Академический Документы
Профессиональный Документы
Культура Документы
Sample History
Загружено:
isprikitik3Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Sample History
Загружено:
isprikitik3Авторское право:
Доступные форматы
7/18/18
Patient was seen and assessed with the following vital signs: BP=110/70, CR=72, RR=20, Temp= 36.5,
O2sat=100%. Patient was unconscious with a GCS score of 8 (E2V1M5). Physical Examination revealed
bilateral rhonchi upon auscultation of the chest. Diet includes Glucorna 5 scoops in 1 glass of water every
4 hours with 30cc pre and post flushing and IVF of PNSS x 60cc/hour. Medications included Polymixin B
150 mg TIV q12, Noripenem 500mg TIV q8, Amlodipine + Indapamide 10/1.5 mg/tab, 1 tablet OD,
Rosuvastatin 10 mg/tab, 1 tablet OD at night, Lactiracetam 100 mg/mL, 10 mL every 12 hours, Duavent
½ +2cc NSS every 6 hours, NAC 600 mg/tab, 1 tab BID, Hexetidine swab q6, Theophylline 125 mg/tab BID,
Nebivolol 5mg/tab, 1 tablet OD, CaCO3 tab, OD, Conzace tab, 1 tablet OD, Paracetamol 500 mg/tab, 1
tablet every 4 hours PRN, Diazepam 5 mg TIV PRN, Insulin glargine 20 units SQ OD. Patient was seen by
ENT-OHNS, and Neuro services and was advised to continue present medications and management.
Patient was also seen by the pulmo service in which they modified the MV setup to FiO2= 30%, PEEP= 14,
VT= 350 mL BVR= 14. Additional procedures advised by the pulmo service included suctioning of
secretions as well as to watch out for Hypotension and desaturation.
7/19/18
Patient was seen and assessed with the following vital signs: BP=100/60, CR=88, RR=20, Temp= 36.5,
O2sat=98%. Patient had no febrile episodes as well as desaturation and hypotension. On evaluation,
patient was unconscious with a GCS score of 10 (E4V1M5). Pertinent findings on physical examination
revealed 3mm pupillary light reflex, bilateral rhonchi upon auscultation of the chest and +2 deep tendon
reflexes. Diet includes Glucorna 5 scoops in 1 glass of water every 4 hours with 30cc pre and post flushing.
CBG monitoring in the morning was requested as part of diagnostics. Medications included Polymixin B
150 mg TIV q12, Noripenem 500mg TIV q8, Amlodipine + Indapamide 10/1.5 mg/tab, 1 tablet OD,
Rosuvastatin 10 mg/tab, 1 tablet OD at night, Lactiracetam 100 mg/mL, 10 mL every 12 hours, Duavent
½ +2cc NSS every 6 hours, NAC 600 mg/tab, 1 tab BID, Hexetidine swab q6, Theophylline 125 mg/tab BID,
Nebivolol 5mg/tab, 1 tablet OD, CaCO3 tab, OD, Conzace tab, 1 tablet OD, Paracetamol 500 mg/tab, 1
tablet every 4 hours PRN, Diazepam 5 mg TIV PRN, Insulin glargine 20 units SQ OD. Patient was seen by
ENT-OHNS service and was advised to continue present medications and management. Additional
instructions include suctioning of secretions as well as to watch out for Hypotension, fever and
desaturation
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Sagittarius ProfileДокумент3 страницыSagittarius ProfileWAQAS SHARIFОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- D6 Gamemasters Aid Screen Weg51019eOGLДокумент40 страницD6 Gamemasters Aid Screen Weg51019eOGLMr DM100% (1)
- Sheiko 13week Beginner ProgramДокумент16 страницSheiko 13week Beginner ProgramAnders DahlОценок пока нет
- 160 78-m1Документ70 страниц160 78-m1George100% (7)
- Clinical Chemistry (Lecture) - PrelimsДокумент12 страницClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Epri Guide For Transmission Line Groundingpdf PDF FreeДокумент188 страницEpri Guide For Transmission Line Groundingpdf PDF FreeHolman Wbeimar Suarez Niño100% (1)
- Project Report - Performance Anaylysis of Mutual Funds in IndiaДокумент52 страницыProject Report - Performance Anaylysis of Mutual Funds in Indiapankaj100% (1)
- Buzan, Barry - Security, The State, The 'New World Order' & BeyondДокумент15 страницBuzan, Barry - Security, The State, The 'New World Order' & Beyondyossara26100% (3)
- ImmunityДокумент70 страницImmunityisprikitik30% (2)
- Evaluation - For External Trainings 06222017Документ1 страницаEvaluation - For External Trainings 06222017isprikitik3Оценок пока нет
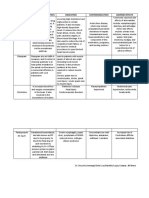
- Drugs Mechanism of Action Indication Contraindication Adverse EffectsДокумент2 страницыDrugs Mechanism of Action Indication Contraindication Adverse Effectsisprikitik3Оценок пока нет
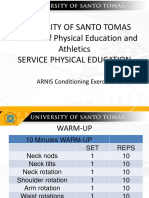
- 6warm Up Conditioning-ExercisesДокумент7 страниц6warm Up Conditioning-Exercisesisprikitik3Оценок пока нет
- 8activity Log Journal For MEN and WomenДокумент2 страницы8activity Log Journal For MEN and Womenisprikitik3Оценок пока нет
- CD RADIO Upper and Lower ExtДокумент12 страницCD RADIO Upper and Lower Extisprikitik3Оценок пока нет
- WHO - Current PartnersДокумент2 страницыWHO - Current Partnersisprikitik3Оценок пока нет
- IM Inside (Therapeutic Index Template)Документ2 страницыIM Inside (Therapeutic Index Template)isprikitik3Оценок пока нет
- San Lazaro Notes PDFДокумент8 страницSan Lazaro Notes PDFisprikitik3Оценок пока нет
- Ao Final ProgramДокумент16 страницAo Final Programisprikitik3Оценок пока нет
- Cyanide Poisoning Written ReportДокумент5 страницCyanide Poisoning Written Reportisprikitik3Оценок пока нет
- Crown Lengthening of ToothДокумент4 страницыCrown Lengthening of Toothisprikitik3Оценок пока нет
- Individual Reflections Format (CPH)Документ2 страницыIndividual Reflections Format (CPH)isprikitik3Оценок пока нет
- Biochemistry 1.6 - ABO Blood Typing and Crossmatching (A1 Group 6)Документ68 страницBiochemistry 1.6 - ABO Blood Typing and Crossmatching (A1 Group 6)isprikitik3Оценок пока нет
- Request LetterДокумент1 страницаRequest Letterisprikitik3Оценок пока нет
- Recommendation LetterДокумент1 страницаRecommendation Letterisprikitik3Оценок пока нет
- God's Creation: Christianity Is An Abrahamic, Monotheistic Religion Based On The Life and OralДокумент2 страницыGod's Creation: Christianity Is An Abrahamic, Monotheistic Religion Based On The Life and Oralisprikitik3Оценок пока нет
- Manuscript Group 2 CPHДокумент30 страницManuscript Group 2 CPHKrisha Mae SalazarОценок пока нет
- Authorization LetterДокумент1 страницаAuthorization Letterisprikitik3Оценок пока нет
- Excuse LettersДокумент7 страницExcuse Lettersisprikitik3Оценок пока нет
- Individual Reflections FormatДокумент1 страницаIndividual Reflections Formatisprikitik3Оценок пока нет
- World LitДокумент4 страницыWorld Litisprikitik3Оценок пока нет
- World LitДокумент4 страницыWorld Litisprikitik3Оценок пока нет
- Request LetterДокумент1 страницаRequest Letterisprikitik3Оценок пока нет
- Intro To My CologyДокумент86 страницIntro To My Cologyisprikitik3Оценок пока нет
- Classification of CarbsДокумент3 страницыClassification of Carbsisprikitik3Оценок пока нет
- MycologyДокумент3 страницыMycologyisprikitik3Оценок пока нет
- MicroscopesДокумент6 страницMicroscopesRenz Mervin RiveraОценок пока нет
- D D D D D D D: SN54HC574, SN74HC574 Octal Edge-Triggered D-Type Flip-Flops With 3-State OutputsДокумент16 страницD D D D D D D: SN54HC574, SN74HC574 Octal Edge-Triggered D-Type Flip-Flops With 3-State OutputsJADERSONОценок пока нет
- What Is E-CollaborationДокумент7 страницWhat Is E-CollaborationToumba LimbreОценок пока нет
- Sap Business Objects Edge Series 3.1 Install Windows enДокумент104 страницыSap Business Objects Edge Series 3.1 Install Windows enGerardoОценок пока нет
- Arch Plan-Agner Boco (For Blue Print) - p1Документ1 страницаArch Plan-Agner Boco (For Blue Print) - p1Jay CeeОценок пока нет
- Admission Prspectus English 2021-2022Документ9 страницAdmission Prspectus English 2021-2022A.B. SiОценок пока нет
- Assignment 2 Management Perspective Son Leadership MotivationДокумент14 страницAssignment 2 Management Perspective Son Leadership MotivationHoneyVasudevОценок пока нет
- Method For Determination of Iron Folic Acid & Vitamin B12 in FRK - 07.11.2023Документ17 страницMethod For Determination of Iron Folic Acid & Vitamin B12 in FRK - 07.11.2023jonesbennetteОценок пока нет
- Unit 8 Atomic Fluorescence Spectrometry PDFДокумент23 страницыUnit 8 Atomic Fluorescence Spectrometry PDFCh AswadОценок пока нет
- Hunk (Aakc) - (Nov 2015)Документ68 страницHunk (Aakc) - (Nov 2015)Russell RiderОценок пока нет
- The Mystery of Putins DissertationДокумент16 страницThe Mystery of Putins DissertationDoinaCebanuОценок пока нет
- Olp Lesson PlanДокумент2 страницыOlp Lesson Planapi-654865620Оценок пока нет
- Questions 1Документ3 страницыQuestions 1krp_212003Оценок пока нет
- Culture NegotiationsДокумент17 страницCulture NegotiationsShikha SharmaОценок пока нет
- Jahnteller Effect Unit 3 2017Документ15 страницJahnteller Effect Unit 3 2017Jaleel BrownОценок пока нет
- Pset 2Документ13 страницPset 2rishiko aquinoОценок пока нет
- 2010 DOE FEMP Exterior Lighting GuideДокумент38 страниц2010 DOE FEMP Exterior Lighting GuideMoideen Thashreef100% (1)
- Kibera Mirror JULYДокумент8 страницKibera Mirror JULYvincent achuka maisibaОценок пока нет
- North-South Railway Project - South LineДокумент49 страницNorth-South Railway Project - South LinesuperОценок пока нет
- Unit 5, Orders and Cover Letters of Orders For StsДокумент13 страницUnit 5, Orders and Cover Letters of Orders For StsthuhienОценок пока нет
- Doyennés Et Granges de L'abbaye de Cluny (A. Guerreau)Документ45 страницDoyennés Et Granges de L'abbaye de Cluny (A. Guerreau)theseus11Оценок пока нет
- History of Nursing: Nursing in The Near EastДокумент7 страницHistory of Nursing: Nursing in The Near EastCatherine PradoОценок пока нет
- Lab 4 SimulationДокумент8 страницLab 4 SimulationaziziОценок пока нет
- Listening 3b Skills Test 1aДокумент3 страницыListening 3b Skills Test 1aPticaSelicaОценок пока нет