Академический Документы
Профессиональный Документы
Культура Документы
No. 355-Physiologic Basis of Pain in Labour and Delivery: An Evidence-Based Approach To Its Management
Загружено:
dianОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
No. 355-Physiologic Basis of Pain in Labour and Delivery: An Evidence-Based Approach To Its Management
Загружено:
dianАвторское право:
Доступные форматы
SOGC CLINICAL PRACTICE GUIDELINE
No. 355, February 2018
No. 355-Physiologic Basis of Pain in Labour
and Delivery: An Evidence-Based Approach to
its Management
Abstract
This Clinical Practice Guideline has been prepared by the
authors listed below, reviewed by the SOGC’s Clinical Practice Objective: To review the evidence relating to nonpharmacological
– Obstetrics; Maternal-Fetal Medicine; Family Physician approaches in the management of pain during labour and delivery.
Advisory and Guideline Management and Oversight To formulate recommendations for the usage of
Committees and approved by the Board of the SOGC. nonpharmacological approaches to pain management.
Julie Bonapace, MEd, Gatineau, QC
Options: Nonpharmacological methods available for pain
Guy-Paul Gagné, MD, Montréal, QC management during labour and delivery exist. These should be
Nils Chaillet, PhD, Québec, QC included in the counselling and care of women.
Raymonde Gagnon, PhD, RM, Trois-Rivières, QC Evidence: PubMed and Medline were searched for articles in French
and English on subjects related to “breastfeeding,” “pain,”
Emmanuelle Hébert, RM, MSc, Montréal, QC
“epidural,” “anaesthesia,” “analgesia,” “labour,” “labor,” and
Sarah Buckley, MB ChB, Dip Obst, University of Queensland, combined with “gate control theory,” “alternative therapies,”
School of Public Health, Australia “massage,” “position,” “mobility,” “TENS,” “bathing,” “DNIC,”
“acupuncture,” “acupressure,” “sterile water injection,” “higher
center,” “control mind,” “cognitive structuring,” “holistic health,”
“complementary therapy(ies),” “breathing,” “relaxation,” “mental
imagery,” “visualization,” “mind focusing,” “hypnosis,” “auto-
hypnosis,” “sophrology,” “mind and body interventions,” “music,”
“odors,” “biofeedback,” “Lamaze,” “Bonapace,” “prenatal training,”
“gymnastic,” “chanting,” “haptonomy,” “environment,”
SPECIAL CONTRIBUTORS “transcutaneous electrical stimulus-stimulation,” “antenatal
Vyta Senikas, MD, Ottawa, ON education,” “support,” “continuous support,” “psychosocial
support,” “psychosomatic medicine,” “supportive care,”
Véronique Toussaint, RN, Québec City, QC
“companion,” “intrapartum care,” “nurse,” “midwife(ves),” “father,”
Disclosure statements have been received from all authors. “doula,” “caregiver,” “ hormones,” “oxytocin,” “endorphin,”
Key Words: Nonpharmacological pain management, labour, delivery “prolactin,” “catecholamine,” “adrenaline,” and “noradrenaline”
from 1990 to December 2015. Additional studies were identified
by screening reference lists from selected studies and from expert
suggestions. No language restrictions were applied.
J Obstet Gynaecol Can 2018;40(2):227–245
Validation methods: The quality of the evidence is rated
https://doi.org/10.1016/j.jogc.2017.08.003
using the criteria described in the Report of the Canadian Task
Copyright © 2018 The Society of Obstetricians and Gynaecologists of Force on Preventive Health Care. Recommendations for
Canada/La Société des obstétriciens et gynécologues du Canada. Pub- practice are ranked according to the method described in this
lished by Elsevier Inc. All rights reserved. report.
This document reflects emerging clinical and scientific advances on the date issued and is subject to change. The information should not be
construed as dictating an exclusive course of treatment or procedure to be followed. Local institutions can dictate amendments to these opin-
ions. They should be well-documented if modified at the local level. None of these contents may be reproduced in any form without prior written
permission of the publisher.
Women have the right and responsibility to make informed decisions about their care in partnership with their health care providers. To fa-
cilitate informed choice women should be provided with information and support that is evidence based, culturally appropriate and tailored to
their needs. The values, beliefs, and individual needs of each woman and her family should be sought and the final decision about the care
and treatment options chosen by the woman should be respected.
FEBRUARY JOGC FÉVRIER 2018 • 227
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
Benefits, risks, and cost: The nonpharmacological method 9. Elevated endorphins in labour help reduce maternal stress and pain
encourages an incremental approach to pain management that and may assist in newborn adaptations (II).
contributes to reduced interventions through optimal use of the 10. Health care providers and the birthing environment can have a major
woman’s neurophysiologic and endocrine resources and a impact on labour progress and experience by paying attention to
better understanding of the physiology of stress and pain during and reducing a woman’s stress level (I).
labour. 11. Prolactin not only promotes breast milk production, it optimizes the
mother’s physiologic and behavioural responses in adapting to her
Guideline update: The guideline will be reviewed 5 years after
role (II).
publication to decide whether all of part of the guideline should be
12. Creating a calm, stress-free environment, encouraging women, and
updated. However, if important new evidence is published prior to
having a positive attitude where possible play an important role to
the 5-year cycles, the review process may be accelerated for a
stimulate the endogenous hormone production that promotes and
more rapid update of some recommendations.
supports the physiologic progress of labour (II).
Sponsors: This guideline was developed with resources funded by 13. Neurophysiologic and hormonal mechanisms contribute to help
The Society of Obstetricians and Gynaecologists of Canada. women cope with the intensity of labour (l).
Summary Statements: Recommendations:
1. It is important that all health care professionals have a good un- 1. Health care providers should be familiar with the neurophysiologi-
derstanding of pain in childbirth including its physiological and cal and hormonal mechanisms and related methods in physiological
psychological management whether or not a person in labour also labour and birth (III-A).
chooses pharmacological relief (III). 2. To help women cope with normal labour, nonpharmacological ap-
2. A growing body of scientific literature supports the use of proaches are recommended as a safe first-line method for pain relief
nonpharmacological approaches to pain management during child- and should be continued throughout labour whether or not pharma-
birth due to their numerous benefits for the mother and child, cologic methods are used (I-A).
including a reduction in the need for obstetrical interventions, labour 3. To prevent suffering, health professionals should address the emo-
augmentation, or Caesarean section (l). tional component of pain (pain unpleasantness). This is most
3. Suffering, as opposed to pain, occurs when a woman is unable to effectively achieved through support and nonpharmacological ap-
activate her own mechanisms for coping with pain, or when her proaches to pain management.
own mechanisms are insufficient to deal with the situation (III). 4. To develop support measures consistent with the wishes of women,
4. The Gate Control Theory mechanism, which consists of creating health professionals should work with women and listen to their needs
pleasant stimulations in the painful area between or during con- (III-A).
tractions is best achieved through ambulation, gentle massage, 5. To further reduce the need for obstetric interventions and avoid as-
stroking, water, or vibrations (I). sociated risks and side-effects, health professionals should provide
5. The Diffuse Noxious Inhibitory Control (which consists of apply- continuous labour support with the addition of at least one other
ing painful stimulations at any site on the body for the duration of nonpharmacological pain modulating mechanism (I-A).
each painful contraction) is best achieved through acupressure, sterile 6. Health professionals should, where possible, promote and support the
water injections, or deep massage (I). physiological progress of labour, delivery, and the postpartum period
6. The Central Nervous System Control mechanism, which consists trusting the woman’s ability to work with her pain and encouraging her
of deviating or focussing the woman’s attention is best activated to rely on her ability to give birth (III-A).
through labour support and the practice of yoga, relaxation, visu- 7. To enhance the endogenous hormone production that promotes and
alization, breathing, auto-hypnosis and cognitive restructuring (I). supports the physiologic process of labour, health care providers
7. Continuous labour support, as part of nonpharmacological ap- should reduce a woman’s stress level by encouraging her and having
proaches to pain management during childbirth, reduces stress, fear, a positive attitude where possible and by creating a calm, stress-
and anxiety, which in turn decreases the frequency of obstetrical free environment (I-A).
interventions (I). 8. Continuous labour support, as part of nonpharmacological ap-
8. Natural oxytocin is not only important for uterine contractions; it en- proaches to pain management during childbirth for women should
hances a sense of calmness and reduces pain. Because synthetic be promoted and provided for all women in labour (I-A).
oxytocin does not cross the blood-brain barrier in a significant 9. Health professionals should encourage parents and the people as-
manner, the analgesic and psychological effects on the mother of sisting them to prepare for the birth by learning about birth physiology
calmness and well-being are lost (II). and gaining skills in working with pain (III-A).
228 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
INTRODUCTION (DNIC), and (3) CNSC activated through continuous labour
support and other psychological mechanisms. A sub-group
P hysiological birth is defined as an approach to labour and
birth that maximizes the inherent strength and normal
physiology of the woman and fetus and refrains from outside
analysis included in this meta-analysis showed a first-line ap-
proach that involved continuous support and at least one other
nonpharmacological method, and a pharmacological method
interventions unless the well-being or safety of the pair are jeop-
as needed or requested by the women produced optimal clini-
ardized. This clinical guideline follows the SOGC Joint Policy
cal outcomes. These approaches provide benefit by reducing
Statement on Normal Childbirth No. 221, published in De-
interventions. Usual care compared to these combined
cember 2008,1 and the SOGC Guideline on the Management
nonpharmacological approaches had increased odds of Cae-
of Spontaneous Labour at Term in Healthy Women,2 which sarean delivery (11 studies, 10 338 patients, OR 2.17),
promote, protect, and support normal birth. In response to con- instrumental delivery (6 studies, 2281 women, OR 1.78), epi-
cerns among many professional associations about the rise in dural analgesia (6 studies, 2207 women, OR 1.42), and the need
medical interventions during labour and delivery, the state- of synthetic oxytocin (6 studies, 2207 patients, OR 1.57). The
ment of principle recommends developing national clinical total duration of labour was reduced compared to usual care
directives in support of nonpharmacological approaches to pain (4 studies, 1254 women, average reduction 73.8 minutes).
management based on scientific data.
The purpose of this guideline is to recommend a frame of Nonpharmacological approaches can also benefit women
reference, for health professionals, that promotes physi- and babies by reducing exposure to the potential risks and
ologic birth while providing physical and emotional relief side-effects of pharmacological pain management.
to women to promote health and well-being for mother and
baby, mother-infant attachment, and breastfeeding. It is noteworthy that “The degree to which a woman is sat-
isfied with the birth experience is not solely associated with
Nonpharmacological methods of pain management, includ- the pain felt.”7 A systematic review found that the four most
ing support during labour, have the potential to reduce important factors for women’s birth satisfaction: personal
obstetrical interventions, increase breastfeeding rates, and expectations, the amount of support from caregivers, the
improve the mother’s satisfaction without increasing morbidity.3–6 quality of the caregiver-patient relationship, and involve-
To facilitate the endogenous physiological mechanisms acti- ment in decision-making, overrode all other influences,
vated during labour and delivery, health professionals, women including self-reported pain and analgesic efficacy.5 In ad-
giving birth, and their birth supporters should have a good un- dition, the presence of pain does not necessarily imply a
derstanding of the neurophysiologic and hormonal activity and negative birth experience—women can have pain coexist-
relevant techniques. A recent meta-analysis (57 randomized ing with satisfaction, enjoyment, and empowerment.8
studies of a total 34 000 women) assessed the effects of
nonpharmacologic approaches organized by mechanism of Summary Statements
action rather than by technique, on obstetrical interventions, 1. It is important that all health care professionals have
labour, maternal, and perinatal outcomes.3 This study ad- a good understanding of pain in childbirth including
dressed the lack of systematic reviews assessing the impact of its physiological and psychological management
nonpharmacologic approaches on obstetric interventions and whether or not a person in labour also chooses phar-
outcomes. In this meta-analysis, techniques were divided in three macological relief (III).
neurophysiologic pain modulating mechanisms: (1) light stimu- 2. A growing body of scientific literature supports the
lation of the painful area (Gate Control Theory), (2) second use of nonpharmacological approaches to pain man-
painful stimulation anywhere on the body during a contraction agement during childbirth due to their numerous
benefits for the mother and child, including a reduc-
tion in the need for obstetrical interventions, labour
ABBREVIATIONS augmentation, or Caesarean section (I).
CNS central nervous system
Recommendation
CNSC control of the higher centres of the CNS
DNIC diffuse noxious inhibitory control 1. Health care providers should be familiar with the neu-
OR odds ratio
rophysiological and hormonal mechanisms and related
methods in physiological labour and birth (III-A).
RCT randomized controlled trial
2. To help women cope with normal labour,
SOGC Society of Obstetricians and Gynaecologists of Canada
nonpharmacological approaches are recommended as
TENS transcutaneous electrical nerve stimulation
FEBRUARY JOGC FÉVRIER 2018 • 229
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
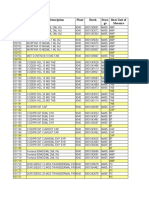
Table 1. Key to evidence statements and grading of recommendations, using the ranking of the Canadian Task Force
on Preventive Health Care
Quality of Evidence Assessmenta Classification of Recommendationsb
I: Evidence obtained from at least one properly randomized A. There is good evidence to recommend the clinical preventive
controlled trial action.
II-1: Evidence from well-designed controlled trials without B. There is fair evidence to recommend the clinical preventive action.
randomization C. The existing evidence is conflicting and does not allow to make a
II-2: Evidence from well-designed cohort (prospective or recommendation for or against use of the clinical preventive
retrospective) or case-control studies, preferably from more than action; however, other factors may influence decision-making.
one centre or research group D. There is fair evidence to recommend against the clinical
II-3: Evidence obtained from comparisons between times or places preventive action.
with or without the intervention. Dramatic results in uncontrolled E. There is good evidence to recommend against the clinical
experiments (such as the results of treatment with penicillin in preventive action.
the 1940s) could also be included in the category. L. There is insufficient evidence (in quantity or quality) to make a
III: Opinions of respected authorities, based on clinical experience, recommendation; however, other factors may influence
descriptive studies, or reports of expert committees decision-making.
a
The quality of evidence reported in these guidelines has been adapted from The Evaluation of Evidence criteria described in the Canadian Task Force on Preventive
Health Care.
b
Recommendations included in these guidelines have been adapted from the Classification of recommendations criteria described in The Canadian Task Force on
Preventive Health Care.
a safe first-line method for pain relief and should be associated with actual or potential tissue damage.”13 Under
continued throughout labour whether or not phar- normal circumstances, pain plays an essential role in pro-
macologic methods are used (I-A). tecting us from danger. Unlike other types of pain, however,
the strong sensations experienced by women in labour are
These clinical findings and a better understanding of the not usually a sign of danger, pathology, or dystocia. During
neurophysiologic and endocrine mechanisms involved in labour, pain performs an important function in the physi-
labour and delivery suggest a need to replace the para- ologic process by producing hormones like endorphins and
digm of “pain relief ” with that of “working with pain.” oxytocin that provide comfort.9,12,14–16 They signal the start
of labour and tell the woman that the time has come to find
In fact, the paradigm of pain relief is based on a set of assump- a safe place to give birth and to surround herself with
tions that labour pain is “abnormal” and unnecessary, that the supporters.10 When a woman can make sounds and move
benefits of analgesia will always exceed the risks, and that effi- freely, these sensations provide her with information about
cient pain relief is systematically correlated with women’s the progress of her labour.17 They help her find the body
satisfaction with the childbirth experience.9 In terms of satis- positions that soothe her, and they guide her expulsion
faction, studies suggest that factors including the amount of efforts.18
support from caregivers and involvement in decision-making are
more important to women than pain relief.5
The dimensions of pain
The “working with pain” paradigm is based on the assump- Pain, especially during childbirth, is a complex phenom-
tion that pain has a physiologic role in childbirth. When enon. According to Marchand et al.,19 pain has at least four
women are properly prepared and supported, they produce dimensions: nociceptive (noxious stimuli), sensory-
endogenous analgesic substances that support them to work discriminative (intensity), affective-motivational (the
with the pain of childbirth. Through working with pain in unpleasant, emotional aspect), and cognitive-behavioural
labour, women can experience a deep sense of satisfac- (behaviour).
tion that enhances their feelings of competency and
confidence in rising to the challenges of parenthood.10,11 With The circular pain model illustrates each of these dimen-
appropriate support, and through a complex hormonal physi- sions and their interrelations (Figure 1). It shows that pain
ology and regulating neurophysiological mechanisms, most can include any or all of these dimensions and be experi-
women have the resources they need to give birth.9,12 enced differently from one person to the next. This model
helps professionals adjust their actions to ensure that re-
I. UNDERSTANDING PAIN
sponses to pain are not based only on what they perceive
in the behaviour of labouring women (dimension 4), but
The International Association for the Study of Pain defines also on other dimensions affecting the woman’s experience
pain as “an unpleasant sensory and emotional experience of her pain. This also helps distinguish pain from suffering.
230 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
Figure 1. The circular pain model.19 Reprinted electronic fetal monitoring (EFM) and eating/drinking rather
with permission from Wolters Kluwer. than a continuous drip therapy) may diminish perceived pain.
2. Sensory-discriminative dimension (physical)
This dimension makes it possible to identify the intensity
and threshold of pain. Among other things, pain can be
modulated by pleasant sensations in the affected area (Gate
Control Theory), by providing another painful stimulus
(DNIC), and through pharmacological approaches (narcot-
ics and epidural).19
3. Affective-motivational dimension (psychological and
emotional)
This dimension is used to gauge the unpleasantness of pain.
It is affected by emotions, values, and experience. It is the
1. The nociceptive dimension element that expresses “suffering.” Interventions to modu-
late this component include approaches that call on the higher
This dimension involves real or potential injury. In the first centres of the brain such as support (feeling safe and pro-
phase of labour, nociception results from stretching of the tected), cognitive restructuring, emotional care, environmental
cervix, ligaments, muscles, structures, and adjacent tissue.17 ambience, and relationship with health care staff.19,24,25
It is typically referred pain that projects sensations to the
lower abdomen and back.20 4. Cognitive-behavioural dimension
During the second phase of labour, nociception can result This refers to the way a person expresses her experience of
from traction on the pelvis caused by the stretching of the pain. This dimension is heavily influenced by cultural, emo-
pelvic floor, perineum, perineal muscles, and pelvic cavity tional, motivational, social, and cognitive factors. Everyone
and strong pressure on the roots of the sacral nerves. externalizes pain differently. Others cannot make assump-
Nociception is transmitted by the pudendal nerve and is felt tions about pain: pain is a perception and there may be no
more keenly in the perineum and anus regions, the lower correlation between what the woman is experiencing and
part of the sacrum, the thighs, and the lower portion of the what others are perceiving.26–28
legs.17
The circular pain model shows that a woman in labour can
In addition, the fetal position (occiput posterior, trans- exhibit any one or all dimensions of pain. Intensity (di-
verse, or asynclitic positioning) plays a role in nociception mension 2) and unpleasantness (dimension 3) are supported
by placing greater pressure on the pelvis and the sacroiliac by two separate and therefore mutually independent neu-
joint and possibly by prolonging the length of labour.10 En- rophysiological pathways. A positive event, like birth, can
couraging women to move freely to ease their pain can help be perceived as more intense than unpleasant.29 The expe-
to modify this dimension. rience is individual; some women can experience an intense
labour (dimension 2) without suffering (dimension 3),
Although the scientific literature describing women’s ex-
whereas others may feel no intensity (dimension 2) after an
perience following the artificial rupture of membranes is
epidural, for example, and yet may still suffer (dimension
limited,21 research suggests that women report more pain
3). This would apply to a woman who may not have wanted
following this intervention.22 This heightened nociceptive
an epidural and sees it as a failure. Conversely, an epidural
signal may result from the absence of amniotic fluid, which
can create physical relaxation and lowered pain intensity (di-
acts like a shock absorber between the baby and the moth-
mension 2). This in turn can lead to emotional relaxation
er’s uterus. Leaving membranes intact may reduce pain
and a reduction in pain unpleasantness (dimension 3).
experienced in labour.
One study reported that women find it extremely stressful Distinguishing between pain and suffering
to be prevented from ambulating as they would like.23 Ac- The purpose of interventions for relieving pain in labour
cordingly, ambulation and avoiding interventions that restrict must be to prevent suffering with consideration for
mobility (intermittent auscultation rather than continuous potential effects on mother and baby and on the progress
FEBRUARY JOGC FÉVRIER 2018 • 231
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
of labour.12 Suffering is defined by a woman’s inability to and (3) CNSC. These mechanisms act on the nervous system
activate her own pain relief mechanisms or the inad- to modulate potentially painful (nociceptive) signals before
equacy of her mechanisms to confront the situation.30 This the brain decodes them as pain.
is the unpleasant dimension of pain (dimension 3). To
prevent suffering, professionals must address the various di- The three endogenous mechanisms
mensions of pain. Special attention must focus on the
motivational affective dimension (dimension 3) because emo- 1. Gate Control Theory
tional stress creates catecholamine, which may slow labour31
and potentially increase the use of obstetrical interventions. The Gate Control Theory,32 or specific inhibitory control
via non-nociceptive stimuli mechanism, is at work during
Making sounds, ambulating, and deep breathing are not nec- non-painful, gentle massaging of the painful area. It acti-
essarily signs of maternal suffering. It is often a mother’s vates large afferent fibres that block the smaller fibres
way of working with pain, and it is largely conditioned by transmitting the pain message. Through this action, the per-
culture (dimension 4). Unless the woman is specifically re- ceived intensity of the pain (dimension 2) is modulated. This
questing otherwise, when labour is advancing normally, offer mechanism includes techniques like conventional non-
nonpharmacological approaches as a first approach. Slowing painful TENS, gentle massage, vibration, baths, warm towels,
of labour may indicate that the labouring woman is expe- and body positioning with movement.
riencing excessive stress and possibly suffering. In this
circumstance, addressing the affective dimension of pain A recent meta-analysis3 on labour pain relief showed that
(emotions) may be effective, noting that it is always impor- when compared with nonpharmacological approaches based
tant to check the labouring woman’s needs and experience on this Gate Control mechanism, usual care increases the
before making this assumption. Pharmacological ap- odds of epidural analgesia (OR = 1.22, 95% CI 1.04–1.43,
proaches, in addition to continuing nonpharmacological RCTs, 3369 women). This analysis also found that women
approaches, should be available and provided if she is suf- who used Gate Control Theory techniques based on
fering and/or requesting them. ambulation experienced a reduction in Caesarean deliver-
ies and use of synthetic oxytocin during labour, and had
Summary Statement lowered maternal anxiety when compared to standard care.
3. Suffering, as opposed to pain, occurs when a woman No significant difference was observed in other obstetri-
is unable to activate her own mechanisms for coping cal interventions or neonatal and maternal morbidity (I-A).
with pain, or when her own mechanisms are insuffi-
cient to deal with the situation (III). Summary Statement
4. The Gate Control Theory mechanism, which con-
Recommendations sists of creating pleasant stimulations in the painful
3. To prevent suffering, health professionals should area between or during contractions is best achieved
address the emotional component of pain (pain un- through ambulation, gentle massage, stroking, water
pleasantness). This is most effectively achieved through or vibrations (I).
support and nonpharmacological approaches to pain
management (I-A). 2. DNIC
4. To develop support measures consistent with the wishes This mechanism is activated by painful stimulation, some-
of women, health professionals should work with times at a site far removed from the painful area.33,34 As
women and listen to their needs (III-A). endorphins are released, the body inhibits pain at all painful
The neurophysiology of pain during labour and areas except the one subjected to the painful stimuli. This
delivery mechanism is activated with all peripheral stimulation tech-
Mechanisms that modulate the pain dimensions discussed niques such as acupuncture, TENS (high-intensity), deep
above can be used to alter the perception of pain by re- tissue massage (acupressure), ice massage, and sterile water
ducing nociceptive stimuli. These mechanisms affect both injections.
the sensory-discriminative and motivational-affective di-
A recent meta-analysis3 on labour pain relief showed that
mensions (dimensions 2 and 3), enabling women to better
when compared with nonpharmacological approaches based
cope with their sensations during labour.
on the DNIC mechanism, standard care is associated with
Neurophysiologic modulating mechanisms are divided into an increase of epidural analgesia (OR = 1.62, 95% CI 1.18–
three categories19,24: (1) The Gate Control Theory, (2) DNIC, 2.21, 6 RCTs, 920 women). The findings also showed an
232 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
increase in the dystocia rate in the second stage of labour, 95% CI 1.06–2.98, 6 RCTs, 2281 women), epidural anal-
increased pain felt by women, and lower maternal satisfac- gesia (OR = 1.42, 95% CI 1.15–1.76, 5 RCTs, 2207 women),
tion with childbirth. No significant difference was detected and the average length of labour by 73.8 minutes (95% CI
in other obstetrical interventions or perinatal and mater- 42.6–105.0), 4 RCTs, 1254 women) (I-A).
nal morbidity (I-A).
These results suggest that labour support (CNSC) associ-
Summary Statement ated with one or more techniques that enlist other
endogenous mechanisms (a combined approach) is the most
5. The Diffuse Noxious Inhibitory Control (which con-
effective method for helping women work with pain.
sists of applying painful stimulations at any site on the
body for the duration of each painful contraction) is
Summary Statement
best achieved through acupressure, sterile water in-
jections, or deep massage (I). 7. Continuous labour support, as part of non-
pharmacological approaches to pain management
3. CNSC during childbirth, reduces stress, fear, and anxiety, which
in turn decreases the frequency of obstetrical inter-
Deviation of attention plays a major role in managing pain ventions (I).
by modifying the message and triggering the pain inhibi-
tion centre (endorphin secretion). In the higher centres of Recommendation
the brain, pain messages create direct and indirect links with 5. To further reduce the need for obstetric interven-
other regions of the brain. These regions are closely asso- tions and avoid associated risks and side-effects, health
ciated with memory and emotion. All behavioural or cognitive professionals should provide continuous labour
approaches used to modulate the perception of pain, such support with the addition of at least one other
as relaxation, hypnosis, attention deviation, yoga, breath- nonpharmacological pain modulating mechanism (I-A).
ing, meditation, aromatherapy, music, support, or placebos
are included in this mechanism. Summary of the hormonal physiology of labour and
3 birth
A recent meta-analysis on labour pain relief showed that
when compared with nonpharmacological approaches based During labour and birth, a series of hormones are re-
on the higher centres of the CNS, standard care is associ- leased for mother and baby that regulate labour, reduce pain,
ated with a significant augmentation of epidural analgesia and prepare the mother to welcome her child, among other
(OR 1.13, 95% CI 1.05–1.23, 11 RCTs, 11 957 women), Cae- effects. These hormones also promote mother and child
sarean deliveries (OR 1.60, 95% CI 1.18–2.18, 27 RCTs, 23 safety and well-being and support the initiation of maternal-
860 women), instrumental delivery (OR 1.21, 95% CI 1.03– infant attachment and breastfeeding.12
1.44, 21 RCTs, 15 591 women), use of synthetic oxytocin In the period preceding the physiologic onset of labour, hor-
(OR 1.20, 95% CI 1.01–1.43, 19 RCTs, 14 293 women), du- monal systems reorganize to optimize hormonal responses
ration of labour (29.7 min, 95% CI 4.5–54.8, 13 RCTs, 4276 in labour and birth. This reorganization includes increases
women), and lesser maternal satisfaction with childbirth (I-A). in the number of receptors, which heightens tissue sensitivity
to and efficacy of hormones released in labour. For example,
Summary Statement
pre-labour increases in uterine oxytocin receptors maximize
6. The Central Nervous System Control mechanism, the uterotonic effects of oxytocin released during labour.
which consists of deviating or focussing the woman’s
attention, is best activated through labour support and Oxytocin
the practice of yoga, relaxation, visualization, breath- Oxytocin is well known for its role in producing uterine con-
ing, auto-hypnosis, and cognitive restructuring (I). tractions during labour. Oxytocin also creates feelings of love
and connection and is released during social and sexual
Combined approaches contact, female and male orgasm, and childbirth and
The meta-analysis by Chaillet et al.3 also showed that a com- breastfeeding, among other situations.35–37
bined approach to pain relief based on continuous
intrapartum support along with at least one other endog- Oxytocin is produced in the limbic system and released both
enous method (Gate Control Theory or DNIC) significantly locally in the brain and into the bloodstream. Its effects are
lowered Caesarean rates (OR = 2.17, 95% CI 1.30–3.61, 11 both psychological and physical. In addition to fostering love,
RCTs, 10 338 women), instrumental deliveries (OR = 1.78, attachment, and calmness,35–37 it also alleviates pain.38
FEBRUARY JOGC FÉVRIER 2018 • 233
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
Figure 2. Oxytocin levels in late pregnancy, in early labour, at birth, and after birth.12
Copyright © 2015. National Partnership for Women & Families. Used with permission.
Oxytocin is also responsible for the ejection reflexes that In addition to augmenting pain by triggering stronger, more
expel the fetus (Ferguson reflex) and the placenta after birth frequent and longer contractions than physiologic
and the milk-ejection (“let-down”) reflex.35 contractions,50 recent studies suggest that synthetic oxyto-
cin exposure in labour may interfere with the release of
Maternal oxytocin levels increase in labour and peak at natural oxytocin during early breastfeeding.51 Although poorly
birth.39,40 Even higher levels postpartum, stimulated by studied, some research suggests lowered success with
maternal-newborn contact, ensure effective uterine con- breastfeeding.49,52-54
tractions and prevent postpartum haemorrhage (Figure 2).12,41
Skin-to-skin contact, eye contact, touch, and nipple stimu- Epidural administration reduces endogenous oxytocin
lation by the baby help release this hormone.35,40 release55–58 and can slow the progress of labour and also in-
crease the risk of instrumental delivery3,59 by inhibiting the
Stress and disturbance can disrupt labour progress via several Ferguson reflex.4,60 Evidence on the clinical impact of epi-
possible hormonal mechanisms. When a labouring woman dural is inconsistent and conflicting,61 but some studies have
perceives her environment as stressful (e.g., transport in labour, shown epidural effects on the success of newborn
bright lights, noise, etc.), supra-physiological levels of cat- breastfeeding54,62–65 and the duration of breastfeeding.4,66,67
echolamines (adrenaline and noradrenaline) and/or
endorphins,42 which are also increased in response to excessive Summary Statements
stress, may inhibit labour by direct and indirect mechanisms.12 8. Natural oxytocin is not only important for uterine con-
tractions; it enhances a sense of calmness and reduces
Although endogenous oxytocin reduces stress and pain by
pain. Because synthetic oxytocin does not cross the
release within the brain, synthetic oxytocin administered in-
blood-brain barrier in a significant manner; the anal-
travenously does not cross the blood-brain barrier in
gesic and psychological effects on the mother of
significant amounts43,44 and so does not produce these central
calmness and wellbeing are lost (II).
effects.12 In addition, prolonged exposure to synthetic oxy-
tocin during labour reduces the sensitivity of uterine oxytocin Recommendations
receptors,45 which can heighten the risk of postpartum
bleeding.46–48 Long-term effects of perinatal exposure to syn- 6. Health professionals should, where possible, promote
thetic oxytocin for mother and offspring are biologically and support the physiological progress of labour, de-
plausible, but poorly studied. One Canadian study showed livery, and the postpartum period trusting the woman’s
a positive correlation between the synthetic oxytocin dose ability to work with her pain and encouraging her to
administered during labour and symptoms of maternal de- rely on her ability to give birth (see Appendix 1) (III-A).
pression, anxiety, or somatization two months after 7. To enhance the endogenous hormone production that
childbirth.49 promotes and supports the physiologic process of
234 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
Figure 3. Women’s endorphin levels: non-pregnant, in labour, and after birth. Copy-
right © 2015. National Partnership for Women & Families. Used with permission.
labour, health care providers should reduce a woman’s Summary Statement
stress level by encouraging her and having a positive at- 9. Elevated endorphins in labour help reduce maternal
titude where possible and by creating a calm, stress-free stress and pain and may assist in newborn adapta-
environment (see Appendix 2) (I-A). tions (II).
Endorphins Adrenalin and noradrenalin
Endorphins are analgesic substances produced in the brain Adrenalin (epinephrine) and noradrenalin (norepineph-
during sexual activity, pregnancy, birth, and breastfeeding.12 rine) belong to the catecholamine group of “fight-or-
Endorphin levels, as measured in the blood, are elevated flight” stress hormones that reach their maximum
during pregnancy,68 increase during labour and birth, and physiological levels at the end of labour, and diminish quickly
decline within 20 minutes after birth (Figure 3).69 after birth (Figure 4).73,74
Through central release, endorphins ease pain and alter the At the end of labour, physiologic catecholamine eleva-
mother’s state of consciousness.12 After the delivery, they tions heighten the mother’s attention and energy level,
can trigger a sense of pleasure and euphoria,12 and may play equipping her with the resources to give birth to her
an important role in mother-child attachment, as they do baby.10,12,75 For the fetus, a late-labour catecholamine surge
in other mammals.70 protects from low oxygen levels and prepares for life outside
the uterus by optimizing respiratory function, metabolic func-
Endorphins foster the release of prolactin,71 which pre- tion, and heat production.76,77 After delivery, maternal
pares the breasts for breastfeeding and is also present in catecholamine levels drop significantly.74 Supra-physiological
breast milk.72 Endorphins activate central reward and plea- levels during labour can inhibit contractions, both directly
sure circuits that create a sense of wellbeing in mother and and possibly via effects on oxytocin.12 Excessive catechol-
child. Their release during maternal-infant interactions, in- amine levels after birth may inhibit, uterine contractility,78
cluding breastfeeding, may be important in motivating and and increase the risks of postpartum hemorrhage.12
rewarding infant contact and breastfeeding.12,70
A negative emotional or physiological state in labouring
Physiologic birth produces high levels of endorphins in early women, including subjective stress, fear, anxiety, hunger, thirst,
breastmilk which may assist with newborn adaptations. The or the feeling of being watched or disturbed could slow
amount of endorphins in colostrum at postpartum day 4 labour by increasing catecholamines and/or via other hor-
was found to be significantly higher among women follow- monal stress responses.12 This response, clearly seen in animal
ing physiologic birth than after a pre-labour Caesarean studies, is likely an evolutionary adaptation to ensure that
delivery.72 labour and birth occur in the safest possible environment.12
FEBRUARY JOGC FÉVRIER 2018 • 235
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
Figure 4. Adrenalin and noradrenaline levels in labour, at birth, and after birth. Copy-
right © 2015. National Partnership for Women & Families. Used with permission.
Health care providers and the birthing environment may have Summary Statement
a significant effect on labour progress and experience by
modifying a woman’s stress level. Several meta-analyses show 11. Prolactin not only promotes breast milk produc-
a diminished need for analgesics when women are continu- tion, it optimizes the mother’s physiologic and
ously supported whether in the hospital setting,79 with behavioural responses in adapting to her role (II).
midwives,80 in birthing centres,81 or at home.82,83 Oxytocin, endorphins, catecholamines, prolactin, and other
hormones help to regulate the progress of labour and
Summary Statement promote essential adaptations after birth for mother and baby.
10. Health care providers and the birthing environ- This hormonal physiology also fosters maternal-newborn
ment can have a major impact on labour progress and attachment and breastfeeding. Hormonal effects are opti-
experience by paying attention to and reducing a mized when the mother feels safe and protected and when
woman’s stress level (I). her need for privacy is met.
Prolactin Obstetrical interventions, though sometimes necessary, can
Prolactin fosters the production of breast milk and ensures disturb hormonal physiology, producing a gap between ex-
successful breastfeeding. As the “mothering” hormone, it pected and actual hormonal experiences for mother and
optimizes the mother’s physiologic and behavioural re- infant. Practices that optimize hormonal physiology such
sponses to adapt to her maternal role.84 as skin-to-skin maternal-newborn contact and support for
breastfeeding can help to restore hormonal physiology, with
To a degree, prolactin may increase anxiety and vigilance, keeping ongoing benefits to breastfeeding and attachment.12 See
breastfeeding mothers alert to their infant’s needs.35 Prolactin may Appendix 1 on obstetrical practices that support the en-
contribute to the beneficial effects of breastfeeding on the ma- dogenous abilities of women.
ternal sleep.85,86 Prolactin is also the “fathering” hormone, and
appears in higher levels in fathers involved with their infant.87 Pro- The birth supporter’s role
lactin reduces stress88 and sexual desire.89
The continuous support and empathy of the father or other
Prolactin levels increase gradually during pregnancy, but the partner, a birth supporter, doula, and/ or a health care pro-
production of breast milk is inhibited hormonally until de- fessional is an important priority in maternity care.3,79
livery of the placenta.90 At the start of labour, prolactin levels Labouring women may need emotional support (a continu-
diminish only to rise again at the end of labour, reaching a ous, reassuring, encouraging presence), physical support
peak at birth and remaining high for several hours thereafter (massage, help to change position, adequate fluid and solid
(Figure 5).91 This prolonged elevation, which may be disrupted intake), information support (about the progress of labour,
by epidural analgesia, may support long-term breastfeeding interventions, tools for working with pain), and/or advo-
success by promoting prolactin receptor formation.92 cacy (to help the woman voice her wishes). 10,79 See
236 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
Figure 5. Maternal prolactin levels in labour, at birth, and after birth. Copyright © 2015.
National Partnership for Women & Families. Used with permission.
Appendix 2 for practical actions that support and help the baby’s safety, bath temperatures should be no higher than
women in labour. 38°C.94,95 Although the findings of a few studies did not find
any increased risk with water births,93 there are currently in-
Summary Statements sufficient data to offer a recommendation concerning the
12. Creating a calm, stress-free environment, encourag- birth stage. Women can be encouraged to shower and take
ing women, and having a positive attitude where baths during labour and delivery.
possible play an important role to stimulate the en-
dogenous hormone production that promotes and 2. Warm/cold packs
supports the physiologic progress of labour (II). Non-painful applications of warm or cold packs at the pain
13. Neurophysiologic and hormonal mechanisms con- site blocks part of the message in the spine, as described
tribute to help women cope with the intensity of in the Gate Control Theory. Cold in particular reduces pain
labour (l). in various clinical trials and can alleviate muscle spasms and
reduce tissue swelling and bruising when it occurs.8
Recommendation
8. Continuous labour support, as part of During or between contractions, warm or cold packs can
nonpharmacological approaches to pain manage- be applied to the back, neck, chest, face, or any other painful
ment during childbirth for women should be promoted area as best suits the woman’s comfort.
and provided for all women in labour (I-A).
3. Gentle massage
II. NONPHARMACOLOGICAL PAIN RELIEF Gentle massage is an easy, nonpharmacological method for
METHODS increasing the release of analgesic hormones96 while block-
ing some of the nociceptive signals in the spine. It can
Gate Control Theory Techniques: Non-Painful alleviate pain97–100 and the frequency of epidurals and their
Stimulation of the Painful Site associated consequences (when performed by a profes-
sional massage therapist).99 It loosens and relaxes the woman’s
1. Water immersion
body, calms her anxiety by creating a sense of safety, and
Water immersion or showering during labour promotes the improves maternal satisfaction and mood.8,100,101
release of oxytocin and endorphin hormones and reduces During or between contractions, stroking or gentle massage
the nociceptive message via pleasant stimuli applied to painful can be performed in areas determined by the woman’s pref-
areas. It reduces pain, accelerates labour, promotes physi- erence (abdomen, shoulders, back, legs, and sacrum).
ologic birth, and gives women a greater sense of satisfaction.93
A Cochrane systematic review did not find an increased in- Partners can be shown gentle massage techniques during
fection risk, whether the membranes are intact or not.93 For the prenatal period or at the start of labour.8
FEBRUARY JOGC FÉVRIER 2018 • 237
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
4. Mobility and positions Figure 6. Acupuncture Reflex points.24 Used with permis-
sion from Les Éditions de l’Homme.
Moving around during labour and vertical positioning ease
pain, produce better fetal-maternal circulation, improve fetal
oxygenation, and produce more effective uterine contrac-
tions. They also reduce the length of labour, facilitate fetal
H-7
descent, and diminish perineal trauma.102 Women request BL-31 L.I.-4
epidural analgesia less often when they use a vertical
position.103
BL-32
BL-33 G.B.-30 S.P.-6
During delivery, women perceive less severe pain when they BL-34 LIV-3
are in a vertical or lateral position.104 Interventions that sig-
nificantly limit mobility may therefore increase pain, including
labour induction, continuous electronic fetal monitoring, and
intravenous drip.102,105 Stimulation using painful deep tissue massage at certain acu-
puncture points can be applied throughout painful
Standing, sitting, squatting, or any other comfortable po- contractions.
sition chosen by the mother can be effective and have no
negative impact on mothers or infants. Women can be en- 2. Sterile water injections
couraged to follow and work with their sensations.
Painful intradermal injections of sterile water in the lower
Women can be offered accessories such as birth balls, birth back (near lumbosacral area) can diminish the pain of women
stools, trapeze bars, or bars to hang from.106 in labour by activating endorphin-producing DNIC. It is ef-
fective for all types of pain, especially lumbar pain,113 and
its effects last from 45 to 120 minutes.113–115 One meta-
DNIC Techniques: Painful Stimulation during a analysis showed that this method reduces Caesarean rates,116
Contraction whereas two Cochrane systematic reviews117,118 reported in-
sufficient data to establish the method’s effectiveness.
1. Acupuncture, electro-acupuncture, acupressure
During a contraction, intradermal sterile water injections may
be administered in the lower back or another area to create
Acupuncture involves inserting fine needles at specific points
a sharp pain. Although the location of the second pain is
on the body. It can be used to facilitate labour (cervical di-
relatively unimportant for the purposes of the DNIC mecha-
lation, descent of baby, perineal relaxation, soothing of
nism, studies suggest the water injections should be
mother, etc.) and/or to ease pain. Electro-acupuncture in-
administered in the lower back, especially for women ex-
volves administering a mild electrical current between the
periencing strong back pain (Figure 7). Repeat the injection
needles, and acupressure involves the acupuncture points
as needed.
being stimulated by painful deep tissue massage rather than
needle insertion. Painful stimulation of acupuncture points
Figure 7. Location of intradermal injections.24 Used with per-
during the painful contraction activates the DNIC mecha- mission from Les Éditions de l’Homme.
nism. Most commonly used acupuncture reflex zones are
Bladder 31–34 (BL-31-34), Large Intestine 4 (L.I.-4- Dimples
Hegu), Gall Bladder 30 (G.B.-30-Huantiao), Liver 3 (LIV-
3-Taichong), Spleen Pancreas 6 (S.P.6-Sanyinjiao), and Heart
7 (H-7-Shenmen) (Figure 6).
RCTs show that women who use acupuncture are less likely
to use other types of analgesic, experience less pain, have BL-32 BL-32
fewer instrumental deliveries, are more relaxed, and have a
greater sense of control.107–109 Other studies have found that
electro-acupuncture during labour diminishes the intensity
of pain110,111 and increases beta-endorphin levels.111 Acu-
pressure also reduces the intensity of pain during labour.107,112
238 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
3. Ice 2. Relaxation and visualization
Creating a second pain anywhere else on the body with the Relaxation and visualization are helpful techniques for physi-
application of ice cubes causes the release of endorphins cally and mentally preparing for labour and birth. Relaxation
(DNIC). Pressure point massage using ice cubes has been may include an awareness of body tensions with deliber-
examined in several studies119,120 and was found effective in ate relaxation of the affected areas. Visualization helps the
alleviating pain during labour. woman deal with stress through positive thoughts, either by
imagining herself in pleasant surroundings or using labour-
For the duration of the painful contraction, second pain can associated metaphors (the cervix as a blossoming flower,
be created by applying ice anywhere on the woman’s body waves for contractions, etc.).
or at acupressure points.
When the woman relaxes and uses positive imagery, she pro-
4. Painful TENS duces endorphins that lower the intensity and, most
importantly, the unpleasantness of her pain.19 This effect
Using a low-frequency electrical current transmitted via elec- is achieved through the attention deviation mechanism or
trodes placed on the skin, TENS produces transcutaneous CNSC of the brain.
electrical neurostimulation that creates a second source of
pain to diminish the pain of a contraction (DNIC). The This technique improves mental and physical well-being,130
woman controls the low-frequency/high-intensity (painful) and reduces anxiety during pregnancy127 and labour.131 It also
stimulation emitted by a portable device. reduces pain intensity, lowers the rate of assisted vaginal de-
livery, and improves maternal satisfaction.128
TENS helps reduce the use of analgesics8,121 and its appli-
cation at specific acupuncture points has proven to be a non- During labour, women can be encouraged to relax through
invasive means of easing pain in the first stage of labour.122 loosened muscle tension in targeted areas (buttocks, mouth,
However, a Cochrane meta-analysis123 showed that women shoulders, hands, etc.) while engaging in positive visualization.
generally reported little difference in the intensity of per-
ceived pain with TENS, except those using it on acupressure 3. Breathing
points. Nevertheless, several women said they would be in-
terested in using this method again in a future labour. Breathing techniques are used to alleviate pain and create
a sense of calmness and confidence. Breathing is one of the
During the contraction, the woman can increase the inten- most effective tools available to women in labour.132 It is often
sity of the electrical stimulation to create a second pain, which encouraged to increase relaxation and to distract attention
releases endorphins. away from the pain.8,132
CNSC Techniques Focused breathing can also increase a woman’s confi-
dence and ability to cope with contractions.8 When a woman
1. Yoga is conscious of her breathing rhythm, how she inhales and
exhales, she is able to adjust her breathing to the intensity
Yoga combines flexibility and strength exercises with breath- of her labour.133 Furthermore, slow, rhythmic breathing com-
ing, relaxation and meditation.124 It prepares women for bined with massage has a “hypnotic” effect.134 A recent, quasi-
childbirth and fosters the release of endorphins125 by CNSC. experimental study showed that breathing techniques are an
It helps increase a sense of competency and enables faster re- effective means of significantly reducing pain in primipa-
covery from stress.126 Two meta-analyses show that yoga during rous women during the first stage of labour.135
pregnancy and labour has a positive impact on controlling
anxiety127 and reducing the intensity of pain.128 Women also During each contraction, the labouring woman can be en-
report greater satisfaction with their labour and greater pain couraged to be aware of her breathing and to fully exhale.
relief. The length of labour diminishes along with the use of She can also be encouraged to make sounds, depending on
pharmacological analgesia.128 These findings are promising, al- her own needs.
though more detailed studies would be helpful.129
4. Hypnosis, self-hypnosis, and hypnobirthing
Where available and accessible, women may be encour-
aged to prepare for childbirth by practising yoga poses, and Hypnosis, self-hypnosis, and hypnobirthing are techniques
becoming familiar with using breathing, relaxation, and medi- used for overcoming the fear of labour. Based on deep re-
tation throughout their pregnancy. laxation, breathing, and visualization techniques, women are
FEBRUARY JOGC FÉVRIER 2018 • 239
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
taught to trust their bodies, regain the belief in their ability method free of side effects that can be used along with other
to give birth, and free themselves from tension and pain. methods during labour to help women work with pain. While
Using these tools, the labouring woman can reach a state some suggest calm music, others support women to choose
of deep relaxation without losing touch with reality. In this the music they prefer.145
state, the woman produces endorphins that reduce the un-
pleasantness and intensity of the pain along with the need During pregnancy, women can be encouraged to prepare
for analgesics, while shortening the stages of labour.136–139 their own playlist of music they enjoy. Using earphones
during labour can help a woman stay in her calm zone of
Hypnosis is an effective means of reducing stress during wellbeing.
the prenatal period and also during childbirth.137 In one study,
higher vaginal delivery rates were achieved among nullipa- 7. Prenatal education
rous women who used hypnotherapy.138 In another study
Birth preparation courses are intended to help parents
women who engaged in self-hypnosis during labour were
develop tools for a better childbirth experience and may also
less likely to use pharmacological analgesic methods, in-
promote parenting skills. The content covered aims to
cluding epidural analgesia, and were more satisfied with their
provide mental, physical, and emotional preparation.
pain management.140 However, further research is needed
to confirm these studies.140,141 Studies looking at possible benefits from childbirth prepa-
ration show conflicting and inconsistent results, which may
As with other techniques involved in CNSC, these work best
reflect the wide variety of programs and lack of high-
when health care professionals avoid disturbing the woman
quality studies.146
in labour. It is ideal to create a space of trust and privacy
with dimmed lighting, silence, calmness, and serenity to Prenatal education courses that have shown the most sig-
protect the woman’s well-being and hormonal physiology.12 nificant benefits feature physiology-based education and offer
a variety of tools for working with pain, while giving par-
5. Aromatherapy and odour ticipants opportunities to practice during classes.147–149
Aromatherapy refers to the use of aromatic plant extracts During pregnancy, encourage women (and their partner or
(essences or essential oils) for medicinal purposes. The ex- labour support person) to take birth preparation classes,
tracts can be applied to the skin, infused on a cloth, or where available and appropriate, that promote physiology
diffused in a bath or in the room, although the latter method and strengthen their skills in working with pain.
is not recommended at birth, as it may overstimulate the
newborn’s sensitive olfactory system and interfere with scent Recommendation
free hospital policies. Odour modulates pain by deviating
9. Health professionals should encourage parents and the
the woman’s attention.
people assisting them to prepare for the birth by learn-
Although systematic reviews have not proven aromathera- ing about birth physiology and gaining skills in working
py’s effectiveness,118,128 this method does not have known with pain (III-A).
side-effects. Women can be encouraged to smell a pleas-
ant odour, such as aromatic plant extracts, or a reassuring CONCLUSION
odour, such as that of her partner or a familiar object (e.g.,
their own pillow), if they desire. Pain management and the prevention of suffering during
labour are complex processes that may not be effectively
6. Music addressed by administering the best available analgesic. As
far as safely possible, health care professionals are encour-
Music during labour, perceived in the right hemisphere of aged to focus on the needs of the labouring woman and
the brain, can stimulate the pituitary gland to release to limit interventions that increase her stress and anxiety or
endorphins.142 It can also alter the perception of pain through disturb her natural hormonal physiology.8 Health care pro-
affect (ameliorating mood, increasing relaxation and low- fessionals can promote and support an environment that
ering anxiety) and cognitive effects (increasing control and values and recognizes the ability of the labouring women,
distraction).143,144 their partners, and their newborns.
Studies show considerable heterogeneity and currently An undisturbed environment that supports hormonal physi-
provide insufficient evidence to support the effectiveness ology for the labouring woman will foster the processes of
of this technique.128 However, music remains a simple labour and birth, help women to work with their pain, and
240 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
provide an ideal postpartum situation for the initiation of 9. At full dilation, wait until the baby passively descends
breastfeeding and mother-child attachment. to the vulva to allow the Ferguson reflex to activate. The
baby’s descent activates oxytocin receptors and the pelvic
A good understanding of neurophysiological mechanisms nerve which release high doses of oxytocin that create
will assist health professionals to work with labouring women contractions causing the baby to descend into the vagina.
to modulate pain stimuli. When labouring women have con- 10. At the time of birth, support undisturbed early contact
tinuous support and ready access to a variety of between mother and newborn and delay cord
nonpharmacological approaches, obstetrical interventions clamping.150 Immediate and uninterrupted skin-to-
and intervention-related risks and side effects can be reduced skin contact, tactile stimulation, and suckling stimulates
and maternal satisfaction improved.3 release of maternal oxytocin which contributes to uterine
contractility inhibiting haemorrhaging.151 It also im-
APPENDIX 1 proves newborn stability and favours the success of
breastfeeding.
Obstetrical practices that support endogenous abilities 11. During the postpartum period, offer unrestricted
maternal-newborn contact and especially support liberal
1. Allow labour to start physiologically to optimize hor- skin-to-skin contact and breastfeeding to encourage
monal activity that soothes and protects the mother- optimal hormonal release.
child pair.
2. Increase the effectiveness of labour by encouraging
actions that support natural oxytocin release. Protect APPENDIX 2
the privacy of the woman and her partner and make
them feel safe. Alleviate stress, which can interfere with Practical ways to support and assist women in labour
labour progress.
3. Maintain intact membranes, except when medically con- 1. When the mother arrives, review and discuss her ob-
traindicated, to avoid increasing nociceptive signals. jectives and wishes for the birth to identify her
4. Encourage women to hydrate and eat as they require: preferences.
stress related to hunger and thirst increases catechol- 2. Find out what kind of support she wants from staff.
amine, which blocks natural oxytocin. 3. Find out what methods she would like to use to help
5. Allow the women to experience the pre-labour, labour, her work with her labour pain.
expulsion, and postpartum phases in the same loca- 4. Prioritize emotional support, and positively support the
tion; changing surroundings can create stress, which can woman and her partner throughout labour and delivery.
interfere with labour progress. 5. Suggest and apply various nonpharmacological tech-
6. Allow women to move about and position themselves niques with her, even if she has had no preparation or
as they prefer throughout labour and delivery. Avoid ob- methods for dealing with pain (ball, positions, massage,
stetrical interventions that limit women’s mobility. In breathing, presence, etc.).
the absence of medical contra-indications, intermit- 6. Instruct and support the partner with nonphar-
tent auscultation should be favoured to continuous macological methods for easing the woman’s pain.
electronic monitoring. Solid food and liquids are pref- 7. Ask open-ended questions to understand the woman’s
erable to intravenous perfusion. In case of an anticipated experience rather than closed-ended questions (“How
need for a rapid intravenous access, the use of a saline do you feel?” rather than “Are you suffering?”).
lock or stopper is to be considered. Ambulation can 8. Trust in the physiological process of birth, in the woman,
reduce the perception of pain by blocking some of the and in her baby.
nociceptive fibres in the spine (Gate Control Theory). 9. Encourage women to stay inside their “bubble,” avoid-
7. Encourage continuous, one-on-one support with the ing any sensory or mental stimulation from questions,
woman to create the sense of trust and safety that sup- clocks, continuous electronic fetal monitoring, noise, etc.
ports hormonal physiology and helps the woman work This will help the woman let go and flow with her in-
with pain and thus assists the physiological progress of voluntary sensations.25
labour. 10. Create a stress-free environment to make the
8. Various nonpharmacological methods to comfort the woman feel safe, protected and supported. A calm en-
women should be considered as primary methods of vironment with dimmed lights reduces the amount of
pain management. Before offering pharmacological intervention during labour, increases spontaneous vaginal
methods, wait until the woman asks. deliveries and creates greater satisfaction in the women.
FEBRUARY JOGC FÉVRIER 2018 • 241
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
11. Encourage women to participate in decisions by ex- 20. McDonald JS. Pain of childbirth. In: Loeser J.D., editor. Bonica’s man-
agement of pain. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;
plaining the risks and benefits of suggested interventions 2001. p. 1388–414.
as well as alternatives.
21. Wei S, Wo BL, Qi HP, et al. Early amniotomy and early oxytocin for
prevention of, or therapy for, delay in first stage spontaneous labour
REFERENCES compared with routine care. Cochrane Database Syst Rev
2013;(8):CD006794.
1. Joint Policy Statement on Normal Childbirth. Continuous support for 22. National Childbirth Trust. Rupture of the membranes in labour.
women during childbirth. J Obstet Gynaecol Can 2008;30:1163–5. London: NCT; 1989.
2. Lee L, Dy J, Azzam H. Management of spontaneous labour at term in 23. Simkin P. Stress, pain, and catecholamines in labor: part 1. A review.
healthy women. J Obstet Gynaecol Can 2016;38:843–65. Birth 1986;13:227–33.
3. Chaillet N, Belaid L, Crochetière C, et al. Nonpharmacologic ap-
24. Bonapace J. Trusting birth with the Bonapace method. Keys to loving
proaches for pain management during labor compared with usual care:
your birth experience. Montreal: Juniper Publishing; 2015.
a meta-analysis. Birth 2014;41:122–37.
4. Dozier AM, Howard CR, Brownell EA, et al. Labor epidural anesthesia, 25. Foureur M. Creating birth space to enable undisturbed birth. In: Fahy
obstetric factors and breastfeeding cessation. Matern Child Health J K., Foureur M., Hastie C., editors. Birth territory and midwifery guard-
2013;17:689–98. ianship: theory for practice, education and research. Edinburgh: Books
for Midwives; 2008. p. 57–78.
5. Hodnett ED. Pain and women’s satisfaction with the experience of
childbirth: a systematic review. Am J Obstet Gynecol 2002;186:S160– 26. Sheiner EK, Sheiner E, Shoham-Vardi I, et al. Ethnic differences influ-
72. ence care giver’s estimates of pain during labour. Pain 1999;81:299–305.
6. Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for 27. Sheiner E, Sheiner EK, Hershkovitz R, et al. Overestimation and under-
women during childbirth. Cochrane Database Syst Rev estimation of labor pain. Eur J Obstet Gynecol Reprod Biol
2013;(7):CD003766. 2000;91:37–40.
7. Ullman R, Smith LA, Burns E, et al. Parenteral opioids for maternal 28. Melzack R, Katz J. Pain measurement in persons in pain. In: McMahon
pain relief in labour. Cochrane Database Syst Rev 2010;(9):CD007396. S., Koltzenburg M., Tracey I., et al., editors. Wall & Melzack’s textbook
of pain. 4th ed. Edinburgh: Churchill Livingstone; 1999. p. 337–51.
8. Simkin P, Bolding A. Update on nonpharmacologic approaches to
relieve Labor pain and prevent suffering. J Midwifery Womens Health 29. Price DD, Harkins SW, Baker C. Sensory-affective relationships among
2004;49(6):489–504. different types of clinical and experimental pain. Pain 1987;28:297–307.
9. Leap N, Dodwell M, Newburn M. Working with pain in labour: an 30. Chapman CR, Gavrin J. Suffering and its relationship to pain. J Palliat
overview of evidence. New Digest 2010;49:22–6. Care 1992;9:5–13.
10. Lowe NK. The nature of labor pain. Am J Obstet Gynecol 31. Lederman RP, Lederman E, Work BA Jr, et al. The relationship of ma-
2002;186:S16–24. ternal anxiety, plasma catecholamines, and plasma cortisol toprogress in
labor. Am J Obstet Gynecol 1978;132:495–500.
11. Lundgren I, Dahlberg K. Women’s experience of pain during child-
birth. Midwifery 1998;14:105–10. 32. Melzack R, Wall PD. Pain mechanisms: a new theory. Science
1965;150:971–9.
12. Buckley SJ. Hormonal physiology of childbearing: evidence and impli-
cations for women, babies and maternity care. Washington, DC: 33. Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory con-
National Partnership for Women & Families; 2015. trols (DNIC). I. Effects on dorsal horn convergent neurones in the rat.
Pain 1979;6:283–304.
13. Lindblom U, Merskey H, Mumford JM, et al. Pain terms—a current list
with definitions and notes on usage with definitions and notes on usage.
34. Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory con-
Pain 1985;3:215–21.
trols (DNIC). II. Lack of effect on non-convergent neurones,
supraspinal involvement and theoretical implications. Pain 1979;6:305–
14. Fuchs AR, Fuchs F, Husslein P, et al. Oxytocin receptors and human
27.
parturition: a dual role for oxytocin in the initiation of labor. Science
1982;215:1396–8.
35. Uvnas-Moberg K. Oxytocin: the biological guide to motherhood. Ama-
15. Fuchs AR, Fuchs F, Husslein P, et al. Oxytocin receptors in the human rillo, TX: Hale Publishing; 2015.
uterus during pregnancy and parturition. Am J Obstet Gynecol
1984;150:734–41. 36. Tom N, Assinder SJ. Oxytocin in health and disease. Int J Biochem Cell
Biol 2010;42:202–5.
16. Buckley SJ. Ecstatic Birth: Nature’s Hormonal Blueprint for Labor.
EBook 2010. Available at: http://sarahbuckley.com/subscribe-to- 37. Alves E, Fielder A, Ghabriel N, et al. Early social environment affects
sarahs-updates. Accessed on March 7, 2013. the endogenous oxytocin system: a review and future directions. Front
Endocrinol (Lausanne) 2015;6:32.
17. Bonica J. Labour pain. In: McMahon S., Koltzenburg M., Tracey I.,
et al., editors. Wall & Melzack’s textbook of pain. New York: Churchill 38. Heinrichs M, Meinlschmidt G, Wippich W, et al. Selective amnesic
Livingston; 1994. effects of oxytocin on human memory. Physiol Behav 2004;83:31–8.
18. Odent M. The fetus ejection reflex. Birth 1987;14:104–5. 39. Nissen E, Lilja G, Widstrom AM, et al. Elevation of oxytocin levels
early post partum in women. Acta Obstet Gynecol Scand 1995;74:530–
19. Marchand S. The Phenomenon of Pain. IASP, 2015. 3.
242 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
40. Matthiesen AS, Ransjo-Arvidson AB, Nissen E, et al. Postpartum ma- 59. Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or
ternal oxytocin release by newborns: effects of infant hand massage and no analgesia in labour. Cochrane Database Syst Rev
sucking. Birth 2001;28:13–9. 2011;(12):CD000331.
41. Kennell JH, McGrath S. What babies teach us: the essential link 60. Goodfellow CF, Hull MG, Swaab DF, et al. Oxytocin deficiency at de-
between baby’s behavior and mother’s biology. Birth 2001;28:20–1. livery with epidural analgesia. BJOG 1983;90:214–9.
42. Russell JA, Leng G, Douglas AJ. The magnocellular oxytocin system, 61. Szabo AL. Review article: intrapartum neuraxial analgesia and
the fount of maternity: adaptations in pregnancy. Front breastfeeding outcomes: limitations of current knowledge. Anesth
Neuroendocrinol 2003;24:27–61. Analg 2013;116:399–405.
43. Mens WB, Witter A, van Wimersma Greidanus TB. Penetration of neu- 62. Brimdyr K, Cadwell K, Widstrom AM, et al. The association between
rohypophyseal hormones from plasma into cerebrospinal fluid (CSF): common labor drugs and suckling when skin-to-skin during the first
half-times of disappearance of these neuropeptides from CSF. Brain hour after birth. Birth 2015;42:319–28.
Res 1983;262:143–9.
63. Ransjo-Arvidson AB, Matthiesen AS, Lilja G, et al. Maternal analgesia
44. Leng G, Caquineau C, Sabatier N. Regulation of oxytocin secretion. during labor disturbs newborn behavior: effects on breastfeeding, tem-
Vitam Horm 2005;71:27–58. perature, and crying. Birth 2001;28:5–12.
45. Phaneuf S, Rodriguez Linares B, TambyRaja RL, et al. Loss of myome- 64. Riordan J, Gross A, Angeron J, et al. The effect of labor pain relief
trial oxytocin receptors during oxytocin-induced and oxytocin- medication on neonatal suckling and breastfeeding duration. J Hum
augmented labour. J Reprod Fertil 2000;120:91–7. Lact 2000;16:7–12.
46. Al-Zirqi I, Vangen S, Forsen L, et al. Effects of onset of labor and 65. Baumgarder DJ, Muehl P, Fischer M, et al. Effect of labor epidural
mode of delivery on severe postpartum hemorrhage. Am J Obstet anesthesia on breast-feeding of healthy full-term newborns delivered
Gynecol 2009;201:e1–9. vaginally. J Am Board Fam Pract 2003;16:7–13.
47. Grotegut CA, Paglia MJ, Johnson LN, et al. Oxytocin exposure during 66. Beilin Y, Bodian CA, Weiser J, et al. Effect of labor epidural analgesia
labor among women with postpartum hemorrhage secondary to uterine with and without fentanyl on infant breast-feeding: a prospective, ran-
atony. Am J Obstet Gynecol 2011;204:e1–6. domized, double-blind study. Anesthesiology 2005;103:1211–7.
48. Selo-Ojeme D, Rogers C, Mohanty A, et al. Is induced labour in the 67. Torvaldsen S, Roberts CL, Simpson JM, et al. Intrapartum epidural an-
nullipara associated with more maternal and perinatal morbidity? Arch algesia and breastfeeding: a prospective cohort study. Int Breastfeed J
Gynecol Obstet 2011;284:337–41. 2006;1:24.
49. Gu V, Feeley N, Gold I, et al. Intrapartum synthetic oxytocin and its 68. Yim IS, Glynn LM, Schetter CD, et al. Prenatal beta-endorphin as an
effects on maternal well-being at 2 months postpartum. Birth early predictor of postpartum depressive symptoms in euthymic
2016;43:28–35. doi:10.1111/birt.12198. e-pub ahead of print. women. J Affect Disord 2010;125:128–33.
50. Caldeyro-Barcia R, Poseiro JJ. Oxytocin and contractility of the preg- 69. Hoffman DI, Abboud TK, Haase HR, et al. Plasma beta-endorphin
nant human uterus. Ann N Y Acad Sci 1959;75:813–30. concentrations prior to and during pregnancy, in labor, and after deliv-
ery. Am J Obstet Gynecol 1984;150:492–6.
51. Jonas K, Johansson LM, Nissen E, et al. Effects of intrapartum oxyto-
cin administration and epidural analgesia on the concentration of 70. Nelson EE, Panksepp J. Brain substrates of infant-mother attachment:
plasma oxytocin and prolactin, in response to suckling during the contributions of opioids, oxytocin, and norepinephrine. Neurosci
second day postpartum. Breastfeed Med 2009;4:71–82. Biobehav Rev 1998;22:437–52.
52. Bell AF, White-Traut R, Rankin K. Fetal exposure to synthetic oxytocin 71. Rivier C, Vale W, Ling N, et al. Stimulation in vivo of the secretion of
and the relationship with prefeeding cues within one hour postbirth. prolactin and growth hormone by beta-endorphin. Endocrinology
Early Hum Dev 2013;89:137–43. 1977;100:238–41.
53. Olza Fernandez I, Marin Gabriel M, Malalana Martinez A, et al. 72. Zanardo V, Nicolussi S, Giacomin C, et al. Labor pain effects on colos-
Newborn feeding behaviour depressed by intrapartum oxytocin: a pilot tral milk beta-endorphin concentrations of lactating mothers. Biol
study. Acta Paediatr 2012;101:749–54. Neonate 2001;79:87–90.
54. Wiklund I, Norman M, Uvnas-Moberg K, et al. Epidural analgesia: 73. Alehagen S, Wijma B, Lundberg U, et al. Fear, pain and stress hor-
breast-feeding success and related factors. Midwifery 2009;25:e31–8. mones during childbirth. J Psychosom Obstet Gynaecol 2005;26:153–
65.
55. Behrens O, Goeschen K, Luck HJ, et al. Effects of lumbar epidural
analgesia on prostaglandin F2 alpha release and oxytocin secretion 74. Neumark J, Hammerle AF, Biegelmayer C. Effects of epidural analgesia
during labor. Prostaglandins 1993;45:285–96. on plasma catecholamines and cortisol in parturition. Acta Anaesthesiol
Scand 1985;29:555–9.
56. Rahm VA, Hallgren A, Hogberg H, et al. Plasma oxytocin levels in
women during labor with or without epidural analgesia: a prospective 75. Odent MR. Position in delivery. Lancet 1990;335:1166.
study. Acta Obstet Gynecol Scand 2002;81:1033–9.
76. Lagercrantz H, Slotkin TA. The “stress” of being born. Sci Am
57. Scull TJ, Hemmings GT, Carli F, et al. Epidural analgesia in early labour 1986;254:100–7.
blocks the stress response but uterine contractions remain unchanged.
Can J Anaesth 1998;45:626–30. 77. Hillman NH, Kallapur SG, Jobe AH. Physiology of transition from
intrauterine to extrauterine life. Clin Perinatol 2012;39:769–83.
58. Stocche RM, Klamt JG, Antunes-Rodrigues J, et al. Effects of intrathe-
cal sufentanil on plasma oxytocin and cortisol concentrations in women 78. Segal S, Csavoy AN, Datta S. The tocolytic effect of catecholamines in
during the first stage of labor. Reg Anesth Pain Med 2001;26:545–50. the gravid rat uterus. Anesth Analg 1998;87:864–9.
FEBRUARY JOGC FÉVRIER 2018 • 243
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
SOGC CLINICAL PRACTICE GUIDELINE
79. Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for 99. Janssen P, Shroff F, Jaspar P. Massage therapy and labor outcomes: a
women during childbirth. Cochrane Database Syst Rev randomized controlled trial. Int J Ther Massage Bodywork 2012;5:15.
2013;(7):CD003766.
100. Mortazavi SH, Khaki S, Moradi R, et al. Effects of massage therapy and
80. Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models presence of attendant on pain, anxiety and satisfaction during labor.
versus other models of care for childbearing women. Cochrane Data- Arch Gynecol Obstet 2012;286:19–23.
base Syst Rev 2013;(8):CD004667.
101. Chang MY, Wang SY, Chen CH. Effects of massage on pain and
81. Hodnett ED, Downe S, Walsh D. Alternative versus conventional insti- anxiety during labour: a randomized controlled trial in Taiwan. J Adv
tutional settings for birth. Cochrane Database Syst Rev Nurs 2002;38:68–73.
2012;(8):CD000012.
102. Zwelling E. Overcoming the challenges: maternal movement and posi-
82. Hutton EK, Cappelletti A, Reitsma AH, et al. Outcomes associated tioning to facilitate labor progress. MCN Am J Matern Child Nurs
with planned place of birth among women with low-risk pregnancies. 2010;35:72.
CMAJ 2016;188:E8–90.
103. Lawrence A, Lewis L, Hofmeyr GJ, et al. Maternal positions and mobil-
83. Hutton EK, Reitsma AH, Kaufman K. Outcomes associated with ity during first stage labour. Cochrane Database Syst Rev
planned home and planned hospital births in low-risk women attended 2009;(5):CD002006.
by midwives in Ontario, Canada, 2003–2006: a retrospective cohort
study. Birth 2009;36:180–9. 104. Gupta JK, Hofmeyr GJ, Smyth R. Position in the second stage of
labour for women without epidural anaesthesia. Cochrane Database Syst
84. Grattan DR, Kokay IC. Prolactin: a pleiotropic neuroendocrine Rev 2009;(4):CD002006.
hormone. J Neuroendocrinol 2008;20:752–63.
105. Spiby H, Slade P, Escott D, et al. Selected coping strategies in labor: an
85. Doan T, Gardiner A, Gay CL, et al. Breast-feeding increases sleep dura- investigation of women’s experiences. Birth 2003;30:189–94.
tion of new parents. J Perinat Neonatal Nurs 2007;21:200–6.
106. Albers LL. The evidence for physiologic management of the active
86. Doan T, Gay CL, Kennedy HP, et al. Nighttime breastfeeding behavior phase of the first stage of labor. J Midwifery Womens Health
is associated with more nocturnal sleep among first-time mothers at one 2007;52:207–15.
month postpartum. Journal of clinical sleep medicine. J Clin Sleep Med
2014;10:313.
107. Smith CA, Collins CT, Crowther CA, et al. Acupuncture or acupressure
for pain management in labour (Review). Cochrane Database Syst Rev
87. Storey AE, Walsh CJ, Quinton RL, et al. Hormonal correlates of pater- 2011;(7):CD009232.
nal responsiveness in new and expectant fathers. Evol Hum Behav
2000;21:79–95.
108. Borup L, Wurlitzer W, Hedegaard M, et al. Acupuncture as pain relief
during delivery: a randomized controlled trial. Birth 2009;36:5–12.
88. Grattan D. A mother’s brain knows. J Neuroendocrinol 2011;23:1188–
9.
109. Cho SH, Lee H, Ernst E. Acupuncture for pain relief in labour: a sys-
tematic review and meta-analysis. BJOG 2010;117:907–20.
89. Bancroft J. The endocrinology of sexual arousal. J Endocrinol
2005;186:411–27.
110. Ma W, Bai W, Lin C, et al. Effects of Sanyinjiao (SP6) with
90. Buhimschi CS. Endocrinology of lactation. Obstet Gynecol Clin North electroacupuncture on labour pain in women. J Altern Complement
Am 2004;31:963–79. Med 2011;19S:13–8.
91. Stefos T, Sotiriadis A, Tsirkas P, et al. Maternal prolactin secretion 111. Qu F, Zhou J. Electro-acupuncture in relieving labor pain. Evid Based
during labor. The role of dopamine. Acta Obstet Gynecol Scand Complement Alternat Med 2007;4:125–30.
2001;80:34–8.
112. Lee EJ, Frazier SK. The efficacy of acupressure for symptom manage-
92. De Carvalho M, Robertson S, Friedman A, et al. Effect of frequent ment: a systematic review. J Pain Symptom Manage 2011;42:589–603.
breast-feeding on early milk production and infant weight gain. Pediat-
rics 1983;72:307–11. 113. Wiruchpongsanon P. Relief of low back labor pain by using intracuta-
neous injections of sterile water : a randomized clinical trial. J Med
93. Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Assoc Thai 2006;89:571.
Database Syst Rev 2009;(2):CD000111.
114. Bahasadri S, Ahmadi-Abhari S, Dehghani-nik M, et al. Subcutaneous
94. Da Silva FMB, de Oliveira SMJV, Nobre MRC. A randomised con- sterile water injection for labour pain: a randomised controlled trial.
trolled trial evaluating the effect of immersion bath on labour pain. Aust N Z J Obstet Gynaecol 2006;46:102–6.
Midwifery 2009;25:286–94.
115. Mårtensson L, Wallin G. Sterile water injections as treatment for
95. Taha M. The effects of water on labour: a randomised controlled trial. lowback pain during labour: a review. Aust N Z J Obstet Gynaecol
Johannesburg, South Africa: Rand Afrikaans University; 2000. 2008;48:369–74.
96. Kimber L, McNabb M, Haines A, et al. Massage or music for pain relief 116. Hutton EK, Kasperink M, Rutten M, et al. Sterile water injection for
in labour: a pilot randomised placebo controlled trial. Eur J Pain labour pain : a systematic review and meta-analysis of randomised con-
2008;12:961–9. trolled trials. BJOG 2009;116:1158–66.
97. Smith CA, Levett KM, Collins CT, et al. Massage, reflexology and other 117. Derry S, Straube S, Moore RA, et al. Intracutaneous or subcutaneous
manual methods for pain management in labour. Cochrane Database sterile water injection compared with blinded controls for pain manage-
Syst Rev 2012;(2):CD009290. ment in labour. Cochrane Database Syst Rev 2012;(1):CD009107.
98. Silva Gallo RB, Santana LS, Jorge Ferreira CH, et al. Massage reduced 118. Jones L, Othman M, Docwswell T, et al. Pain management for women
severity of pain during labour: a randomised trial. J Physiother in labour: an overview of systematic reviews. Cochrane Database Syst
2013;59:109–16. Rev 2012;(3):CD009234.
244 • FEBRUARY JOGC FÉVRIER 2018
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
No. 355-Physiologic Basis of Pain in Labour and Delivery
119. Hajiamini Z, Masoud SN, Ebadi A, et al. Comparing the effects of ice 135. Thomas ME, Dhiwar MS. Effectiveness of patterned breathing tech-
massage and acupressure on labor pain reduction. Complement Ther nique in reduction of pain during first stage of labour among
Clin Pract 2012;1:169–72. primigravidas. Sinhgad e-J Nurs 2011;1:6–8.
120. Field T. Pregnancy and labor alternative therapy research. Altern Ther 136. VandeVusse L, Irland J, Healthcare WF, et al. Hypnosis for childbirth: a
Health Med 2008;14:28. retrospective comparative analysis of outcomes in one obstetrician’s
practice. Am J Clin Hypn 2007;50:109–19.
121. Bundsen P, Peterson LE, Selstam U. Pain relief in labor by transcutane-
ous electrical nerve stimulation: a prospective matched study. Acta 137. Brown DC, Hammond DC. Evidence-based clinical hypnosis for ob-
Obstet Gynecol Scand Suppl 1981;60:459–68. stetrics, labor and delivery, and preterm labor. Int J Clin Exp Hypn
2007;55:355–71.
122. Chao AS, Chao A, Wang TH, et al. Pain relief by applying transcutane-
ous electrical nerve stimulation (TENS) on acupuncture points during 138. Cyna AM, Andrew MI, Robinson JS, et al. Hypnosis Antenatal Training
the first stage of labor: a randomized double-blind placebo-controlled for Childbirth (HATCh): a randomised controlled trial [NCT00282204].
trial. Pain 2007;127:214–20. BMC Pregnancy Childbirth 2006;6:1–12.
123. Dowswell T, Bedwell C, Lavender T, et al. Transcutaneous electrical 139. Ernst E, Pittler M, Wider B, et al. Mind-body therapies: are the trial
nerve stimulation (TENS) for pain management in labour. Cochrane data getting stronger? Altern Ther Health Med 2007;13:62.
Database Syst Rev 2011;(9):CD007214.
140. Smith CA, Collins CT, Cyna AM, et al. Complementary and alternative
124. Marks GK. Alternative therapies. In: Nichols F.H., Humenick S.S., therapies for pain management in labour. Cochrane Database Syst Rev
editors. Childbirth education: practice, research and theory. Philadel- 2006;(4):CD003521.
phia: Saunders; 2000. p. 376–98.
141. Madden K, Middleton P, Cyna AM, et al. Hypnosis for pain manage-
125. Kumar SB, Yadav R, Yadav RK, et al. Telomerase activity and cellular ment during labour and childbirth. Cochrane Database Syst Rev
aging might be positively modified by a yoga-based lifestyle interven- 2012;(11):CD009356.
tion. J Altern Complement Med 2015;21:370–2. doi:10.1089/
acm.2014.0298. e-pub ahead of print. 142. Boso M, Politi P, Barale F, et al. Neurophysiology and neurobiology of
the musical experience. Funct Neurol 2006;21:187–91.
126. Dykema R. Yoga for fitness and wellness. Belmont, CA: Thomson/
Wadsworth; 2006. p. 192. 143. Trout KK. The neuromatrix theory of pain: implications for selected
nonpharmacologic methods of pain relief for labor. J Midwifery
127. Marc I, Toureche N, Ernst E, et al. Mind-body interventions during Womens Health 2004;49:482–8.
pregnancy for preventing or treating women’s anxiety. Cochrane Data-
base Syst Rev 2011;(7):CD007559. 144. Menon V, Levitin DJ. The rewards of music listening: response and
physiological connectivity of the mesolimbic system. Neuroimage
128. Smith C, Levett KM, Collins CT, et al. Relaxation techniques for pain 2005;28:175–84.
management. Cochrane Database Syst Rev 2011;(12):CD009514.
145. Browning CA. Using music during childbirth. Birth 2000;27:272–6.
129. Curtis K, Weinrib A, Katz J. Systematic review of yoga for pregnant
women: current status and future directions. Evid Based Complement 146. Gagnon AJ, Sandall J. Individual or group antenatal education for child-
Alternat Med 2012;2012:1–13. birth or parenthood, or both. Cochrane Database Syst Rev
2007;(3):CD002869.
130. Urech C, Fink NS, Hoesli I, et al. Effects of relaxation on psychobio-
logical wellbeing during pregnancy: a randomized controlled trial. 147. Mehdizadeh A, Roosta F, Chaichian S, et al. Evaluation of the impact
Psychoneuroendocrinology 2010;35:1348–55. of birth preparation courses on the health of the mother and the
newborn. Am J Perinatol 2005;22:7–9.
131. Gedde-Dahl M, Fors EA. Impact of self-administered relaxation and
guided imagery techniques during final trimester and birth. Complement 148. Ip WY, Tang CS, Goggins WB. An educational intervention to improve
Ther Clin Pract 2012;18:60–5. women’s ability to cope with childbirth. J Clin Nurs 2009;18:2125–35.
132. Hunter LP. A descriptive study of “being with woman” during labor 149. Escott D, Slade P, Spiby H. Preparation for pain management during
and birth. J Midwifery Womens Health 2009;54:111–8. childbirth: the psychological aspects of coping strategy development in
antenatal education. Clin Psychol Rev 2009;29:617–22.
133. Adam ED, Bianchi AL. A practical approach to labor support. J Obstet
Gynecol Neonatal Nurs 2008;37:106–15. 150. McDonald SJ, Middleton P, Dowswell T, et al. Effect of timing of um-
bilical cord clamping of term infants on maternal and neonatal
134. Nabb MTM, Kimber L, Haines A, et al. Does regular massage from late outcomes. Cochrane Database Syst Rev 2013;(7):CD004074.
pregnancy to birth decrease maternal pain perception during labour and
birth?—A feasibility study to investigate a programme of massage, con- 151. Begley CM, Gyte GML, Devane D, et al. Active versus expectant man-
trolled breathing and visualization, from 36 weeks of pregnancy until agement for women in the third stage of labour. Cochrane Database
birth. Complement Ther Clin Pract 2006;12:222–31. Syst Rev 2015;(3):CD007412.
FEBRUARY JOGC FÉVRIER 2018 • 245
Downloaded for Muhammad Fuad Alamsyah (fuadalamsyah9@gmail.com) at Universitas Muslim Indonesia from ClinicalKey.com by Elsevier on March 21, 2018.
For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
Вам также может понравиться
- Assignment 3: Final Project - Comprehensive Literature ReviewДокумент18 страницAssignment 3: Final Project - Comprehensive Literature ReviewJay JalaliОценок пока нет
- Application of Orems Theory To NSG PracticeДокумент26 страницApplication of Orems Theory To NSG PracticeLorde Sungcad Ricafrente100% (3)
- Perioperative Care For CABG PatientsДокумент32 страницыPerioperative Care For CABG PatientsAya EyadОценок пока нет
- Listening Jahshan OET Collection-1 PDFДокумент139 страницListening Jahshan OET Collection-1 PDFss78% (27)
- Guideline No. 402 Diagnosis and Management of Placenta PreviaДокумент13 страницGuideline No. 402 Diagnosis and Management of Placenta PreviaAndrés Gaviria CОценок пока нет
- Maternal and Child Health NursingДокумент11 страницMaternal and Child Health NursingNoelle FabrosОценок пока нет
- Manual of Fertility Enhancing HysterosДокумент210 страницManual of Fertility Enhancing HysterosDinorah MarcelaОценок пока нет
- Research Priorities in Obstetrics SeminarДокумент7 страницResearch Priorities in Obstetrics SeminarSharmistha Debnath83% (6)
- Hydro-, Balneo-, and Spa Treatment in Pain Management PDFДокумент5 страницHydro-, Balneo-, and Spa Treatment in Pain Management PDFfriend717100% (1)
- 9 The Post Anesthesia Care UnitДокумент77 страниц9 The Post Anesthesia Care Unitsanjivdas100% (1)
- Outcomes of HypnoBirthingДокумент21 страницаOutcomes of HypnoBirthingdjoko vincenzho100% (2)
- Nur 091 Midterm PDFДокумент29 страницNur 091 Midterm PDFKIMBERLY CABATOОценок пока нет
- Guideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementДокумент26 страницGuideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementYo Me100% (1)
- Medical Surgical Nursing Patient Centered Collaborative Care Single Volume 8th Edition Ignatavicius Test BankДокумент17 страницMedical Surgical Nursing Patient Centered Collaborative Care Single Volume 8th Edition Ignatavicius Test BankLarryPiercexteaz100% (13)
- Neuroprotección Con MgSO4 CJOG 2019Документ18 страницNeuroprotección Con MgSO4 CJOG 2019Fabricio EguíaОценок пока нет
- Fetal Neural Tube 2021 12 LMBR PDFДокумент24 страницыFetal Neural Tube 2021 12 LMBR PDFwayansiagaОценок пока нет
- Neonatal Pain Assessment EvidenceДокумент4 страницыNeonatal Pain Assessment EvidenceDewi MaharaniОценок пока нет
- Effectiveness of Birth Plan Counselling Based On Shared Decision Making - A Cluster Randomized Controlled Trial (APLANT) .Документ21 страницаEffectiveness of Birth Plan Counselling Based On Shared Decision Making - A Cluster Randomized Controlled Trial (APLANT) .Lúcia CostaОценок пока нет
- Primary Dysmenorrhea ConsensusДокумент11 страницPrimary Dysmenorrhea ConsensusNorman AjxОценок пока нет
- Indonesian ART OutLook From Nursing Care in ART NisaДокумент36 страницIndonesian ART OutLook From Nursing Care in ART NisaAnisah WijayaОценок пока нет
- Disposal of Fetal Remains and Products of ConceptionДокумент8 страницDisposal of Fetal Remains and Products of Conceptionmadimadi11Оценок пока нет
- Massage Intervention For Preterm Infants by Their Mothers: A Randomized Controlled TrialДокумент7 страницMassage Intervention For Preterm Infants by Their Mothers: A Randomized Controlled TrialopanocayОценок пока нет
- 10 1016@j Ijnurstu 2017 02 009 PDFДокумент18 страниц10 1016@j Ijnurstu 2017 02 009 PDFDesiОценок пока нет
- Evans Et Al-2017-Journal of Advanced NursingДокумент41 страницаEvans Et Al-2017-Journal of Advanced NursingBides RebornОценок пока нет
- Technical NotesДокумент8 страницTechnical NotesIsmi Nur KhasanahОценок пока нет
- Journal Homepage: - : Manuscript HistoryДокумент5 страницJournal Homepage: - : Manuscript HistoryIJAR JOURNALОценок пока нет
- Pengkajian Riwayat Dan Pemeriksaan Fisik Pasian PaliatifДокумент7 страницPengkajian Riwayat Dan Pemeriksaan Fisik Pasian PaliatifnrjОценок пока нет
- A Study To Assess The Effectiveness of Interventional Module On Stress Levels Among Infertile Women Attending Infertility Clinics of Selected Hospitals at BagalkotДокумент8 страницA Study To Assess The Effectiveness of Interventional Module On Stress Levels Among Infertile Women Attending Infertility Clinics of Selected Hospitals at BagalkotInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Guideline No. 422a: Menopause: Vasomotor Symptoms, Prescription Therapeutic Agents, Complementary and Alternative Medicine, Nutrition, and LifestyleДокумент18 страницGuideline No. 422a: Menopause: Vasomotor Symptoms, Prescription Therapeutic Agents, Complementary and Alternative Medicine, Nutrition, and LifestyleCARLOS JAVIER DIAZ PINEDAОценок пока нет
- 3 AssignmentДокумент6 страниц3 AssignmentDhasarathanОценок пока нет
- Effect of Birth Ball On Labor Pain Relief A Systematic ReviewДокумент8 страницEffect of Birth Ball On Labor Pain Relief A Systematic Reviewgina hardiatiОценок пока нет
- Maduracion Pulmonar Jurnal Obstetric CanadaДокумент21 страницаMaduracion Pulmonar Jurnal Obstetric CanadaSoy PatoОценок пока нет
- Articulo 1 TraducidoДокумент18 страницArticulo 1 TraducidoPercy AstocazaОценок пока нет
- Intrauterine Growth Restriction: Screening, Diagnosis, and ManagementДокумент8 страницIntrauterine Growth Restriction: Screening, Diagnosis, and ManagementEndang Sri WidiyantiОценок пока нет
- Emss 58085Документ68 страницEmss 58085Moh Hendra Setia LОценок пока нет
- Nursing Interventions For Identifying and Managing Acute Dysphagia Are Effective For Improving Patient OutcomesДокумент9 страницNursing Interventions For Identifying and Managing Acute Dysphagia Are Effective For Improving Patient OutcomesawinsyОценок пока нет
- Prevention and Management of Procedural Pain in The Neonate An U 2016Документ13 страницPrevention and Management of Procedural Pain in The Neonate An U 2016Indra WijayaОценок пока нет
- Harrison Prevention and Management of Pain and Stress in The Neonate 2015Документ8 страницHarrison Prevention and Management of Pain and Stress in The Neonate 2015Sasha Hidayat FullОценок пока нет
- No. 262-Prenatal Screening For and Diagnosis of Aneuploidy in Twin PregnanciesДокумент15 страницNo. 262-Prenatal Screening For and Diagnosis of Aneuploidy in Twin PregnanciesDewa Made Sucipta PutraОценок пока нет
- The Effect and Implication of Developmental Supportive Care Practices in Preterm BabiesДокумент23 страницыThe Effect and Implication of Developmental Supportive Care Practices in Preterm BabiesInternational Journal of Innovative Science and Research Technology100% (1)
- Neetu, Poonam Sheoran, Rashmi PanchalДокумент6 страницNeetu, Poonam Sheoran, Rashmi PanchalMuzdalifah Karina DMОценок пока нет
- Scholarly Capstone PaperДокумент5 страницScholarly Capstone Paperapi-738778945Оценок пока нет
- TecnicasДокумент11 страницTecnicasMonse SantillánОценок пока нет
- Cultural Adaptation and Psychometric Validation ofДокумент20 страницCultural Adaptation and Psychometric Validation ofAhlem MtiraouiОценок пока нет
- Management of Pain Associated With The Insertion of Intrauterine ContraceptivesДокумент9 страницManagement of Pain Associated With The Insertion of Intrauterine ContraceptivesLeonardo Daniel MendesОценок пока нет
- NANDA - Interrupted BreastfeedingДокумент16 страницNANDA - Interrupted BreastfeedingSuéllen EmidioОценок пока нет
- What Impact Does Pregnancy Have On Anxiety About Health?Документ8 страницWhat Impact Does Pregnancy Have On Anxiety About Health?Altar ParssoyОценок пока нет
- The Effectiveness of Complementary ManualДокумент10 страницThe Effectiveness of Complementary ManualAli DptОценок пока нет
- The Guidelines Regarding PuerpДокумент8 страницThe Guidelines Regarding Puerpdyah ayu noer fadilaОценок пока нет
- AnsiedadeДокумент15 страницAnsiedadeTayná MayerОценок пока нет
- 4 Organisation Services WHOДокумент92 страницы4 Organisation Services WHObeno wibowoОценок пока нет
- Emerging Science Combined With Common Sense Gives Parents Better Options For Preventing Autism by Maureen McDonnell, RNДокумент5 страницEmerging Science Combined With Common Sense Gives Parents Better Options For Preventing Autism by Maureen McDonnell, RNautismoneОценок пока нет
- Proposal Presentation SanaДокумент6 страницProposal Presentation SanaGazala ParveenОценок пока нет
- Wa0008. PDFДокумент12 страницWa0008. PDFLal NandaniОценок пока нет
- Contraception For Women With Psychiatric DisordersДокумент14 страницContraception For Women With Psychiatric DisordersFourtiy mayu sariОценок пока нет
- ArtigoДокумент11 страницArtigoDébora AlvesОценок пока нет
- Volume 10 Number 8 Agustus 2018 IJNM PDFДокумент9 страницVolume 10 Number 8 Agustus 2018 IJNM PDFBertus AwОценок пока нет
- A RCT of Psychotherapy in Women With Nausea and Vomiting of PregnancyДокумент10 страницA RCT of Psychotherapy in Women With Nausea and Vomiting of PregnancyvioletavrsОценок пока нет
- Breastfeeding BehaviourДокумент8 страницBreastfeeding Behaviourmaria jose giraldo muneraОценок пока нет
- PJN Jan June 2021 Final Version CompleteДокумент130 страницPJN Jan June 2021 Final Version CompleteJohn Vincent LacuestaОценок пока нет
- Management of Late Intrauterine Fetal Death and Stillbirth - Hywell Dda Guideline 2017Документ9 страницManagement of Late Intrauterine Fetal Death and Stillbirth - Hywell Dda Guideline 2017thariq mubarakОценок пока нет
- Uman2005 PDFДокумент12 страницUman2005 PDFmagda cardenasОценок пока нет
- Capstone Scholarly Paper FinalДокумент5 страницCapstone Scholarly Paper Finalapi-739624128Оценок пока нет
- Preconception Care To Improve Pregnancy Outcomes: The ScienceДокумент8 страницPreconception Care To Improve Pregnancy Outcomes: The SciencekofiОценок пока нет
- WHO Guideline On Antenatal Care (2016)Документ41 страницаWHO Guideline On Antenatal Care (2016)agriloОценок пока нет
- Acu Back PelvicPain in Pregnancy RCT 1Документ6 страницAcu Back PelvicPain in Pregnancy RCT 1QuackeryОценок пока нет
- NBS - 2013may - The Newborn Screening Story - How One Simple Test Changed Lives Science and Health in AmericaДокумент50 страницNBS - 2013may - The Newborn Screening Story - How One Simple Test Changed Lives Science and Health in AmericaMónica Galvan-MSalОценок пока нет
- Perinatal Palliative Care: A Clinical GuideОт EverandPerinatal Palliative Care: A Clinical GuideErin M. Denney-KoelschОценок пока нет
- 4539 8480 1 SMДокумент8 страниц4539 8480 1 SMdianОценок пока нет
- 5-Hubungan Tekanan Darah Dan Paritas Dengan Kejadian Eklampsia-Wibowo SafitriДокумент6 страниц5-Hubungan Tekanan Darah Dan Paritas Dengan Kejadian Eklampsia-Wibowo SafitriAkhmad Ahdiyat BudiantoОценок пока нет
- Contraception: Chapter OutlineДокумент15 страницContraception: Chapter OutlinedianОценок пока нет
- 3 s2.0 B9780323321082000585Документ17 страниц3 s2.0 B9780323321082000585dianОценок пока нет
- 3 s2.0 B9780323321082000585Документ17 страниц3 s2.0 B9780323321082000585dianОценок пока нет
- Risk Factors For Complete Uterine Rupture: ObstetricsДокумент8 страницRisk Factors For Complete Uterine Rupture: ObstetricsdianОценок пока нет
- Scandinavian Journal of Pain: Harald BreivikДокумент2 страницыScandinavian Journal of Pain: Harald BreivikdianОценок пока нет
- Eng PDFДокумент136 страницEng PDFCătălina PoselețchiОценок пока нет
- G1NLCX022373035Документ1 страницаG1NLCX022373035dianОценок пока нет
- Endo Pharmaceuticals Visual GuideДокумент6 страницEndo Pharmaceuticals Visual GuideDUNCAN0420Оценок пока нет
- The Polyanalgesic Consensus Conference PACC Recommendations For Trialing of Intrathecal Drug Delivery Infusion Therapy. Neuromodulation 2017Документ22 страницыThe Polyanalgesic Consensus Conference PACC Recommendations For Trialing of Intrathecal Drug Delivery Infusion Therapy. Neuromodulation 2017Michael HuntОценок пока нет
- ANALGESIC DRUGS (DR - Dlawer)Документ37 страницANALGESIC DRUGS (DR - Dlawer)OMAR NASSERОценок пока нет
- Sketchy OpioidsДокумент1 страницаSketchy OpioidsSandy MaeОценок пока нет
- Problems With PainДокумент3 страницыProblems With PainMayanda UtamiОценок пока нет
- Kartu Stock Obat: Apotek EmpangДокумент17 страницKartu Stock Obat: Apotek EmpangKlinik EmpangОценок пока нет
- Opioids, Pain, and FearДокумент3 страницыOpioids, Pain, and FearlucianaclarkОценок пока нет
- Laporan Rak NarkotikaДокумент18 страницLaporan Rak NarkotikaaliyahОценок пока нет
- Opioid Use Disorder: A VA Clinician's Guide To Identification and Management of Opioid Use Disorder (2016)Документ20 страницOpioid Use Disorder: A VA Clinician's Guide To Identification and Management of Opioid Use Disorder (2016)Hollman Salamanca DimasОценок пока нет
- UMT 02 - PT 652 Pharmacology in Rehabilitation - 01.13.2021.2020Документ14 страницUMT 02 - PT 652 Pharmacology in Rehabilitation - 01.13.2021.2020Nabil KhatibОценок пока нет
- Analgesics in PeriodonticsДокумент43 страницыAnalgesics in PeriodonticsRicha BhosaleОценок пока нет
- 592-Article Text-1029-1-10-20190429Документ6 страниц592-Article Text-1029-1-10-20190429Abed AlhaleemОценок пока нет
- YSA v. Najam Azmat, 11th Cir. (2015)Документ60 страницYSA v. Najam Azmat, 11th Cir. (2015)Scribd Government DocsОценок пока нет
- MassageДокумент7 страницMassageMuhammad NasrullahОценок пока нет
- CFC Foundation CriteriaДокумент7 страницCFC Foundation CriteriaalrsxvxОценок пока нет
- Preoperative Pain Management Education An Evidence-Based Practice ProjectДокумент8 страницPreoperative Pain Management Education An Evidence-Based Practice Projectfachrudin arОценок пока нет
- TadeДокумент154 страницыTadeCHALIE MEQU100% (1)
- AlgesiaДокумент1 страницаAlgesiaenirdnas14100% (2)
- Jurnal Low Back Pain PDFДокумент5 страницJurnal Low Back Pain PDFFikar AxlrosesОценок пока нет
- A Review of Pain Management in The Neonate: Evidence-Based Pharmacy PracticeДокумент4 страницыA Review of Pain Management in The Neonate: Evidence-Based Pharmacy PracticeAndriy SubieОценок пока нет
- Chemistry H3 Notes The Synthesis of ParacetamolДокумент15 страницChemistry H3 Notes The Synthesis of ParacetamolSimon KohОценок пока нет
- KetamineДокумент7 страницKetamineAshiyan IrfanОценок пока нет