Академический Документы
Профессиональный Документы
Культура Документы
UTI Treatment Guidelines PDF
Загружено:
Muhammad IhsanuddinИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
UTI Treatment Guidelines PDF
Загружено:
Muhammad IhsanuddinАвторское право:
Доступные форматы
Guidelines for the Diagnosis and Management of Urinary Tract Infections
6/1/2017
When to treat with antibiotics:
BOTH symptoms and microbiologic criteria must be present in order to diagnose UTI1. (See algorithm for
diagnosis and treatment of UTI at end of document)
Microbiologic criteria Symptom criteria*
Positive urinalysis (WBC≥ Acute dysuria
10/HPF) and --OR--
Positive urine culture¥ Fever† + at least 1 of following (new or worsening):*
(≥105 cfu/mL in voided If no fever, 2 of the following (new or worsening)
No specimen) Urinary urgency
indwelling AND Frequency
catheter
Suprapubic pain
Gross hematuria
Costovertebral angle tenderness
Urinary incontinence
Positive urinalysis (WBC≥ At least 1 of the following (new or worsening):
10/HPF) and Fever†
Positive urine culture (≥103 Costovertebral angle (CVA) tenderness
cfu/mL) AND Rigors (shaking chills)
Indwelling
Delirium
catheterǂ
Flank pain (back, side pain)
pelvic discomfort
Acute hematuria
Malaise or lethargy with no other cause
*New onset delirium is NOT a symptomatic criterion of a UTI for patients without an indwelling catheter
† Fever: >37.9ºC [100ºF] or 1.5ºC [2.4ºF] increase above baseline temperature
¥ Some use a lower colony count cut off of 102CFU/mL in a specimen collected by in and out catheter
ǂ If catheter in place for >2 weeks, change catheter before obtaining a urine sample for culture
Treatment:
Definitions
Uncomplicated UTI – infection in a structurally/functionally normal urinary tract.
Complicated UTI – patients with a structural or functional abnormality of the urinary tract.
Lower UTI – UTI without involvement of the kidneys (whether complicated or uncomplicated)
Upper UTI/pyelonephritis – infection of the kidney. Signs/symptoms = flank pain, fever.
Empiric therapy
Local antibiotic resistance should guide empiric treatment choice; a use of a facility specific
antibiogram recommended.
E. coli is the most common organism isolated from urine cultures in the nursing home
population.
Consider resident’s prior urine culture results when starting empiric treatment.
Funded by The New York State Department of Health
Severely ill patients (high fever, shaking chills, hypotension, etc.)
Agent Notes
Can be used safely in patients with mild penicillin
1st line Ceftriaxone
allergy (i.e. rash), cross-reactivity very low2
ONLY in patients who need parenteral therapy and have
nd
2 line Gentamicin severe IgE mediated penicillin allergy
Significant nephrotoxicity/ototoxicity concerns
Cystitis*/Lower UTI (complicated or uncomplicated)
Agent Notes
Most active agent against E. coli
Avoid if CrCl < 30 mL/min
Nitrofurantoin Avoid if systemic signs of infection/suspicion of
pyelonephritis or prostatitis
Does not cover Proteus
1st line Do not use for empiric treatment if resistance >20%
Drug-drug interactions with warfarin
Monitor potassium level if concomitant use of
TMP-SMX
spironolactone, angiotensin-converting enzyme
inhibitors (ACEIs), angiotensin receptor blockers (ARBs)
Renal dose adjustments, avoid if CrCl < 15 mL/min
2nd line Cephalexin Active against E. coli, Proteus, and Klebsiella
Active against E. coli, Enterococcus. Is also active
3rd line Fosfomycin† against ESBL positive E. coli. Fosfomycin susceptibility
tests recommended.
Pyelonephritis/ Upper UTI
Agent Notes
Patient should receive 1 dose of IV/IM ceftriaxone prior
st
1 line TMP-SMX to starting oral therapy
Do not use for empiric treatment if resistance >20%
2nd line Ciprofloxacin If patient unable to tolerate Bactrim
Data suggests that oral beta-lactams are inferior to
Bactrim or fluoroquinolones for pyelonephritis3
3rd line Beta-lactams
Initial dose of IV/IM ceftriaxone and longer treatment
duration of 10-14 days are recommended
*Due to high levels of resistance in E. coli and high risk of C. diff infection, fluoroquinolones should be
avoided for empiric therapy of cystitis
†Fosfomycin has poor insurance coverage
Streamlined therapy (pending susceptibility results)
Organism Recommended antimicrobials
Candida Usually responds to replacement of urinary catheter without antifungal therapy
Citrobacter Nitrofurantoin, TMP-SMX
E. coli Nitrofurantoin, TMP-SMX
Enterobacter TMP-SMX, ciprofloxacin
Enterococcus Nitrofurantoin, amoxicillin
Klebsiella TMP-SMX, cephalexin
Proteus TMP-SMX, cephalexin
Pseudomonas Ciprofloxacin
Funded by The New York State Department of Health
Targeted therapy
Most narrow agent to which the organism is susceptible should be selected
Above empiric agents are still preferred if organism is susceptible
Fluoroquinolones should be avoided for uncomplicated cystitis unless there are no other options
Empiric antibiotics should be discontinued if urine culture is negative.
Dosing
Drug Dose Renal adjustment
Amoxicillin 500mg PO TID CrCl 10-50 mL/min: 500mg BID
CrCl < 10 mL/min: 500mg once daily
Ceftriaxone 1g IM/IV q24h None
Cefpodoxime 100mg PO BID (cystitis) CrCl < 30 mL/min: Administer once daily
200mg PO BID (pyelonephritis)
Cephalexin 500mg PO BID (cystitis) CrCl 10-50 mL/min: max dose 500mg TID
500mg PO QID (complicated) CrCl < 10 mL/min: 500mg once daily
Ciprofloxacin 250mg PO BID (uncomplicated cystitis) CrCl < 30 mL/min: Administer once daily
500mg PO BID (pyelonephritis)
400mg IV BID (severely ill)
Doxycycline 100mg PO BID None
Fluconazole 200mg PO once daily CrCl < 50 mL/min: 100mg once daily
Gentamicin* ≤ 60kg: 60mg IM/IV q24h CrCl < 30 mL/min: use caution, may need
61-80kg: 80mg IM/IV q24h prolonged dosing intervals
≥81kg: 100-120mg IM/IV q24h (1
mg/kg)
Levofloxacin 250mg PO q24h (cystitis) None
750mg PO p 24hrs (pyelonephritis) CrCl< 20-49 mL/min 750 mg q 48 hrs
CrCl 10-20 mL 750 mg then 500 mq q 48
hrs
Nitrofurantoin 100mg PO BID CrCl < 30 mL/min: avoid4-5
(Macrobid)
TMP-SMX 1 SS tab bid (preferred in older adults) CrCl 15-30 mL/min: 1 DS tab once daily
1 DS tab (800-160mg) PO BID (for --OR-- 1 SS tab BID
normal CrCL) CrCl < 15 mL/min: avoid
Fosfomycin 3-g sachet in a single dose None
3 g sachet every 48-72 hours for
complicated UTI
Duration of therapy
Lower UTI/Cystitis3,6:
o Bactrim or fluoroquinolones: 3 days
o Nitrofurantoin, β lactam: 5 days
Upper UTI/Pyelonephritis6,7:
o 7 days if patient improves rapidly
o 10-14 days if patient has delayed response
Catheter related UTI2:
o 7 days if rapid improvement
o 10-14 days if delayed response
Funded by The New York State Department of Health
References
1. Loeb M, Bentley DW, Bradley S, et al. Development of minimum criteria for the initiation of
antibiotics in residents of long-term-care facilities: results of a consensus conference. Infection control
and hospital epidemiology : the official journal of the Society of Hospital Epidemiologists of America
2001;22:120-4
2. Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-
associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the
Infectious Diseases Society of America. Clin Infect Dis 2010;50:625-663
2. Campagna JD, Bond MC, Schabelman E, Hayes BD. The use of cephalosporins in penicillin-allergic
patients: a literature review. The Journal of emergency medicine 2012;42:612-20
3. Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of
acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases
Society of America and the European Society for Microbiology and Infectious Diseases. Clinical infectious
diseases : an official publication of the Infectious Diseases Society of America 2011;52:e103-20
4. Oplinger M, Andrews CO. Nitrofurantoin contraindication in patients with a creatinine clearance
below 60 mL/min: looking for the evidence. The Annals of pharmacotherapy 2013;47:106-11.5
5. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use
in Older Adults. JAGS 2015
6. Nicolle LE. Urinary tract infection in the elderly Clin Geriatr Med 2009 (25): 423-436
7. Drekonja EM et al. Urinary Tract Infection in Male Veterans Treatment Patterns and Outcomes. JAMA
Intern Med. 2013; 173(1):62-68
8. Crnich CJ, Drinka P. Improving the Management of Urinary Tract Infections in Nursing Homes: It’s
Time to Stop the Tail From Wagging the Dog.
http://www.managedhealthcareconnect.com/article/improving-management-urinary-tract-infections-
nursing-homes-it-s-time-stop-tail-wagging-dog
Funded by The New York State Department of Health
Crnich CJ et al. (reference 8)
Funded by The New York State Department of Health
Вам также может понравиться
- Shivani PDFДокумент3 страницыShivani PDFdeepukumarОценок пока нет
- Ulcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsОт EverandUlcerative Colitis, A Simple Guide To The Condition, Treatment And Related ConditionsОценок пока нет
- UTI GuidelineДокумент10 страницUTI Guidelinecatalin petreОценок пока нет
- Adult Infectious Disease Bulletpoints HandbookОт EverandAdult Infectious Disease Bulletpoints HandbookРейтинг: 4.5 из 5 звезд4.5/5 (9)
- Urinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideДокумент5 страницUrinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideLaoMed plusОценок пока нет
- UTI Guideline Example 2 Appendix B PDFДокумент4 страницыUTI Guideline Example 2 Appendix B PDFamira catriОценок пока нет
- Gamutin Drug Study-PediatricsДокумент6 страницGamutin Drug Study-PediatricsJhulia GamutinОценок пока нет
- Generic NameДокумент8 страницGeneric Namemel aquinoОценок пока нет
- Urinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of MedicineДокумент25 страницUrinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of Medicineولاء إبراهيمОценок пока нет
- Infeksi Saluran Kemih: Oleh Hendra Santoso Pembimbing Dr. Hasnawaty SP - OGДокумент22 страницыInfeksi Saluran Kemih: Oleh Hendra Santoso Pembimbing Dr. Hasnawaty SP - OGHendra SantosoОценок пока нет
- UTI Treatment Algorithm - Sharp Mesa Vista 2Документ3 страницыUTI Treatment Algorithm - Sharp Mesa Vista 2Fitri 1997Оценок пока нет
- Acute Uncomplicated PyelonephritisДокумент5 страницAcute Uncomplicated PyelonephritisoreaОценок пока нет
- UTI TreatmentДокумент3 страницыUTI TreatmentMaria RezitadinaОценок пока нет
- BCCA AB in Febrile Neutropenia GuidelinesДокумент2 страницыBCCA AB in Febrile Neutropenia GuidelinesAlvy SyukrieОценок пока нет
- Urological InfectionsДокумент21 страницаUrological Infections<_>Оценок пока нет
- Urinary Tract Infections (UTI) in Older Adults WWW - Rxfiles.caДокумент7 страницUrinary Tract Infections (UTI) in Older Adults WWW - Rxfiles.caAwais KhanОценок пока нет
- Zinnat PIДокумент10 страницZinnat PIfsdfОценок пока нет
- UTI in ElderlyДокумент18 страницUTI in ElderlyBarkahafrilian100% (1)
- Literature Review On UTIДокумент31 страницаLiterature Review On UTINishchal Dhakal0% (1)
- 17 Urological InfectionsДокумент18 страниц17 Urological InfectionsntadudulОценок пока нет
- Pathophysiology of Pyelonephritis: How It HappensДокумент6 страницPathophysiology of Pyelonephritis: How It HappensReno Jun NagasanОценок пока нет
- Malaria and LeptospirosisДокумент18 страницMalaria and LeptospirosisRasYa DIОценок пока нет
- Uti TreatmentДокумент4 страницыUti TreatmentAnne OhОценок пока нет
- Antibiotka PicuДокумент4 страницыAntibiotka Picusunu rachmat100% (1)
- Antibiotik Dan Antiseptik Saluran KemihДокумент29 страницAntibiotik Dan Antiseptik Saluran KemihPutri Sari SeptirianiОценок пока нет
- IMG EmpAposterДокумент1 страницаIMG EmpAposterChiu LeoОценок пока нет
- Cefuroxime Inhibits Bacterial Cell Wall Synthesis by Binding To One 1 or More of The Penicillin-Binding Proteins (PBPS) WhichДокумент12 страницCefuroxime Inhibits Bacterial Cell Wall Synthesis by Binding To One 1 or More of The Penicillin-Binding Proteins (PBPS) WhichMr rawrОценок пока нет
- Comprehension of Acute PyelonephritisДокумент23 страницыComprehension of Acute PyelonephritisAmeliaОценок пока нет
- Comprehension of Acute PyelonephritisДокумент23 страницыComprehension of Acute PyelonephritisAmeliaОценок пока нет
- ErythromycinДокумент2 страницыErythromycinBtob meloОценок пока нет
- University of Maryland Medical Center Fluconazole (Diflucan®)Документ6 страницUniversity of Maryland Medical Center Fluconazole (Diflucan®)damondouglasОценок пока нет
- Urinary Tract InfectionДокумент24 страницыUrinary Tract InfectionZaki Achmad NhrОценок пока нет
- Treatment of Urinary Tract Infections PDFДокумент24 страницыTreatment of Urinary Tract Infections PDFGoutham MОценок пока нет
- Pharmacotherapy of Urinary Tract InfectionДокумент75 страницPharmacotherapy of Urinary Tract InfectionMariana CreciunОценок пока нет
- NCLEX REVIEW AntibioticsДокумент7 страницNCLEX REVIEW Antibioticsneonstar100% (1)
- Antimicrobial Dosage Adjustments in Renal Impairment For FormularyДокумент20 страницAntimicrobial Dosage Adjustments in Renal Impairment For Formularyangkatanjuli2019Оценок пока нет
- Treatment PDFДокумент6 страницTreatment PDFWorku KifleОценок пока нет
- Urinary Tract InfectionsДокумент28 страницUrinary Tract Infectionsleensaeed26Оценок пока нет
- Sepsis GuidelinesДокумент1 страницаSepsis GuidelinesYezenashОценок пока нет
- Ceftriaxone Drug StudyДокумент1 страницаCeftriaxone Drug StudyEsmareldah Henry SirueОценок пока нет
- Hello Everyone: Prof. (DR.) Akhilesh ShrivastavaДокумент19 страницHello Everyone: Prof. (DR.) Akhilesh Shrivastavaarpitagupta28Оценок пока нет
- EAU Pocket Guidelines On Urological Infections 2021Документ25 страницEAU Pocket Guidelines On Urological Infections 2021Noel Saúl Argüello SánchezОценок пока нет
- Patients With Multiple DisordersДокумент7 страницPatients With Multiple DisordersKathleen Joy PingenОценок пока нет
- Eau Guidelines On Urological Infections: (Limited Text Update March 2020)Документ22 страницыEau Guidelines On Urological Infections: (Limited Text Update March 2020)LUIS MIGUEL CASTILLA MORANОценок пока нет
- Name of Drug: Ceftriaxone 2g/IVДокумент3 страницыName of Drug: Ceftriaxone 2g/IVAllan DiazОценок пока нет
- Antibiotic Policy JIPMER UTIДокумент6 страницAntibiotic Policy JIPMER UTIRpmhouseОценок пока нет
- 2012 Aug IMG Poster 165760a SepsisДокумент1 страница2012 Aug IMG Poster 165760a SepsisTeng Huei LeeОценок пока нет
- EAU Pocket Guidelines Urological Infections 2019Документ22 страницыEAU Pocket Guidelines Urological Infections 2019felixОценок пока нет
- Drug Study GabrielaДокумент4 страницыDrug Study GabrielaNimrodОценок пока нет
- EAU Pocket Guidelines Urological - Infections 2012 PDFДокумент18 страницEAU Pocket Guidelines Urological - Infections 2012 PDFbrukner30Оценок пока нет
- Urinary Tract Infection (UTI) Definitions: PyelonephritisДокумент4 страницыUrinary Tract Infection (UTI) Definitions: PyelonephritisSanthosh KumarОценок пока нет
- UTI Algorithm-Inpatient RQHRДокумент1 страницаUTI Algorithm-Inpatient RQHRDe RadianОценок пока нет
- Prophylaxis Action: Tetanus: Injection: 5 To 10 LF Units ofДокумент10 страницProphylaxis Action: Tetanus: Injection: 5 To 10 LF Units ofElle RosalesОценок пока нет
- Pseudomonas Aeruginosa PfizerДокумент3 страницыPseudomonas Aeruginosa PfizerPutri Kania DewiОценок пока нет
- 8 Urinary Tract InfectionДокумент4 страницы8 Urinary Tract Infectionzainabd1964Оценок пока нет
- Escalation Guide For Gram-Negative Bacteremia StanfordДокумент3 страницыEscalation Guide For Gram-Negative Bacteremia StanfordLuis MedinaОценок пока нет
- Drug Study: Adult: ChildДокумент4 страницыDrug Study: Adult: ChildKristian Karl Bautista Kiw-isОценок пока нет
- Anti - Infectives AgentsДокумент83 страницыAnti - Infectives AgentsRhien Yrah P. CabalongaОценок пока нет
- Bone and Joint Infections BNHFT 2010 PDFДокумент3 страницыBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriОценок пока нет
- Ringkasan Dosis Obat 7th RevisedДокумент38 страницRingkasan Dosis Obat 7th RevisedMuhammad IhsanuddinОценок пока нет
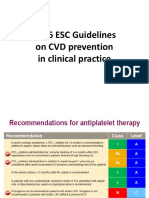
- 2016 ESC Guidelines On CVD Prevention in Clinical PracticeДокумент8 страниц2016 ESC Guidelines On CVD Prevention in Clinical PracticeMuhammad IhsanuddinОценок пока нет
- Referat Airway ManagementДокумент24 страницыReferat Airway ManagementVerarisnaОценок пока нет
- Ipa Belum Di TranslateДокумент5 страницIpa Belum Di TranslateMuhammad IhsanuddinОценок пока нет
- Mechanism Molecular SepsisДокумент4 страницыMechanism Molecular SepsisMuhammad IhsanuddinОценок пока нет
- Tourist Behaviour Unit I & IIДокумент83 страницыTourist Behaviour Unit I & IIRashmiranjanОценок пока нет
- Daftar Nama Dosen Pembimbing Periode 2020-1 PagiДокумент3 страницыDaftar Nama Dosen Pembimbing Periode 2020-1 PagiNufita Twandita DewiОценок пока нет
- Stochastic Frontier Analysis and DEAДокумент3 страницыStochastic Frontier Analysis and DEAHa M ZaОценок пока нет
- Moy Ya Lim Yao vs. Commissioner of ImmigrationG.R. No. L-21289 SCRA 292 DigestДокумент2 страницыMoy Ya Lim Yao vs. Commissioner of ImmigrationG.R. No. L-21289 SCRA 292 DigestKhen Tamdang100% (1)
- Unveiling The Factors Shaping Financial Choices Among Women in The Professional Sphere: An Analytical Framework Utilizing Structural Equation Modeling in Behavioral Finance.Документ17 страницUnveiling The Factors Shaping Financial Choices Among Women in The Professional Sphere: An Analytical Framework Utilizing Structural Equation Modeling in Behavioral Finance.International Journal of Innovative Science and Research TechnologyОценок пока нет
- Aperin TOS Entrepreneurship Grade12Документ2 страницыAperin TOS Entrepreneurship Grade12Arvin Austria AperinОценок пока нет
- Factors Affecting Young People Buying Decision On Green Products: A Case Study in Ho Chi Minh CityДокумент53 страницыFactors Affecting Young People Buying Decision On Green Products: A Case Study in Ho Chi Minh CityBăng BăngОценок пока нет
- The Making of R.A. 1425Документ3 страницыThe Making of R.A. 1425Reje CuaresmaОценок пока нет
- Management QuestionsДокумент5 страницManagement QuestionsAhmedAlhosaniОценок пока нет
- Kyrosoft Technologies: A User Guide & Manual OnДокумент20 страницKyrosoft Technologies: A User Guide & Manual OnjagsmcОценок пока нет
- College Thesis. - BSED - 2022Документ201 страницаCollege Thesis. - BSED - 2022Justin MirandoОценок пока нет
- Detailed Collection of All Synonyms From Cambridge IELTS BooksДокумент78 страницDetailed Collection of All Synonyms From Cambridge IELTS BooksAli Mehdi Maknojia92% (13)
- Team Building Breakout ScriptДокумент12 страницTeam Building Breakout ScriptMelanie PajaronОценок пока нет
- Interest GroupsДокумент25 страницInterest GroupsnikkivОценок пока нет
- English A SbaДокумент13 страницEnglish A Sbacarlton jackson50% (2)
- Unit23 SolutionsДокумент7 страницUnit23 SolutionsAbcОценок пока нет
- Cardiohelp System Brochure-En-Non Us JapanДокумент16 страницCardiohelp System Brochure-En-Non Us JapanAnar MaharramovОценок пока нет
- The Urantia Book (Public Domain)Документ1 806 страницThe Urantia Book (Public Domain)Lenny100% (13)
- Victor M Orozco 8860 SW 123 CT APT K310 Miami FL 33186Документ4 страницыVictor M Orozco 8860 SW 123 CT APT K310 Miami FL 33186Wa Riz LaiОценок пока нет
- Right On 1Документ2 страницыRight On 1Lingva Lingva BinestОценок пока нет
- Sets&StatisticsДокумент6 страницSets&StatisticsFarah AghaverdiyevaОценок пока нет
- Geo5 Fem Theoretical GuideДокумент113 страницGeo5 Fem Theoretical GuideAnonymous 87xpkIJ6CFОценок пока нет
- Meeresstille NotesДокумент5 страницMeeresstille NotesJayOngОценок пока нет
- 12th Bio Botany EM Important Questions English Medium PDF DownloadДокумент7 страниц12th Bio Botany EM Important Questions English Medium PDF DownloadPrase 1815Оценок пока нет
- Applying The Rossiter-Percy Grid To Online Advertising Planning - The Role of Product - Brand Type in Previsit IntentionsДокумент9 страницApplying The Rossiter-Percy Grid To Online Advertising Planning - The Role of Product - Brand Type in Previsit Intentionsa861108Оценок пока нет
- Covid FeversДокумент7 страницCovid FeversdbvidyaОценок пока нет
- Dictogloss Strategy and Listening Comprehension Performance of Secondary School StudentsДокумент12 страницDictogloss Strategy and Listening Comprehension Performance of Secondary School StudentsSilvi AlizaОценок пока нет
- Favoritism Bad Habbit of Some TeacherДокумент2 страницыFavoritism Bad Habbit of Some TeacherQasim TapsiОценок пока нет
- Cawis vs. Cerilles - G.R. No. 170207 - April 19, 2010Документ2 страницыCawis vs. Cerilles - G.R. No. 170207 - April 19, 2010Lordy Jessah AggabaoОценок пока нет
- Clase 1-Fisiopatología de La Artritis ReumatoideaДокумент45 страницClase 1-Fisiopatología de La Artritis ReumatoideaPercy Williams Mendoza EscobarОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (35)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeОт EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeРейтинг: 4.5 из 5 звезд4.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (5)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionОт EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionОценок пока нет
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsОт EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsРейтинг: 4.5 из 5 звезд4.5/5 (39)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (44)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (46)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (254)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОт EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОценок пока нет
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!От EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Рейтинг: 5 из 5 звезд5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (267)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedРейтинг: 4 из 5 звезд4/5 (61)