Академический Документы
Профессиональный Документы
Культура Документы
Case7.Fung Et Al-1998-Ultrasound in Obstetrics & Gynecology
Загружено:
wijeАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Case7.Fung Et Al-1998-Ultrasound in Obstetrics & Gynecology
Загружено:
wijeАвторское право:
Доступные форматы
Ultrasound Obstet Gynecol 1998;12:430–433
Poor perinatal outcome associated with vasa
previa: is it preventable? A report of three cases
and review of the literature
T. Y. Fung and T. K. Lau
Department of Obstetrics and Gynaecology, Prince of Wales Hospital, The Chinese University of Hong Kong, Shatin,
Hong Kong
Key words: VASA PREVIA, PREGNANCY OUTCOME, ULTRASOUND
ABSTRACT
We describe three cases of vasa previa and review the We describe here the perinatal management of three
English-language literature for all cases reported since cases of vasa previa, and review the literature.
1980. Antenatal diagnosis was significantly associated with
decreased fetal mortality (p = 0.033). A low- lying placenta
is a risk factor for vasa previa, as it occurred in 81% of
CASE 1
patients. A 29-year-old woman, gravida 3, para 1, had an ante-
partum hemorrhage at 29 weeks of gestation. An ultra-
sound scan revealed an anterior placenta which extended
over the internal os. A repeat ultrasound scan at 32 weeks
INTRODUCTION showed the placenta not to be low lying. The woman was
Vasa previa is a condition in which the umbilical vessels, admitted again because of vaginal bleeding at 35 weeks of
unsupported by either the umbilical cord or placental gestation, and vasa previa was suspected on trans-
tissue, traverse the fetal membranes of the lower segment in abdominal sonography and confirmed with color Doppler
front of the presenting part1. The true incidence is still (Figures 1 and 2). An elective lower segment Cesarean
unknown, but varies from 1 in 1275 to 1 in 50002–5. Vasa section was performed at 36 weeks, and a bilobed placenta
previa generally occurs only in association with velamen- was found with vessels running across the internal os. A
tous insertion of the umbilical cord, bipartite placenta, or 2500-g female was delivered with Apgar scores of 7 and 9
succenturiate lobe. at 1 and 5 min, respectively. The baby required no resusci-
Vasa previa is an important obstetric complication; the tation and there were no neonatal complications.
associated perinatal mortality rate has been reported to be
as high as 52–66%1,6,7. This high fetal loss rate is probably
due to the following factors. Fetal vessels, which are
CASE 2
normally protected by Wharton’s jelly within the umbilical A 20-year-old woman, gravida 3, para 0, was admitted for
cord, are unsupported in vasa previa. These vessels are ‘heavy show’ at 39 weeks of gestation. The antenatal
firmly adherent to overlying chorionic membranes, which course was uncomplicated and no antenatal ultrasound
at the time of either spontaneous or artificial rupture may examination was performed. Labor was induced with arti-
lead to tearing of the underlying vessels. Furthermore, ficial rupture of membranes, which revealed clear amniotic
hemorrhage due to vasa previa is rapidly fatal, because the fluid. There were recurrent delay decelerations soon after
bleeding is from the fetus which has only a small circula- the rupture of membranes. The fetus was therefore deliv-
tory volume. To prevent this cascade of complications, one ered by emergency Cesarean section, at which the diagnosis
must have a high index of suspicion when managing of vasa previa was made. The baby boy weighed 3200 g,
women with antepartum hemorrhage, so that affected with an Apgar score of 3 at 1 min and 5 at 5 min. The baby
pregnancies can be delivered early. Alternatively, a good required immediate resuscitation, including intubation,
fetal outcome can be expected if this condition is diagnosed mechanical ventilation and blood transfusion; he sub-
and the fetus delivered before the onset of bleeding. sequently developed convulsions. Examination of the
Correspondence: Dr T.Y. Fung, Department of Obstetrics and Gynaecology, Prince of Wales Hospital, The Chinese University of Hong Kong,
Shatin, Hong Kong
CA SE REPO RT 430 Received 20–11–97
Revised 7–5–98
Accepted 11–5–98
AMA: First Proof 97/199
Vasa previa Fung and Lau
that the vessels close to the site of amniotomy had rup-
tured. There was no evidence of direct injury to the vessels
by the instruments used.
DISCUSSION
With the advances in ultrasound technology in recent
Colour
years, vasa previa has been successfully visualized and diag-
nosed antenatally by means of transabdominal sonography,
transvaginal sonography and spectral and color Doppler.
From the three cases reported here, we found that antenatal
diagnosis of vasa previa was associated with the better
outcome. To confirm this observation, and to identify
possible risk factors, we identified all cases of vasa previa
reported in the English-language literature by CD-Plus
Medline using the key word ‘vasa previa’. The latest review
Figure 1 Longitudinal section through the internal cervical os
on vasa previa was reported in the 1980s, when examina-
with color Doppler showing the vasa previa
tion by ultrasound, especially Doppler ultrasound, was still
not widespread6. We therefore limited our review to the
period between 1980 and 1997. The original papers were
retrieved and reviewed and references were checked. We
recorded all those fetuses with Apgar scores of less than 7
at 5 min (excluding stillbirths and neonatal deaths) and all
those fetuses who suffered from anemia or required blood
transfusion after delivery.
Colour
Including our three cases, there were 48 cases of vasa
previa reported in 34 papers between 1980 and 19978–41.
There were five sets of twins and 43 singleton pregnancies.
The fetal outcomes according to the time of diagnosis of
vasa previa are shown in Table 1. Overall, there were six
stillbirths and one neonatal death, giving a perinatal mor-
tality rate of 13.2% (seven of 53 babies). In the remaining
46 who were live born, ten (21.7%) had a 5-min Apgar
score of less than 7 (overall 18.9%) and 14 fetuses (30.4%)
suffered from anemia or required blood transfusion (over-
Figure 2 Slightly oblique view across the cervical os, demonstrat-
all 26.4%). Among these 14 patients, 12 fetuses required
ing by color Doppler the running of the vessels that pass above
neonatal blood transfusion22,29,31,35–37,39–41 and two fetuses
the os
had suffered from anemia27,34. The fetal loss rate
(p = 0.033; Fisher’s exact test), the incidence of 5-min
placenta confirmed velamentous insertion of the cord and Apgar scores less than 7 (p = 0.033; Fisher’s exact test) and
that the velamentous portion of the vessels had ruptured. the incidence of fetal anemia or neonatal blood transfusion
(p = 0.002; Fisher’s exact test) were significantly less if the
diagnosis was made in the antenatal period (Table 1).
CASE 3 When antenatal diagnosis was not made before the on-
A 34-year-old woman, gravida 4, para 3, had an ultra- set of labor, all the five fetuses (including one pair of twins)
sound scan performed at 23 weeks of gestation because of complicated with antepartum hemorrhage had very poor
a previous intrauterine death. The fetus was normal but outcomes (Table 1). The fetal mortality was significantly
observations of the placental site were not recorded. The higher than in those who had vaginal bleeding during
woman was admitted at 37 weeks for proteinuria and labor, irrespective of whether it was spontaneous
impaired renal function. An ultrasound scan was repeated (p = 0.010; Fisher’s exact test) or after obstetric manipula-
and the placenta was shown to be situated in the upper tion (p = 0.032; Fisher’s exact test). The difference in neo-
posterior uterine wall. Induction of labor was performed natal outcome was most probably because of early
by artificial rupture of membranes, which revealed blood- detection and intervention for fetal distress by intrapartum
stained amniotic fluid and was followed by recurrent late fetal monitoring when bleeding occurred during labor.
decelerations. An emergency Cesarean section was per- Since more fetal losses occurred among those with a
formed and vasa previa was confirmed. A female baby was history of antepartum hemorrhage when vasa previa was
delivered with birth weight of 2500 g and Apgar scores of not diagnosed antenatally, it remains to be proved that
8 and 10 at 1 and 5 mins, respectively. Examination of the prenatal diagnosis of vasa previa reduces mortality com-
placenta showed velamentous insertion of the cord, and pared to active management of intrapartum bleeding or
Ultrasound in Obstetrics and Gynecology 431
97/199 AMA: First Proof
Vasa previa Fung and Lau
Table 1 Fetal outcome according to the time of diagnosis of vasa previa
Number of
Number of fetuses suffering Number of
Number fetuses with from anemia or Number of fetuses with
Time of diagnosis of Apgar score of requiring blood stillbirths and unknown
of vasa previa References fetuses < 7 at 5 min transfusion neonatal deaths outcome
Antenatal 8–22, case 1 22 1 (4.5%) 1 (4.5%) 0 (0.0%) 0
No history of vaginal bleeding 8–17, 20 16 0 0 0 0
History of antepartum 18–22, case 1 6 1 1 0 0
hemorrhage
Intrapartum or after delivery 23–41, cases 2,3 31 9 (29%)* 13 (41.9%)** 7 (22.5%)*** 1
No intrapartum bleeding
no history of vaginal bleeding 23–27, 39 6 0 0 1 1
history of antepartum 20, 28–30 5 1 1 4 0
hemorrhage (vasa previa
not diagnosed antenatally)
Intrapartum bleeding
spontaneous 26, 27, 30–37 12 4 8 1 0
after manipulation (digital 26, 38–41, 8 4 4 1 0
examination, artificial cases 2,3
rupture of membranes or
insertion of scalp electrode)
Total 53 10 (18.9%) 14 (26.4%) 7 (13.2%) 1
The asterisks represent significant differences between the ‘Antenatal’ and ‘Intrapartum or after delivery’ groups. *p = 0.033 (Fisher’s
exact test); **p = 0.002 (Fisher’s exact test); ***p = 0.033 (Fisher’s exact test)
distress with expeditious fetal delivery. However, it should placenta in this group of patients (81%) was significantly
be noted that fetal morbidity, e.g. with fetal anemia, or (p < 0.001) higher than that in the general population
with neonatal blood transfusion or low 5-min Apgar score, which has been estimated to be 53/100042. In fact, the
was significantly increased when intrapartum bleeding diagnosis of vasa previa or bilobed placenta was estab-
occurred (p < 0.002 and p = 0.02, respectively; Fisher’s lished with color Doppler in 12 cases during subsequent
exact test). With the current information, however, it is scans. The diagnosis was missed in the remaining five cases
unclear whether the low Apgar score was a direct result of and in none of these cases was Doppler ultrasound
fetal bleeding or was secondary to compression of unpro- reported to have been used. On the basis of these findings,
tected vessels by the presenting part. we suggest that low-lying placenta before 30 weeks of
The results of our review show that the major risk of gestation is an important risk factor for vasa previa.
vasa previa to fetal mortality and morbidity is potentially The observed association between low-lying placenta
preventable if the correct diagnosis is made before the onset and vasa previa is in agreement with the theory of tropho-
of labor. Various methods have been used to diagnose vasa tropism first proposed in 1902 by Strassmann, who des-
previa. Among the 20 cases (including two sets of twins) in cribed the pathogenesis of velamentous insertion of
which diagnosis was made antenatally, 16 were by ultra- the umbilical cord from a low-lying placenta in early
sound, three by direct visualization either by endoscopy or gestation43.
by amnioscopy17 and one by the Apt test22. Among all On the basis of our findings, we suggest that the placen-
diagnostic methods, ultrasound appears to be the most tal site and extraplacental lobe should be recorded in all
non-invasive, and one that potentially could be used in all routine second-trimester ultrasound scans. If an extra-
cases. However, it is important to determine which patients placental lobe is detected in the second trimester, vasa
should have an ultrasound examination to exclude vasa previa should be excluded or confirmed by transvaginal
previa. B-mode or Doppler ultrasound with or without color-
Vasa previa is usually associated with velamentous coding. If the placenta is found to be low lying in the
insertion of the umbilical cord or a bilobed placenta. If second trimester, the cord insertion needs to be determined.
either of these two conditions is detected on ultra- A repeat ultrasound examination must be performed in the
sound examination, vasa previa must be excluded. The third trimester to exclude placenta previa, which occurs in
visualization of fetal vessels over the lower segment may be 10% of these patients42. If placenta previa is not present in
facilitated by the use of spectral and color Doppler the subsequent examination, particular attention should be
ultrasound9–16,18–20. paid to exclude the presence of vasa previa, by transvaginal
Among the 48 cases reviewed, 21 had a documented B-mode or Doppler ultrasound.
ultrasound scan performed before 30 weeks’ gestation In summary, vasa previa is strongly associated with ab-
(14–30 weeks of gestation). The placental site was des- normal placentation before 30 weeks of gestation. Both
cribed as low lying in 17 cases8–15,18–20,26,32,34,40,Case 1 (81%), vasa previa and abnormal placentation in the second tri-
as bilobed in one17, not low in one17 and was not com- mester can be accurately diagnosed by modern ultrasound
mented upon in two21,Case 3. The incidence of low-lying technology. Most of the adverse fetal outcomes associated
432 Ultrasound in Obstetrics and Gynecology
AMA: First Proof 97/199
Vasa previa Fung and Lau
with vasa previa should be preventable if the correct diag- 21. Nimmo MJ, Kinsella D, Andrews HS. MRI in pregnancy: the
nosis is made antenatally. diagnosis of vasa previa by magnetic resonance imaging.
Bristol Med Chir J 1988;103:12
22. VanDrie DM, Kammeraad LA. Vasa previa. Case report, re-
REFERENCES view and presentation of a new diagnostic method. J Reprod
Med 1981;26:577–80
1. Evans GM. Vasa praevia. Br Med J 1952;2:1243 23. Bright DA, Becker LJ. Vasa previa: an unusual cause of fetal
2. Carp HJ, Mashiach S, Serr DM. Vasa previa: a major compli- distress. J Am Board Fam Pract 1991;4:465–7
cation and its management. Obstet Gynecol 1979;53:273–5 24. Burton G, Saunders DM. Vasa praevia: another cause for
3. Vago T, Caspi EL. Antepartum binding due to injury of vela- concern in in vitro fertilization pregnancies. Aust NZ J Obstet
mentous placental vessels. Obstet Gynecol 1962;20:671–4 Gynaecol 1988;28:180–1
4. Quek S, Tan KL. Vasa praevia. Aust NZ J Obstet Gynaecol 25. Cordero DR, Helfgott AW, Landy HJ, Reik RF, Medina C,
1972;12:206–9 O’Sullivan MJ. A non-hemorrhagic manifestation of vasa
5. Torrey WE. Vasa previa. Am J Obstet Gynecol 1952;63: previa: a clinicopathologic case report. Obstet Gynecol 1933;
146–52 82:698–700
6. Kouyoumdjian A. Velamentous insertion of the umbilical 26. Dougall A, Baird CH. Vasa praevia – report of three cases and
cord. Obstet Gynecol 1980;56:737–42 review of literature. Br J Obstet Gynaecol 1987;94:712–15
7. Rucker MP, Tureman GR. Vasa previa. Virginia Med 27. Good MC, Copas PR, Kleinman GE, Caudle MR. Vasa
Monthly 1952; 72:202–7 previa. J Tenn Med Assoc 1990;83:499–501
8. Clerici G, Burnelli L, Lauro V, Pilu GL, Di Renzo GC. Pre- 28. Antoine C, Young BK, Silverman F, Greco MA, Alvarez SP.
natal diagnosis of vasa previa presenting as amniotic band. ‘A Sinusoidal fetal heart rate pattern with vasa previa in twin
not so innocent amniotic band’. Ultrasound Obstet Gynecol pregnancy. J Reprod Med 1982;27:295–300
1996;7:61–3 29. Gantt PA, Bird JS Jr, Randall GW. Sinusoidal fetal heart rate
9. Devesa R, Munoz A, Torrents M, Carrera JM. Prenatal diag- pattern with vasa previa. J Tenn Med Assoc 1990;83:393–4
nosis of vasa previa with transvaginal color Doppler ultra- 30. Jones KP, Wheater AW, Musgrave W. Simple test for bleeding
sound [Letter]. Ultrasound Obstet Gynecol 1996;8:139–41 from vasa praevia [published erratum appears in Lancet 1988;
10. Daly-Jones E, Hollingsworth J, Sepulveda W. Vasa praevia: 1:314]. Lancet 1987;2:1430–1
second trimester diagnosis using colour flow imaging. Br J 31. Hanretty KP. Ruptured vasa praevia. Scot Med J 1985;30:
Obstet Gynaecol 1996;103:284–6 115–16
11. Gianopoulos J, Carver T, Tomich PG, Karlman R, Gadwood 32. Arts H, Eyck JV. Antenatal diagnosis of vasa previa by trans-
K. Diagnosis of vasa previa with ultrasonography. Obstet vaginal color Doppler sonography. Ultrasound Obstet Gyne-
Gynecol 1987;69:488–91 col 1993;3:276–8
12. Hata K, Hata T, Fujiwaki R, Ariyuki Y, Manabe A, Kitao M. 33. Kruitwagen RF, Nijhuis JG. Ruptured vasa praevia indicated
An accurate antenatal diagnosis of vasa previa with trans- by a sinusoidal fetal heart rate pattern: a case report. Eur J
vaginal color Doppler ultrasonography. Am J Obstet Gynecol Obstet Gynecol Reprod Biol 1991;39:147–50
1994;171:265–7 34. Reuter KL, Davidoff A, Hunter T. Vasa previa. J Clin Ultra-
13. Hsieh FJ, Chen HF, Ko TM, Hsieh CY, Chen HY. Antenatal sound 1988;16:346–8
diagnosis of vasa previa by color-flow mapping. J Ultrasound 35. Tollison SB, Huang PH. Vasa previa. A case report. J Reprod
Med 1991;10:397–9 Med 1988;33:329–30
14. Nelson LH, Melone PJ, King M. Diagnosis of vasa previa with 36. Schellpfeffer MA. Improved neonatal outcome of vasa previa
transvaginal and color flow Doppler ultrasound. Obstet with aggressive intrapartum management. A report of two
Gynecol 1990;76:506–9 cases. J Reprod Med 1995;40:327–32
15. Meyer WJ, Blumenthal L, Cadkin A, Gauthier DW, 37. Silva PD, Stoskopf CG, Keegan KA, Murata Y. Use of fetal
Rotmensch S. Vasa previa: prenatal diagnosis with trans- scalp hematocrit in the diagnosis of severe hemorrhage from
vaginal color Doppler flow imaging. Am J Obstet Gynecol vasa previa. Am J Obstet Gynecol 1985;153:307–8
1993;169:1627–9 38. Bhattacharyya N. Vasa praevia. J Ind Med Assoc 1990;88:
16. Raga F, Ballester MJ, Osborne NG, Bonilla-Musoles F. Role 229–30
of color flow Doppler ultrasonography in diagnosing vela- 39. Paavonen J, Jouttunpaa K, Kangasluoma P, Aro P, Heinonen
mentous insertion of the umbilical cord and vasa previa. A PK. Velamentous insertion of the umbilical cord and vasa
report of two cases. J Reprod Med 1995;40:804–8 previa. Int J Gynaecol Obstet 1984;22:207–11
17. Young M, Yule N, Barham K. The role of light and sound 40. Pun TC, Ng JC. Vasa praevia – antepartum haemorrhage with
technologies in the detection of vasa praevia. Reprod Fertil sinusoidal fetal heart pattern. Aust NZ J Obstet Gynaecol
Dev 1991;3:439–45 1987;27:68–9
18. Fleming AD, Johnson C, Targy M. Diagnosis of vasa previa 41. Duenhoelter JH. Survival of twins after acute fetal hemor-
with ultrasound and color flow Doppler: a case report. Nebr rhage from ruptured vasa previa. Obstet Gynecol 1989;73:
Med J 1996;81:191–3 866–7
19. Harding JA, Lewis DF, Major CA, Crade M, Patel J, Nageotte 42. Rizos N, Doran TA, Mskin M, Benzie BJ, Ford JA. Natural
MP. Color flow Doppler – a useful instrument in the diagnosis history of placenta previa ascertained by diagnostic ultra-
of vasa previa. Am J Obstet Gynecol 1990;163:1566–8 sound. Am J Obstet Gynecol 1979;133:287–91
20. Hurley VA. The antenatal diagnosis of vasa praevia: the role 43. Strassmann P. Placenta praevia. Arch Gynecol 1902;67:
of ultrasound. Aust NZ J Obstet Gynaecol 1988;28:177–9 112–275
Ultrasound in Obstetrics and Gynecology 433
97/199 AMA: First Proof
Вам также может понравиться
- Natural History of Vasa Previa Across Gestation Using A Screening ProtocolДокумент7 страницNatural History of Vasa Previa Across Gestation Using A Screening ProtocolwijeОценок пока нет
- Pi Is 0849583116304554Документ7 страницPi Is 0849583116304554wijeОценок пока нет
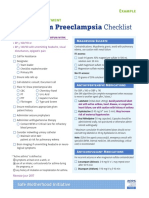
- Postpartum Preeclampsia Checklist: Emergency Department ExampleДокумент1 страницаPostpartum Preeclampsia Checklist: Emergency Department ExamplewijeОценок пока нет
- AnnMedHealthSciRes MAcrosomiaДокумент6 страницAnnMedHealthSciRes MAcrosomiawijeОценок пока нет
- Jurnal Akut Abdomen PDFДокумент8 страницJurnal Akut Abdomen PDFwijeОценок пока нет
- Good18.Prenatally Diagnosed Vasa Previa A.30Документ9 страницGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- v1 Ref Status: Indexed, Http://f1000r.es/2f8Документ5 страницv1 Ref Status: Indexed, Http://f1000r.es/2f8wijeОценок пока нет
- VASA Previa CaseДокумент3 страницыVASA Previa CasewijeОценок пока нет
- Case Vasa PreviaДокумент1 страницаCase Vasa PreviawijeОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Antepartum Haemorrhage - CTM Guideline 2020Документ20 страницAntepartum Haemorrhage - CTM Guideline 2020Kvy OngОценок пока нет
- Novia Painan Tim 4 KsДокумент17 страницNovia Painan Tim 4 KsNatasha AnditaОценок пока нет
- Health Teaching During PergnancyДокумент4 страницыHealth Teaching During PergnancyAnuradha MauryaОценок пока нет
- Obstetrics and GynaecologyДокумент31 страницаObstetrics and GynaecologyLana LocoОценок пока нет
- Antepartum HemorrhageДокумент6 страницAntepartum HemorrhageEsam EsamОценок пока нет
- Uterine Fibroids (Leiomyomas) : Issues in Pregnancy - UpToDateДокумент23 страницыUterine Fibroids (Leiomyomas) : Issues in Pregnancy - UpToDaterilla saeliputriОценок пока нет
- Seminar On AphДокумент46 страницSeminar On AphKaruna KumariОценок пока нет
- Clinical Risk Factor For Preterm BirthДокумент22 страницыClinical Risk Factor For Preterm BirthGabyBffОценок пока нет
- WNHS Og AntepartumHaemorrhageДокумент17 страницWNHS Og AntepartumHaemorrhagelydia amaliaОценок пока нет
- A Study of Maternal and Fetal Outcome in Antepartum HaemorrhageДокумент4 страницыA Study of Maternal and Fetal Outcome in Antepartum HaemorrhagechairulОценок пока нет
- OsceДокумент100 страницOsceTess WilliamsОценок пока нет
- Antepartum Haemorrhage (APH) : Prepared by Helen CookeДокумент22 страницыAntepartum Haemorrhage (APH) : Prepared by Helen CookejojolilimomoОценок пока нет
- Health Centre Stgs - Federal Government of SomaliaДокумент102 страницыHealth Centre Stgs - Federal Government of SomaliaAhmed MohamedОценок пока нет
- Obstetrics and Gynecology Question PapersДокумент22 страницыObstetrics and Gynecology Question Papersprinceej84% (19)
- Antepartum Haemorrage (APH) : Dr. Mtumweni, MDДокумент42 страницыAntepartum Haemorrage (APH) : Dr. Mtumweni, MDmarco luenaОценок пока нет
- Antepartum HemorrhageДокумент105 страницAntepartum HemorrhageBablablo LolaleОценок пока нет
- Kode Icd-10 Maternal Dan NeonatalДокумент64 страницыKode Icd-10 Maternal Dan NeonatalEndah TriОценок пока нет
- Antepartum HaemorrhageДокумент9 страницAntepartum Haemorrhageareeb khanОценок пока нет
- 1700 Questions Not in PLABABLEДокумент131 страница1700 Questions Not in PLABABLEDaniah Marwan Dawood DAWOODОценок пока нет
- Vaginalbleedinginlate Pregnancy: Janet S. Young,, Lindsey M. WhiteДокумент14 страницVaginalbleedinginlate Pregnancy: Janet S. Young,, Lindsey M. WhiteEka NataОценок пока нет
- Placenta FunctionsДокумент46 страницPlacenta Functionsvenkata sryanamala50% (2)
- LHV 2022 TestДокумент1 страницаLHV 2022 TestMuhammad AliОценок пока нет
- Placenta PreviaДокумент33 страницыPlacenta PreviamidoОценок пока нет
- Kode Icd-10 Maternal Dan NeonatalДокумент49 страницKode Icd-10 Maternal Dan NeonatalciptaningtyasОценок пока нет
- Postpartum HemorrhageДокумент30 страницPostpartum HemorrhageMusekhirОценок пока нет
- High Risk PregnancyДокумент104 страницыHigh Risk PregnancyNovelyn PuaОценок пока нет
- Abruptio PlacentaeДокумент23 страницыAbruptio PlacentaeSharoon KumarОценок пока нет
- Antepartum HaemorrhageДокумент13 страницAntepartum HaemorrhagedanielОценок пока нет
- Obs Muhs LaqsДокумент66 страницObs Muhs Laqs2n72wdwv45Оценок пока нет
- 1.antepartum HeamorrhageДокумент26 страниц1.antepartum Heamorrhagems khanОценок пока нет