Академический Документы
Профессиональный Документы
Культура Документы
hpv162 PDF
Загружено:
Laura PutriОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
hpv162 PDF
Загружено:
Laura PutriАвторское право:
Доступные форматы
Original Article
Postdialysis Hypertension: Associated Factors, Patient
Profiles, and Cardiovascular Mortality
Attilio Losito,1 Lucia Del Vecchio,2 Goffredo Del Rosso,3 and Francesco Locatelli2
BACKGROUND AND OBJECTIVES dialysis vintage, be male, have lower SBP, lower changes in weight
A postdialytic increase in blood pressure (BP) is a recognized but often during HD, and receive more antihypertensive medications. These
an overlooked complication. The epidemiology and predisposing predictive factors were shown to be associated with an interaction
factors are still not well defined. We studied a large sample of Italian between weight loss and dialysis, suggesting a volume-related
dialysis patients to assess the prevalence of postdialysis hypertension mechanism in its pathogenesis. PDHYPER was also associated with
(PDHYPER), defined as any increase of systolic BP (SBP) >10 mm, Hg CV mortality.
above the predialysis value, the associated factors and its role in cardio-
vascular (CV) mortality. CONCLUSIONS
In our study on a large Italian cohort of dialysis patients, the preva-
PATIENTS AND METHODS lence of PDHYPER was higher than what was previously reported
In this observational study, we assessed dialysis associated changes in and is a significant risk factor for CV mortality in dialysis patients.
BP in 4,292 hemodialysis (HD) patients over 1 month (51,504 sessions). The pathogenesis is multifactorial but hypertensive state, antihyper-
We compared the clinical characteristics of the patients with stable tensive medications, and extracellular volume expansion appear to
BP values during the HD session with those with PDHYPER. We also play a major role.
assessed the impact of PDHYPER on CV mortality.
Keywords: blood pressure; hemodialysis; hypertension; postdialysis
RESULTS hypertension; volume expansion.
A total of 994 (23.1%) patients had PDHYPER. Patients with
PDHYPER were more likely to be hypertesive, older, have a shorter doi:10.1093/ajh/hpv162
An increase in blood pressure (BP) during hemodialysis (HD), This represents a potential bias since, in general, a single
although recognized for many years, is often overlooked.1 center has a homogeneous policy on the dialytic and medi-
There is also a lack of a unifying criteria for the diagnosis of cal management of patients. A step forward toward its better
postdialytic hypertension (PDHYPER), although an increase understanding can help reduce the high rate of cardiovascu-
in systolic BP (SBP) >10 mm Hg from pre- to postdialysis has lar (CV) morbidity occurring in HD patients.6
been proposed and is widely used.2 There is also a scarcity The aim of this large, multicenter, observational study is to
of systematic studies on its prevalence and consequences.3 investigate HD- and patient-related factors associated with
Research on the mechanisms causing PDHYPER has been PDHYPER and its impact on mortality.
addressed to both the HD treatment and patient character-
istics. The results obtained are often conflicting. Among the
possible pathogenetic mechanisms, ultrafiltration-induced PATIENTS AND METHODS
hypovolemia may trigger the renin–angiotensin system and Study design
induce vasoconstriction, which is mediated by an increase
in blood viscosity/hemoconcentration favored by higher The study is a retrospective analysis of data collected for a
hemoglobin (Hb) levels and/or treatment with erythropoiesis previous prospective study.7,8 In brief, patients were assessed
stimulating agents.4 The removal of antihypertensive drugs by at enrollment and were followed thereafter. CV mortality
dialysis is another possible cause of intradialytic hypertension. was drawn from death certificate and reported by participat-
Finally, electrolyte disequilibrium, sympathetic over activity, ing centers. The information requested from participating
and endothelial cell dysfunction may play a role.5 units on the cause of death were: death due to cerebrovascu-
Unfortunately, the majority of the available studies con- lar disease, ischemic or hemorrhagic, death due to any CV
sidered 1 single hypothetical factor at a time or were per- condition, comprising ischemic heart disease, heart failure,
formed on a small number of patients from a single center. and sudden death.
1Renal Unit, Ospedale Santa Maria Della Misericordia, Perugia, Italy;
Correspondence: Attilio Losito (atlosito@tin.it).
2Renal Unit, Ospedale Manzoni, Lecco, Italy; 3Renal Unit, Ospedale
Initially submitted June 27, 2015; date of first revision August 4, Mazzini, Teramo, Italy.
2015; accepted for publication August 30, 2015; online publication
© American Journal of Hypertension, Ltd 2015. All rights reserved.
September 21, 2015.
For Permissions, please email: journals.permissions@oup.com
684 American Journal of Hypertension 29(6) June 2016
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Postdialytic Hypertension and Cardiovascular Mortality
Patients’ characteristics presented as proportions and compared by Pearson’s χ2.
Means were compared by the analysis of variance with
All adult patients (≥18 years old), in 77 HD centers across Dunnett’s post hoc test. To detect the predictors of postdi-
Italy, receiving HD thrice weekly for at least 3 months were alysis changes in SBP, we performed a multiple regression
considered for inclusion. Patients with body weights less analysis with Δ SBP as the continuous dependent variable.
than 35 kg, cachexia due to malignancies, severe malnutri- Logistic regression analysis was used to detect factors associ-
tion or with known severe heart disease (New York Heart ated with PDHYPER as a dichotomous dependent variable.
Association (NYHA) class III or IV) were excluded. The The analysis was also carried out using different thresholds
diagnosis of heart failure, assigned to consultant cardiolo- for PDHYPER: 5 and 15 mm Hg. An unadjusted model
gists of the participating centers, was based mainly on clinical was built only with the variables that were significant to the
grounds or on the finding of left ventricular ejection fraction model. The adjusted model also included nonsignificant
<50% at transthoracic echocardiography. Along with BP, the variables. Both models were evaluated for goodness of fit
following data were recorded: age, sex, smoking and alco- by the Hosmer and Lemeshow test and by the area under
hol intake history, serum cholesterol, body mass index, and the receiver-operating characteristic curve. On the basis of
a history of diabetes serum albumin, Hb, parathyroid hor- the results of the logistic regression analysis, we investigated
mone. Recorded parameters concerning dialysis treatment biological interaction, as defined by Rothman, among pre-
were: length of session and dialysis modality, Kt/V as meas- dialysis SBP, Δ weight during HD and the use of antihyper-
ured with 2-point Daugirdas formula, Δ body weight during tensive medications.11 We calculated the relative excess risk
HD (as a proxy of ultrafiltration). Due to the frequent modi- because of interaction (RERI) by using the methods outlined
fications in antihypertensive treatment in dialysis patients, by Andersson et al.12 In the absence of a biological interac-
we asked the participating centers to maintain the therapy tion, the RERI is 0. Logistic regression was repeated after
stable during the 12 dialysis period and to provide informa- stratification by tertiles of weight loss due to dialysis.
tion about antihypertensive medication (yes/no). The type
and dose of erythropoiesis stimulating agent were also col-
lected. HD modality was divided into 2 categories according Survival analysis
to the use of convective techniques.
The association between Δ SBP and mortality was assessed
by the Cox proportional hazard model. Models were built
Blood pressure measurement with the following covariates: age, sex, dialysis vintage, pres-
ence of diabetes, CHOL, body mass index, albumin, Hb, par-
In every dialysis unit, BP was measured by trained nurses athyroid hormone, Kt/V, Δ weight, and predialysis SBP. The
according to National Kidney Foundation Outcomes Quality proportional hazards assumption of the models was assessed
Initiative (KDOQI) guidelines.9 The nursing staff was spe- using the Shoenfeld residuals. In the analysis, the etiology of
cifically instructed accordingly. Predialysis BP was measured kidney disease was tested for its association with PHYPER
after the patient had been sitting for at least 5 minutes before and mortality.
the needles for dialysis access were placed. Postdialysis BP All tests were performed by Stata 11 statistical package
was measured at least 5 minutes after the end of the proce- (Stata, College Station, TX).
dure for 12 consecutive sessions. Likewise, predialysis and
postdialysis pulse pressures were calculated from the meas-
ured BP; heart rate (HR) was also recorded. RESULTS
For the analysis, we used the mean of BP changes in 12
At the baseline, we obtained data from 4,292 dialysis
consecutive HD sessions. A change (Δ) in SBP was defined as
patients (>99% Caucasian) for a total of 51,504 dialysis ses-
postdialysis minus predialysis SBP. On the basis of published
sions; 2,353 patients were assessed for the presence of heart
evidence, showing an increase was associated with a number
failure that was detected in 557 subjects (23.6%). The main
of complications and with mortality, we defined PDHYPER
characteristics of the whole cohort and those of patients
as being an increase in SBP during HD greater than 10 mm
grouped according to SBP changes with dialysis are pre-
Hg above the predialysis BP measurement.2 According to
sented in Table 1. A mean postdialysis SBP increase >10 mm
current guidelines, postdialysis hypotension (PDHYPO) is
Hg (PDHYPER) was detected in 994 (23.1%) patients,
defined as a decrease of SBP greater than 20 mm Hg below
among them 73.5% had a diagnosis of hypertension. In
the predialysis value.10
patients with a predialysis SBP <140 mm Hg, the prevalence
For the analysis, we divided the patients into 3 groups
was 28.7%, in those with a predialysis SBP >140 mm Hg the
according to SBP changes during HD: group 1: Δ SBP
prevalence was 15.4% (P < 0.001, relative risk 0.537).
between −20 and + 10 mm Hg, group 2: Δ SBP > +10 mm
Multivariable regression analysis with dialytic Δ SBP as a
Hg, group 3: Δ SBP > −20 mm Hg. Patients with heart failure
continuous dependent variable produced a significant model
were examined separately.
(adjusted R2 = 0.212, F = 74.1, Prob > F = 0.0001) (Table 2).
Statistical analysis Postdialysis hypertension
Continuous variables are presented as means and Compared to patients with no changes in BP (group
SDs unless otherwise specified. Categorical variables are 1), those with PDHYPER (group 2) were more likely to
American Journal of Hypertension 29(6) June 2016 685
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Losito et al.
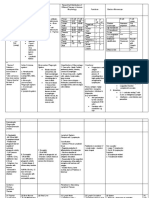
Table 1. Characteristics of the cohort
Variable Whole cohort Controls PDHYPO PDHYPER
Number 4,292 2,580 718 994
Age (years, mean ± SD) 65.1 ± 18.9 64.1 ± 19.6 65.3 ± 17.2 70.2 ± 13.3*
Male sex (%) 62.0 62.6 55.8* 64.2
Dry weight (kg, mean ± SD) 65.9 ± 16.4 66.0 ± 17.8 67.6 ± 14.1 64.0 ± 12.9
Delta weight with dialysis (kg, mean ± SD) 2.55 ± 0.88 2.56 ± 0.86 2.88 ± 0.84* 2.29 ± 0.93*
Body mass index (kg/m2) 24.2 ± 4.3 24.2 ± 4.3 25.2 ± 4.8* 23.4 ± 3.9*
Dialytic vintage (months, mean ± SD) 67.5 ± 74.9 61.2 ± 81.8 64.6 ± 68.4 57.2 ± 63.2*
Dialysis session time (min, mean ± SD) 231.7 ± 20.0 230.9 ± 20.5 234.7 ± 18.5* 231.1 ± 19.0
Single pool Kt/V 1.31 ± 0.26 1.31 ± 0.26 1.33 ± 0.26* 1.31 ± 0.23
Hemoglobin (g/dl, mean ± SD) 11.4 ± 1.2 11.4 ± 1.2 11.6 ± 1.3 11.3 ± 1.27
Albumin (g/dl, mean ± SD) 3.82 ± 0.48 3.82 ± 0.48 3.84 ± 0.46 3.79 ± 0.49
Cholesterol (mg/dl, mean ± SD) 164.2 ± 41.2 164.1 ± 41.1 167.9 ± 41.1 164.2 ± 42.3
PTH (pg/ml, mean ± SD) 291.2 ± 285.9 292.6 ± 287.6 337.6 ± 334.8* 255.7 ± 288.2*
Convective HD (%) 24.9 25.4 26.7 22.9
Predialysis SBP (mm Hg, mean ± SD) 136.3 ± 20.6 134.2 ± 20.2 149.7 ± 19.1* 130.7 ± 18.4*
Predialysis PP (mm Hg, mean ± SD) 63.9 ± 18.2 61.2 ± 15.8 75.9 ± 24.6* 61.8 ± 15.6
Predialysis heart rate (b/min, mean ± SD) 73.1 ± 10.2 73.5 ± 9.8 74.6 ± 10.1 71.2 ± 10.5*
Postdialysis heart rate (b/min, mean ± SD) 74.3 ± 11.3 74.5 ± 11.0 76.1 ± 11.6 72.3 ± 11.6*
Diabetes (%) 19.4 18.2 25.5* 17.7
ESA (%) 90.4 90.2 89.8 91.8
Antihypertensive medications (%) 56.5 54.9 59.0 65.7*
Heart failure (%) 23.6 24.6 29.1* 22.1
Control, group 1: Δ SBP between −20 and + 10 mm Hg, group 2: Δ SBP > −20 mm Hg, group 3: Δ SBP > +10 mm Hg.
Abbreviations: SBP, systolic blood pressure; HD, hemodialysis; PP, pulse pressure; PTH, parathyroid hormone; ESA, erythropoiesis stimulat-
ing agent; PDHYPO, postdialysis hypotension; PDHYPER, postdialysis hypertension.
*P < 0.05 in the comparison with group 1.
Table 2. Multivariable regression model results for Δ SBP (mm Hg) in dialysis patients
Δ SBP (mm Hg)
Variable Coefficient SE P Overall adjusted R2
Δ Weight (kg) −3.798 0.378 <0.0001 0.2067
Predialysis SBP (mm Hg) −0.336 0.019 <0.001
Predialysis PP (mm Hg) 0.098 0.025 <0.001
Predialysis HR (b/min) −0.096 0.044 0.002
Postdialysis HR (b/min) −0.121 0.040 0.002
Hb (g/dl) −0.813 0.243 0.001
BMI (kg/m2) −0.310 0.071 <0.001
Dialytic vintage (months) −0.010 0.004 0.011
Abbreviations: SBP, systolic blood pressure; PP, pulse pressure; HR, heart rate; Hb, hemoglobin; BMI, body mass index.
be older, have a shorter dialysis vintage, lower body mass analysis, using PDHYPER as a dichotomous depend-
index, lower Δ weight during HD, lower Hb, lower para- ent variable, produced 2 significant models (1 adjusted
thyroid hormone, lower predialysis SBP, and heart rate. and 1 unadjusted) (Table 3). For the unadjusted model,
Furthermore, the proportion of patients on antihyperten- the area under the receiver-operating characteristic curve
sive medications was higher, as well as the percentage of was = 0.729, correctly classified as 85.34%. The Hosmer
patients with an ejection fraction <50%. Logistic regression and Lemeshow χ2 was 4.91 with probabilities > χ2 =0.767.
686 American Journal of Hypertension 29(6) June 2016
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Postdialytic Hypertension and Cardiovascular Mortality
Table 3. Unadjusted and adjusted odds ratios for postdialysis hypertension
Unadjusted Adjusted
Predictor OR 95% CI P OR 95% CI P
Age 1.02 1.01–1.03 <0.001 1.02 1.01–1.03 0.030
Male sex 1.36 1.04–1.78 0.024 1.33 0.99–1.78 0.058
Dialysis session time 1.01 1.00–1.02 <0.001 1.01 0.99–1.02 0.065
Δ Weight with dialysis 0.57 0.49–0.68 <0.001 0.59 0.49–0.70 <0.001
Predialysis SBP 0.96 0.95–0.97 <0.001 0.96 0.95–0.97 <0.001
Predialysis PP 1.02 1.01–1.03 0.003 1.02 1.01–1.03 0.002
Predialysis HR 0.98 0.96–0.99 0.030 0.98 0.96–0.99 0.002
ESA 0.58 0.37–0.91 0.019 0.55 0.35–0.87 0.010
Antihypertensive medications 2.35 1.76–3.14 <0.001 1.57 1.01–2.43 0.044
Body mass index 0.98 0.94–1.01 0.233
Diabetes 0.90 0.63–1.28 0.573
Single pool Kt/V 1.09 0.65–1.81 0.741
Hemoglobin 0.94 0.87–1.02 0.133
Albumin 0.99 0.99–1.01 0.934
Cholesterol 1.00 0.99–1.00 0.843
PTH 0.99 0.99–1.00 0.338
Convective HD 1.97 0.70–1.34 0.858
Abbreviations: CI, confidence interval; ESA, erythropoiesis stimulating agent; SBP, systolic blood pressure; PP, pulse pressure; HR, heart
rate; HD, hemodialysis; PTH, parathyroid hormone.
For the adjusted model, the area under receiver-operating antihypertensive medications (RERI −1.793, CI −2.572 to
characteristic curve was = 0.732, correctly classified 85.53%. 1.015). These values indicate interaction on an additive scale,
The Hosmer and Lemeshow χ2 was 5.50, with probabilities meaning that the combined effect is less than the sum of the
>χ2 = 0.702. The tests indicated a good discrimination for factors examined singly.
both models. The use of antihypertensive medications, male
sex, increased predialysis pulse pressures, increased age, and Patients with heart failure
longer length of the HD session were significant predictors
of PDHYPER. Conversely, Δ weight during HD, erythro- The logistic regression performed in patients with heart
poiesis stimulating agent use, predialysis SBP, and predialy- failure showed the following predictors of PDHYPER: pre-
sis HR were predictors, inversely associated, of postdialysis dialysis SBP (OR 1.25, CI 1.17–1.34; P < 0.001), female sex
hypertension. Diabetes and heart failure were found not to (0.17, CI = 0.05–0.63; P = 0.008).
be predictors. The analysis, repeated after stratification by
tertiles of weight loss by dialysis, showed that the follow- Survival and changes in BP with dialysis
ing variables were significantly predictive: use of antihyper-
tensive medications, predialysis SBP, and predialysis pulse Patients were followed up for a mean of 26.8 ± 11.1 months;
pressures. Logistic regression was also carried out with 2 348 patients who were lost to follow-up were either trans-
different thresholds for PDHYPER (5 and 15 mm Hg). With planted or transferred to different units. On the basis of the
the 5 mm Hg threshold, found in 28.7% of the patients, the results of the above logistic regression, we excluded from
results were concordant with those obtained with the 10 mm the analysis subjects with heart failure. We had data for CV
Hg threshold. Raising the threshold to 15 mm Hg, 10.5% of mortality in the remaining 3,196 patients, among whom
the patients presented PDHYPER. In the analysis, only age, 420 deaths were recorded. Of those, 318 were ascribed to
Δ weight, and heart rate were significant predictors. a heart disease and 102 to a cerebrovascular event. The
Cox analysis produced a significant model with the fol-
Interaction between factors lowing predictors of CV mortality: age (HR 1.05, CI 1.03–
1.07; P < 0.001), dialysis vintage (HR 1.01, CI 1.00–1.02;
We found a significant interaction between predialysis P = 0.038), PDHYPER (HR 1.69, CI 1.12–2.57; P = 0.012)
SBP and Δ weight during HD (RERI −2.830, confidence (Figure 1). Predialysis SBP (> or <140 mm Hg) was not a
interval (CI) −3.088 to 2.573), between Δ weight during HD predictor of mortality. Apart from hypertension, no other
and the use of antihypertensive medications (RERI −1.881, association was found between the etiology of kidney dis-
CI −2.631 to 1.131) and between predialysis SBP and use of ease and PHYPER or mortality.
American Journal of Hypertension 29(6) June 2016 687
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Losito et al.
Figure 1. Cox analysis in patients without heart failure. CV mortality plot. Controls are patients with a postdialysis SBP Δ comprised between −20 and
+ 10 mm Hg, PDHYPER: Δ SBP > +10 mm Hg, PDHYPO: Δ SBP > −20 mm Hg. Only PDHYPER shows a significant difference from controls. Abbreviations:
PDHYPO, postdialysis hypotension; PDHYPER, postdialysis hypertension.
DISCUSSION body compartment, especially in patients with a low pre-
dialysis plasma sodium concentration (as is often the case
PDHYPER is generally perceived as an uncommon com- in patients with low sodium intake). The consequence of a
plication of dialytic treatment.13,14 In different surveys, adopt- positive sodium balance at the end of the dialytic session is
ing the same criteria as the present study, the occurrence of an increase in extracellular fluid volume that may be over-
an increase in BP from pre- to postdialysis was found in less looked.15 The end of the process is a positive sodium balance
than 15% of maintenance HD patients.4 In our large sample with consequent hypertension requiring ever more antihy-
of Italian dialysis patients, we showed that PDHYPER is a pertensive medications. A longer duration of the dialysis ses-
relatively common phenomenon, occurring in nearly 1 of 4 sion, which is associated with postdialysis hypertension, may
patients. We also found that the main factors influencing SBP increase drug removal and give more time for the diffusive
changes during HD were a hypertensive state, predialysis SBP transport of sodium from the dialysate to the plasma and,
and pulse pressures, pre- and postdialysis HR, Δ weight during thus, a more positive sodium balance. Unfortunately, we did
HD, Hb, dialytic vintage, and body mass index. not collect information regarding sodium concentrations in
We have also found that, in patients without heart failure, plasma and in dialysate to better support this hypothesis.
PDHYPER is a significant predictor of CV mortality. The Nevertheless, this interpretation is in line with data from
mechanism leading to PDHYPER is not so straightforward. small cohorts of dialysis patients16 and experimental studies
The interaction between the use of antihypertensive medi- aimed at investigate specific mechanisms of PDHYPER.17 In
cations and Δ weight during HD may suggest an increased a post hoc analysis of the Dry-weight reduction in hyperten-
need for medications in patients with inadequate intradia- sive hemodialysis patients (DRIP) trial, the authors meas-
lytic weight loss compared to their dry weight. Medications ured the slopes of intradialytic BP during dialysis and tested
explain lower predialysis SBP and their removal with dialy- the effect of dry-weight reduction on these slopes and found
sis is a reasonable cause of PDHYPER. Furthermore, these that intradialytic BP changes were associated with changes in
patients are more likely to have a shorter dialysis vintage dry body weight.18 These results suggested that PDHYPER is
and thus residual diuresis and/or adherence to a low sodium a marker of volume excess. Recently, Nongnuch et al. sub-
diet. This setting may lead to a reduced sodium pool, as testi- mitted 531 dialysis patients to multiple-frequency bioelectri-
fied by lower predialysis SBP. A lower Δ weight during HD cal impedance and found that the ratio of extracellular water
may lead to reduced convective loss of sodium when using to total body water was significantly higher in the patients
a standard dialysate with a sodium concentration of 139 with PDHYPER.19
mEq/l. This may allow a diffusive flux of sodium toward the
688 American Journal of Hypertension 29(6) June 2016
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Postdialytic Hypertension and Cardiovascular Mortality
The prevalence of heart failure in dialysis patients is high 3. Chou KJ, Lee PT, Chen CL, Chiou CW, Hsu CY, Chung HM, Liu CP,
and the prognosis is ominous, especially in the presence of Fang HC. Physiological changes during hemodialysis in patients with
intradialysis hypertension. Kidney Int 2006; 69:1833–1838.
hypertension.20In patients with heart failure in our study, the 4. Inrig JK. Intradialytic hypertension: a less-recognized cardiovascular
factors associated with PDHYPER were not the same as the complication of hemodialysis. Am J Kidney Dis 2010; 55:580–589.
ones we found in the others. Interestingly, Δ weight was not a 5. Inrig JK, Van Buren P, Kim C, Vongpatanasin W, Povsic TJ, Toto RD.
predictor, indicating a more complex mechanism operating Intradialytic hypertension and its association with endothelial cell dys-
function. Clin J Am Soc Nephrol 2011; 6:2016–2024.
in this subset of patients. Predialysis SBP was a more sig- 6. Chazot C, Jean G. Intradialytic hypertension: it is time to act. Nephron
nificant predictor. These findings show that factors associ- Clin Pract 2010; 115:c182–c188.
ated with changes in BP during dialysis vary according to the 7. Del Vecchio L, Lusenti T, Del Rosso G, Malandra R, Balducci A,
individual characteristics of patients. Losito A; Group For Arterial Hypertension of the Italian Society Of
Our study has a number of limitations. We did not per- Nephrology. Prevalence of hypertension in a large cohort of Italian
hemodialysis patients: results of a cross-sectional study. J Nephrol 2013;
form a direct examination of extracellular volume.21 Thus, 26:745–754.
we can give only indirect evidence about the causative effect 8. Losito A, Del Vecchio L, Lusenti T, Del Rosso G, Malandra R, Sturani
of volume expansion on PDHYPER and we cannot rule out A; Gruppo di Studio Dell’Ipertensione Arteriosa Società Italiana
other contributing factors, such as dialysate sodium concen- Nefrologia. Systolic blood pressure and mortality in chronic hemodi-
alysis patients: results of a nationwide Italian study. J Clin Hypertens
tration, renin–angiotensin–aldosterone system, and sympa- (Greenwich) 2013; 15:328–332.
thetic activation. We did not collect information on the class 9. K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardio-
and number of antihypertensive medications. Thus, we can vascular disease in dialysis patients. Am J Kidney Dis 2005; 45(Suppl
just speculate around medication removal by dialysis. On 3):S1–S153.
the other hand, the large number of enrolled patients and 10. K/DOQI Clinical Practice Guidelines for Cardiovascular Disease in
Dialysis Patients. Intradialytic hypotension. Am J Kidney Dis 2005;
collected variables, together with the homogeneity of the 45(Suppl 3):S76–S80.
population, strengthen the validity of the results obtained. 11. Rothman, KJ: Measuring interactions. Epidemiology: An Introduction.
In conclusion, our multicenter study shows that the preva- Oxford University Press: New York, 2002, pp. 168–180.
lence of PDHYPER is higher than that previously reported 12. Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A.
Calculating measures of biological interaction. Eur J Epidemiol 2005;
and that it is associated with high CV mortality. 20:575–579.
13. Davenport A. Intradialytic complications during hemodialysis.
Hemodial Int 2006; 10:162–167.
14. Fellner SK. Intradialytic hypertension: II. Semin Dial 1993; 6: 371–373.
15. Agarwal R, Andersen MJ, Pratt JH. On the importance of pedal edema
ACKNOWLEDGMENTS in hemodialysis patients. Clin J Am Soc Nephrol 2008; 3:153–158.
16. Cirit M, Akçiçek F, Terzioğlu E, Soydaş C, Ok E, Ozbaşli CF, Başçi A,
The study was brought about on behalf of the of hyperten- Mees EJ. ‘Paradoxical’ rise in blood pressure during ultrafiltration in
sion study group of The Italian Society of Nephrology. dialysis patients. Nephrol Dial Transplant 1995; 10:1417–1420.
17. Agarwal R, Light RP. Intradialytic hypertension is a marker of volume
excess. Nephrol Dial Transplant 2010; 25:3355–3361.
DISCLOSURE 18. Agarwal R, Alborzi P, Satyan S, Light RP. Dry-weight reduction in
hypertensive hemodialysis patients (DRIP): a randomized, controlled
The authors declared no conflict of interest. trial. Hypertension 2009; 53:500–507.
19. Nongnuch A, Campbell N, Stern E, El-Kateb S, Fuentes L, Davenport A.
Increased postdialysis systolic blood pressure is associated with extra-
cellular overhydration in hemodialysis outpatients. Kidney Int 2015;
87:452–457.
REFERENCES 20. Losito A, Del Vecchio L, Del Rosso G, Malandra R; Gruppo di Studio
Dell’Ipertensione Arteriosa, Società Italiana di Nefrologia. Blood pres-
1. Levin N. Intradialytic hypertension I. Semin Dial 1993; 6:370–371. sure and cardiovascular mortality in dialysis patients with left ventricu-
2. Inrig JK, Oddone EZ, Hasselblad V, Gillespie B, Patel UD, Reddan D, lar systolic dysfunction. Am J Hypertens 2014; 27:401–408.
Toto R, Himmelfarb J, Winchester JF, Stivelman J, Lindsay RM, Szczech 21. Locatelli F, Cavalli A, Tucci B, Viganò S, Di Filippo S. Can chronic
LA. Association of intradialytic blood pressure changes with hospitali- volume overload be recognized and prevented in hemodialysis
zation and mortality rates in prevalent ESRD patients. Kidney Int 2007; patients? Newer methods to assess volume status. Semin Dial 2009;
71:454–461. 22:492–494.
American Journal of Hypertension 29(6) June 2016 689
Downloaded from https://academic.oup.com/ajh/article-abstract/29/6/684/2622379
by guest
on 24 June 2018
Вам также может понравиться
- Pulmonary Hypertension in Hemodialysis PatientsДокумент5 страницPulmonary Hypertension in Hemodialysis PatientsDr. Jatin GargОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 4: VascularОт EverandComplementary and Alternative Medical Lab Testing Part 4: VascularОценок пока нет
- Pi Is 0272638616302645Документ9 страницPi Is 0272638616302645Eko PrasОценок пока нет
- Exercise Stress Test As An Antidote For Anxiety Ne PDFДокумент2 страницыExercise Stress Test As An Antidote For Anxiety Ne PDFmehrshad Farahpour Gp5Оценок пока нет
- Clinical Study: The Association Between Intradialytic Hypertension and Metabolic Disorders in End Stage Renal DiseaseДокумент9 страницClinical Study: The Association Between Intradialytic Hypertension and Metabolic Disorders in End Stage Renal Diseasecynthia nataliaОценок пока нет
- Special Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionДокумент8 страницSpecial Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionDavid SantosoОценок пока нет
- Hypertension in End-Stage Renal Disease: Eview RticleДокумент6 страницHypertension in End-Stage Renal Disease: Eview RticleGaema MiripОценок пока нет
- Predictors of Intradialytic Hypertension in Chronic End Stage Renal Dialysis Patients in A Tertiary Government Hospital in Davao CДокумент13 страницPredictors of Intradialytic Hypertension in Chronic End Stage Renal Dialysis Patients in A Tertiary Government Hospital in Davao CSari ChaerunisahОценок пока нет
- 1998 - Zager Et Al. - 'U' Curve Association of Blood Pressure and Mortality in Hemodialysis PatientsДокумент9 страниц1998 - Zager Et Al. - 'U' Curve Association of Blood Pressure and Mortality in Hemodialysis PatientsKTKL RSABОценок пока нет
- Intradialitic HypotensionДокумент7 страницIntradialitic HypotensionanitaОценок пока нет
- Intradialytic Hypertension in End Stage Renal Disease Patient: Prevalence and Clinical CharacteristicДокумент6 страницIntradialytic Hypertension in End Stage Renal Disease Patient: Prevalence and Clinical CharacteristicAmalОценок пока нет
- HipertensiДокумент37 страницHipertensiValentina PujiОценок пока нет
- Hipertension TranshemodialisisДокумент10 страницHipertension TranshemodialisisMonica HerreraОценок пока нет
- Comparison of Inflammatory Markers in HTNДокумент6 страницComparison of Inflammatory Markers in HTNDan JohnstonОценок пока нет
- Mechanisms, Clinical Implications, and Treatment of Intradialytic HypotensionДокумент7 страницMechanisms, Clinical Implications, and Treatment of Intradialytic Hypotensionhemer hadyn calderon alvitesОценок пока нет
- Cost Effectiveness and Resource AllocationДокумент7 страницCost Effectiveness and Resource AllocationSarah AmeliaОценок пока нет
- Hypertension Control, Apparent Treatment Resistance, and Outcomes in The Elderly Population With Chronic Kidney DiseaseДокумент12 страницHypertension Control, Apparent Treatment Resistance, and Outcomes in The Elderly Population With Chronic Kidney Diseasetika_876267153Оценок пока нет
- Hypertension Management in Transition From CKD A ERDS 2016Документ7 страницHypertension Management in Transition From CKD A ERDS 2016hemer hadyn calderon alvitesОценок пока нет
- Tgs Jurnal 1Документ7 страницTgs Jurnal 1suciОценок пока нет
- Diabetes Mellitus and Heart Failure 2017 The American Journal of MedicineДокумент11 страницDiabetes Mellitus and Heart Failure 2017 The American Journal of MedicineAlina PopaОценок пока нет
- JASN SDHD Paper 2005Документ11 страницJASN SDHD Paper 2005Carlos EghiОценок пока нет
- HTN Guidelines 1Документ12 страницHTN Guidelines 1lakshminivas PingaliОценок пока нет
- DNB Vol25 No2 142Документ7 страницDNB Vol25 No2 142Apsopela SandiveraОценок пока нет
- Go 2006Документ12 страницGo 2006my accountОценок пока нет
- Art Enfermedad Renal CronicaДокумент8 страницArt Enfermedad Renal CronicaLisset FernandezОценок пока нет
- Journal Reading PsikosisДокумент21 страницаJournal Reading PsikosisApsopela SandiveraОценок пока нет
- Research Article: Elevated Heparin-Induced Antibodies Are More Common in Diabetic Patients With Vascular DiseaseДокумент6 страницResearch Article: Elevated Heparin-Induced Antibodies Are More Common in Diabetic Patients With Vascular DiseaseAntony Boston MichaelОценок пока нет
- Arterial Hypertension e Clinical Trials Update 2021Документ11 страницArterial Hypertension e Clinical Trials Update 2021Dana MОценок пока нет
- Jurnal Int 2Документ14 страницJurnal Int 2rike aprilianaОценок пока нет
- Journal of Hypertension: Open Access: Hypertension-A Challenge To Modern MedicineДокумент2 страницыJournal of Hypertension: Open Access: Hypertension-A Challenge To Modern MedicineReiner ImranОценок пока нет
- Blood Pressure Management in Children On DialysisДокумент12 страницBlood Pressure Management in Children On DialysisinaОценок пока нет
- JCH 13 523Документ6 страницJCH 13 523Bunga dewanggi NugrohoОценок пока нет
- Ipri 36 1499588Документ6 страницIpri 36 1499588fani rudiyantiОценок пока нет
- CKD HT 3Документ8 страницCKD HT 3Peer TutorОценок пока нет
- Low Systemic Vascular ResistanceДокумент7 страницLow Systemic Vascular ResistanceMuhammad BadrushshalihОценок пока нет
- 228A ABSTRACTS - Cardiac Function and Heart Failure Jacc March 3, 2004Документ2 страницы228A ABSTRACTS - Cardiac Function and Heart Failure Jacc March 3, 2004Yulianty Saulina FransiscaОценок пока нет
- Nikhil Thesis AbstractДокумент28 страницNikhil Thesis AbstractNikhil KalasareОценок пока нет
- Cardiovascular Manifestations in Hyperthyroidism: Research ArticleДокумент7 страницCardiovascular Manifestations in Hyperthyroidism: Research Articlenurharyanti darmaningtyasОценок пока нет
- Management of Hypertension According To JNC 7: by Sandar Kyi, MDДокумент27 страницManagement of Hypertension According To JNC 7: by Sandar Kyi, MDDiana Da SilvaОценок пока нет
- Georgio Poul Ou 2010Документ16 страницGeorgio Poul Ou 2010ireneaureliaОценок пока нет
- Hubungan Neutrophyl To Lymphocyte Ratio Dengan Derajat Disfungsi Diastolik Pada Pasien HipertensiДокумент7 страницHubungan Neutrophyl To Lymphocyte Ratio Dengan Derajat Disfungsi Diastolik Pada Pasien HipertensiLutfhi ArshaldoОценок пока нет
- Epidemiology and Risk Factors in CKD Patients With Pulmonary HypertensionДокумент8 страницEpidemiology and Risk Factors in CKD Patients With Pulmonary HypertensionshaheershayanqaziОценок пока нет
- FCVM 09 860322Документ7 страницFCVM 09 860322Muh SutraОценок пока нет
- Management of HypertensionДокумент8 страницManagement of HypertensionJoe SingleОценок пока нет
- Association of Orthostatic Hypotension WithДокумент11 страницAssociation of Orthostatic Hypotension WithAulia Whiratama PutraОценок пока нет
- HHS Public Access: Pathophysiology and Implications of Intradialytic HypertensionДокумент13 страницHHS Public Access: Pathophysiology and Implications of Intradialytic HypertensionSari ChaerunisahОценок пока нет
- Prognostic Significance of Diastolic Dysfunction With Multiple Comorbidities in Heart Failure PatientsДокумент11 страницPrognostic Significance of Diastolic Dysfunction With Multiple Comorbidities in Heart Failure PatientsDefriyan RamziОценок пока нет
- The Prognostic Role of Anemia in Heart Failure PatientsДокумент7 страницThe Prognostic Role of Anemia in Heart Failure PatientsAnonymous rprdjdFMNzОценок пока нет
- 2359 4802 Ijcs 34 04 0400.x98175Документ9 страниц2359 4802 Ijcs 34 04 0400.x98175leo leioaОценок пока нет
- Nota 2Документ8 страницNota 2Hector GuzmanОценок пока нет
- Hypertension ThesisДокумент31 страницаHypertension ThesisNavin AdhikariОценок пока нет
- Relation Between Vascular Risk Factors and Cognition at Age 75Документ7 страницRelation Between Vascular Risk Factors and Cognition at Age 75Fajar Rudy QimindraОценок пока нет
- Intradialytic Hypertension and The Association WitДокумент9 страницIntradialytic Hypertension and The Association WitMimi MuhammidaОценок пока нет
- Diagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensiДокумент8 страницDiagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensidhyassОценок пока нет
- The Dynamics of Haemostatic Parameters in Acute Psychotic Patients: A One-Year Prospective StudyДокумент8 страницThe Dynamics of Haemostatic Parameters in Acute Psychotic Patients: A One-Year Prospective StudyApsopela SandiveraОценок пока нет
- Transfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaДокумент41 страницаTransfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaAETCM Emergency medicineОценок пока нет
- Plasma Lipids: Optimal Levels for HealthОт EverandPlasma Lipids: Optimal Levels for HealthAmerican Health FoundationОценок пока нет
- The Prevalence of ArterialДокумент8 страницThe Prevalence of ArterialInternational Medical PublisherОценок пока нет
- The Prevalence of Resistant Hypertension Among TypДокумент7 страницThe Prevalence of Resistant Hypertension Among TypProfessor Kamel AjlouniОценок пока нет
- Surviving Sepsis Hour 1 Bundle InfographДокумент1 страницаSurviving Sepsis Hour 1 Bundle InfographLaura PutriОценок пока нет
- Guidelines On Chronic Kidney Disease: (NKF K/Doqi)Документ32 страницыGuidelines On Chronic Kidney Disease: (NKF K/Doqi)Laura PutriОценок пока нет
- Morning Report Monday, 5 February 2018: Dept of Neurology G29Документ21 страницаMorning Report Monday, 5 February 2018: Dept of Neurology G29Laura PutriОценок пока нет
- Optical Prescription Details August 20XXДокумент3 страницыOptical Prescription Details August 20XXLaura PutriОценок пока нет
- Print FriendlyДокумент14 страницPrint FriendlyLaura PutriОценок пока нет
- Colloidsdengue 11 1 C RДокумент21 страницаColloidsdengue 11 1 C RLaura PutriОценок пока нет
- Protein Uri AДокумент12 страницProtein Uri ALaura PutriОценок пока нет
- 2005 Lipid Lowering DrugsДокумент22 страницы2005 Lipid Lowering DrugsLaura PutriОценок пока нет
- Penatalaksanaan: Amirah Muhammad AДокумент8 страницPenatalaksanaan: Amirah Muhammad ALaura PutriОценок пока нет
- Jadwal Pembelajaran Blok Neuromuskuloskeletal I Kelas A (Warna Hijau) TAHUN AJARAN 2013/2014 Update 5/11/2013Документ3 страницыJadwal Pembelajaran Blok Neuromuskuloskeletal I Kelas A (Warna Hijau) TAHUN AJARAN 2013/2014 Update 5/11/2013Laura PutriОценок пока нет
- 2121-Article Text-9456-1-10-20230131Документ8 страниц2121-Article Text-9456-1-10-20230131Çağdaş BaytarОценок пока нет
- Giant Bowen's Disease On The Face: Case Report and Review of The LiteratureДокумент4 страницыGiant Bowen's Disease On The Face: Case Report and Review of The LiteraturezoeyОценок пока нет
- Case Files PedsДокумент54 страницыCase Files PedsSam ZeezОценок пока нет
- ISMP Voluume 15 No 10 Oct 2017-NurseAdviseERR201710Документ4 страницыISMP Voluume 15 No 10 Oct 2017-NurseAdviseERR201710uss uusОценок пока нет
- Bhavishya Arogya ProspectusДокумент7 страницBhavishya Arogya ProspectusHarsh RajОценок пока нет
- .Au Files Dysbiosis ScoreДокумент2 страницы.Au Files Dysbiosis ScorekenetmartinОценок пока нет
- YH-5504SB ManualДокумент17 страницYH-5504SB ManualBill BrownОценок пока нет
- Ontogeny and Phylogeny of Immune SystemДокумент3 страницыOntogeny and Phylogeny of Immune SystemPM Basiloy - AloОценок пока нет
- CLUBFOOT GuidelineДокумент111 страницCLUBFOOT GuidelineNuhiat NahreenОценок пока нет
- Chapter 1: Introduction To Operative DentistryДокумент11 страницChapter 1: Introduction To Operative DentistryMariam AdnanОценок пока нет
- Disorders of The Adrenal Glands: Adrenal Cortical Adenoma and CarcinomaДокумент9 страницDisorders of The Adrenal Glands: Adrenal Cortical Adenoma and Carcinomahussain AltaherОценок пока нет
- Abdul Malik Hassim Lecturer DMA Management & Science UniversityДокумент21 страницаAbdul Malik Hassim Lecturer DMA Management & Science UniversitykimmgizelleОценок пока нет
- Effects of Advanced Carbohydrate Counting On Glucose Control and QolДокумент9 страницEffects of Advanced Carbohydrate Counting On Glucose Control and QollloplОценок пока нет
- TURBT FinalДокумент52 страницыTURBT FinalMuhammad RafiОценок пока нет
- Slide Materi Dr. Kevin Triangto, SPKFR - Heart Failure - PMR4GP 2022Документ27 страницSlide Materi Dr. Kevin Triangto, SPKFR - Heart Failure - PMR4GP 2022Maulia Wisda Era ChresiaОценок пока нет
- Contact Urticaria Syndrome: Occupational Aspects: Becky S. Li, Iris S. Ale, and Howard I. MaibachДокумент34 страницыContact Urticaria Syndrome: Occupational Aspects: Becky S. Li, Iris S. Ale, and Howard I. MaibachsaskiakonitaОценок пока нет
- Abortion in CattleДокумент6 страницAbortion in CattlekumarpujariОценок пока нет
- Hepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseДокумент12 страницHepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseSarah FaziraОценок пока нет
- Treating Lupus Using Tung PointstДокумент5 страницTreating Lupus Using Tung PointstOmer Binmahfooz100% (4)
- 8 Cns StimulantsДокумент46 страниц8 Cns StimulantslouradelОценок пока нет
- Acute Kidney InjuryДокумент49 страницAcute Kidney InjuryfikasywОценок пока нет
- Emergency Report Thursday:, October 07 2021Документ21 страницаEmergency Report Thursday:, October 07 2021Wilson WijayaОценок пока нет
- CBCT-Scan in DentistryДокумент24 страницыCBCT-Scan in DentistryBilly Sam80% (5)
- Cumulative Trauma DisordersДокумент70 страницCumulative Trauma DisordersBishal BistaОценок пока нет
- Giardia Duodenalis Affect Farmers Child Growth and DevelopmentДокумент2 страницыGiardia Duodenalis Affect Farmers Child Growth and DevelopmentAnitaОценок пока нет
- Frederick Griffith: Bacterial TransformationДокумент4 страницыFrederick Griffith: Bacterial Transformationrasha nada100% (1)
- Failure of Weaning:: According To The European Respiratory Society (ERS) Task ForceДокумент12 страницFailure of Weaning:: According To The European Respiratory Society (ERS) Task ForceAmr El Taher0% (1)
- Colchicine Drug Study For Gouty ArthritisДокумент3 страницыColchicine Drug Study For Gouty ArthritisLeslie PaguioОценок пока нет
- REAL in Nursing Journal (RNJ)Документ8 страницREAL in Nursing Journal (RNJ)Anonymous 8hlR5KvОценок пока нет
- Medical Terms and Definitons Commonly Used in MCNДокумент15 страницMedical Terms and Definitons Commonly Used in MCNjoemel gregoriОценок пока нет