Академический Документы
Профессиональный Документы
Культура Документы
A New Classification of Head Injury Based On
Загружено:
Jejem Marandra EmkamasИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A New Classification of Head Injury Based On
Загружено:
Jejem Marandra EmkamasАвторское право:
Доступные форматы
A new classification of head injury based on
computerized tomography
LAWRENCE F. MARSHALL, M.D., SHARON BOWERS MARSHALL, B.S.N.,
MELVILLE R. KLAUBER, M.D., ANO MARJAN VAN BERKUM CLARK, R.N.
Division of Neurosurgery, Universityof California Medical Center, San Diego, California
HOWARD M. EISENBERG, M.D.
Division of Neurosurgery, Universityof Texas Medical Branch, Galveston, Texas
JOHN A. JANE, M.D.
Department of Neurosurgery, Universityof Virginia School of Medicine, Charlottesville, Virginia
THOMAS G. LUERSSEN, M.D.
Division of Neurosurgery, Indiana UniversityMedical Center, Indianapolis, Indiana
ANTHONY MARMAROU, PH.D.
Division of Neurosurgery, Medical College of Virginia, Richmond, Virginia
MARY A. FOULKES, PH.D.
Biometry and Field Studies Branch, National Institute of Neurological Disorders and Stroke, Bethesda,
Maryland
A new classification of head injury based primarily on information gleaned from the initial computerized
tomography (CT) scan is described. It utilizes the status of the mesencephalic cisterns, the degree of midline
shift in millimeters, and the presence or absence of one or more surgical masses. The term "diffuse head
injury" is divided into four subgroups, defined as follows: Diffuse Injury I includes all diffuse head injuries
where there is no visible pathology; Diffuse Injury II includes all diffuse injuries in which the cisterns are
present, the midline shift is less than 5 mm, and/or there is no high- or mixed-density lesion of more than 25
cc; Diffuse Injury III includes diffuse injuries with swelling where the cisterns are compressed or absent and
the midline shift is 0 to 5 mm with no high- or mixed-density lesion of more than 25 cc; and Diffuse Injury
IV includes diffuse injuries with a midline shift of more than 5 mm and with no high- or mixed-density lesion
of more than 25 cc. There is a direct relationship between these four diagnostic categories and the mortality
rate. Patients suffering diffuse injury with no visible pathology (Diffuse Injury I) have the lowest mortality rate
(10%), while the mortality rate in patients suffering diffuse injury with a midline shift (Diffuse Injury IV) is
greater than 50%. When used in conjunction with the traditional division of intracranial hemorrhages
(extradural, subdural, or intracerebral), this categorization allows a much better assessment of the risk of
intracranial hypertension and of a fatal or nonfatal outcome. This more accurate categorization of diffuse
head injury, based primarily on the result of the initial CT scan, permits specific subsets of patients to be
targeted for specific types of therapy. Patients who would appear to be at low risk based on a clinical
examination, but who are known from the CT scan diagnosis to be at high risk, can now be identified.
KEY WOROS Traumatic Coma Data Bank 9 head injury 9 coma 9
intracranial pressure 9 computerized tomography 9 grading system
'EUROSURGEONSand others interested in treating of prognosis. It is generally recognized that patients
N head-injured patients have traditionally cate-
gorized head injury on the basis of focal or
nonfocal lesions or, more recently, on the basis of
with diffuse injury have a lower mortality rate than do
patients with mass lesions. However, this type o f pool-
ing of patient data might mask groups of patients with
diffuse versus focal or mass lesions. ~'2 These categori- diffuse injury who are at risk from intracranial hyper-
zations, while helpful in subdividing head injury into tension and who in fact have a high mortality rate.
two major groups, have significant limitations in terms A general lack of recognition of the importance o f
$14 J. Neurosurg. / Volume 75/November, 1991
New classification of head injury based on CT
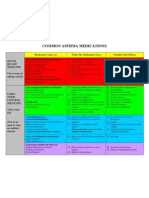
certain computerized tomography (CT) findings, par- TABLE 1
ticularly in patients who appear to be at low risk based Dingnostic categories of types of abnormalities visualized on
on their clinical examination, led us to develop a new CT scanning*
classification of head injury'. This classification was de-
signed on the basis of our experience in the pilot phase Category Definition
of the Traumatic Coma Data Bank (TCDB) study.: Diffuse Injury 1 no visibleintracranial pathologyseen on
Despite the fact that the TCDB included only patients (no visible CT scan
with severe head injury, the present categorization lends palhology)
itself to inclusion of other grades of head injury as well. Diffuse Injury.II cisterns are present with midline shift 0-5
For example, among patients with more moderate in- mm and/or:
lesion densitiespresent
juries, an "unexpected" adverse outcome occurs not no high-or mixed-densitylesion > 25 cc
infrequently because the benign clinical status and lack may include bone fragmentsand foreign
of a mass lesion on the initial CT scan are interpreted bodies
as indicating that the patient is at little risk of develop- Diffuse Injury III cisterns compressedor absent with midline
(swelling) shift 0-5 mm, no high- or mixed-density
ing intracranial hypertension. It is for this group of pa- lesion > 25 cc
tients that a more refined classification, such as the one Diffuse Injury IV midline shift > 5 ram, no high-or mixed-
described here, would be useful. (shift) density lesion > 25 cc
A significant number of patients in the United States evacuated mass lesion any lesion surgicallyevacuated
who have compression or absence of the mesencephalic nonevacuated mass high- or mixed-densitylesion > 25 cc, not
lesion surgically evacuated
cisterns on their initial CT scan are treated as if their
CT scans were normal because their clinical evaluation * CT = computerizedtomography.
is good. Probably hundreds and perhaps thousands of
these patients have a catastrophic outcome each year.
Thus, a new classification is needed that can identify
patients at particular risk for developing intracranial provides virtually complete coverage of severe head
hypertension. Such a classification would allow for early injuries, in contrast to the traditional categories of
prediction of outcome when only a few factors, such as intracranial hemorrhages, which gives only partial cov-
age, clinicaI status, and CT findings, are known. Fur- erage. Only 17 (2%) of 746 patients in our study were
thermore, the frequency of intracranial hypertension classified as having an "unknown" diagnosis, 16 of
has been shown to be high in patients who are operated whom died.
on for mass lesions. In such patients, it is possible that A more accurate categorization of such injuries
a CT scan performed immediately or within 24 hours would ultimately allow for the initiation of new thera-
after surgery might be extremely useful in predicting pies in some subgroups of severely injured patients and
the likelihood of that patient developing intracranial make decisions regarding further treatment more logical
hypertension and might better identify the need for if, for example, the CT diagnosis and some other factors,
continuous monitoring of the intracranial pressure such as the patient's age, indicated an unsalvageable
(ICP) in such patients. patient. Early in the study, it was the view of the TCDB
The development of a new classification of head investigators and the Biometry and Field Studies
injury was considered to be important in order to Branch of the National Institute of Neurological Dis-
permit a more accurate description of the kinds of orders and Stroke that such a classification might also
injuries the patients have suffered and to assess the be useful in a more general sense for describing subsets
relationship between the pattern of brain injury deter- of patients with more modest injuries who are at risk
mined by CT and, in part, by clinical examination. The of a poor outcome.
diagnostic categories of this new classification and their
definitions are presented in Table 1. The intent of this Clinical Material and Methods
new classification was twofold: 1) to allow a more
accurate classification of severe head injury so that Protocol
subsets of patients at particular risk for deterioration In the period from January 1, 1984, through Septem-
could be identified; and 2) to allow more accurate ber 30, 1987, 1030 patients were admitted to the TCDB
predictive statements at the time of the patient's initial hospitals. Of these, 284 were excluded from this analysis
evaluation regarding the likelihood of a fatal or nonfatal because they had suffered gunshot wounds of the brain
outcome. or were brain-dead on admission, leaving 746 patients
It is not the purpose of the new classification scheme with severe head injury available for the present analy-
to replace the Glasgow Coma Scale 9 (GCS) or any other sis. Severe head injury was defined as a GCS score of 8
measure of injury severity. We wish to show that the or less following nonsurgical resuscitation. A format for
new classification, when used in conjunction with es- the description of the major CT findings was established
tablished predictors, provides a more accurate basis during the pilot phase of the TCDB study] Based on
upon which to predict outcome than that provided by our analysis and experience with this initial CT Scan
the established predictors alone. The new classification Form, a new CT collection instrument and a manual
J. Neurosurg. / Volume 75/November, 1991 $15
L. F. Marshall, el al.
FiG. 1. Computerized tomography scans showing examples of Diffuse InjuD' II: diffuse injury with limited
shift or mass effect (left); diffuse injury with multifocal hemorrhages (center); and diffuse injury marked by
deep central hemorrhage (right). The right scan shows a hemorrhage in the midbrain without effacement into
the mesencephalic cisterns.
for its use were developed for the full-phase TCDB
study. Particular emphasis was placed on the appear-
ance of the mesencephalic cisterns and on the degree
of midline shift. Mechanisms for the determination of
these changes were tested during the initial phase of the
TCDB study.
All patients considered to be salvageable at the time
of admission to the four TCDB hospitals underwent
CT scanning, usually within the first hours following
admission. While the CT Scan Form was used to permit
a comprehensive description o[ the CT findings, a much
smaller number of factors were used to classify the
patients into the diagnostic categories shown in Table
1. The accuracy of the CT diagnoses was ensured by FIG. 2. Admission computerized tomography scan of a
several methods. Quality assurance trials were carried patient with Diffuse Injury III: diffuse injury with swelling,
out among the centers involved in the pilot phase of showing virtual obliteration of the cisterns without midline
the TCDB study on a series of scans sent to each center. shift or mass effect. This 23-year-old patient was a victim of
a motorcycle accident with an admitting Glasgow Coma Scale
A second set of scans was reviewed during the early score of 7.
part of the full-phase TCDB study as well. Methodolog-
ical changes including exact criteria for measuring shift
and for ventficular asymmetry were made during the
pilot phase of the TCDB study to ensure that all defi- ogy" (Diffuse Injury I) means exactly that: the CT scan
nitions and categories were applied in a uniform fash- in such patients must be entirely normal for a patient
ion. All scans in each institution were read by one of that specific age and preinjury health status. The
individual, which permitted a high level of internal distinction between the remaining categories was based
consistency. The center interpretations were compared on observations made during the pilot phase of the
during a series of reviews carried out by the TCDB TCDB study that intracmnial hypertension became pro-
principal investigators. A manual providing stringent gressively more frequent as the status of the mesence-
definitions for each category on the CT Scan Form was phalic cisterns became more compromised and as the
developed and utilized by all the centers. degree of midline shift increasedJ ~ Thus, while the
classifications of diffuse injury, diffuse injury with
Diagnostic Categories. Examples swelling, and diffuse injury with midline shift are ad-
Examples of CT scans for each of the diagnostic mittedly arbitrary, they are based on substantial expe-
categories are shown in Figs. 1 to 6. It is important to rience which strongly suggested that such subclassifica-
emphasize that "diffuse injury with no visible pathol- tions would permit more accurate identification of
Sl 6 J. Neurosurg. / Volume 75/November, 1991
New classification of head injury based on CT
FJ(;. 5. Computerized tomography scans of a patient with
multiple lesions. Left: Admission scan showing pathology
initially not considered to need surgical treatment. Right:
FIG. 3. Admission computerized tomography scan of a Scan obtained 18 hours after admission showing progressive
patient with Diffuse Injury IV: diffuse injuD, with shift, show- enlargement of both the subdural hematoma and the intra-
ing a 22-mm shift of midline from left to right and obliteration cerebral hemorrhage. Based on this appearance, evacuation
of the perimesencephalic cisterns. This 18-year-old man was was carried out.
involved in a motor-vehicle accident and his Glasgow Coma
Scale score on admission was 4.
strates a deep contusion or intraparenchymal hemor-
rhage in the brain stem which produced no disturbance
of the mesencephalic cisterns. Thus, within each of
patients at progressively higher risk for intracranial
these new diagnostic categories, a variety of pathologi-
hypertension and death, s'~~
cal processes may be present.
It is important to emphasize that the category of
The need for a classification scheme to be strictly
Diffuse Injury II describes the status of the mesence-
defined yet capable of responding to a change in patient
phalic cisterns and the degree or lack of midline shift,
status is illustrated in Figs. 5 and 6. Figure 5A illustrates
even though a variety of pathological pictures may be
the preoperative CT appearance of a patient with a
present. Three specific examples of Diffuse Injury II
small intracerebral hemorrhage in the right posterior
are illustrated: Fig. 1A illustrates a small superficial
frontal region and a contralateral small subdural he-
contusion with a minimum degree of midline shift, Fig.
matoma. In this patient, the mesencephalic cisterns
1B shows the petechial hemorrhages of the brain char-
were initially normal and therefore, in spite of the
acteristic of diffuse axonal injury, and Fig. 1C demon-
presence of two distinct lesions, the patient would have
been classified as having a Diffuse Injury II. However,
the subdural hematoma subsequently enlarged to 75 cc
and surgery was undertaken, at which time both lesions
were removed. The patient's diagnostic category was
FIG. 6. A demonstration of the dynamic aspects of brain
injury on the computerized tomography scans of a 26-year-
FIG. 4. Admission computerized tomography scan of a old man who was struck by an automobile. Left: Initial scan
patient in the "evacuated mass lesion" category showing a showing open cisterns and no midline shift. Right: Follow-
large intracerebral hemorrhage which required surgical evac- up scan obtained 13 hours later showing significant midline
uation. shift and development of a surgical subdural hematoma.
J. Neurosurg. / Volume 75/November, 199I S17
L. F. Marshall, et al.
TABLE 2
Outcomeatdischa~einrelationloinlracranialdiagnosis*
Diffuse Diffuse Diffuse Diffuse Evacuated Nonevacuated Brain-Stem
Outcome Unknown Totals
Injury I Injury II Injury III Injury IV Mass Mass Injury
at Discharge
No. % No. % No. % No. % No. % No. % No. % No. % No. %
good 14 27.0 15 8.5 5 3.3 1 3.1 14 5.1 1 2.8 0 0 0 0 50 7.0
moderate 18 34.6 46 26.0 20 13.1 1 3.1 49 17.7 3 8.3 0 0 1 5.9 138 18.5
severe 10 19.2 72 40.7 41 26.8 6 18.8 72 26.1 7 19.4 1 33.3 0 0 209 28.0
vegetative 5 9.6 20 11.3 35 22.9 6 18.8 34 12.3 6 16.7 0 0 0 0 106 14.0
dead 5 9.6 24 13.5 52 34.0 18 56.2 107 38.8 19 52.8 2 66.7 16 94.1 243 32.5
totals 52 100 177 100 153 100 32 100 276 100 36 100 3 100 17 100 746 100
* Outcome classified by the Glasgow Outcome Scale? For a description of Diffuse Injury I to IV, see Table 1.
then changed to acute subdural hematoma with a sec- Other factors are needed in addition to the CT clas-
ondary diagnosis of intraparenchymal hemorrhage. Fig- sification for prognostic purposes, as evidenced by the
ure 6 illustrates a substantial change in the CT picture outcome differences by age for a single category, Diffuse
within 12 hours, requiring a change in patient catego- Injury II (Table 3). For this diagnosis, 39% of the
rization. Thus, the dynamic nature of the patient's patients under the age of 40 years had a good or
injury can only be characterized by serial scans, but the moderate outcome versus 8% for those over 40 years;
concept that these categories are of value in predicting conversely, the older age group had over fourfold risk
the patient's course still holds. of death in comparison to the younger age group.
The CT diagnosis was a highly significant independ-
Statistical Analysis ent predictor of mortality (p = 0.0001) when age and
The association between the GCS score and the new motor score were included in the model. This three-
classification ("unknowns" omitted) was first tested by factor predictor model showed excellent fit to data (p =
the Monte Carlo approach (that is, empirical randomi- 0.86; values close to 1 indicate good fit). On the other
zation) using the Kruskal-Wallis statistic; for this, the hand, when CT diagnosis was not included, the fit was
StatXact program was employed with 10,000 random- poor (p = 0.041). Evidently, the improvement in pre-
izations. The Monte Carlo approach was indicated be- diction increased the sensitivity of the model (ability
cause of the small numbers in some of the groups in to predict deaths) by 6% (from 53% to 59%), but speci-
the classification. Logistic regression was used to show ficity was virtually unchanged. This is understandable
the improvement obtainable by the use of the new since the specificity of the two-factor prediction model
classification (excluding brain-stem and unknown in- was already very high (87%). The models themselves
juries) both above that using best postresuscitation mo- are not presented because, as has been shown elsewhere,
tor score and alone. Motor score was used instead of a truly comprehensive model takes into account addi-
the GCS score as a predictor because of missing obser- tional factors such as eye opening, hypotension, and
vations in the GCS categories. 3 The correlation between others.
motor score and GCS score in our study was 0.90, the There was a strong linkage between the ultimate
highest of the GCS subscores. Logistic regression was outcome and the degree of brain swelling and the degree
also used to develop a prediction model for Diffuse of midline shift as seen on the CT scans of patients
Injury III (swelling).
Results
TABLE 3
There is a striking direct relationship between out- Outcome of Diffuse Injury H at last evaluation by patient age*
come and initial CT scan diagnosis (p = 0.0002) (Table
2). Given the fact that the diagnostic categories in large Age (yrs)
Outcome
measure are a reflection of changes in brain volume, it (At Last _< 40 > 40 Totals
is tempting to conclude that what one is seeing is an Visit)
early indicator of the degree of intracranial hyperten- No. % No. % No. %
sion that is likely to occur in such patients. It is impor- good 15 10.0 0 0 15 8.5
tant to recognize that the degree of change in brain moderate 44 28.7 2 8.3 46 26.0
severe 63 41.1 9 37.5 72 40.7
bulk is a function of a series of complex phenomena vegetative 17 11.1 3 12.5 20 11.3
including the degree of impact injury, the presence or dead 14 9.1 10 41.7 24 13.6
absence of ischemia or ischemic hypoxia prior to CT totals 153 100 24 100 177 100
scanning, and perhaps a host of other factors not yet * Outcome classified by the Glasgow Outcome Scale. 4 For a de-
identified. scription of Diffuse Injury I1, see Table 1.
S18 J. Neurosurg. / Volume 75/November, 1991
New classification of head injury based on CT
with nonsurgical lesions. As an adequate sample size ship between the CT scan appearance, mortality, and
was available in the category of Diffuse Injury III (swell- the frequency of elevated ICP in the population indi-
ing), a logistic regression equation was developed in this cates that the CT findings are strongly predictive of the
group to determine the factors that might be helpful likelihood of intracranial hypertension and that there
during the first 72 hours in sharpening the 6-month is a relationship, perhaps not completely defined, be-
outcome mortality rate prediction in such patients. As tween the degree of intracranial hypertension and the
shown in Table 4, the most powerful predictor of likelihood of death. Undoubtedly other factors, partic-
outcome in patients with Diffuse Injury II1 (swelling) ularly the actual impact injury in the severely injured
was the highest ICP. In contrast, within the other groups patient, determine the postinjury course. However, in
(not shown), age and motor scores were the most pow- patients with less substantial biomechanical injuries, it
erful predictors. Further serving to emphasize the ad- appears likely that early intervention might prevent the
verse consequences of high ICP in these patients, those development of other insults and improve both mortal-
in Diffuse Injury III group with good motor scores did ity and the overall quality of life. Certainly, the rather
relatively less well than the TCDB cohort as a whole in low mortality rate for institutions utilizing systematic
which postresuscitation GCS scores closely correlated treatment schemes for patients with GCS scores of 6,
with outcome. 7, or 8, when compared to results in hospitals with a
There is, of course, an interdependence between the much smaller experience in the care of such patients,
degree of motor dysfunction and the status of the brain suggests that therapeutic intervention does matter.
stem and the cisterns seen on CT scan. However, for This new categorization offers the possibility of early
the specific diagnostic categories used here, the CT scan identification of patients at risk as well as earlier pre-
often appeared to be a more accurate predictor of the diction of severely head-injured patients falling into
ultimate course of patients with absent or compressed broad outcome categories. While this concept needs to
cisterns than the patient's initial clinical examination if be tested in a large series of patients for whom predic-
the latter revealed a less severe injury. This was also our tions are made within 24 hours using the limited infor-
experience in the pilot phase of the TCDB study? mation that would then be available, our preliminary
It is beyond the scope of this article to deal with the experience in one center with this approach is prom-
specific question as to the reversibility of the CT scan ising.
findings based on therapeutic intervention. However, it The new classification of head injury also permits
is important to note that, within the TCDB, a substan- the early identification of patients potentially at high
tial reduction in mortality from elevated ICP has been risk from intracranial hypertension and allows the
reported in a preliminary fashion in patients with absent neurosurgeon the option of early intervention. Such a
or compressed cisterns who had less severe injuries classification also allows the identification of specific
(GCS scores of 6, 7, or 8). This suggests, at least for subsets of patients from within the overall grouping of
some patients, that early intervention for intracranial diffuse injury who have remarkably similar courses and
hypertension might play an important role in prevent- mortality rates when compared to patients with extra-
ing deterioration, a vegetative outcome, or death. axial and intra-axial mass lesions: these include patients
with diffuse injury with swelling (Diffuse Injury III) and
Discussion diffuse injury with midline shift (Diffuse Injury IV).
The CT classification introduced here appears to Diffuse Injury categories III and IV appear to be anal-
have significant application in the clinical care of the ogous in many ways to patients harboring acute, sizable
acutely head-injured patient. The very strong relation- hemorrhagic lesions and are logical groups for clinical
trials to test the efficacy of presently available as well
as new therapies. Furthermore, although the frequency
of diffuse head injury with midline shift (Diffuse Injury
TABLE 4
IV) was relatively low, its very high mortality rate in
Potential predictors of mortality ratefor patients with an head-injury centers that are experienced in the care of
intracranial diagnosis of Diffuse Injury 111 (swelling)*
such patients suggests that these patients represent a
Goodness- target group in which innovative therapies might first
Prediction
Predictor of-Fit1" be tested?
(p value) (p value)
highest ICP (first 72 hrs) < 0.001 0.038 References
pupil reactivity (postresuscitation) < 0.001 0.610
lowest 1CP (first 72 hrs) 0.023 0.930 1. Becker DP, Miller JD, Ward JD, et al: The outcome from
best motor score (postresuscitation) 0.510 0.970 severe head injury with early diagnosis and intensive
age 0.680 0.970 management, d Neurosurg 47:491-502, 1977
* ICP = intracranial pressure.For a definition of DiffuseInjuryIII, 2. Gennarelli TA, Speilman GM, Langfitt TW, et al: Influ-
see Table 1. ence of the type of intracranial lesion on outcome from
t By the Hosmer-Lemeshowtest, p value for each row for model severe head injury. J Neurosurg 56:26-32, 1982
fit including predictorsin its row and above(the higher the p value, 3. Hosmer DW, Lemeshow S: Applied Logistic Regression.
the betterthe fit). New York: John Wiley & Sons, 1989
J. Neurosurg. / Volume 75/November, 1991 S19
L. F. Marshall, et al.
4. Jennett B, Bond M: Assessment of outcome after severe consciousness. A practical scale. Lancet 2:81-84, 1974
brain damage. A practical scale. Lancet 1:480-484, 1975 10. Toutant SM, Klauber MR, Marshall LF, et al: Absent or
5. Lobato RD, Sarabia R, Cordobes F, etal: Posttraumatic compressed basal cisterns on first CT scan: ominous
cerebral hemispheric swelling. Analysis of 55 cases stud- predictors of outcome in severe head injury. J Nenrosurg
ied with computerized tomography. J Neurosurg 68: 61:691-694, 1984
417-423, 1988 1I. van Dongen KJ, Braakman R, Gelpke GJ: The prognostic
6. Luerssen TG, Hults K, Klauber M, et al: Improved out- value of computerized tomography in comatose head-
come as a result of recognition of absent or compressed injured patients. J Neurosurg 59:951-957, 1983
cisterns on initial CT scans, in Hoff JT, Betz AL (eds):
Intracranial Pressure VII. Berlin: Springer-Verlag, 1989,
pp 598-602
7. Marshall LF, Becker DP, Bowers SA, et al: The National This work was additionally supported by National Insti-
Traumatic Coma Data Bank. Part 1: Design, purpose, tute of Neurological Disorders and Stroke Contracts NO1-NS-
goals, and results. J Neurosurg 59:276-284, 1983 9-2306, 2307, 2308, 2309, and 2313 for the Pilot Traumatic
8. Teasdale E, Cardoso E, Galbraith S, el al: CT scan in Coma Data Bank.
severe diffuse head injury: physiological and clinical cor- Address reprint requests to: Lawrence F. Marshall, M.D.,
relations. J Neurol Neurosurg Psychiatry 47:600-603, Division of Neurosurgery, University of California Medical
1984 Center, 225 Dickinson Street H-501, San Diego, California
9. Teasdale G, Jennett B: Assessment of coma and impaired 92103-1990.
$20 J. Neurosurg. / Volume 75/November, 1991
Вам также может понравиться
- Picmonic NCLEX Study PlanДокумент38 страницPicmonic NCLEX Study PlanHannah Adams73% (33)
- DM Self AssessmentДокумент6 страницDM Self AssessmentruguОценок пока нет
- Know Your Magnetic FieldДокумент75 страницKnow Your Magnetic FieldAtma Jnani100% (5)
- Final - HOSPITAL BILL FORMAT PDFДокумент2 страницыFinal - HOSPITAL BILL FORMAT PDFH C85% (13)
- Oxygen Therapies: Interview With Ed MccabeДокумент5 страницOxygen Therapies: Interview With Ed MccabeOrlando Gunther100% (1)
- Nclex-Rn Essential Questions and RationalesДокумент96 страницNclex-Rn Essential Questions and RationalesGloryJane100% (1)
- Common Asthma MedicationsДокумент1 страницаCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyОценок пока нет
- Anna O's Significance in PsychologyДокумент3 страницыAnna O's Significance in PsychologycaironsalamОценок пока нет
- Bad ObjectsДокумент12 страницBad ObjectsmariaagaОценок пока нет
- Abigail Domingo Physical AssessmentДокумент87 страницAbigail Domingo Physical AssessmentVenus Maui RoqueОценок пока нет
- Subdural Hematomas in The ElderlyДокумент19 страницSubdural Hematomas in The ElderlyRegina PhilyriaОценок пока нет
- Pediatric Basic Life SupportДокумент50 страницPediatric Basic Life SupportnurmauliarizkyОценок пока нет
- ECG Definition: - PurposeДокумент2 страницыECG Definition: - PurposeJustine Karl Pablico100% (1)
- A New Classification of Head Injury Based On Computerized Tomography PDFДокумент7 страницA New Classification of Head Injury Based On Computerized Tomography PDFHendry SusantoОценок пока нет
- Blunt Cerebrovascular Injuries - Advances in Screening, Imaging, and Management TrendsДокумент9 страницBlunt Cerebrovascular Injuries - Advances in Screening, Imaging, and Management TrendsJuliana Mendoza MantillaОценок пока нет
- Journal of International Medical Research 2009 Zhu 983 95Документ13 страницJournal of International Medical Research 2009 Zhu 983 95Annisa ChastallaОценок пока нет
- Neuro RX 002000372Документ12 страницNeuro RX 002000372denisОценок пока нет
- CarotidДокумент4 страницыCarotidAns FitriОценок пока нет
- Management of Blunt and Penetrating Neck TraumaДокумент15 страницManagement of Blunt and Penetrating Neck TraumaJuan Jose SarastiОценок пока нет
- Cooper 1992Документ7 страницCooper 1992Edwin Sugondo TaufikОценок пока нет
- Clinical Issues: Blunt Cardiac TraumaДокумент5 страницClinical Issues: Blunt Cardiac Traumacharlietuna1Оценок пока нет
- The Parkland Protocol's Modified Berne-Norwood Criteria Predict Two Tiers of Risk For Traumatic Brain Injury ProgressionДокумент7 страницThe Parkland Protocol's Modified Berne-Norwood Criteria Predict Two Tiers of Risk For Traumatic Brain Injury ProgressionJaime XavierОценок пока нет
- Antikoagulan JurnalДокумент5 страницAntikoagulan JurnalansyemomoleОценок пока нет
- Marshall1991 The Outcome of Severe Closed Head InjuryДокумент9 страницMarshall1991 The Outcome of Severe Closed Head InjuryJulieta PereyraОценок пока нет
- Intracranial Pathophysiology, Zainal MДокумент25 страницIntracranial Pathophysiology, Zainal MTina HerreraОценок пока нет
- Dural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-AnalysisДокумент14 страницDural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-Analysisclaudio RivasОценок пока нет
- Thrombectomy in Extensive Stroke May Not Be Beneficial and Is Associated With Increased Risk For HemorrhageДокумент9 страницThrombectomy in Extensive Stroke May Not Be Beneficial and Is Associated With Increased Risk For HemorrhageAlex LüttichОценок пока нет
- Clinical Characterization of Traumatic Acute Interhemispheric Subdural HematomaДокумент7 страницClinical Characterization of Traumatic Acute Interhemispheric Subdural HematomaDavid Christian HaurissaОценок пока нет
- Indications For CT Scanning in Minor Head Injuries: A ReviewДокумент6 страницIndications For CT Scanning in Minor Head Injuries: A ReviewariqОценок пока нет
- Jurnal Saraf PDFДокумент11 страницJurnal Saraf PDFkade silabanОценок пока нет
- Trauma KepalaДокумент6 страницTrauma KepalaWiwikОценок пока нет
- Which CT Features Help Predict Outcome After Head Injury?: PaperДокумент5 страницWhich CT Features Help Predict Outcome After Head Injury?: PaperLady KweeОценок пока нет
- Emergency Chest ImagingДокумент156 страницEmergency Chest ImagingAshutosh KafleОценок пока нет
- Assessing The Severity of Traumatic Brain Injury-Time For A Change?Документ12 страницAssessing The Severity of Traumatic Brain Injury-Time For A Change?Anonymous R6ex8BM0Оценок пока нет
- Head Trauma CT Scan Case StudyДокумент8 страницHead Trauma CT Scan Case Studytruevine_ministry100% (1)
- Trauma CERVICAL-Radiol Clin N.A.2012Документ14 страницTrauma CERVICAL-Radiol Clin N.A.2012Pepe pepe pepeОценок пока нет
- Practice Management Guidelines For The Management of Mild Traumatic Brain Injury: The EAST Practice Management Guidelines Work GroupДокумент23 страницыPractice Management Guidelines For The Management of Mild Traumatic Brain Injury: The EAST Practice Management Guidelines Work GroupDian Caroline 吴慧娟Оценок пока нет
- Management of Penetrating Wounds of The HeartДокумент2 страницыManagement of Penetrating Wounds of The HeartInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Chest Pain Units (Issue of Cardiology Clinics Journal) - M. Crawford, Ed., (Elsevier, 2005) WWДокумент215 страницChest Pain Units (Issue of Cardiology Clinics Journal) - M. Crawford, Ed., (Elsevier, 2005) WWRomeo-Remus RaffaiОценок пока нет
- Clinics 5Документ19 страницClinics 5Renju KuriakoseОценок пока нет
- Tirado-Bsn 4d-Journal Summary and ReflectionДокумент3 страницыTirado-Bsn 4d-Journal Summary and ReflectionJeniper Marie Cute29Оценок пока нет
- Intracranial CystsДокумент9 страницIntracranial CystsjosephОценок пока нет
- Medical Management of StrokeДокумент6 страницMedical Management of StrokemehakОценок пока нет
- Polin1997 PDFДокумент11 страницPolin1997 PDFRaul VillacresОценок пока нет
- Report Information From Proquest: 09 September 2015 10:04Документ20 страницReport Information From Proquest: 09 September 2015 10:04Wilko WilliamОценок пока нет
- A Stroke Watershed: APRIL2020Документ2 страницыA Stroke Watershed: APRIL2020Ioan DogariuОценок пока нет
- Trauma CraneoencefalicoДокумент18 страницTrauma CraneoencefalicoUCIADULTO UPEDОценок пока нет
- Epidural Hematoma: Continuing Education ActivityДокумент16 страницEpidural Hematoma: Continuing Education ActivityIka AriandanaОценок пока нет
- Uso Milrinone VasoespasmoДокумент7 страницUso Milrinone VasoespasmoHernando CastrillónОценок пока нет
- Acv PDFДокумент14 страницAcv PDFFelipe AlcainoОценок пока нет
- CT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingДокумент9 страницCT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingPari Pengda BaliОценок пока нет
- Protocols: Destiny Ii: Decompressive Surgery For The Treatment of Malignant Infarction of The Middle Cerebral Artery IiДокумент8 страницProtocols: Destiny Ii: Decompressive Surgery For The Treatment of Malignant Infarction of The Middle Cerebral Artery Iirodolfo riosОценок пока нет
- Bacterial Brain Abscess: An Outline For Diagnosis and ManagementДокумент10 страницBacterial Brain Abscess: An Outline For Diagnosis and ManagementWIWI HRОценок пока нет
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeДокумент7 страниц(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroОценок пока нет
- J NeuroIntervent Surg 2013 González Neurintsurg 2013 010715Документ7 страницJ NeuroIntervent Surg 2013 González Neurintsurg 2013 010715Rogério HitsugayaОценок пока нет
- Stroke NarrativeДокумент10 страницStroke Narrativecfalcon.medicinaОценок пока нет
- Intracranial Infections Clinical and Imaging CharacteristicsДокумент20 страницIntracranial Infections Clinical and Imaging CharacteristicsRiyan NuelОценок пока нет
- Detecting Intracranial Hemorrhage With Deep LearningДокумент5 страницDetecting Intracranial Hemorrhage With Deep LearningManoj MaggotОценок пока нет
- Thick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageДокумент9 страницThick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageVanessa LandaОценок пока нет
- Flaherty 2016Документ6 страницFlaherty 2016Diornald MogiОценок пока нет
- Terson Syndrome: Don't Let It Go Unrecognized: Ophthalmic PearlsДокумент2 страницыTerson Syndrome: Don't Let It Go Unrecognized: Ophthalmic PearlsSherley CruzОценок пока нет
- Imaging Findings of Intraventricular and Ependymal LesionsДокумент16 страницImaging Findings of Intraventricular and Ependymal Lesionsanggi abОценок пока нет
- Ging of Acute Ischemic Stroke: Marwan El-Koussy, Gerhard Schroth, Caspar Brekenfeld, Marcel ArnoldДокумент23 страницыGing of Acute Ischemic Stroke: Marwan El-Koussy, Gerhard Schroth, Caspar Brekenfeld, Marcel ArnoldAnonymous iea4m0ZRОценок пока нет
- Síndrome Compartimental 2016Документ9 страницSíndrome Compartimental 2016luisaОценок пока нет
- Evaluation of Patients With Possible Cardiac Chest Pain: A Way Out of The JungleДокумент2 страницыEvaluation of Patients With Possible Cardiac Chest Pain: A Way Out of The JungleBenny TrisaktyariОценок пока нет
- Chinese Journal of TraumatologyДокумент5 страницChinese Journal of Traumatologybulan hasanОценок пока нет
- Jamacardiology Van Rosendael 2020 Oi 190097 1609877359.99205Документ9 страницJamacardiology Van Rosendael 2020 Oi 190097 1609877359.99205Linda SuciОценок пока нет
- Iht Nejm 2014Документ10 страницIht Nejm 2014Ademir Ruiz EcheverríaОценок пока нет
- SNH CraniotomyДокумент8 страницSNH CraniotomyxshreОценок пока нет
- Daño Miocardico Perioperatorio 2021Документ6 страницDaño Miocardico Perioperatorio 2021Ramos Zavala Julio CesarОценок пока нет
- Femur Fractures Should Not Be Considered Distracting Injuries For CervicalДокумент6 страницFemur Fractures Should Not Be Considered Distracting Injuries For CervicalnellyОценок пока нет
- Target Volume Delineation for Pediatric CancersОт EverandTarget Volume Delineation for Pediatric CancersStephanie A. TerezakisОценок пока нет
- Institute of Surgical Research Surgical Technics: A1 Practical ModulДокумент39 страницInstitute of Surgical Research Surgical Technics: A1 Practical ModulJejem Marandra EmkamasОценок пока нет
- Practice EssentialsДокумент10 страницPractice EssentialsJejem Marandra EmkamasОценок пока нет
- Mkti2012 0202 109115 PDFДокумент7 страницMkti2012 0202 109115 PDFSulyasti nomleniОценок пока нет
- WHO Dengue Guidelines 2013Документ160 страницWHO Dengue Guidelines 2013Jason MirasolОценок пока нет
- Pediculosis CapitisДокумент11 страницPediculosis CapitisJejem Marandra EmkamasОценок пока нет
- Kang GoroДокумент12 страницKang GoroJejem Marandra EmkamasОценок пока нет
- Jurnal AnakДокумент5 страницJurnal AnakJejem Marandra EmkamasОценок пока нет
- Topical Antibiotics in DermatologyДокумент19 страницTopical Antibiotics in DermatologyJejem Marandra EmkamasОценок пока нет
- Mirror Therapy in Unilateral Neglect After Stroke (MUST Trial)Документ6 страницMirror Therapy in Unilateral Neglect After Stroke (MUST Trial)Jejem Marandra EmkamasОценок пока нет
- Parental Obesity and Early Childhood Development: BackgroundДокумент12 страницParental Obesity and Early Childhood Development: BackgroundJejem Marandra EmkamasОценок пока нет
- Postischemic Inflammation in Acute Stroke: Open AccessДокумент9 страницPostischemic Inflammation in Acute Stroke: Open AccessJejem Marandra EmkamasОценок пока нет
- Bmjopen 2016 012293Документ8 страницBmjopen 2016 012293Jejem Marandra EmkamasОценок пока нет
- Endovascular Vs Medical Management of Acute Ischemic StrokeДокумент9 страницEndovascular Vs Medical Management of Acute Ischemic StrokeJejem Marandra EmkamasОценок пока нет
- Jurnal HemoroidДокумент9 страницJurnal HemoroidJejem Marandra EmkamasОценок пока нет
- Adb RedyДокумент10 страницAdb RedyJejem Marandra EmkamasОценок пока нет
- Journal Severe Traumatic InjuryДокумент27 страницJournal Severe Traumatic InjuryMarcha FerraОценок пока нет
- Azithromycin in Labor LowersДокумент7 страницAzithromycin in Labor LowersJejem Marandra EmkamasОценок пока нет
- Critical Care Management of Severe Traumatic Brain Injury in AdultsДокумент15 страницCritical Care Management of Severe Traumatic Brain Injury in AdultsMohd Faie RamliОценок пока нет
- TB in Pregnancy - 4Документ8 страницTB in Pregnancy - 4fadlydrОценок пока нет
- Jurnal MGSO4Документ23 страницыJurnal MGSO4Jejem Marandra EmkamasОценок пока нет
- Adb RedyДокумент10 страницAdb RedyJejem Marandra EmkamasОценок пока нет
- Journal Reading MgSO4Документ12 страницJournal Reading MgSO4Jejem Marandra EmkamasОценок пока нет
- Bilevel VentilationДокумент18 страницBilevel VentilationBonehead7Оценок пока нет
- Sydney System For The Classification of Chronic GastritisДокумент8 страницSydney System For The Classification of Chronic GastritisJuniorОценок пока нет
- Laboratory Tests To Evaluate Fluid StatusДокумент52 страницыLaboratory Tests To Evaluate Fluid StatusLester Exconde Alfonso0% (1)
- NCP Alleine PregnantДокумент2 страницыNCP Alleine PregnantAlleine YvethОценок пока нет
- International Journal of Surgery Case ReportsДокумент4 страницыInternational Journal of Surgery Case Reportshussein_faourОценок пока нет
- Performance of PRISM III and PELOD-2 Score in A PICUДокумент6 страницPerformance of PRISM III and PELOD-2 Score in A PICUAnantaBenvenutoОценок пока нет
- Perspektif Pasien Dan Manajemen Tentang Mutu Pelayanan IGDДокумент10 страницPerspektif Pasien Dan Manajemen Tentang Mutu Pelayanan IGDBenn TennОценок пока нет
- Truth Telling To Terminally Ill Patients To Tell or Not To Tell 2155 9627 4 159 PDFДокумент2 страницыTruth Telling To Terminally Ill Patients To Tell or Not To Tell 2155 9627 4 159 PDFJeffrey ViernesОценок пока нет
- Physical and DiagnosticДокумент20 страницPhysical and DiagnosticHaziq MarsОценок пока нет
- Journal Ivp-WPS OfficeДокумент8 страницJournal Ivp-WPS OfficeDyahtripОценок пока нет
- Definition of Aquatic ExerciseДокумент3 страницыDefinition of Aquatic Exercisevenkata ramakrishnaiahОценок пока нет
- Manuel Zwecker, MD: Department of Neurological Rehabilitation, Sheba Medical Center, Tel HashomerДокумент61 страницаManuel Zwecker, MD: Department of Neurological Rehabilitation, Sheba Medical Center, Tel Hashomerzwecker4458Оценок пока нет
- Ectopic and Molar PregnancyДокумент22 страницыEctopic and Molar Pregnancyapi-381845148Оценок пока нет
- Pe StressДокумент50 страницPe StressAngelica OrbizoОценок пока нет
- SIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDДокумент54 страницыSIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDMahendra PrasetyoОценок пока нет
- Biological Explanations of Aggression: Sychology ActsheetsДокумент4 страницыBiological Explanations of Aggression: Sychology ActsheetsAyse Kerim100% (1)
- Dinoprostone GelДокумент7 страницDinoprostone GelSahil AliОценок пока нет
- Boy: - 2. Bus: - 3. Box: - 4. Mouse: - 5. Child: - 6. BabyДокумент3 страницыBoy: - 2. Bus: - 3. Box: - 4. Mouse: - 5. Child: - 6. BabyMurni Abu BakarОценок пока нет