Академический Документы
Профессиональный Документы
Культура Документы
Trigeminal Neuralgia: Quick Recertific Ation Series
Загружено:
sarahsamalia0 оценок0% нашли этот документ полезным (0 голосов)
24 просмотров2 страницыTrigeminal Neuralgia
Оригинальное название
10.1097@01.JAA.0000511034.41821.df
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документTrigeminal Neuralgia
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
24 просмотров2 страницыTrigeminal Neuralgia: Quick Recertific Ation Series
Загружено:
sarahsamaliaTrigeminal Neuralgia
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 2
QUICK RECERTIFICATION SERIES
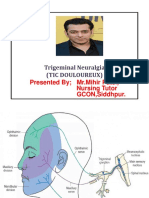
Trigeminal neuralgia
Lindsay Gietzen, MS, PA-C
GENERAL FEATURES found unless the patient is checked immediately after a
• Also known as tic douloureux burst of pain; observe for areas of the face that are neglected
• Characterized by episodic unilateral facial pain in one • Any jaw or facial weakness or dysphagia suggests another
or more of the divisions of the trigeminal nerve (cranial cause
nerve V)
¡ Ophthalmic nerve (V1) provides sensation to the fore- DIAGNOSIS
head and eyes • Thorough history and physical examination
¡ Maxillary nerve (V2) provides sensation to the cheeks, • The diagnostic test of choice is MRI of the brain with
upper lip, and roof of the mouth and without contrast to exclude tumors and assess for
¡ Mandibular nerve (V3) provides sensation to the jaw causes of compression of the trigeminal nerve
and lower lip and provides movement of the muscles • Diagnostic criteria for trigeminal neuralgia developing
involved in biting, chewing, and swallowing without apparent cause other than neurovascular com-
• Idiopathic but believed to be the result of compression pression, according to the International Classification of
of the trigeminal nerve by a vessel or lesion Headache Disorders, 3rd edition:
• Most commonly affects women; typical onset is ages 60 ¡ Criterion A: At least three attacks of unilateral facial
to 70 years pain fulfilling criteria B and C
• More commonly affects the right side of the face ¡ Criterion B: Occurring in one or more divisions of the
• High incidence in patients with multiple sclerosis trigeminal nerve, with no radiation beyond the tri-
• Exacerbations most commonly occur in the fall and spring geminal distribution
¡ Criterion C: Pain has at least three of the following
CLINICAL ASSESSMENT four characteristics:
• The differential diagnosis includes postherpetic neuralgia, t Recurring in paroxysmal attacks lasting from a frac-
cluster headache, temporomandibular joint disorder, and tion of a second to 2 minutes
dental abscess
• Patients commonly complain of an unrelenting sinus pain
or toothache lasting for hours, triggered by moving the QUESTIONS
jaw or drinking fluids 1. A 60-year-old woman presents to the office with
• Patients may complain of electrical, shock-like pain that complaints of episodic stabbing, electrical pain that
begins to fade within seconds, only to give way to a courses down the right jawline. The pain started 3
burning ache lasting seconds to minutes months ago and is triggered by chewing or talking.
• History should focus on pain localization, quality, fre- She recently went to the dentist and had a normal
quency, and triggers (such as touching the skin lightly, examination. Her neurologic examination also is
washing, shaving, brushing teeth, blowing the nose, normal. What is the first-line medication to consider in
drinking hot or cold beverages, encountering a light this patient?
breeze, applying makeup, smiling, or talking) a. acyclovir
• Patients may be afraid of stimulating a trigger point dur- b. carbamazepine
ing the physical examination c. ibuprofen
• Physical examination typically reveals normal findings on d. hydrocodone
the neurologic examination; sensory loss typically is not
2. Which of the following is an expected physical
Lindsay Gietzen is an assistant professor and clinical coordinator in
examination finding in a patient with trigeminal
the PA program at Wayne State University in Detroit, Mich. The author neuralgia?
has disclosed no potential conflicts of interest, financial or otherwise. a. facial weakness
Dawn Colomb-Lippa, MHS, PA-C, department editor b. jaw weakness
DOI:10.1097/01.JAA.0000511034.41821.df
c. dysphagia
d. unrelenting pain triggered by moving the jaw
Copyright © 2017 American Academy of Physician Assistants
46 www.JAAPA.com Volume 30 • Number 1 • January 2017
Copyright © 2017 American Academy of Physician Assistants
Trigeminal neuralgia
t Severe intensity ¡ Risks of surgical management include permanent facial
t Electric shock-like, shooting, stabbing, or sharp in anesthesia and anesthesia dolorosa
quality • Trigeminal neuralgia may evolve into a chronic pain
t Precipitated by innocuous stimuli to the affected side syndrome because of its high rate of recurrence after
of the face treatment. Patients also may suffer from depression and
¡ Criterion D: No clinically evident neurologic deficit related loss of daily function.
¡ Criterion E: Not better accounted for by another • Patients may choose to limit activities that cause pain,
International Classification of Headache Disorders such as chewing, which could lead to weight loss in
diagnosis extreme circumstances. JAAPA
TREATMENT cause of pain.
• Medical management Facial or jaw weakness or dysphagia suggests another
¡ Carbamazepine drinking fluids is characteristic of trigeminal neuralgia.
¡ Gabapentin (most effective for patients with multiple 2. D. Unrelenting pain triggered by moving the jaw or
sclerosis) neuralgia.
¡ Also consider pregabalin, phenytoin, lamotrigine,
are not effective in treating pain related to trigeminal
valproic acid, tricyclic antidepressants hydrocodone would not be appropriate because they
• Surgical management of trigeminal neuralgia. Acyclovir, ibuprofen, and
¡ Microvascular decompression (about an 80% success antidepressants can be used for medical management
rate, but most invasive option) phenytoin, lamotrigine, valproic acid, and tricyclic
¡ Percutaneous procedures, such as balloon compression, 1. B. Carbamazepine, gabapentin, pregabalin,
glycerol rhizotomy, and radiofrequency thermocoagu-
lation (high rate of recurrent pain) Answers
¡ Gamma knife radiosurgery (about a 75% success rate)
JAAPA Journal of the American Academy of Physician Assistants www.JAAPA.com 47
Copyright © 2017 American Academy of Physician Assistants
Вам также может понравиться
- Mendoza Outline of DiseasesДокумент28 страницMendoza Outline of DiseasesAleks MendozaОценок пока нет
- Management Trigeminal NeuralgiaДокумент28 страницManagement Trigeminal NeuralgiaApeksha JadhavОценок пока нет
- B. Wayne Blount, MD, MPHДокумент28 страницB. Wayne Blount, MD, MPHSanjaya Deeptha ThennakoonОценок пока нет
- Trigeminal Neuralgia (Tic Douloureux)Документ49 страницTrigeminal Neuralgia (Tic Douloureux)Mohsin HabibОценок пока нет
- TrigeminalNeuralgiaPracticeEssentials, Background, Anatomy 1700148132569Документ9 страницTrigeminalNeuralgiaPracticeEssentials, Background, Anatomy 1700148132569esthersilingi12Оценок пока нет
- Trigeminal Neuralgia Outline ScriptДокумент4 страницыTrigeminal Neuralgia Outline ScriptRogerQuxОценок пока нет
- Orofacial Pain KhojaДокумент79 страницOrofacial Pain Khojashamshada2000Оценок пока нет
- Trigeminal Neuralgia: DR Tay Kwang Hui Dept of Anaesthesia 08 January 2011Документ40 страницTrigeminal Neuralgia: DR Tay Kwang Hui Dept of Anaesthesia 08 January 2011Shalim BagusОценок пока нет
- Trigeminal Neuralgia Recent Approach in ClassificaДокумент9 страницTrigeminal Neuralgia Recent Approach in ClassificaFKUPR 2017Оценок пока нет
- Trigeminal NeuralgiaДокумент27 страницTrigeminal Neuralgiamelencio olivasОценок пока нет
- Migraine and The Scope of HomeopathyДокумент6 страницMigraine and The Scope of HomeopathyDiego RodriguezОценок пока нет
- Trigeminal Neuralgia: Rowena R. Tosoc RN, PHDДокумент54 страницыTrigeminal Neuralgia: Rowena R. Tosoc RN, PHDMARICRIS NEBIARОценок пока нет
- Trigeminal NeuralgiaДокумент5 страницTrigeminal Neuralgiawidad syairoziОценок пока нет
- Trigeminal Neuralgia: Dr. Deepthi AthuluruДокумент69 страницTrigeminal Neuralgia: Dr. Deepthi AthuluruLakshya NainОценок пока нет
- Migraine Headache Prophylaxis - American Family PhysicianДокумент16 страницMigraine Headache Prophylaxis - American Family Physiciando leeОценок пока нет
- What Is Trigeminal Neuralgia?Документ4 страницыWhat Is Trigeminal Neuralgia?Tiger_2011Оценок пока нет
- Management of Neurologic ConditionsДокумент193 страницыManagement of Neurologic ConditionsAnna ReyesОценок пока нет
- Trigeminal NeuralgiaДокумент6 страницTrigeminal NeuralgiamimirkuОценок пока нет
- Trigeminal NeuralgiaДокумент72 страницыTrigeminal NeuralgiaCocoMathewОценок пока нет
- NCP AccДокумент19 страницNCP AccAthyrah KadirОценок пока нет
- Rehabilitation of Patients Suffering Trigeminal Nerve NeuragiaДокумент22 страницыRehabilitation of Patients Suffering Trigeminal Nerve NeuragiacosornoОценок пока нет
- Neuralgia TrigeminalДокумент5 страницNeuralgia TrigeminalcantikarevieraОценок пока нет
- Trigeminal Neuralgia (Facial Pain)Документ6 страницTrigeminal Neuralgia (Facial Pain)Aisyah AlviОценок пока нет
- Orofacial Pain: DR Samreen Younas Pgr-I (FCPS) OmfsДокумент49 страницOrofacial Pain: DR Samreen Younas Pgr-I (FCPS) OmfsmishaОценок пока нет
- HeadacheДокумент33 страницыHeadacheMpanso Ahmad AlhijjОценок пока нет
- Jurnal RadaДокумент3 страницыJurnal RadaMuh Ridho AkbarОценок пока нет
- Practice: A 32-Year-Old Woman With HeadacheДокумент2 страницыPractice: A 32-Year-Old Woman With HeadacheFeliОценок пока нет
- Trigeminal NeuralgiaДокумент3 страницыTrigeminal NeuralgiaAira Alaro50% (2)
- Nerve InjuriesДокумент22 страницыNerve InjuriesFuture DentОценок пока нет
- Finseth PPT ReviewДокумент206 страницFinseth PPT ReviewTracy NwanneОценок пока нет
- Trigeminal Neuralgia: Amithbabu.C.B Mscd-EndoДокумент18 страницTrigeminal Neuralgia: Amithbabu.C.B Mscd-EndoDR.AMITHBABU.C.BОценок пока нет
- DaweДокумент41 страницаDawemichaelwillsonОценок пока нет
- Chapter 16 - HeadacheДокумент7 страницChapter 16 - HeadacheSerious LeoОценок пока нет
- Jurnal Trigeminal Neuralgia 1Документ12 страницJurnal Trigeminal Neuralgia 1nabilla putriОценок пока нет
- Lapsus Ablasi Radiofrekuensi Pada Neuralgia Trigeminal Dengan Panduan FluoroskopiДокумент8 страницLapsus Ablasi Radiofrekuensi Pada Neuralgia Trigeminal Dengan Panduan FluoroskopivalenciaОценок пока нет
- Trigeminal Neuralgia Overview: Sleep Anxiety Depression Malnutrition SuicidalДокумент57 страницTrigeminal Neuralgia Overview: Sleep Anxiety Depression Malnutrition SuicidalAmy Rose EugenioОценок пока нет
- Trigeminal NeuralgiaДокумент35 страницTrigeminal NeuralgiaMahad abuukarОценок пока нет
- Diseases of Nerves and MusclesДокумент46 страницDiseases of Nerves and MusclesAME DENTAL COLLEGE RAICHUR, KARNATAKAОценок пока нет
- Management of Intracranial Pain: Aliah Shivaan I Sara Anne William Sailo Aisyah Jayson Yuen Alice Hafizah Archan AДокумент63 страницыManagement of Intracranial Pain: Aliah Shivaan I Sara Anne William Sailo Aisyah Jayson Yuen Alice Hafizah Archan AWilliam OngОценок пока нет
- Migrraine Review 2017 NEJMДокумент9 страницMigrraine Review 2017 NEJManscstОценок пока нет
- Trigeminal NeuralgiaДокумент15 страницTrigeminal NeuralgiaMihir Patel75% (4)
- Journal of The American Academy of Physician Assistants Volume 30 Issue 12 2017 (Doi 10.1097/01.JAA.0000526785.27024.Bb) Gelbart, David - TetanusДокумент2 страницыJournal of The American Academy of Physician Assistants Volume 30 Issue 12 2017 (Doi 10.1097/01.JAA.0000526785.27024.Bb) Gelbart, David - TetanusPutri YunandaОценок пока нет
- Facialpain 150204113108 Conversion Gate01Документ51 страницаFacialpain 150204113108 Conversion Gate01Muhammad IrfanОценок пока нет
- Differentiating Trigeminal Neuropathy From Trigeminal NeuralgiaДокумент11 страницDifferentiating Trigeminal Neuropathy From Trigeminal NeuralgiaGarryОценок пока нет
- Trigeminal Neuralgia - A Practical GuideДокумент12 страницTrigeminal Neuralgia - A Practical Guide전영우Оценок пока нет
- BMJ 39085 614792 BeДокумент5 страницBMJ 39085 614792 BeSaranya MohanОценок пока нет
- Trigeminal Neuralgia (Tic Douloureux) : Presented by MR - Mihir Patel, Nursing Tutor GCON, SiddhpurДокумент15 страницTrigeminal Neuralgia (Tic Douloureux) : Presented by MR - Mihir Patel, Nursing Tutor GCON, Siddhpurandreas kevinОценок пока нет
- Manajemen NyeriДокумент33 страницыManajemen NyeriEL SHITAОценок пока нет
- Acc 61 - Supp2 96Документ7 страницAcc 61 - Supp2 96intermediosamberesОценок пока нет
- GYLLE Meningitis Otitis Media Pertussis Pneumonia Rotavirus 1Документ37 страницGYLLE Meningitis Otitis Media Pertussis Pneumonia Rotavirus 1Marie Ashley CasiaОценок пока нет
- Lambru2021 2Документ12 страницLambru2021 2Deyvid CapeloОценок пока нет
- Algoritma Neck PainДокумент12 страницAlgoritma Neck PainAri SudarsonoОценок пока нет
- Neuralgia Trigeminal-EnglishДокумент29 страницNeuralgia Trigeminal-EnglishUcc Ang BangarenОценок пока нет
- Question Examples: (Updated July 2012)Документ17 страницQuestion Examples: (Updated July 2012)Galgalo GarbichaОценок пока нет
- Case 1Документ12 страницCase 1Denisa-Alexandra MănăstireanuОценок пока нет
- Wilhour-Nahas2018 Article The NeuralgiasДокумент8 страницWilhour-Nahas2018 Article The NeuralgiasCamilo Benavides BurbanoОценок пока нет
- Cranial Neuralgia Keynote PDFДокумент21 страницаCranial Neuralgia Keynote PDFRuki HartawanОценок пока нет
- Trigeminal NeurlgiaДокумент5 страницTrigeminal NeurlgiaAnonymous V1tCwPHlDОценок пока нет
- A Simple Guide to Neuralgia and Related Nerve DisordersОт EverandA Simple Guide to Neuralgia and Related Nerve DisordersРейтинг: 5 из 5 звезд5/5 (5)
- What Is An Office Hysteroscopy?Документ4 страницыWhat Is An Office Hysteroscopy?ericОценок пока нет
- 0003489414532777Документ10 страниц0003489414532777Lilia ScutelnicОценок пока нет
- Taylor Tofil MSN, APRN-CNPДокумент4 страницыTaylor Tofil MSN, APRN-CNPapi-620258967Оценок пока нет
- Sutures and Suturing PDFДокумент56 страницSutures and Suturing PDFFrederick Alexander Trisna0% (1)
- Anna Aabakke - AfhandlingДокумент63 страницыAnna Aabakke - AfhandlingFebyan AbotОценок пока нет
- Self Study Intraoral Anatomy RadiologyДокумент80 страницSelf Study Intraoral Anatomy RadiologydeenmОценок пока нет
- Comparison of Hydrocephalus Outcome Questionnaire Scores To Neuropsychological Test Performance in School-Aged ChildrenДокумент6 страницComparison of Hydrocephalus Outcome Questionnaire Scores To Neuropsychological Test Performance in School-Aged ChildrenAnnisa HasnaОценок пока нет
- Current Diagnosis Treatment Pediatrics 24Th Edition Edition William Hay Full ChapterДокумент67 страницCurrent Diagnosis Treatment Pediatrics 24Th Edition Edition William Hay Full Chapterbill.groff554100% (4)
- Gingival Esthetics in PeriodonticsДокумент20 страницGingival Esthetics in PeriodonticsKoyyalamudi PrudhviОценок пока нет
- Watson and Raynor 1920Документ9 страницWatson and Raynor 1920ShaneLee10267% (3)
- Jurnal CT ScanДокумент9 страницJurnal CT ScanPungki Putra TamaraОценок пока нет
- HEYER VizOR - Product List - en 0314 2Документ7 страницHEYER VizOR - Product List - en 0314 2kalandorka92Оценок пока нет
- Azithromycin Monograph - PaediatricДокумент7 страницAzithromycin Monograph - PaediatrictynОценок пока нет
- Ilizarov Technique For Complex Foot and Ankle Deformities Oxidative Stress Amp DiseaseДокумент476 страницIlizarov Technique For Complex Foot and Ankle Deformities Oxidative Stress Amp DiseaseSathyadharan Paneer100% (4)
- Apocrine Breast LesionsДокумент7 страницApocrine Breast LesionscandiddreamsОценок пока нет
- Atlas of Oral Diseases 2016Документ198 страницAtlas of Oral Diseases 2016Desi Sri Astuti100% (1)
- 1 Apgar and MMDST 1Документ34 страницы1 Apgar and MMDST 1Abigail BrillantesОценок пока нет
- Anatomy MCQДокумент23 страницыAnatomy MCQPirabakar Mahendran100% (3)
- Community Acquired Pneumonia in Malaysia PDFДокумент2 страницыCommunity Acquired Pneumonia in Malaysia PDFCassОценок пока нет
- Diabetes Ebook:Diabetes Damages and TreatmentsДокумент358 страницDiabetes Ebook:Diabetes Damages and TreatmentsHealthCareОценок пока нет
- Developmental Dysplasia of The HipДокумент5 страницDevelopmental Dysplasia of The HipMavra zОценок пока нет
- Presentation of Neurogenic Shock Within The Emergency Department - TaylorДокумент6 страницPresentation of Neurogenic Shock Within The Emergency Department - TaylorAnprtma kaunangОценок пока нет
- Nephrotic Case Study With AnswersДокумент3 страницыNephrotic Case Study With AnswersKBОценок пока нет
- Hirschprung Associated EnterocolitisДокумент9 страницHirschprung Associated Enterocolitiskeyla_shineeeОценок пока нет
- Poliomyelitis Disease Investigation GuidelineДокумент11 страницPoliomyelitis Disease Investigation Guidelineaikohama89Оценок пока нет
- 26 Lessons Learned As A NurseДокумент2 страницы26 Lessons Learned As A NurseAnthonyBernardoAbustanОценок пока нет
- A Review of Maxillary Expansion in Relation To Rate of Expansion and Patient's AgeДокумент6 страницA Review of Maxillary Expansion in Relation To Rate of Expansion and Patient's AgeParameswaran ManiОценок пока нет
- Arch Width and Form - A ReviewДокумент9 страницArch Width and Form - A ReviewMafe SalazarОценок пока нет
- Al Ameen Medical CollegeДокумент13 страницAl Ameen Medical CollegeRakeshKumar1987Оценок пока нет
- MBBS Enrolment Cheat Sheet - Year 6Документ2 страницыMBBS Enrolment Cheat Sheet - Year 6Tom JОценок пока нет