Академический Документы
Профессиональный Документы
Культура Документы
Clinical Chemistry 3: Endocrinology
Загружено:
Romie SolacitoИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Clinical Chemistry 3: Endocrinology
Загружено:
Romie SolacitoАвторское право:
Доступные форматы
ENDOCRINOLOGY REVIEW NOTES
ENDOCRINOLOGY – the study of endocrine glands and their secretions
HYPOTHALAMUS – secretes PINEAL GLAND – secretes melatonin
antidiuretic hormone and oxytocin
PITUITARY GLAND – ANTERIOR:
THYROID – secretes thyroxine, secretes adrenocorticotropic
triiodothyronine, and calcitonin hormone, thyroid stimulating
hormone, growth hormone, prolactin,
THYMUS GLAND – secretes follicle stimulating hormone,
thymosin luteinizing hormone; POSTERIOR:
stores antidiuretic hormone and
HEART – secretes natriuretic oxytocin
peptides
PARATHYROID GLAND –
secretes parathyroid hormone
ADRENAL GLAND – CORTEX:
secretes cortisol and aldosterone; STOMACH – secretes gastrin, secretin,
MEDULLA: secretes adrenaline and somatostatin, and cholecystokinin
noradrenaline
PANCREAS – secretes
KIDNEYS – secretes erythropoietin insulin and glucagon
TESTES – secretes androgen OVARIES – secretes
and testosterone estrogen and progesterone
neurotransmitter
SHORT-TERM;
QUICK
RESPONSE
target cell with receptor
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 1
ENDOCRINOLOGY REVIEW NOTES
HORMONES – chemical substance produced by glands that has specific LONG-TERM;
regulatory effect on the activity of a certain organ/s or cell type SLOW RESPONSE
➢ The interaction between the hormone and its receptor triggers a cascade of biochemical reactions in
the target cell that eventually modify the cell’s function or activity.
PURPOSE:
➢ Growth and development
➢ Homeostatic control
➢ Energy production and metabolic regulation
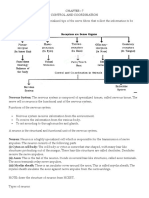
CELL SIGNALING:
AUTOCRINE EXOCRINE ENDOCRINE PARACRINE NEUROENDOCRINE JUXTACRINE
Action of hormone Action of Action of hormone Action of hormone Associated with the Contact
with in the same hormone on to a distant area with in the local central nervous system dependent
cell surface area signaling; plays a
key role in immune
response
CLASSIFICATION OF HORMONES
STEROID PROTEINS AMINES
➢ Nature: Lipid - Cholesterol ➢ Nature: Glycoproteins or ➢ Nature: Amino Acids
➢ Bound to carrier molecules Polypeptides ➢ Water soluble and insoluble
➢ Water Insoluble ➢ Water soluble ➢ Not or bound to carrier
➢ Immediate diffusion through the ➢ Not bound to carrier molecules molecules
cell using the lipid bilayer ➢ Short half-life: 4 to 40 minutes ➢ Examples: Catecholamines
➢ Long half-life: 4 to 120 minutes ➢ Examples: Glycoprotein – and Thyroxine
➢ Examples: Testosterone, FSH, TSH, EPO, Beta-HCG;
Estrogen, Cortisol, Polypeptides – Insulin, PTH, MNEMONIC: CT
Progesterone ACTH, ADH, GH, Calcitonin
MNEMONIC: PECT MNEMONIC: Glycoprotein - BEFT
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 2
ENDOCRINOLOGY REVIEW NOTES
POSITIVE FEEDBACK
➢ Stabilizes hormone axis when the level or effect is
MECHANISM
FEEDBACK
BELOW normal
➢ Leads the glands to Increased Production
NEGATIVE FEEDBACK
➢ Stabilizes hormone axis when the level or effect is
ABOVE normal
➢ Leads the glands to Decreased Production
HORMONE-RECEPTOR REGULATION
• Excessively increased levels of hormones may be regulated
through decreased receptors.
DOWN REGULATION OR DESENSITIZATION
• Example: Increased levels of insulin may lead to obesity –
Diabetes Mellitus Type 2
• AFFINITY – how likely the agonist will bind to the receptor
• EFFICACY – how good is the agonist in stimulating the receptor to cause biochemical changes in the cell
1. UNCOUPLING: The receptors
ability to interact with the
downstream effect pathway
2. SEQUESTRATION:
Endocytosis of the receptor and
stored in the early endosome
3. DOWN REGULATION: Stores
the receptors from the cell
surface to the early endosome –
late endosome –lysosome -
digested
PLATELET PATHWAYS (G PROTEIN)
A ligand attaches to the Results in a mechanical Triggers the Guanosine DP will be
receptor change in the receptor G protein replaced by Guanosine TP
Activate phospholipase C Phospholipase C degrades Release of Activates protein
by the transfer of P to PC the phospholipids Calcium kinase or any enzyme
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 3
ENDOCRINOLOGY REVIEW NOTES
SPECIFICITY SPILL OVER
• High concentrations of hormones can affect certain unintended actions through a receptor – effector
pathway different from but homologous to normal signaling mechanisms.
• Example: Increased levels of cortisol (glucocorticoid) may cause it to perform mineralocorticoid
function
Hormone Multi-specificity - Excessively increased levels of hormones may cause relative changes to
related hormones produced in the same organ.
HYPOTHALAMUS & PITUITARY GLANDS
PITUITARY GLAND HYPOTHALAMUS
• Pituitary literally means to “spit • Endocrine and
mucus” Autonomic
• Master Gland • BEHAVIORAL
• The pituitary is also referred to • Function to regulates
as the hypophysis, from Greek 8 major hormones
meaning “undergrowth” by the hypophysis;
• The pituitary resides in a pocket temperature
of the sphenoid (the sella regulation; controls
turcica, meaning “Turkish food and water
saddle”) and is surrounded by intake; sexual
dura mater behavior and
• Function to cessation of growth; reproduction;
alterations in metabolism; mediation of
Failure of Gonadal, Thyroidal, emotional responses
Adrenal Function
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 4
ENDOCRINOLOGY REVIEW NOTES
HYPOTHALAMUS REGIONS
➢ Composed of Supraoptic and Paraventricular nuclei (secretes CRH) which
synthesized Vasopressin/Antidiuretic Hormone & Oxytocin and released
to Supraopticohypophysial Tract and Tuberohypophyseal Tract and stored to
Supraoptic/Anterior Posterior Pituitary
Region
➢ Damaged: Diabetes Insipidus – absent or decreased ADH secretion from
the hypothalamus or neurohypophysis
Mnemonic: SSP
➢ Superchiasmatic Nucleus – controls the Diurnal or Circadian Rhythms and
inhibits release of Melatonin
▪ “Body Clock”; Body Temperature; Hormone Secretion; Menstrual Cycle
➢ Ventromedial Nucleus - controls eating and satiety center
▪ Damaged: Hyperphagia - abnormally increased appetite for food
Tuberal/Middle
➢ Lateral Hypothalamus - controls appetite and feeding center
Region
▪ Damaged: Lack of Appetite
Mnemonic: VAL • Arcuate Nucleus - secretes releasing and inhibiting hormones
▪ Activates the release of Growth hormone, Adrenocorticotropic hormone,
Follicle stimulating hormone, and Prolactin
Mamillary/Posterior • Function for thermoregulation and cognitive reasoning
Region
• The Hypothalamus is PITUITARY GLAND
sensitive to different ✓ Controlled by hypothalamic releasing hormones stimulate the
stimulus in the body. cells of the anterior pituitary to release hormones.
• The Hypothalamus produces ✓ Nerve impulses from the hypothalamus stimulates nerve
hormones that activates the endings.
pituitary gland. ✓ Hormones are released in a pulsatile manner - Luteinizing
• The main function of the hormones (55 mins)
hypothalamus is to maintain ✓ Circadian Rhythms – ACTH, nadir - 11:00 p.m. and 3:00 a.m.,
body homeostasis and peak - 6:00 to 9:00 a.m.
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 5
ENDOCRINOLOGY REVIEW NOTES
EMBRYOLOGY AND ANATOMY
✓ Three distinct parts:
o Par intermedialis - poorly developed
o Posterior/Neurohypophysis - storage
and release of oxytocin and vasopressin
o Anterior/Adenohypophysis – from
Rathke’s pouch, enveloped by the
sphenoid bone.
✓ Median eminence and Pituitary stalk –
formation of the hypothalamic-hypophyseal
unit.
PITUITARY GLAND: Adenohypophysis
✓ Receives 80% to 90% of its blood supply
and many hypothalamic factors via the
hypothalamic– hypophyseal portal system,
also contained in the stalk.
PROGENITOR CELL TYPES
Somatotrophs Lactotrophs Thyrotrophs Gonadotrophs Corticotrophs
Growth Hormones Prolactin Thyroid Luteinizing Adrenocorti-
Stimulating Hormone; Follicle cotropic Hormone
Hormone Stimulating
Hormone
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 6
ENDOCRINOLOGY REVIEW NOTES
EFFECTS OF THE ANTERIOR PITUITARY HORMONES
GH ACTH TSH LH FSH PRL
Promotes Stimulates the Stimulates the Controls Controls Milk production
growth adrenal cortex thyroid to reproductive reproductive
release thyroid functions functions
hormones
PITUITARY GLAND: Adenohypophysis (cont.)
✓ These pituitary hormones are either tropic - specific
for another endocrine gland, or they are direct
effectors -act directly on peripheral tissue.
✓ Tropic hormones: FLAT
o LH - directs testosterone production from Leydig
cells in men and ovulation in women
o FSH - responsible for ovarian recruitment and
early folliculogenesis in women and
spermatogenesis in men
o TSH - directs thyroid hormone production from the
thyroid
o ACTH - regulates adrenal steroidogenesis
GROWTH HORMONE
• also called somatotropin, is structurally related GROWTH HORMONE FUNCTION:
to prolactin and human placental lactogen. • Decrease Adipose – increased lipolysis;
• Secreted by the somatotrophs of the pituitary decreased glucose uptake
gland • Increased Liver Function – Increase
• The most abundant pituitary hormone protein synthesis; increase
gluconeogenesis; increased insulin like
• Reference value: <7 ng/ml
growth factor/somatomedins.
• Increase Muscle Mass – increase
protein intake; decrease glucose uptake.
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 7
ENDOCRINOLOGY REVIEW NOTES
• Regulated by Growth Hormone Regulating Hormone and Somatostatin (inhibits)
• Somatomedins/Insulin-like
Growth Factor – indirect
effect
o Produced and secreted
primarily by the liver
o Similar subunit with
insulin
o Anabolic hormone:
GROWTH
o Binds to insulin receptors
o Increase Protein, RNA,
and DNA
o Increase protein intake
and decrease glucose
uptake
• Elevated plasma growth
hormone levels
• Growth hormone facilitates
the movement of free fatty
acids
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 8
ENDOCRINOLOGY REVIEW NOTES
NOTES:
• IGF binding protein 3 (IGFBP-3) -
pathophysiology of several human
cancers.
• P53 tumor suppressor gene was recently
shown to upregulate active IGFBP-3
secretion.
• Low levels of IGFBP-3 were positively
correlated with higher rates of colorectal
cancer risk
GROWTH HORMONE DISORDERS
Gigantism Acromegaly Dwarfism
• Robert Wadlow: 6 feet tall • Hypersecretion of growth • Patients retain their normal
when he was 8 years old. hormone in adulthood body proportion relative to the
• Cause: hypersecretion of • Excess GH produced after severity of GH deficiency.
growth hormone in childhood the closure of the epiphyseal • Commonly, it does not affect
• Excess GH production prior plate mental capabilities
to closure of epiphyseal plate • Treatment: Surgery; Trans- • Treatment: Recombinant
sphenoidal adenomectomy; Human Growth Hormone
Focused beam or irradiation
INTERPRETATION:
Laboratory Diagnosis - Considerations: • Persistent increase = ACROMEGALY
• Fasting (with 30 minutes rest prior to
• If decreased:
collection)
• If increased, do confirmatory test: o Insulin Tolerance Test: insulin
Overnight Fasting Serum induced hypoglycemia – gold standard
• Give 100 grams OGT after taking basal o Arginine Stimulation Test: GHRH
GH coupled with L-arginine
• Take serum sample is taken at zero, **Failure to increase GH more than 5 ng/ml
60min and 120min (Adult) and 10ng/ml (Children) indicates GH
deficiency
PROLACTIN
• Effector hormone
• Initiates and maintains lactation PROLACTIN DISORDERS:
• Decreased Levels:
• Promotes breast tissue development o Menstrual Irregularity, infertility, amenorrhea,
• Major inhibitor: Dopamine and galactorrhea
• Highest: 4am, 8am, 8pm, and 10pm o Iatrogenic: aldomet, phenothiaines, reserpine
• Increased Levels
o >150 ng/mL indicate prolactinoma
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 9
ENDOCRINOLOGY REVIEW NOTES
PROLACTIN DISORDERS –
PROLACTINOMA:
• Most common type of functional
pituitary tumor.
• Women: menstrual irregularity or
amenorrhea, infertility, or galactorrhea.
• Men: reduced libido, or complaints of
erectile dysfunction.
LABORATORY DIAGNOSIS
•Considerations: Overnight Fasting, and blood
MANAGEMENT OF PROLACTINOMA:
collected 3 - 4 hours after the individual • depends on the size of the tumor
awakened (macroadenomas [tumor size >10 mm or
• Usually tested with Thyroid Hormone Panel microadenomas [tumor size < 10 mm].
o If Increased Thyroid • Dopamine Agonist for macroprolactinoma –
bromocriptine mesylate (parlodel) or
Releasing Hormone =
cabergoline (dostinex) for macroprolactinoma.
Idiopathic Thyroid Stimulating
Galactorrhea – Hormone = Prolactin
lactation occurring in o If tertiary increase: Thyroid Releasing Hormone = Thyroid Stimulating
women with normal Hormone = Prolactin
prolactin. o If secondary increase: Thyroid Stimulating Hormone = Prolactin
o If primary increase:
Oxytocin and Vasopressin - the
Thyroxin and Triiodothyronine but
synthesis of each of these hormones is
decreased Prolactin
tightly linked to the production of
neurophysin and it is plausible they have
POSTERIOR PITUITARY GLAND
an autocrine or a paracrine function.
• An outgrowth of the hypothalamus composed of
neural tissue.
• Hypothalamic neurons pass through the neural stalk and end in the posterior pituitary.
• Does not have cells that produce hormones
• Oxytocin and Antidiuretic Hormone/Vasopressin synthesized in the supraoptic and
paraventricular nuclei of the hypothalamus and transported to the neurohypophysis via their axons
in the hypothalamoneurohypophyseal tract.
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 10
ENDOCRINOLOGY REVIEW NOTES
OXYTOCIN
• Peptide like VASOPRESSIN/ADH
• Transported by carrier protein
• stimulated by stretching of the cervix and
vagina during parturition called
“Fergusson Reflex”
• Stimulated by birth canal, uterus and
touch receptors of the breast
• Used for labor induction and to support
labor in case of difficult parturition.
• Use to stimulate breast feeding
• Common drug name: Pitocin, Syntocin
ANTIDIURETIC HORMONE/VASOPRESSIN
• Peptide hormone about 2.3 to 3.1 pg/ml
• Increases distal convoluted tubules and collecting ducts’
water permeability
• Promotes water homeostasis
• Regulated by plasma osmolality and blood pressure
LABORATORY DIAGNOSIS
• Overnight Water Deprivation Test
(Concentration Test)
o 8 to 12 hours water deprivation
o Urine osmolality does not rise
above 300 mOsm/kg
• Normal ADH Level: 1 to 5 pcg/ml
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 11
ENDOCRINOLOGY REVIEW NOTES
ANTIDIURETIC HORMONE DISEASE ASSOCIATION
Diabetes Insipidus True Diabetes Nephrogenic Diabetes Gestational Diabetes
Insipidus Insipidus Insipidus
• Normoglycemia • Hypothalamic/ • Normal ADH with • Pregnant women
• Polyuria with low neurogenic/ cranial deficient receptors produce
specific gravity • Deficiency of ADH • Failure of kidneys vasopressinase in
• Polydipsia with normal ADH to respond to ADH the placenta, which
• Polyphagia receptors levels breaks down ADH.
• Failure of Pituitary • Associated with
gland to secrete pre-eclampsia,
ADH HELLP syndrome,
and acute fatty liver
in pregnancy
TREATMENT
• Desmopressin intake (Neurogenic
and Gestational DI)
• Carbamazepine (Neurogenic DI)
• Hydrochlorothaizideor
Indomethacin (nephrogenic)
SYNDROME OF INAPPROPRIATE ADH
SECRETION (SIADH)
• It is a condition characterized by excessive
secretion of ADH. It is often associated with
hyponatremia and total body fluid is
increased
o Brain injury or trauma
o Brain tumor
o Fluid imbalance after surgery
o Infection in the brain or in the myelin
sheets
o Small cell carcinoma in the lungs
o Stroke
• Treatment: Anti - ADH antagonist receptor
drugs (Conivaptan, Tolvaptan) and ADH
Inhibitor (Demeclocycline)
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 12
ENDOCRINOLOGY REVIEW NOTES
ADRENAL GLAND
• Pyramid shaped gland
• Composed of two conjoined
but distinct glands:
o Inner Medulla
o Outer Cortex
THE CORTEX
• The yellow outer region
• Major site of steroid production
• Utilized cholesterol as precursor for steroids
• Cyclopentanoperhydrophenanthrene Ring
ZONES OF CORTEX
• Outermost layer • Mineralocorticoids:
ZONA • Comprises 10% of the cortex Aldosterone
GLOMERULOSA • Secretes the mineralocorticoids • Potassium
(response to RAAS)
• Middle layer • Glucocorticoid: Cortisol
ZONA
• Comprises 75% of the cortex • ACTH
FASICULATA
• Secretes Glucocorticoids
• Innermost layer (before • Androgens (Weak):
ZONA medulla) Androstenedione and
RETICULARIS • Comprises 10% of the cortex Dehydroepiandrosterone
• Secretes androgens • ACTH
Go Find Romie Make Good Sex
CORTEX: GLUCOCORTICOIDS - CORTISOL
SYNTHESIS & SYNTHESIS of
• Most important glucocorticoid CORTISOL
• Regulated by Adrenocorticotropic Hormone • Prolonged fasting
(ACTH) and Corticotropic Hormone (CTH) • Prolonged exercise
• Stress
• The only adrenal hormone that exhibits
• Circadian Rhythm
negative feedback to the pituitary
• 90 to 95% are inactive and are bound to Cortisol-
Binding Protein Globulin (Transcortin)
• Highest at 6am to 9am and lowest at 11pm to 3am
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 13
ENDOCRINOLOGY REVIEW NOTES
CORTEX: GLUCOCORTICOID
INCREASE INHIBIT ALLOWS
• Protein Catabolism • Adrenocorticotropic Hormone • Sensitization of arterioles to
• Hepatic glycogen synthesis secretion action of noradrenaline
• Hepatic gluconeogenesis • Water excretion
CHRONIC CORTISOL RELEASE
• May affect the brain
o Atrophy: inability to convert short term
memory to long term memory
o Inability to concentrate and make decisions
o Anxiety and Depression
• May affect the Thymus
o Inability to produce immune cells (Immune
Suppression)
DISEASE ASSOCIATION: ADRENAL HYPOFUNCTION
CAUSES:
COMMON: IATA
• Autoimmune adrenalitis Adrenal Crisis • Infection, trauma and surgery
• Tuberculosis Hypovolemia • Meningococcemia
• Adrenalectomy Hypoglycemia • Waterhouse Friderichsen
• Iatrogenic (most common)
LESS COMMON: THAHA HYPOCORTISOLISM
• Tumor PRIMARY SECONDARY
HYPOCORTISOLISM HYPOCORTISOLISM
• Amyloidosis
Addison’s Disease Secondary Adrenal
• Hemochromatosis
• Chronic Adrenal Insufficiency
• Histoplasmosis
Insufficiency • Cause: ACTH loss; may
• Adrenal hemorrhage be associated with tumor
• Addisonian crisis
• Autoimmune Disease • Characteristic Finding:
• Infections absence of
HYPOCORTISOLISM LAB. DIAG.
hyperpigmentation and
• ACTH Stimulation Test: decreased ACTH with
Corsyntropinstimulation test and normal adrenal
Synacthen Stimulation Test stimulation
• Metyrapone Test
• Insulin Tolerance Test: Gold
Standard for Secondary and
Tertiary Hypocortisolism
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 14
ENDOCRINOLOGY REVIEW NOTES
SYNACTHEN STIMULATION TEST
SYNACTHEN STIMULATION
• Tetracosactide (synacthen) stimulates the release of TEST PROCEDURE
corticosteroids such as cortisol from the adrenal glands. • Collect blood at 9am
• Normal result: Plasma cortisol baseline: >190mmol/L • Inject 250ug Synacthen IM
• Measure cortisol after 30mins
and After Synacthen: increment of 200nmol/L with peak
and 60mins
>550 nmol/L • Day 1: inject 1mg Synacthen
• Primary Adrenal Insufficiency: Plasma cortisol on Day • Repeat on Day 2 and Day 3
4 is <200 nmol/L • Measure plasma cortisol at 9am
• Secondary Adrenal Insufficiency: Cortisol level is at
least 200 nmol/L or above
METYRAPONE TEST
TREATMENT
• Cortisol injection • Metyrapone - 11 B-Hydroxylase inhibitor (cortisol precursor)
• Hydrocortisone
• Alternative confirmatory for secondary and tertiary adrenal
• Prednisone/Prednisolone
insufficiency
• Normal result: Increase of ACTH; increase urine cortisol
• Positive result: Decrease of ACTH
HYPERCORTISOLISM LAB. DIAG.
ADRENAL HYPERFUNCTION/HYPERCORTISOLISM
• Screening Test – 24SOI
– Cushing’s Syndrome o 24-Hour Urinary Free Cortisol
o Overnight Dexamethasone
• Corticosteroid or ACTH treatment – Cushing’s Test
Syndrome o Salivary Cortisol Test
• Pituitary Hypersecretion – Cushing’s Disease o Insulin Hypoglycemia Test
• Adrenal Adenoma/Carcinoma • Confirmatory Test – Late
Midnight Cable
• Ectopic ACTH Secretion
o Low-Dose Dexamethasone
Test
o Midnight Plasma Cortisol
DEXAMETHASONE PROCEDURE
o CRH Stimulation Test
• Administered 1mg to suppress
early morning cortisol at 11pm
• Low Dose: 1 to 2mg HYPERCORTISOLISM TREATMENT:
• High Dose: 8mg
• Adrenalectomy
NOTE: Suppressed total cortisol <3.6 • Drugs that block steroid synthesis (ketoconazole,
ug/dL: 8am to 9am = negative test metyrapone, and amino glutethimide)
• Anti-neoplastic drugs (Mitotane)
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 15
ENDOCRINOLOGY REVIEW NOTES
CORTEX: MINERALOCORTICOID
• Aldosterone
• Most important
mineralocorticoid
• Regulates water and electrolyte
homeostasis by:
o Na and Cl Retention and
o K and H excretion
• Affects systemic blood
pressure
DISEASE ASSOCIATION: Primary
Hyperaldosteronism - Conn’s
Syndrome
• Characterized by increased
Aldosterone production
including Hypokalemia,
Hypernatremia,
Hypertension and DISEASE ASSOCIATION: Liddle’s DISEASE ASSOCIATION:
Syndrome Secondary Hyperaldosteronism
metabolic Alkalosis
• Low renin level and low to normal • Barterr’s syndrome
• Adrenal adenoma Aldosterone • Defect in the kidney's ability to
• Zona Glomerulsa • Inherited defect of Kidney reabsorb sodium
hypertrophy tubule causing excess sodium • Excess sodium excretion
reabsorption and potassium loss causing a rise in aldosterone
level
• potassium wasting
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 16
ENDOCRINOLOGY REVIEW NOTES
MINERALOCORTICOIDS: LABORATORY DIAGNOSIS
• Screening Test: Plasma Aldosterone
Concentration/Plasma Renin Activity Ratio
(PAC/PRA)
• Confirmatory Test: Saline Suppression Test
o Normal result: <5 ng/dL aldosterone; increase
may indicate Conn’s Syndrome
SALINE SUPPRESSION PROCEDURE
• Infuse 2L Saline in 4 hours or oral
10-12 mg NaCl for 3 days
• Collect sample
• Measure Aldosterone
MINERALOCORTICOIDS: HYPOALDOSTERONISM HYPERALDOSTERONISM
TREATMENT
• Caused by destruction of adrenal glands and or
• Aldosterone Antagonist Drug:
deficiency of precursors Spironolactone
• Associated with enzyme deficiency: 21-Hydroxylase • Tumor Ablation
• Maybe Iatrogenic cause (ACE inhibitors, NSAIDs, • Diuretic Drugs: Triamterene,
Cyclosporine) Amiloride
• Renal Dysfunction due to Diabetic Nephropathy.
• Characterized by hyperkalemia and metabolic
HYPOALDOSTERONISM
acidosis LABORATORY DIAGNOSIS
HYPOALDOSTERONISM TREATMENT • Renin Stimulation Challenge Test
• Fludrocortisone administration in combination o Uses 40 - 80mg furosemide
with Thiazides orally or IM and compare to
basal Renin Activity after 4 hours
in UPRIGHT POSTURE
MINERALOCORTICOIDS: Congenital Adrenal o Normal result: Renin’s increase
Hyperplasia 1-6ng/ml/hr
• In-born error in adrenal hormone biosynthesis
• Its abnormality depends on the lacking enzyme CONGENITAL ADRENAL
o 21 Hydroxylase HYPERPLASIA TREATMENT:
o 11-B Hydroxylase • Hormone replacement via Intra-
o 3-B Hydroxysteroid dehydrogenase-isomerase venous infusion on what hormones
are lacking.
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 17
ENDOCRINOLOGY REVIEW NOTES
ADRENAL MEDULLA CHROMAFFIN CELLS:
• Innermost part of the adrenal gland • Produces Catecholamine Hormones: Epinephrine,
• Composed mainly of hormone-producing Norepinephrine, and Dopamine
Pheochromocytes (chromaffin cells) • Produces Endogenous Opioids: Enkephalin
• Receives synaptic input from other neuronal cells
• Intended for more rapid responses
o Depolarize and generate action potentials in
• Extension of sympathetic nervous system response to sympathetic stimulation
• The cells of the adrenal medulla are (Acetylcholine)
modified sympathetic ganglia o Release the stored secretory material in
response to depolarization.
• Neural – Acetylcholine; Hormonal –
• High Concentrations of Epinephrine and
Epinephrine and Norepinephrine Norepinephrine are stored
• Medullary hormones are responsible for: • DBH catalyzed reactions occurs in the granules
Fight-or-Flight-or-Freeze
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 18
ENDOCRINOLOGY REVIEW NOTES
• Has a 17:3
CHROMAFFIN CELLS ANOTHER HORMONE:
Norepinephrine to
• Neuropeptide Y: Neuromodulator
Epinephrine Ratio when • Calcitonin Related Gene: Vasodilator
released in the • Chromogranin (A, B, C): Intracellular traffic
circulation. • Methionine and Leucine Enkephalin: Binds to opiate
receptors
CATECHOLAMINES
• Sympathetic Preganglionic activation
• Release of Acetylcholine
• Depolarization of chromaffin cells
• Exocytosis of all the vesicle contents
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 19
ENDOCRINOLOGY REVIEW NOTES
MEDULLA: EPINEPHRINE
• Most abundant catecholamine in the dense RELATIONSHIP OF CORTISOL AND
EPINEPHRINE
granules (80%) EPINEPHRINE CORTISOL
• Glycogenolysis and Gluconeogenesis – Increased • Immediate response • Long term effector
Glucose hormone • Increases the amount
• Lipase – Lipolysis • Modulates existing of existing enzymes
• Inhibiting the release of insulin enzymes • Increase glucose
• Increase glucose synthesis and release
• Prevents exhaustion of the pancreas in releasing synthesis and release • Increase lipolysis
insulin • Increase lipolysis • Inhibits glucose use
• Stimulates glucose use • Stimulates protein
MEDULLA: NOREPINEPHRINE breakdown
• Second most abundant catecholamine in the EFFECTS OF EPINEPHRINE AND
NOREPINEPHRINE
dense granules (15%)
HEART Increase heart rate
• Synthesized mostly in the CNS LUNGS Increase respiratory rate
• Adrenal medulla only produces 7% of the 15% Vasoconstriction and
total NE in the granules. vasodilation
SYSTEMIC
• Has the same function with Epinephrine Triggers lipolysis
Muscle contraction
• Also serves as a neurotransmitter in the CNS Stimulates
LIVER
glycogenolysis
MEDULLA: DOPAMINE
• Produced in the medulla at small amounts. High ADRENERGIC RECEPTORS
amounts of dopamine are secreted by the • Alpha-Adrenergic Receptors – A1 (vascular
and smooth muscle contraction) and A2
Hypothalamus and Basal ganglia of the brain.
(inhibits norepinephrine)
• Precursor substance of other catecholamines • Beta-Adrenergic Receptors – B1 (heart rate),
• Counteracts Norepinephrine and Epinephrine B2 (veins), B3 (lipolysis)
response after Flight and Fight response. • Dopamine Receptors – D1 (Stimulation of the
adenylyl cyclase system and Found post-
synoptically in the brain) and D2 (Inhibit the
MEDULLA DISEASE ASSOCIATION: ADRENAL
formation of cAMP, open potassium channels,
MEDULLARY HYPOFUNCTION and decrease calcium influx.)
• Causes: Removal of the adrenal gland that leads
to loss of catecholamines ADRENAL MEDULLARY HYPOFUNCTION
• Autonomic Insufficiency: Syringomyelia, Familial TREATMENT:
dysautonomia, Shy-Drager Syndrome, • Vasoconstrictive Drugs (Ephedrine,
Parkinson's Disease, Tabes dorsalis phenylephrine, metaraminol, monoamine
oxidase inhibitors, levodopa, propranolol, and
indomethacin)
• Plasma volume expanders (fludrocortisone)
• Alpha adrenergic agonist drugs (Octreotide,
midodrine)
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 20
ENDOCRINOLOGY REVIEW NOTES
MEDULLA DIASEASE ASSOCIATION: ADRENAL
MEDULLA DIASEASE ASSOCIATION:
MEDULLARY HYPERFUNCTION
ADRENAL MEDULLARY HYPERFUNCTION
SYMPTOMS: • Pheochromocytoma - tumors that arise from the
• Headache adrenal medulla.
• Sweating • This persistent hypersecretion of catecholamines
• Forceful heartbeat with or without by most pheochromocytomas is probably due to
tachycardia lack of feedback inhibition on tyrosine hydroxylase
• Anxiety or fear of impending death
• Pheochromocytoma cells ordinarily contain more
• Tremor
• Fatigue or exhaustion norepinephrine than epinephrine – inverse ratio
• Nausea and vomiting • Causes:
• Abdominal or chest pain o Multiple Endocrine Neoplasia Type 2 (MEN 2)
• Visual disturbances o Von Hippel-Lindau Disease
• Increased sweating o Von Recklinghausen's (Type 1)
• Cold hands and feet
Neurofibromatosis (NF-1)
• Weight loss
o Familial Pheochromocytomas
• Constipation
FACTORS TO CONSIDER BEFORE TESTING
MEDULLA DIASEASE ASSOCIATION:
• Food intake (Coffee, Caffeine rich foods,
LBAORATORY DIAGNOSIS - cus
Banana, Peppers) • Catecholamines and Metanephrines
• Drugs (Acetaminophen, Aldomet, Levels
Amphetamines, Bronchodilators, Ephedrine) • Serum Chromogranin A Levels
• Radio Contrast Media (meglumine acetrizoate) • Urinary Vanillylmandelic Acid (VMA)
• Diseases (Guillain-Barré Syndrome,
Hypoglycemia, Lead poisoning)
TREATMENT:
• Calcium Channel Blockers
(Nicardipine, Nifedipine)
• Adrenalectomy
• Alpha-adrenergic Blockers
(Phenoxybenzamine, Prasozine)
• Angiotensin-converting Enzyme
(Ace) Inhibitors
• Beta-adrenergic Blockers
(Propanolol, Labetalol)
• METYROSINE (Α-methylparatyrosine)
MEDICAL LABORATORY SCIENCE | CLINICAL CHEMISTRY 3 | ROMIE SOLACITO 21
Вам также может понравиться
- Clinical Laboratory Science Review by Theriot - JarreauДокумент12 страницClinical Laboratory Science Review by Theriot - JarreauJuneya Koo100% (1)
- Urinalysis and Body Fluids for Cls & MltОт EverandUrinalysis and Body Fluids for Cls & MltОценок пока нет
- Self-assessment Q&A in Clinical Laboratory Science, IIIОт EverandSelf-assessment Q&A in Clinical Laboratory Science, IIIРейтинг: 3 из 5 звезд3/5 (1)
- Clinical Chemistry Board ReviewДокумент14 страницClinical Chemistry Board ReviewWellaBaylasОценок пока нет
- Clin Path Lab 6 Urinalysis Part 2Документ7 страницClin Path Lab 6 Urinalysis Part 2api-3743217100% (3)
- Hematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeОт EverandHematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeРейтинг: 5 из 5 звезд5/5 (2)
- Must To Know in Clinical ChemistryДокумент56 страницMust To Know in Clinical ChemistryJosephine Armanne Aluyen100% (1)
- Safe Blood: Purifying the Nations Blood Supply in the Age of AОт EverandSafe Blood: Purifying the Nations Blood Supply in the Age of AОценок пока нет
- Clinical ChemistryДокумент12 страницClinical ChemistryClark Lopez100% (1)
- Quick guide to Laboratory Medicine: a student's overviewОт EverandQuick guide to Laboratory Medicine: a student's overviewОценок пока нет
- Clinical Chemistry ReviewerДокумент4 страницыClinical Chemistry ReviewerJudith Dayag Dorado100% (1)
- Microbiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeОт EverandMicrobiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeОценок пока нет
- Clinical ChemistryДокумент26 страницClinical Chemistryazoooz502Оценок пока нет
- Clinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeОт EverandClinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeРейтинг: 5 из 5 звезд5/5 (1)
- Hematology Ii Lectures Introduction To HemostasisДокумент28 страницHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Clinical Chemistry NotesДокумент24 страницыClinical Chemistry Notesclower112100% (3)
- Multiple Choice Questions for Haematology and Core Medical TraineesОт EverandMultiple Choice Questions for Haematology and Core Medical TraineesОценок пока нет
- Transfusion Medicine and Hemostasis: Clinical and Laboratory AspectsОт EverandTransfusion Medicine and Hemostasis: Clinical and Laboratory AspectsРейтинг: 4 из 5 звезд4/5 (9)
- Accurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionОт EverandAccurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionРейтинг: 5 из 5 звезд5/5 (1)
- Practical Manual for Detection of Parasites in Feces, Blood and Urine SamplesОт EverandPractical Manual for Detection of Parasites in Feces, Blood and Urine SamplesОценок пока нет
- CLINICAL MICROSCOPY (Urinalysis)Документ131 страницаCLINICAL MICROSCOPY (Urinalysis)Roderick95% (19)
- Hematology ReviewДокумент4 страницыHematology ReviewAlfred ChowОценок пока нет
- Clinical Chemistry Notes - ABIДокумент32 страницыClinical Chemistry Notes - ABIAnya Ignacio100% (1)
- Medical Laboratory Technician: Passbooks Study GuideОт EverandMedical Laboratory Technician: Passbooks Study GuideОценок пока нет
- Review in Clinical MicrosДокумент103 страницыReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Clinical Chemistry Notes - AbiДокумент34 страницыClinical Chemistry Notes - AbiAnya Ignacio100% (1)
- The Kidney: Morphology, Biochemistry, PhysiologyОт EverandThe Kidney: Morphology, Biochemistry, PhysiologyCharles RouillerОценок пока нет
- Clinical Chemistry KeyNotes For Board ExaminationДокумент12 страницClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Urinalysis and Body Fluids Q & AДокумент79 страницUrinalysis and Body Fluids Q & ADarla YsavelОценок пока нет
- Intro To Medtech Clinical Chemistry ReviewerДокумент11 страницIntro To Medtech Clinical Chemistry Reviewerjesanndei100% (1)
- Handbook of Transfusion MedicineОт EverandHandbook of Transfusion MedicineChristopher HillyerРейтинг: 4 из 5 звезд4/5 (4)
- Clinical Chemistry ReviewДокумент6 страницClinical Chemistry Reviewclower112100% (1)
- Must Know (Complete)Документ304 страницыMust Know (Complete)tev26Оценок пока нет
- Hematology - Steininger ReviewДокумент30 страницHematology - Steininger ReviewIssa AlejoОценок пока нет
- Chapter 1: An Overview of Clinical LaboratoryДокумент13 страницChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- CHEM 2 CH 29 Review QuestionsДокумент2 страницыCHEM 2 CH 29 Review QuestionsthrowawyОценок пока нет
- Clinical Microscopy ExamДокумент3 страницыClinical Microscopy ExamKarla GiorlaОценок пока нет
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4От EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4Оценок пока нет
- Transfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeОт EverandTransfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeРейтинг: 3 из 5 звезд3/5 (1)
- Haematology Case Studies with Blood Cell Morphology and PathophysiologyОт EverandHaematology Case Studies with Blood Cell Morphology and PathophysiologyРейтинг: 5 из 5 звезд5/5 (4)
- Clinical ChemistryДокумент8 страницClinical Chemistryleizej29Оценок пока нет
- MUST To KNOW in Immunohematology Blood BankingДокумент18 страницMUST To KNOW in Immunohematology Blood BankingDanielJeremy DelaCruz Paragas79% (14)
- Blood Bank Harmening Chapter 10Документ14 страницBlood Bank Harmening Chapter 10ichummy19100% (3)
- Biotin and Other Interferences in Immunoassays: A Concise GuideОт EverandBiotin and Other Interferences in Immunoassays: A Concise GuideОценок пока нет
- Hematology in Practice, 2nd EditionДокумент385 страницHematology in Practice, 2nd Editionjaviergmar84% (19)
- Beginings of MTДокумент65 страницBeginings of MTMel JamitoОценок пока нет
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsОт EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsОценок пока нет
- Strasinger Q&A BLANKДокумент68 страницStrasinger Q&A BLANKJayniel MollenoОценок пока нет
- EndocrinologyДокумент12 страницEndocrinologyNathaniel Derige AndesОценок пока нет
- 68th AACC Annual Scientific Meeting Abstract eBookОт Everand68th AACC Annual Scientific Meeting Abstract eBookОценок пока нет
- Urine CrystalsДокумент4 страницыUrine CrystalsRomie SolacitoОценок пока нет
- Hematoxylin and Eosin ProcedureДокумент1 страницаHematoxylin and Eosin ProcedureRomie SolacitoОценок пока нет
- Clinical Hematology Case StudyДокумент6 страницClinical Hematology Case StudyRomie SolacitoОценок пока нет
- CPG GoutДокумент2 страницыCPG GoutRomie SolacitoОценок пока нет
- Introduction To ParasitologyДокумент2 страницыIntroduction To ParasitologyRomie SolacitoОценок пока нет
- Immuno-Serology & Blood Banking Case Study: Systemic Lupus ErythematosusДокумент6 страницImmuno-Serology & Blood Banking Case Study: Systemic Lupus ErythematosusRomie SolacitoОценок пока нет
- Immuno-Serology & Blood Banking Case StudyДокумент8 страницImmuno-Serology & Blood Banking Case StudyRomie SolacitoОценок пока нет
- Edical Aboratory Cience: Prelim Defense Sheet - Anti-Streptolysin OДокумент1 страницаEdical Aboratory Cience: Prelim Defense Sheet - Anti-Streptolysin ORomie SolacitoОценок пока нет
- Copper Deficiency Anemia and Neutropenia Due To Ketogenic DietДокумент11 страницCopper Deficiency Anemia and Neutropenia Due To Ketogenic DietRomie SolacitoОценок пока нет
- Microbiology Case Study: Cryptococcal MeningitisДокумент16 страницMicrobiology Case Study: Cryptococcal MeningitisRomie SolacitoОценок пока нет
- Immuno-Serology: Antistreptolysin 0Документ13 страницImmuno-Serology: Antistreptolysin 0Romie SolacitoОценок пока нет
- SPMC - Microbiology Case StudyДокумент9 страницSPMC - Microbiology Case StudyRomie SolacitoОценок пока нет
- AUBF - MidtermsДокумент14 страницAUBF - MidtermsRomie Solacito100% (1)
- Basic Pharmacology - Medical TechnologyДокумент4 страницыBasic Pharmacology - Medical TechnologyRomie SolacitoОценок пока нет
- Cytogenetics: Preliminaries: Mccarty Shows That Dna Can Transform BacteriaДокумент5 страницCytogenetics: Preliminaries: Mccarty Shows That Dna Can Transform BacteriaRomie SolacitoОценок пока нет
- Hematology: RBC Thalassemia: Chromosome 16: Alpha Gene and Zeta Gene Chromosome 11: Beta Gene, Delta Gene, GammaДокумент3 страницыHematology: RBC Thalassemia: Chromosome 16: Alpha Gene and Zeta Gene Chromosome 11: Beta Gene, Delta Gene, GammaRomie SolacitoОценок пока нет
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CДокумент12 страницImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- Aub F Urine Screening For Metabolic DisordersДокумент4 страницыAub F Urine Screening For Metabolic DisordersRomie SolacitoОценок пока нет
- MUST To KNOW in BacteriologyДокумент35 страницMUST To KNOW in BacteriologyJohn TamayoОценок пока нет
- Hematology PreliminariesДокумент7 страницHematology PreliminariesRomie SolacitoОценок пока нет
- Blood Banking: RH Blood Group SystemДокумент2 страницыBlood Banking: RH Blood Group SystemRomie Solacito100% (1)
- Immunology & Serology Week 1Документ2 страницыImmunology & Serology Week 1Romie SolacitoОценок пока нет
- Thyroid Panel MLS4C PDFДокумент111 страницThyroid Panel MLS4C PDFRomie SolacitoОценок пока нет
- Histopathologic TechniquesДокумент22 страницыHistopathologic TechniquesRomie SolacitoОценок пока нет
- HISTOPATHOLOGY: Diagnostic CytologyДокумент14 страницHISTOPATHOLOGY: Diagnostic CytologyRomie SolacitoОценок пока нет
- Clinical Chemistry 2Документ6 страницClinical Chemistry 2Romie SolacitoОценок пока нет
- Eaching THE GE OF DolescenceДокумент14 страницEaching THE GE OF DolescenceSundeep GargОценок пока нет
- AP-2 Lab Report - Lab 01 The Endrocine SystemДокумент15 страницAP-2 Lab Report - Lab 01 The Endrocine Systemrcdunfee86% (7)
- Egyankosh..Unit 2..influencing FactorsДокумент9 страницEgyankosh..Unit 2..influencing FactorsAnshita SharmaОценок пока нет
- Chapter One A CellДокумент46 страницChapter One A CellLeon MarkoОценок пока нет
- Hormonal Response To ExerciseДокумент44 страницыHormonal Response To ExerciseMuhammad shayan umarОценок пока нет
- Chapter Notes - Control and Coordination - Class 10 Science - PANTOMATHДокумент16 страницChapter Notes - Control and Coordination - Class 10 Science - PANTOMATHsourav9823Оценок пока нет
- Chapter 34 The Endocrine SystemДокумент39 страницChapter 34 The Endocrine Systemtheia28Оценок пока нет
- Asm 2380Документ2 страницыAsm 2380Aryaan LaskarОценок пока нет
- Chemical Coordination and ControlДокумент18 страницChemical Coordination and ControlGovind RajputОценок пока нет
- Hillson Thyroid DisordersДокумент90 страницHillson Thyroid DisordersGirish SubashОценок пока нет
- Control of Hormone SecretionДокумент77 страницControl of Hormone Secretionjohanna deguzmanОценок пока нет
- Endocrine System Anatomy and PhysiologyДокумент17 страницEndocrine System Anatomy and PhysiologyKBD0% (1)
- Endocrinology Module Study Guide 2023 FinalДокумент24 страницыEndocrinology Module Study Guide 2023 Finaldomitam105Оценок пока нет
- CAMBRIDGE IGCSE BIOLOGY Chapter 14 Coordination and ResponseДокумент203 страницыCAMBRIDGE IGCSE BIOLOGY Chapter 14 Coordination and ResponseVentus Tan100% (1)
- Endocrine System - Part 2Документ31 страницаEndocrine System - Part 2Maryem NabawiОценок пока нет
- Answer Sheet Week 7Документ6 страницAnswer Sheet Week 7kathleenjaneОценок пока нет
- VisibleBody Endocrine SystemДокумент15 страницVisibleBody Endocrine Systemcascavelette0% (1)
- Journal of Endocrine DisordersДокумент9 страницJournal of Endocrine DisordersAustin Publishing GroupОценок пока нет
- Notes Chapter 7Документ16 страницNotes Chapter 7KxelviiОценок пока нет
- Endocrine Histology NotesДокумент5 страницEndocrine Histology NotesJulie TranОценок пока нет
- EndocrinologyДокумент46 страницEndocrinology[161]Shuaib AktherОценок пока нет
- Elective 1 Outline ReviewerДокумент18 страницElective 1 Outline ReviewerAna Rosemarie Rafinian EnaoОценок пока нет
- 202 Multiple Choice QuestionsДокумент5 страниц202 Multiple Choice QuestionsFawad TunioОценок пока нет
- Anph111 FinalsДокумент50 страницAnph111 FinalsxeanОценок пока нет
- TLE Hilot Wellness Massage G 10 Module 3 HWM Lesson1 Identify Information of Client 3Документ30 страницTLE Hilot Wellness Massage G 10 Module 3 HWM Lesson1 Identify Information of Client 3Fatima BatasОценок пока нет
- Integrated ScienceДокумент10 страницIntegrated ScienceFaadiyaОценок пока нет
- EndocrinologyДокумент10 страницEndocrinologyJohn Daniel AriasОценок пока нет
- Endo Crinal Voice Disorders - PDF /KUNNAMPALLIL GEJOДокумент90 страницEndo Crinal Voice Disorders - PDF /KUNNAMPALLIL GEJOKUNNAMPALLIL GEJO JOHNОценок пока нет
- Biology: Edexcel International Gcse (9 - 1)Документ10 страницBiology: Edexcel International Gcse (9 - 1)Shibraj DebОценок пока нет
- Psychology (Psy10) PowerpointДокумент134 страницыPsychology (Psy10) PowerpointEdin AbolenciaОценок пока нет