (Zyvox) bacterial protein vomiting, diarrhea, antidepressants,
synthesis seizures, hypoglycemia monoamine oxidase
inhibitors, or selective
serotonin reuptake
inhibitors. Monitor
blood pressure
Clindamycin* (Cleocin) Bacteriostatic; binds 600 mg PO q8h Can inhibit toxin Diarrhea, esophagitis, Can cause Clostridium
to 50 S ribosomal production by MRSA hypersensitivity difcileassociated
subunit to inhibit diarrhea. Caution with
bacterial protein asthma, severe hepatic
synthesis disease
Vancomycin (Vancocin) Bactericidal; inhibits 1520 mg/kg IV q812h Active against MRSA, Ototoxicity, nephrotoxicity, Avoid rapid infusion
cell wall and RNA with extensive clinical neutropenia, nausea, (causes histamine
synthesis experience. Is not hypokalemia release). Avoid
optimal therapy for extravasation. Monitor
methicillin-susceptible trough concentrations.
Staphylococcus aureus In chronic kidney
disease, individualize
dose
Antipseudomonal Bactericidal, interferes Piperacillin/tazobactam, Active against Anaphylaxis, rash, nausea, Only use for patients with
-lactams with peptidoglycan 3.375 mg q46h IV. pneumococci and vomiting, diarrhea, pseudomonal risk
Piperacillin/tazobactam cross-linking, and Cefepime, 12 g q12h IV Pseudomonas phlebitis, seizures (high factors, although
Cefepime prevents formation Imipenem, 1 g q8h IV aeruginosa doses), hypokalemia (high generally active against
Imipenem of the bacterial cell Meropenem, 1 g q8h IV doses), elevated liver tests, DRSP. Can dose daily if
Meropenem wall prolonged prothrombin patient has renal
time (especially if on insufciency
coumadin). Seizure
potential greater with
imipenem than
meropenem
Cephalosporins Bactericidal, interferes Cefuroxime, 500 mg bid PO. Active against Anaphylaxis, rash, nausea, Not to be used alone in
Cefuroxime with peptidoglycan Cefpodoxime, 400 mg bid pneumococci and vomiting, diarrhea, CAP. Combine with a
Cefpodoxime cross-linking, and PO. Ceftriaxone, 12 g Haemophilus elevated liver function test macrolide. Although
Ceftriaxone prevents formation q1224h (usually q24h). inuenzae, including results, interstitial cefuroxime can be used
Cefotaxime of the bacterial cell Cefotaxime, 1 g q8h -lactamase- nephritis, altered as oral therapy, it
wall producing organisms coagulation, should not be used IV,
pseudomembranous because it is not as
colitis active against DRSP as
other cephalosporins
Glycylcycline Bacteriostatic; binds 100 mg IV initially, then 50 mg IV Can be used for CAP, but Vomiting, diarrhea, Avoid with pregnancy.
Tigecycline* (Tygacil) to 30 S ribosomal q12 h. Infuse over 3060 min use only when there hepatotoxicity, With severe hepatic
subunit to inhibit are no other options. pancreatitis, anemia. disease, use 25 mg for
bacterial protein Penetrates well into Increase in all-cause maintenance infusion
synthesis respiratory secretions; mortality
active against
pneumococcus and
atypical pathogens,
but not P. aeruginosa
Macrolides Bacteriostatic, binds Azithromycin, 500 mg on day 1 Covers pneumococcus, Nausea, vomiting, diarrhea, Use as monotherapy only
Azithromycin to the 50S (IV or PO), followed by 500 atypical pathogens, QT prolongation, in patients without
Clarithromycin ribosomal subunit, mg (IV or PO) for 710 days and H. inuenzae dyspepsia (clarithromycin) cardiopulmonary
and inhibits for hospitalized patients. 250 disease or modifying
bacterial protein mg on days 25 for factors. Otherwise,
synthesis outpatients. Azithromycin in combine with a
the microspheres oral -lactam agent.
extended-release formulation, Erythromycin is less
2 g on day 1 (PO) without expensive but not
follow-up dosing for recommended because
outpatients. Clarithromycin, of the need for more
500 mg bid PO, or 1000 mg/d frequent dosing, more
PO (extended-release intestinal upset, and no
preparation) for outpatients coverage of H.
inuenzae
Penicillins Bactericidal, interferes Amoxicillin/clavulanate, 875 mg Active against Anaphylaxis, rash, nausea, Do not use alone in CAP.
Amoxicillin/clavulanate with peptidoglycan bid PO. Ampicillin, 5001000 pneumococci and vomiting, diarrhea, Combine with a
Ampicillin cross-linking, and mg tid PO. Ampicillin/ -lactamase- phlebitis, seizures (high macrolide
Ampicillin/sulbactam prevents formation sulbactam, 12 g q6h IV producing H. doses), hypokalemia (high
of the bacterial cell inuenzae. High doses doses), elevated liver tests,
wall (1 g tid) active against prolonged prothrombin
DRSP time (especially if on
coumadin)
Quinolones Bactericidal, interferes Ciprooxacin, 400 mg q8h IV. Active against P. Seizures, hypersensitivity, Ciprooxacin: Only use in
Ciprooxacin with bacterial DNA Gemioxacin, 320 mg/d (PO aeruginosa, atypicals photosensitivity, tendon severe CAP. Not always
Levooxacin gyrase. Kills only). Levooxacin, 500-750 and H. inuenzae. rupture, nausea, vomiting, reliable against
Moxioxacin bacteria in a mg/d (IV or PO). Moxioxacin, Levooxacin and diarrhea, QT prolongation pneumococci, and
concentration- 400 mg/d (IV or PO) moxioxacin are the should be combined
dependent fashion respiratory with other agents if
quinolones with DRSP is possible. If used
activity against DRSP, in severe CAP, do not
H. inuenzae, and use as monotherapy
atypical pathogens
Tetracyclines: Bacteriostatic, binds 100 mg bid (IV or PO) Active against key Nausea, vomiting, diarrhea, Not always fully reliable
Doxycycline to 30 S ribosomal bacterial and atypical photosensitivity against pneumococci
subunit, and pathogens
interferes with
bacterial protein
synthesis
bid = twice daily; CAP = community-acquired pneumonia; DNA = deoxyribonucleic acid; DRSP = drug-resistant Streptococcus
pneumonia; FDA = U.S. Food and Drug Administration; IV = intravenous; MIC = minimum inhibitory concentration; MRSA =
methicillin-resistant Staphylococcus aureus; PO = oral; tid = three times daily.
* Black box warning.
6 October 2015 Annals of Internal Medicine In the Clinic 2015 American College of Physicians
Downloaded From: http://annals.org/ by a University of York User on 11/21/2016
Вам также может понравиться
- Spotting Signs of AutismДокумент23 страницыSpotting Signs of AutismAutism Parenting100% (3)
- VA Office of Inspector GeneralДокумент46 страницVA Office of Inspector Generalryan turbevilleОценок пока нет
- COPD (Chronic Obstructive Pulmonary Disease)Документ8 страницCOPD (Chronic Obstructive Pulmonary Disease)Emily Anne86% (7)
- E Learning Geriatric Oncology An IntroductionДокумент65 страницE Learning Geriatric Oncology An IntroductionHarold JeffersonОценок пока нет
- Cabg Vs OpcabДокумент17 страницCabg Vs OpcabVijay AnandОценок пока нет
- Handbook of Anticancer Pharmacokinetics and Pharmacodynamics 2004Документ623 страницыHandbook of Anticancer Pharmacokinetics and Pharmacodynamics 2004Harsh KoshtiОценок пока нет
- Hand Hygiene in Dental Health-Care SettingsДокумент55 страницHand Hygiene in Dental Health-Care SettingsManu DewanОценок пока нет
- Acls GuidelineДокумент10 страницAcls GuidelineReynaldoBinsarОценок пока нет
- MayoclinprocДокумент12 страницMayoclinprocpriyaОценок пока нет
- FULL-TEXT - NCLEX-RN Practice Quiz Test Bank 3 - NurseslabsДокумент91 страницаFULL-TEXT - NCLEX-RN Practice Quiz Test Bank 3 - NurseslabsRonaldo Matos Perez100% (1)
- Vasopressors and Inotropes in ShockДокумент8 страницVasopressors and Inotropes in ShockRiska PashaОценок пока нет
- Pulmonary HTNДокумент51 страницаPulmonary HTNMuhammad HaekalОценок пока нет
- Beta BlockersДокумент70 страницBeta BlockersIrina Cabac-PogoreviciОценок пока нет
- PneumoniaДокумент38 страницPneumoniaAzhar GhoriОценок пока нет
- Renal Dosing Protocol - Renal Dosing ProtocolДокумент3 страницыRenal Dosing Protocol - Renal Dosing Protocoldjwa163Оценок пока нет
- Severe Lactic Acidosis During Cardiac SurgeryДокумент9 страницSevere Lactic Acidosis During Cardiac SurgeryMarta Quiroz SotoОценок пока нет
- Community Acquired PneumoniaДокумент5 страницCommunity Acquired PneumoniaJerrica Charlene GalopeОценок пока нет
- PATHO Glomerular and Tubulointerstitial DiseaseДокумент43 страницыPATHO Glomerular and Tubulointerstitial DiseaseHananya ManroeОценок пока нет
- HANDOUTS-Non Invasive VentilationДокумент15 страницHANDOUTS-Non Invasive VentilationKristine MangasepОценок пока нет
- Daniel A Lichtenstein US PrincipalДокумент25 страницDaniel A Lichtenstein US PrincipalEvans AzandeОценок пока нет
- Blood ConservationДокумент7 страницBlood ConservationbobbykrishОценок пока нет
- Necrotizing PneumoniaДокумент7 страницNecrotizing PneumoniaMahdalenaSyahОценок пока нет
- Acute Kidney InjuryДокумент15 страницAcute Kidney InjuryManish VijayОценок пока нет
- Drug Study - Vitamin B ComplexДокумент1 страницаDrug Study - Vitamin B ComplexmikErlh0% (1)
- Antifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesДокумент18 страницAntifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesgopscharanОценок пока нет
- BLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllДокумент12 страницBLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllChristiaan CordovaОценок пока нет
- Sepsis WhoДокумент36 страницSepsis WholcycrlnОценок пока нет
- DISCHARGE PLANNING - AnemiaДокумент2 страницыDISCHARGE PLANNING - AnemiaJOEY MEAD ARUGAY0% (1)
- Refractory Septic ShockДокумент5 страницRefractory Septic ShockBrian Antonio Veramatos LopezОценок пока нет
- Stress Ulcer Prophylaxis GuidelinesДокумент4 страницыStress Ulcer Prophylaxis GuidelinesAzi Rifki NasutionОценок пока нет
- 7 Adverse Reactions ToДокумент11 страниц7 Adverse Reactions TodrkamalakarОценок пока нет
- Clinical Applications of Induced Hypothermia: Mark Luscombe John C AndrzejowskiДокумент5 страницClinical Applications of Induced Hypothermia: Mark Luscombe John C AndrzejowskiSajid NadafОценок пока нет
- ELSO Guidelines General All ECLS Version1.1 PDFДокумент24 страницыELSO Guidelines General All ECLS Version1.1 PDFBranka KurtovicОценок пока нет
- Brain Death Testing Protocol (Rev220605) PDFДокумент2 страницыBrain Death Testing Protocol (Rev220605) PDFRei Irinco100% (1)
- Hemodialysis Emergencies: Core Curriculum 2021.Документ14 страницHemodialysis Emergencies: Core Curriculum 2021.Tariq ZayanОценок пока нет
- KodingДокумент12 страницKodingAva Vav100% (1)
- Powell 2022 Oi 221002 1664506604.73378Документ12 страницPowell 2022 Oi 221002 1664506604.73378AntoineОценок пока нет
- Spirometry E-Guide 2013Документ28 страницSpirometry E-Guide 2013Vidal Odon Ramos MermaОценок пока нет
- Renal - Replacement - TherapyДокумент128 страницRenal - Replacement - TherapyEmОценок пока нет
- 2 - 5201750207762531221 EntДокумент561 страница2 - 5201750207762531221 EntArun Raj100% (1)
- Miller's Anesthesia, 8th Edition: Anesthesiology April 2016Документ3 страницыMiller's Anesthesia, 8th Edition: Anesthesiology April 2016Sabbir AhammedОценок пока нет
- 10 12 16 Journal Club ExampleДокумент52 страницы10 12 16 Journal Club ExampleSandra BaiОценок пока нет
- APICON 2019 Brochure PDFДокумент24 страницыAPICON 2019 Brochure PDFrasakatla jaswanthОценок пока нет
- 2015 Chest - Blue & Falls ProtocolsДокумент12 страниц2015 Chest - Blue & Falls ProtocolsWilmer Yanquen VillarrealОценок пока нет
- Supportive & Preventive Medicine PDFДокумент29 страницSupportive & Preventive Medicine PDFhuong L100% (1)
- Seizures in Children JULIO 2020Документ29 страницSeizures in Children JULIO 2020Elizabeth HendersonОценок пока нет
- Guidelines For Platelet Transfusions in Dengue FeverДокумент4 страницыGuidelines For Platelet Transfusions in Dengue FeverGuru Prasad100% (1)
- Clinical Cheat Sheet: Radiographic AssessmentДокумент1 страницаClinical Cheat Sheet: Radiographic AssessmentTracy PopeОценок пока нет
- Etika Hub DR - PasienДокумент23 страницыEtika Hub DR - PasienyonetsaniОценок пока нет
- Renal Replacement Therapy in Acute Kidney Injury 2017Документ14 страницRenal Replacement Therapy in Acute Kidney Injury 2017piero reyes100% (1)
- TEMPLATE Clinical Reasoning Case Study2Документ10 страницTEMPLATE Clinical Reasoning Case Study2Ianne MerhОценок пока нет
- Evaluation of Headache in AdultsДокумент21 страницаEvaluation of Headache in AdultsMaicon RamosОценок пока нет
- Viral Hepatitis PDFДокумент4 страницыViral Hepatitis PDFNina BracyОценок пока нет
- Continuous Renal Replacement Therapy - Who, When, Why, and HowДокумент13 страницContinuous Renal Replacement Therapy - Who, When, Why, and HowLee Foo WengОценок пока нет
- 18 Consultative HematologyДокумент40 страниц18 Consultative HematologyJose Luis Gutierrez RamirezОценок пока нет
- Use of Vasopressors and InotropesДокумент14 страницUse of Vasopressors and InotropesEdwin VargasОценок пока нет
- Approach To Septic ShockДокумент16 страницApproach To Septic ShockRaja EllysyaОценок пока нет
- Fluid and Hyponatremia Management: by Craig B. Whitman, Pharm.D., BCPS, BCCCPДокумент16 страницFluid and Hyponatremia Management: by Craig B. Whitman, Pharm.D., BCPS, BCCCPAleksandar Dimovski100% (1)
- Scape Vs FospeДокумент5 страницScape Vs FospeDr. FarhanОценок пока нет
- Ventilators Global Market - Forecast To 2027Документ5 страницVentilators Global Market - Forecast To 2027VinayОценок пока нет
- Blood Transfusion Therapy DefinitionДокумент27 страницBlood Transfusion Therapy DefinitionEvangelin MelvinОценок пока нет
- Predanalitika KoagulacijaДокумент10 страницPredanalitika KoagulacijaAnonymous w4qodCJОценок пока нет
- ACCP Standards of PracticeДокумент4 страницыACCP Standards of Practiceryuurecca0% (1)
- Acute Medicine BlueprintДокумент1 страницаAcute Medicine BlueprintKo KhiОценок пока нет
- Kidney TransplantДокумент11 страницKidney TransplantPrincess Xzmae RamirezОценок пока нет
- NatureDP 2020 DeliriumДокумент26 страницNatureDP 2020 DeliriumPaloma GBОценок пока нет
- Vascular Responses to PathogensОт EverandVascular Responses to PathogensFelicity N.E. GavinsОценок пока нет
- Carpal Tunnel Syndrome and WorkДокумент5 страницCarpal Tunnel Syndrome and WorkDaniel Puentes SánchezОценок пока нет
- Theoretical Aspects of Goal SettingДокумент8 страницTheoretical Aspects of Goal SettingDaniel Puentes SánchezОценок пока нет
- Design and Analysis of Heavily Loaded Reinforced Concrete Link Beams For Burj DubaiДокумент10 страницDesign and Analysis of Heavily Loaded Reinforced Concrete Link Beams For Burj DubaiJoão Rocha de Lima100% (1)
- Design and Analysis of Heavily Loaded Reinforced Concrete Link Beams For Burj DubaiДокумент10 страницDesign and Analysis of Heavily Loaded Reinforced Concrete Link Beams For Burj DubaiJoão Rocha de Lima100% (1)
- Guardian - Dental PPO Plan Summary 2022Документ4 страницыGuardian - Dental PPO Plan Summary 2022Jessi ChallagullaОценок пока нет
- Seftarolin, Antibiotik Baru Dengan Aktivitas Anti-MRSA: Sebuah Kajian Efektivitas, Keamanan, Dan Biaya PenggunaanДокумент21 страницаSeftarolin, Antibiotik Baru Dengan Aktivitas Anti-MRSA: Sebuah Kajian Efektivitas, Keamanan, Dan Biaya PenggunaanDhanang Prawira NugrahaОценок пока нет
- Lab Policies Alkaline Phosphatase C311 Lab 8803Документ4 страницыLab Policies Alkaline Phosphatase C311 Lab 8803Valdez Francis ZaccheauОценок пока нет
- Opioid-Free AnesthesiaДокумент8 страницOpioid-Free AnesthesiaPaulina LugoОценок пока нет
- VDL Biopsy SubmissionДокумент26 страницVDL Biopsy SubmissionThomas Karl Anthony QUILANGОценок пока нет
- Program Studi Pendidikan Spesialis Ilmu Penyakit Dalam: Fakultas Kedokteran Universitas BrawijayaДокумент4 страницыProgram Studi Pendidikan Spesialis Ilmu Penyakit Dalam: Fakultas Kedokteran Universitas BrawijayaHelsa EldatarinaОценок пока нет
- CVA Impaired Physical MobilityДокумент2 страницыCVA Impaired Physical MobilitycessyanneОценок пока нет
- Uji Karsinogenik & MutagenikДокумент23 страницыUji Karsinogenik & MutagenikMariadi CaniagoОценок пока нет
- Ghai 10ed CompetenciesДокумент15 страницGhai 10ed Competenciesghimansi50Оценок пока нет
- Streptococci and Enterococci and OthersДокумент11 страницStreptococci and Enterococci and OthersthedarkwingОценок пока нет
- CH 5 Providing Psychosocial CareДокумент79 страницCH 5 Providing Psychosocial CareKevin FacunОценок пока нет
- PulpotecДокумент5 страницPulpotecRuel MarmolejoОценок пока нет
- Jama Naggie 2023 Oi 230017 1676655303.18801Документ10 страницJama Naggie 2023 Oi 230017 1676655303.18801Mahmoud AbouelsoudОценок пока нет
- NehaДокумент91 страницаNehaPawan MeenaОценок пока нет
- The Use of Vancomycin With Its Therapeutic and Adverse Effects: A ReviewДокумент11 страницThe Use of Vancomycin With Its Therapeutic and Adverse Effects: A Reviewdea yuniarОценок пока нет
- HiperkolesterolДокумент60 страницHiperkolesterolAnonymous 1jCVqQuОценок пока нет
- Specification Points - 4.3.1.8 Antibiotics and PainkillersДокумент11 страницSpecification Points - 4.3.1.8 Antibiotics and PainkillersMahi NigamОценок пока нет
- Manual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-CoptДокумент80 страницManual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-Coptayesha solОценок пока нет
- TRS 987Документ286 страницTRS 987NGOTTAОценок пока нет
- Textbook ReadingДокумент275 страницTextbook ReadingNovitasari EkaОценок пока нет