Академический Документы
Профессиональный Документы
Культура Документы
Table 1. Indications For Initiating and Switching Nonbiologic and Biologic Dmards Disease Activity Recommendation
Загружено:
Regina ArningsariОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Table 1. Indications For Initiating and Switching Nonbiologic and Biologic Dmards Disease Activity Recommendation
Загружено:
Regina ArningsariАвторское право:
Доступные форматы
Table 1.
Indications for Initiating and Switching Nonbiologic and Biologic DMARDs
Disease Activity Recommendation
Early RA (< 6 mo) Administer DMARD combination therapy (eg, double or triple
therapy) in those with moderate or high disease activity and poor
prognostic features (functional limitation, extra-articular disease,
positive RF or anti-CCP antibodies, bony erosions on x-ray)
Use an anti-TNF agent MTX in those with high disease activity and
poor prognostic featuresexcept for infliximab, which is used in
combination with MTX only (ie, do not use infliximab as
monotherapy)
Established RA (=6 mo or meets Initiating and switching among nonbiologic DMARDs
1987 ACR RA classification criteria)
In patients without prognostic features who deteriorate after 3 mo of
If prognosis is not mentioned, DMARD monotherapy from low to moderate/high disease activity, add
use or switch to a nonbiologic MTX, hydroxycholoroquine, or leflunomide
or biologic DMARD regardless In patients with persistent moderate/high disease activity after 3 mo of
of prognostic features MTX or MTX-DMARD combination therapy, either add or switch to
another non-MTX DMARD
Switching from nonbiologic to biologic DMARDs
Alternatively, in patients with persistent moderate/high disease activity
after 3 mo of MTX monotherapy or MTX-DMARD combination
therapy, add or switch to an anti-TNF biologic agent, abatacept, or
rituximab
In patients with persistent moderate/high disease activity after 3 mo of
intensified DMARD combination therapy or after a second DMARD,
add or switch to an anti-TNF biologic agent
Switching among biologic agents because of lack or loss of benefit
In patients with persistent moderate/high disease activity after 3 mo of
anti-TNF biologic therapy because of lack or loss of treatment benefit,
switch to another anti-TNF biologic agent or a non-TNF biologic agent
In patients with persistent moderate/high disease activity after 6 mo of
non-TNF biologic therapy because of lack or loss of treatment benefit,
switch to another non-TNF biologic agent or an anti-TNF biologic
agent
Switching among biologic agents because of adverse effects
In patients with high disease activity after failure of anti-TNF biologic
therapy because of a serious adverse event, switch to a non-TNF
biologic agent
In patients with moderate or high disease activity after failure of anti-
TNF biologic therapy because of a nonserious adverse event, switch to
another anti-TNF biologic agent or a non-TNF biologic agent
In patients with moderate or high disease activity after failure of non-
TNF biologic therapy because of either a serious or a nonserious
adverse event, switch to another non-TNF biologic agent or an anti-
TNF biologic agent
ACR = American College of Rheumatology; CCP = cyclic citrullinated peptide; DMARD = disease-modifying
antirheumatic drug; MTX = methotrexate; RA = rheumatoid arthritis; RF = rheumatoid factor; TNF = tumor
necrosis factor.
Source: Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American College of Rheumatology
recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of
rheumatoid arthritis. Arthritis Care Res (Hoboken). 2012 May;64(5):625-39.
Table 2. 2012 ACR Recommendations for Further Evaluation After Initial/Repeat TB Screening
Results
Result of
Initial/Repeat TST Recommendation
or IGRA
Positive Obtain chest x-ray
If the chest x-ray is suspicious for active TB, obtain sputum examination for active
disease
Negative In patients with RA but without risk factors or clinical suspicion for TB
No further workup is needed
In patients with RA and immunosuppression plus LTBI risk factors
LBTI is not excluded
Repeat the TST or IGRA 1-3 wk after an initial negative test result
Active/latent TB Treat with appropriate antitubercular therapy
Refer to a specialist as necessary
Initiate or resume biologic agents after either 1 mo of treatment of LTBI with
antitubercular regimen or completion of treatment for active TB
Screen annually in individuals with RA who (1) are continuing on biologic agents while
living, traveling, or working in situations of likely TB exposure and (2) have a positive
baseline for TST or IGRA; TST or IGRA may still be positive after successful TB
therapy; monitor for clinical signs or symptoms of recurrent TB
ACR = American College of Rheumatology; IGRA = interferon gamma release assay; LBTI = latent tuberculosis
infection; RA = rheumatoid arthritis; TB = tuberculosis; TST = tuberculin skin test.
Source: Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American College of Rheumatology
recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of
rheumatoid arthritis. Arthritis Care Res (Hoboken). 2012 May;64(5):625-39.[67]
Вам также может понравиться
- Frontiers in Clinical Drug Research - Anti-Cancer Agents: Volume 5От EverandFrontiers in Clinical Drug Research - Anti-Cancer Agents: Volume 5Оценок пока нет
- CPG Rheumatic ArthritisДокумент15 страницCPG Rheumatic ArthritisCece PaduaОценок пока нет
- Handbook of Drug Interaction and the Mechanism of InteractionОт EverandHandbook of Drug Interaction and the Mechanism of InteractionРейтинг: 1 из 5 звезд1/5 (1)
- Siemens Healthineers N Latex aTNFa AssayДокумент8 страницSiemens Healthineers N Latex aTNFa AssayMatej NekićОценок пока нет
- SP - Management of MDR-TBДокумент6 страницSP - Management of MDR-TBvikaОценок пока нет
- Mdrtuberculosis DR GyanДокумент64 страницыMdrtuberculosis DR GyanSanket AgrawalОценок пока нет
- Dosing and Administration Guide: IndicationДокумент12 страницDosing and Administration Guide: IndicationenggajbОценок пока нет
- Tofacitinib For Psoriatic Arthritis in Patients With An Inadequate Response To TNF InhibitorsДокумент12 страницTofacitinib For Psoriatic Arthritis in Patients With An Inadequate Response To TNF InhibitorsPutri YunandaОценок пока нет
- TB Case PresДокумент5 страницTB Case PresAlwina May Parojinog BarlisanОценок пока нет
- Chapter Four: Treatment of Tuberculosis Disease: A. General Principles of TB TherapyДокумент14 страницChapter Four: Treatment of Tuberculosis Disease: A. General Principles of TB TherapyErick Kristianto LimasОценок пока нет
- Aieop-Bfm All 2017: Author: Julia Dobke, Janina Heilmann, Erstellt Am 2018/09/05, Last Modification: 2021/08/25Документ5 страницAieop-Bfm All 2017: Author: Julia Dobke, Janina Heilmann, Erstellt Am 2018/09/05, Last Modification: 2021/08/25Mihu Dragostin0% (1)
- Antituberculous Drugs - An Overview - UpToDateДокумент21 страницаAntituberculous Drugs - An Overview - UpToDateBryan Tam ArevaloОценок пока нет
- New Drugs and Regimens for TB: 2015 UpdateДокумент21 страницаNew Drugs and Regimens for TB: 2015 UpdateNop PiromОценок пока нет
- Intermittent RifampicinДокумент18 страницIntermittent RifampicinRhea DerijeОценок пока нет
- Kanamycin (Mode of Administration)Документ3 страницыKanamycin (Mode of Administration)Waseem MaroofiОценок пока нет
- Tuberculosis Treatment GuideДокумент30 страницTuberculosis Treatment GuideIbrahim JeldiОценок пока нет
- Alemtuzumab 12 MG-1.2 ML (Lemtrada Solution For Infusion)Документ22 страницыAlemtuzumab 12 MG-1.2 ML (Lemtrada Solution For Infusion)asdwasdОценок пока нет
- British Rheumatology Biologic Safety GuidelinesДокумент38 страницBritish Rheumatology Biologic Safety GuidelinesNathania Nadia BudimanОценок пока нет
- Rational Drug UseДокумент37 страницRational Drug UseTushar BahetiОценок пока нет
- Understanding Drug-Resistant TBДокумент18 страницUnderstanding Drug-Resistant TBMohammed HammedОценок пока нет
- Clinical Neurology and Neurosurgery: Erica Braun, Francesca M. Gualano, Prabha Siddarth, Eric SegalДокумент4 страницыClinical Neurology and Neurosurgery: Erica Braun, Francesca M. Gualano, Prabha Siddarth, Eric SegalNicolas LondoñoОценок пока нет
- Adverse Effects of Anti Tubercular Drugs. MDR TBДокумент75 страницAdverse Effects of Anti Tubercular Drugs. MDR TBDr.U.P.Rathnakar.MD.DIH.PGDHM100% (1)
- 3.0 Drug ResistanceДокумент18 страниц3.0 Drug ResistanceRey AlwiwikhОценок пока нет
- Research Article: The Effect of Prednisone On Tuberculin Skin Test Reaction in Patients With Rheumatoid ArthritisДокумент6 страницResearch Article: The Effect of Prednisone On Tuberculin Skin Test Reaction in Patients With Rheumatoid ArthritisWidya Ibunda DdffОценок пока нет
- Xeljanz Initiation ChecklistДокумент8 страницXeljanz Initiation ChecklistRawan ZayedОценок пока нет
- MyelomaДокумент25 страницMyelomasquallОценок пока нет
- Fingolimoid - 2014Документ9 страницFingolimoid - 2014rodicasept1967Оценок пока нет
- Choice of AMAs and Combined Use of AMAsДокумент23 страницыChoice of AMAs and Combined Use of AMAsJagirОценок пока нет
- mdm230 PDFДокумент3 страницыmdm230 PDFDanus RamadanusОценок пока нет
- Roger Case Study and Nursing Process 2Документ9 страницRoger Case Study and Nursing Process 2E.R.OОценок пока нет
- NRG Gy023Документ7 страницNRG Gy023Yagami SinОценок пока нет
- Epidemiology: Isoniazid (INH) Rifampicin (RMP) First-LineДокумент14 страницEpidemiology: Isoniazid (INH) Rifampicin (RMP) First-LineEttedab Abrogar ChavezОценок пока нет
- Presented By: Hazel Tiam Wat-Ututalum WMSU, College of NursingДокумент12 страницPresented By: Hazel Tiam Wat-Ututalum WMSU, College of NursingYasyas Tiamwat UtutalumОценок пока нет
- 47 Antimycobacterial DrugsДокумент77 страниц47 Antimycobacterial DrugsKriziaoumo P. OrpiaОценок пока нет
- Primary Nonresponse and Secondary Loss of Response For The Treatment With Anti TNFДокумент21 страницаPrimary Nonresponse and Secondary Loss of Response For The Treatment With Anti TNFiman naОценок пока нет
- Prior Authorization Conditions For Approval of Humira® (Adalimumab)Документ4 страницыPrior Authorization Conditions For Approval of Humira® (Adalimumab)Mitul PatelОценок пока нет
- DR Zuhair Sabbagh - Biologics in Rheumatoid Arthritis - Medics Index MemberДокумент7 страницDR Zuhair Sabbagh - Biologics in Rheumatoid Arthritis - Medics Index MemberMedicsindex Telepin Slidecase100% (2)
- SP Farmakologi TBДокумент5 страницSP Farmakologi TBvikaОценок пока нет
- Tuberculosis Treatment, MDR, XDR, Resistance, Prophylaxis, VaccinationДокумент44 страницыTuberculosis Treatment, MDR, XDR, Resistance, Prophylaxis, Vaccinationskeisham11Оценок пока нет
- Clinical Outcomes of Golimumab As First, Second or Third Anti-TNF Agent in Patients With Moderate-to-Severe Ulcerative ColitisДокумент9 страницClinical Outcomes of Golimumab As First, Second or Third Anti-TNF Agent in Patients With Moderate-to-Severe Ulcerative ColitisDiana GCОценок пока нет
- Paediatric TB Treatment LandscapeДокумент11 страницPaediatric TB Treatment Landscapegiant nitaОценок пока нет
- Diagnosis and Treatment of Drug-Resistant Tuberculosis-Hermanto QuedarusmanДокумент20 страницDiagnosis and Treatment of Drug-Resistant Tuberculosis-Hermanto QuedarusmanHermanto QuedarusmanОценок пока нет
- Emerging Treatments For Crohn's Disease: Cells, Surgery, and Novel TherapeuticsДокумент10 страницEmerging Treatments For Crohn's Disease: Cells, Surgery, and Novel Therapeuticsellya theresiaОценок пока нет
- Multi-Drug-Resistant Tuberculosis (MDR-TB) Is Defined: EpidemiologyДокумент3 страницыMulti-Drug-Resistant Tuberculosis (MDR-TB) Is Defined: EpidemiologyJhemar Handa JulhamidОценок пока нет
- B7 PDFДокумент13 страницB7 PDFFernanda RibeiroОценок пока нет
- 02 Relapsed CLL - Sequencing, Combinations, and Novel AgentsДокумент8 страниц02 Relapsed CLL - Sequencing, Combinations, and Novel AgentsEunice RojasОценок пока нет
- Methotrexate in Rheumatoid Arthritis Efficacy and Safety 2329 6887 2 127Документ4 страницыMethotrexate in Rheumatoid Arthritis Efficacy and Safety 2329 6887 2 127Saifuddin HaswareОценок пока нет
- S 5359 LBLДокумент58 страницS 5359 LBLNidershan SuguneshwaranОценок пока нет
- Access Third Line ART CentrallyДокумент2 страницыAccess Third Line ART Centrallyadamu shumetОценок пока нет
- Case Scenario Drug Study - VicenteДокумент4 страницыCase Scenario Drug Study - VicenteLouraine VicenteОценок пока нет
- Data Sheet Mabthera: Pharmaceutical FormДокумент42 страницыData Sheet Mabthera: Pharmaceutical FormHeba_Al_KhozaeОценок пока нет
- Pharmacotherapy of Tuberculosis Treatment SchemesДокумент31 страницаPharmacotherapy of Tuberculosis Treatment SchemesjabirОценок пока нет
- Adherence, Dosing, and Managing Toxicities With Tri Uridine/tipiracil (TAS-102)Документ8 страницAdherence, Dosing, and Managing Toxicities With Tri Uridine/tipiracil (TAS-102)Amina GoharyОценок пока нет
- Nitrofurantoin efficacy and safety for UTIsДокумент9 страницNitrofurantoin efficacy and safety for UTIsSEPTIANA SAPUTRIОценок пока нет
- HIV/Infectious Diseases: Curtis L - Smith, Pharm. D., BCPSДокумент42 страницыHIV/Infectious Diseases: Curtis L - Smith, Pharm. D., BCPSandirio7486Оценок пока нет
- Multi-Drug-resistant Tuberculosis - Wikipedia, The Free EncyclopediaДокумент8 страницMulti-Drug-resistant Tuberculosis - Wikipedia, The Free Encyclopedianayan555Оценок пока нет
- Case-Based Learning Nausea and Vomiting: Sang Ayu Putu Wahyu Pratiwi NIM. 2208612048Документ8 страницCase-Based Learning Nausea and Vomiting: Sang Ayu Putu Wahyu Pratiwi NIM. 2208612048sang ayu putu wahyu pratiwi233Оценок пока нет
- Antiemetic Guidelines For ChemotherapyДокумент11 страницAntiemetic Guidelines For ChemotherapyAaron AntonioОценок пока нет
- Fibromyalgia & Trazodone+Pregabalin 2011Документ9 страницFibromyalgia & Trazodone+Pregabalin 2011Apostolos T.Оценок пока нет
- Brosur 1Документ1 страницаBrosur 1Regina ArningsariОценок пока нет
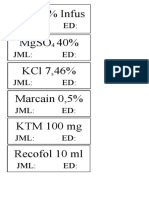
- Labek High AlertДокумент1 страницаLabek High AlertRegina ArningsariОценок пока нет
- Daftar NamaДокумент1 страницаDaftar NamaRegina ArningsariОценок пока нет
- Di@ Bisa Agen: Hubungi: Arning/ 0822 3513 3091Документ2 страницыDi@ Bisa Agen: Hubungi: Arning/ 0822 3513 3091Regina ArningsariОценок пока нет
- Patofisiologi PneumoniaДокумент1 страницаPatofisiologi PneumoniaRegina ArningsariОценок пока нет
- List of Medications and DosagesДокумент8 страницList of Medications and DosagesRegina ArningsariОценок пока нет
- Nama Obat High AlertДокумент4 страницыNama Obat High AlertRegina ArningsariОценок пока нет
- Acyclovir 5% Salf Albothyl 10 ML Bedak Salicyl: Betametason 0,1% CreamДокумент3 страницыAcyclovir 5% Salf Albothyl 10 ML Bedak Salicyl: Betametason 0,1% CreamRegina ArningsariОценок пока нет
- Tugas SosialogiДокумент108 страницTugas SosialogiRegina ArningsariОценок пока нет
- Presentation 1 RosaДокумент22 страницыPresentation 1 RosaRegina ArningsariОценок пока нет
- Format Laporan Obat MasterДокумент19 страницFormat Laporan Obat MasterRegina ArningsariОценок пока нет
- Presentation 1 RosaДокумент22 страницыPresentation 1 RosaRegina ArningsariОценок пока нет
- PME Feb.Документ52 страницыPME Feb.Fernando ComasОценок пока нет
- Role of Dmards in Ra-Psa-Sp2019Документ94 страницыRole of Dmards in Ra-Psa-Sp2019GregОценок пока нет
- Choosing The Most Appropriate Biologic Therapy For Crohn's Disease According To Concomitant Extra-Intestinal Manifestations, Comorbidities, or Physiologic ConditionsДокумент44 страницыChoosing The Most Appropriate Biologic Therapy For Crohn's Disease According To Concomitant Extra-Intestinal Manifestations, Comorbidities, or Physiologic ConditionsBernadett FarkasОценок пока нет
- Ceohns Disease ECCO Guideline SumarizedДокумент19 страницCeohns Disease ECCO Guideline Sumarizednishad nilangaОценок пока нет
- Guidelien RaДокумент16 страницGuidelien RaNurul Kamilah SadliОценок пока нет
- Abbott PowerPoint Slide Style GuideДокумент22 страницыAbbott PowerPoint Slide Style GuideloicfrevilleОценок пока нет
- ArchRheumatol 32 21Документ5 страницArchRheumatol 32 21indriОценок пока нет
- Chron Skin Allergy Oct 2010Документ32 страницыChron Skin Allergy Oct 2010shannon3458Оценок пока нет
- AbbVie Generics LawsuitДокумент248 страницAbbVie Generics LawsuitRobert GarciaОценок пока нет
- Final Rheumatoid Arthritis - PPT 2Документ51 страницаFinal Rheumatoid Arthritis - PPT 2Tino kashiriОценок пока нет
- Keeling 2019Документ8 страницKeeling 2019senkonenОценок пока нет
- Pohon Masalah AnsietasДокумент16 страницPohon Masalah AnsietasDeva NatarummandaОценок пока нет
- 10 1080@1744666X 2019 1705785Документ85 страниц10 1080@1744666X 2019 1705785infectologia larazaОценок пока нет
- Rheumatoid ArthritisДокумент77 страницRheumatoid ArthritisTalal SafdarОценок пока нет
- What Is RemicadeДокумент30 страницWhat Is RemicademanikhatОценок пока нет
- Arthritis Digest 3 - 2016 UK PDFДокумент32 страницыArthritis Digest 3 - 2016 UK PDFani5220Оценок пока нет
- European S3-Guidelines On The Systemic Treatment of PsoriasisДокумент208 страницEuropean S3-Guidelines On The Systemic Treatment of Psoriasisghitza80Оценок пока нет
- General Principles of Management of Rheumatoid ArthritisДокумент19 страницGeneral Principles of Management of Rheumatoid ArthritisSakinah Ginna RОценок пока нет
- Executive Summary: Leading Drug Safety Issues of 2012Документ21 страницаExecutive Summary: Leading Drug Safety Issues of 2012aghniajolandaОценок пока нет
- Wasserman 2011 PDFДокумент8 страницWasserman 2011 PDFAnonymous ofwo6IsB6Оценок пока нет
- Multiple Clinical and Business Milestones in 2014 for Immune PharmaceuticalsДокумент21 страницаMultiple Clinical and Business Milestones in 2014 for Immune PharmaceuticalsSusan LaskoОценок пока нет
- Rheumatoid Arthritis Treatment and Management GuideДокумент32 страницыRheumatoid Arthritis Treatment and Management GuideamirthaОценок пока нет
- Ankylosing Spondylitis...Документ6 страницAnkylosing Spondylitis...mfahrizaОценок пока нет
- TNF InhibitorsДокумент1 страницаTNF InhibitorsSam RassamОценок пока нет
- 744 FullДокумент16 страниц744 FullDaniela PopaОценок пока нет
- HS treatment options under 40 charactersДокумент52 страницыHS treatment options under 40 charactersRenzo Cruz CaldasОценок пока нет
- Cytokine Storm in COVID-19 and TreatmentДокумент24 страницыCytokine Storm in COVID-19 and TreatmentPierre FlorentínОценок пока нет
- Axial Psoriatic Arthritis An UpdateДокумент10 страницAxial Psoriatic Arthritis An Updateproject zoroОценок пока нет
- Tumor Necrosis Factor Inhibitors in Patients With Takayasu Arteritis: Experience From A Referral Center With Long-Term FollowupДокумент5 страницTumor Necrosis Factor Inhibitors in Patients With Takayasu Arteritis: Experience From A Referral Center With Long-Term FollowupMikhail PisarevОценок пока нет
- Rheumatoid Arthritis: A Review of Its History, Stages, and TreatmentДокумент12 страницRheumatoid Arthritis: A Review of Its History, Stages, and TreatmentAdhelaAuroraFransiskaОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesОт EverandThe Ultimate Guide To Memory Improvement TechniquesРейтинг: 5 из 5 звезд5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementОт EverandTechniques Exercises And Tricks For Memory ImprovementРейтинг: 4.5 из 5 звезд4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОценок пока нет
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 5 из 5 звезд5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingОт EverandThe Happiness Trap: How to Stop Struggling and Start LivingРейтинг: 4 из 5 звезд4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 5 из 5 звезд5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 3.5 из 5 звезд3.5/5 (31)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОт EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОценок пока нет
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossОт EverandThe Tennis Partner: A Doctor's Story of Friendship and LossРейтинг: 4.5 из 5 звезд4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisОт EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisРейтинг: 5 из 5 звезд5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)