Академический Документы
Профессиональный Документы
Культура Документы
Hypocalcemia in The Newborn
Загружено:
renjith0 оценок0% нашли этот документ полезным (0 голосов)
43 просмотров5 страниц1. Hypocalcemia in newborns can occur early (within 3 days of life) or late (after the first week). Early onset is usually asymptomatic and detected by screening high-risk infants like preterms and infants of diabetic mothers.
2. Calcium levels normally drop after birth before rising again by day 3 as the parathyroid gland increases PTH levels. Hypocalcemia is defined as a total calcium less than 7mg/dL or ionized calcium less than 4mg/dL.
3. Treatment depends on severity and symptoms but involves calcium supplementation either orally or by IV, monitoring for side effects like arrhythmias from rapid IV administration. Prolonged or resistant hypocal
Исходное описание:
Hypocalcemia in the Newborn
Оригинальное название
Hypocalcemia in the Newborn
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документ1. Hypocalcemia in newborns can occur early (within 3 days of life) or late (after the first week). Early onset is usually asymptomatic and detected by screening high-risk infants like preterms and infants of diabetic mothers.
2. Calcium levels normally drop after birth before rising again by day 3 as the parathyroid gland increases PTH levels. Hypocalcemia is defined as a total calcium less than 7mg/dL or ionized calcium less than 4mg/dL.
3. Treatment depends on severity and symptoms but involves calcium supplementation either orally or by IV, monitoring for side effects like arrhythmias from rapid IV administration. Prolonged or resistant hypocal
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
43 просмотров5 страницHypocalcemia in The Newborn
Загружено:
renjith1. Hypocalcemia in newborns can occur early (within 3 days of life) or late (after the first week). Early onset is usually asymptomatic and detected by screening high-risk infants like preterms and infants of diabetic mothers.
2. Calcium levels normally drop after birth before rising again by day 3 as the parathyroid gland increases PTH levels. Hypocalcemia is defined as a total calcium less than 7mg/dL or ionized calcium less than 4mg/dL.
3. Treatment depends on severity and symptoms but involves calcium supplementation either orally or by IV, monitoring for side effects like arrhythmias from rapid IV administration. Prolonged or resistant hypocal
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
Hypocalcemia in the Newborn
Hypocalcemia in the newborn period
Introduction
During the 3rd trimester, calcium is transferred from mother to the fetus by active transport. Serum calcium
in the fetus is 10-11 mg/dl at term (1-2 mg higher as compared to mother). Parathyroid hormone (PTH) and
Calcitonin (CT) do not cross the placental barrier. After delivery, calcium levels start decreasing and
reaches a nadir of 7.5-8.5 mg/dl in healthy term babies, by day 2 of life. The drop in postnatal serum calcium
may be related to the peak in calcitonin level, which occurs by 12-24 hours of age. PTH levels
increase gradually in the first 48 hours of life and normal levels of serum calcium are regained by day 3 of
life. This transition process is responsible for the increased risk of early onset hypocalcemia in high-risk
neonates.
Calcium homeostasis in newborn Body calcium exists in two major compartments; (a) Skeleton (99%) and
(b)Extracellular fluid (1%). Calcium in the extracellular fluid is present in 3 forms: (a)bound to albumin
(40%) (b) bound to anions like phosphorus, citrate, sulfate and lactate(10%) and (c) free ionized form
(50%). Ionized calcium is crucial for many biochemical processes including blood coagulation,
neuromuscular excitability, cell membrane integrity and function, and cellular enzymatic and secretory
activity. Estimation of total calcium levels is a poor substitute for measuring the ionized levels.
Definition
Hypocalcemia is defined as total serum calcium <7 mg/dl or ionized calcium < 4mg/dl.The values in mg/dl
may be converted to molar units (mmol/L) by dividing by 4.
Early onset Neonatal Hypocalcemia (ENH)
This condition is fairly common and seen within the first 3 days of life. Prematurity: Preterm babies born
at a gestation ≤32 weeks are at an increased risk of ENH in the first 3 days of postnatal life. This may be
related to premature termination of trans-placental supply, exaggeration of the postnatal drop to
hypocalcemic levels and diminished target organ responsiveness to parathyroid hormone. Infant of diabetic
mother: (gestational and insulin dependent). This may be related to increased calcium demands of a
macrosomic baby. Perinatal asphyxia: Hypocalcemia and hyperphosphatemia in this condition may be
related to renal insufficiency, metabolic acidosis and diminished parathyroid hormone secretion.
Small for gestational age is not an independent risk factor for ENH.
Screening is recommended in at-risk neonates:
1.Preterm infants (≤32 weeks)
2. Infant of diabetic mothers
3. Severe perinatal asphyxia defined as Apgar score <4 at 1 minute of age.
Screening for hypocalcemia is not needed in small for gestational age (SGA) infants unless additional risk
factors like asphyxia are present.
Time schedule for screening:
At 24 and 48 hours in high-risk babies
Clinical presentation:
1.Asymptomatic: Early onset hypocalcemia is usually asymptomatic unlike the late onset variety and is
diagnosed on routine screening.
2.Symptomatic: The symptoms are neither specific nor related to the severity of hypocalcemia. These
include jitteriness, lethargy, apnea, hypotonia, high-pitched cry,stridor, irritability and seizures
Diagnosis
1.Laboratory: Total or ionized serum calcium (total <7 mg/dL or ionized <4.0 mg/dL).
Ionized calcium is the preferred mode for diagnosis of hypocalcemia.
2.ECG: QoTc >0.2 seconds or QTc >0.45 seconds
A diagnosis of hypocalcemia based only on ECG criteria is likely to yield a high false positive rate.
Neonates suspected to have hypocalcemia by ECG criteria should have the diagnosis confirmed by
measurement of serum calcium levels.
Treatment: (1 ml of calcium gluconate (10%) gives 9 mg of elemental calcium)
1.Patients at increased risk of hypocalcemia: Preterm infants (≤32 weeks), sick infants of diabetic mothers
and those with severe perinatal asphyxia should receive 40 mg/kg/day of elemental calcium (4 ml/kg/day
of 10% calcium gluconate). Infants tolerating oral feeds may receive this calcium orally q 6 hourly. Therapy
should be continued for 3 days.
2.Patients diagnosed to have asymptomatic hypocalcemia: Infants detected to have hypocalcemia on
screening and who are otherwise asymptomatic should receive 80-mg/kg/day elemental calcium (8
ml/kg/day of 10% calcium gluconate) for 48 hours. This may be tapered to 50% dose for another 24 hours
and then discontinued. Neonates tolerating oral feeds may be treated with oral calcium (IV preparation may
be used orally).
3.Patients diagnosed to have symptomatic hypocalcemia: These patients should receive a bolus dose of 2
ml/kg/dose diluted 1:1 with 5% dextrose over 10 minutes, under cardiac monitoring. This should be
followed by a continuous IV infusion of 80-mg/kg/day elemental calcium for 48 hours. Continuous infusion
is preferred to IV bolus doses (1ml/kg/dose q 6 hourly). Calcium infusion should be dropped to 50% of the
original dose for the next 24 hours and then discontinued.
The infusion may be replaced with oral calcium therapy on the last day. Normal calcium values should be
documented at 48 hours before weaning the infusion. All categories of hypocalcemia should be treated for
at least 72 hours. Continuous infusion is preferred to IV bolus doses. Symptomatic hypocalcemia should
be treated with a continuous infusion for at least 48 hours.
Precautions and side effects
Bradycardia and arrhythmia are known side effects of bolus IV calcium administration and bolus doses of
calcium should be diluted 1:1 with 5% dextrose and given under cardiac monitoring. An umbilical venous
catheter (UVC) may be used for administration of calcium only after ensuring that the tip of the catheter is
in the inferior vena cava.Hepatic necrosis may occur if the tip of the UVC lies in a branch of the portal
vein.Umbilical artery catheter (UAC) should never be used for giving calcium injections. Accidental
injection into the UAC may result in arterial spasms and intestinal necrosis. Skin and subcutaneous tissue
necrosis may occur due to extravasation. Hence IV sites where calcium is being infused should be checked
at least q 6 hourly to monitor for extravasation and avoid subcutaneous tissue necrosis.
Prolonged or resistant hypocalcemia:
This condition should be considered in the following situations:
Symptomatic hypocalcemia unresponsive to adequate doses of calcium therapy
Infants needing calcium supplements beyond 72 hours of age
Hypocalcemia presenting at the end of the first week.
These infants should be investigated for causes of LNH (see below).
2. Late onset neonatal hypocalcemia (LNH)
This condition is rare as compared to ENH. It usually presents at the end of the first week
It is usually symptomatic in the form of neonatal tetany. The causes are listed in table 1.
Investigations
These should be considered in LNH or if the hypocalcemia does not respond to adequate
doses of calcium.
Serum magnesium: Magnesium levels <1.2 mg/dL should be treated
Serum phosphate (P): Phosphate levels are increased in renal failure, top feeding with cow’s milk
and hypoparathyroidism.
Alkaline phosphatase (ALP): ALP levels are increased in hypoparathyroidism
PTH levels: PTH is decreased in hypoparathyroidism.
Urine calcium/ creatinine ratio: Ratio >0.2 is suggestive of hypoparathyroidism
Chest x-ray: Absence of thymus is suggestive of DiGeorge syndrome
Maternal calcium, phosphate and alkaline phosphatase levels: These would be helpful in detection
of maternal vitamin D deficiency
Treatment of LNH
The treatment of LNH is specific to etiology and may in certain diseases be life-long
1. Hypomagnesemia: Symptomatic hypocalcemia unresponsive to adequate doses of IV calcium therapy is
usually due to hypomagnesemia. It may present either as ENH or later as LNH. The neonate should receive
2 doses of 0.2ml/kg of 50% MgSO4 injection, 12 hours apart, deep IM followed by a maintenance dose of
0.2 ml/kg/day of 50% MgSO4,PO, 3 days.
2. High phosphate load: These infants have hyperphosphatemia with near normal calcium levels. Exclusive
breast-feeding should be encouraged and top feeding with cow’s milk should be discontinued. Phosphate
binding gels should be avoided.
3. Hypoparathyroidism: These infants tend to be hyperphosphatemic and hypocalcemic with normal renal
functions. Elevated phosphate levels in the absence of exogenous phosphate load (cow’s milk) and presence
of normal renal functions indicates parathormone inefficiency. These neonates need supplementation with
calcium (50mg/kg/day in 3 divided doses) and 1,25(OH)2 Vitamin D3 (0.5-1 µg/day). Syrup Shelcal has
250 mg/5ml of calcium and Vitamin D3 (calcitriol) is available as 0.25 µg capsules. Therapy may be
stopped in hypocalcemia secondary to maternal hyperparathyroidism after 6 weeks.
4. Vitamin D deficiency states: These babies have hypocalcemia associated with hypophosphatemia due to
an intact parathormone response on the kidneys. They benefit from Vitamin D3 supplementation in a dose
of 30-60 ng/kg/day
References:
1. Oden J, Bourgeois M. Neonatal endocrinology. Indian J Pediatr 2000;67:217-23
2. Schwartz R, Teramo KA. Effects of diabetic pregnancy on the fetus and newborn.
Semin Perinatol 2000;24:120-35
3. Salle BL, Delvin EE, Lapillonne A, Bishop NJ, Glorieux FH. Perinatal
metabolism of vitamin D. Am J Clin Nutr 2000;71(5 suppl):1317S-24S.
4. Marx SJ. Hyperparathyroid and hypoparathyroid disorders. N Engl J Med
2000;343:1863-75
5. Mimouni F, Tsang RC. Neonatal hypocalcemia: to treat or not to treat? J Am Coll
Nutr 1994;13:408-15
6. Salle BL, Delvin E, Glorieux F, David L. Human neonatal hypocalcemia. Biol
Neonate 1990;58(suppl 1):22-31
Causes of late onset hypocalcemia
Hypomagnesemia
Increased phosphate load
Cows milk
Hypoparathyroidism
Idiopathic, transient
Hypoplasia, aplasia of parathyroid glands.
(DiGeorge’s syndrome)
Pseudohypoparathyroidism
Maternal hyperparathyroidism
Vitamin deficiency
Maternal vitamin D deficiency
Malabsorption
Maternal anticonvulsant therapy
Renal insufficiency
Hepatobiliary disease
Вам также может понравиться
- Hypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- HypocalcemiaДокумент8 страницHypocalcemiaTheresa MendoncaОценок пока нет
- Hypocalcemia - 2019 PDFДокумент12 страницHypocalcemia - 2019 PDFDeep ShahОценок пока нет
- Hypocalcemia - 2019Документ10 страницHypocalcemia - 2019Mischief ManagerОценок пока нет
- Protocol on Neonatal HypocalcemiaДокумент3 страницыProtocol on Neonatal HypocalcemiaYogeshRavalОценок пока нет
- Keto LogДокумент7 страницKeto LogKim Justin InfantadoОценок пока нет
- Government College of Nursing: JodhpurДокумент9 страницGovernment College of Nursing: JodhpurpriyankaОценок пока нет
- Anaemia in Pregnancy-MaklapДокумент34 страницыAnaemia in Pregnancy-MaklapBronson KaturkanaОценок пока нет
- Total Parenteral Nutrition in NeonatesДокумент5 страницTotal Parenteral Nutrition in NeonatesRisma WatiОценок пока нет
- HypocalcemiaДокумент12 страницHypocalcemiaKrinessa May100% (1)
- Hypocalcemia CasesДокумент4 страницыHypocalcemia CasesRahmah Shah BahaiОценок пока нет
- Calcitriol-0.25mcg Soft Gelatin CapsuleДокумент8 страницCalcitriol-0.25mcg Soft Gelatin CapsuleMd. Abdur RahmanОценок пока нет
- Summary - Midterm Review (Mother)Документ6 страницSummary - Midterm Review (Mother)Jaimie BanaagОценок пока нет
- Tatalaksana Bayi Dari Ibu Penderita Diabetes MelitusДокумент17 страницTatalaksana Bayi Dari Ibu Penderita Diabetes MelituspuspaОценок пока нет
- Anemia and Pregnancy: Sunil Kumar DahaДокумент43 страницыAnemia and Pregnancy: Sunil Kumar DahaBhawna JoshiОценок пока нет
- Calcitriol, Calcium Carbonate and Zinc Capsules Calzem CompositionДокумент5 страницCalcitriol, Calcium Carbonate and Zinc Capsules Calzem CompositionAnjali MongaОценок пока нет
- Characteristics Risks Metabolic Disorders Post Term InfantДокумент3 страницыCharacteristics Risks Metabolic Disorders Post Term Infantgeorgeloto12Оценок пока нет
- Anemia in Pregnancy: Causes, Effects and TreatmentДокумент6 страницAnemia in Pregnancy: Causes, Effects and TreatmentLeroy LoyОценок пока нет
- لقطة شاشة ٢٠٢٤-٠٢-٢٦ في ٣.٠٨.٢٩ مДокумент32 страницыلقطة شاشة ٢٠٢٤-٠٢-٢٦ في ٣.٠٨.٢٩ مali1alio11aaОценок пока нет
- C - VVV VV VVVV VVV - VVV VV - VVVV VV VVДокумент3 страницыC - VVV VV VVVV VVV - VVV VV - VVVV VV VVBea Angela Bithao AnonoyОценок пока нет
- Dr. Ramya Moderator: DR - PallaveeДокумент71 страницаDr. Ramya Moderator: DR - PallaveeMonika shankarОценок пока нет
- HypocalcemiaДокумент2 страницыHypocalcemiaRachel Frances SorillaОценок пока нет
- CYANOCOBALAMIN-cyanocobalamin Injection, S Olution Vitruvias TherapeuticsДокумент12 страницCYANOCOBALAMIN-cyanocobalamin Injection, S Olution Vitruvias TherapeuticsGreen HanauОценок пока нет
- Neonatal HypocalcemiaДокумент5 страницNeonatal HypocalcemiaLekshmi ManuОценок пока нет
- Jurnal Reading MandiriДокумент5 страницJurnal Reading MandiriRio PotterОценок пока нет
- Calcium Requirements in Hypoparathyroidism During PregnancyДокумент4 страницыCalcium Requirements in Hypoparathyroidism During PregnancyLailatul FitriОценок пока нет
- Oracal: Composition ActionДокумент4 страницыOracal: Composition ActionmohammadОценок пока нет
- Obg 2Документ150 страницObg 2PrathibhaОценок пока нет
- Management of Anaemia in PregnancyДокумент8 страницManagement of Anaemia in PregnancyAnonymous 9dVZCnTXSОценок пока нет
- Neonatal HypoglycemiaДокумент14 страницNeonatal HypoglycemiaAkankshaОценок пока нет
- Cardiavascular: - Patent Ductus ArteriosusДокумент27 страницCardiavascular: - Patent Ductus ArteriosusHadi AbdullahОценок пока нет
- Calcitriol Capsules for Bone and Kidney HealthДокумент8 страницCalcitriol Capsules for Bone and Kidney HealthsoftintОценок пока нет
- Hypocalcemia in NewbornsДокумент2 страницыHypocalcemia in NewbornsEunice Lan ArdienteОценок пока нет
- Teaching TY HaematinicsДокумент66 страницTeaching TY HaematinicssahirbuleОценок пока нет
- Calcium Carbonate Chewable Tablets SPCДокумент5 страницCalcium Carbonate Chewable Tablets SPCanand1540Оценок пока нет
- Presentation On Neonatal Hypocalcemia, Hypoglycemia, HypomagnesaemiaДокумент55 страницPresentation On Neonatal Hypocalcemia, Hypoglycemia, HypomagnesaemiaSivabarathyОценок пока нет
- Management of Pregnancy JaundiceДокумент28 страницManagement of Pregnancy JaundiceShailani Thakur100% (1)
- Endocrine Emergencies in PicuДокумент10 страницEndocrine Emergencies in PicuDr.MohanОценок пока нет
- Revesion Nelson Notes 20Документ205 страницRevesion Nelson Notes 20Hanouf BakriОценок пока нет
- 12 Neonatal Hypocalcemia, Glycemia and MagnesemiaДокумент55 страниц12 Neonatal Hypocalcemia, Glycemia and MagnesemiaRana Vandana100% (1)
- SA Anemia PregnancyДокумент10 страницSA Anemia PregnancyPujanaWiaktaОценок пока нет
- Nica 109Документ5 страницNica 109Jhanica M UlnasОценок пока нет
- Severe Acute Malnutrition - MSF Medical GuidelinesДокумент6 страницSevere Acute Malnutrition - MSF Medical GuidelinesAnas AdamuОценок пока нет
- Small Ruminant Nutritional DiseaseДокумент11 страницSmall Ruminant Nutritional DiseasePrince PrinceОценок пока нет
- Neonatal HypoglycemiaДокумент5 страницNeonatal Hypoglycemiadiana rossОценок пока нет
- Blood Group and Mechanism of IncompabilityДокумент5 страницBlood Group and Mechanism of IncompabilityshaveimernОценок пока нет
- Chapter 22.2 Organic AcidemiasДокумент3 страницыChapter 22.2 Organic Acidemiaspriyanshu mathurОценок пока нет
- Neonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualДокумент7 страницNeonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualNugraha SultanОценок пока нет
- Mendiola-Neonatal Hypoglycemia PPT 1Документ49 страницMendiola-Neonatal Hypoglycemia PPT 1Maysa IsmailОценок пока нет
- Orig 1 S 040 LBLДокумент7 страницOrig 1 S 040 LBLpatgarettОценок пока нет
- Drug Study - Potassium ChlorideДокумент6 страницDrug Study - Potassium ChlorideBalloonsRus PHОценок пока нет
- Approach To A Child Presenting With Rickets: Navoda AtapattuДокумент5 страницApproach To A Child Presenting With Rickets: Navoda AtapattuVijayakanth VijayakumarОценок пока нет
- SOGP AnaemiaДокумент16 страницSOGP AnaemiaMuhammad Farrukh ul IslamОценок пока нет
- Hypocalcemia - and HypomagnesemiaДокумент1 страницаHypocalcemia - and HypomagnesemiaHero StoreОценок пока нет
- Hypokalemic Periodic ParalysisДокумент5 страницHypokalemic Periodic ParalysisyanamatshahОценок пока нет
- Pregestational ConditionsДокумент46 страницPregestational ConditionsSheryl M. Ablao50% (2)
- Metabolism Disorders in Dairy CowsДокумент100 страницMetabolism Disorders in Dairy Cowsghazal zainОценок пока нет
- Iron Deficiency Anemia.1Документ21 страницаIron Deficiency Anemia.1Rumaisa AbdullahОценок пока нет
- PatientДокумент1 страницаPatientrenjithОценок пока нет
- HypocalcemiaДокумент1 страницаHypocalcemiarenjithОценок пока нет
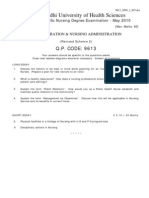
- Nursing Exam Papers from Rajiv Gandhi UniversityДокумент10 страницNursing Exam Papers from Rajiv Gandhi UniversityVantrigaru Veeresh Bangi100% (4)
- Seminar On Minor Ailments and Complications of PuerperiumДокумент74 страницыSeminar On Minor Ailments and Complications of PuerperiumKaruna Kumari89% (46)
- Hypocalcemia in The NewbornДокумент5 страницHypocalcemia in The NewbornrenjithОценок пока нет
- Uterine FibroidДокумент6 страницUterine FibroidrenjithОценок пока нет
- Command List-6Документ3 страницыCommand List-6Carlos ArbelaezОценок пока нет
- Real Estate Broker ReviewerREBLEXДокумент124 страницыReal Estate Broker ReviewerREBLEXMar100% (4)
- Applied Statics and Strength of Materials 6th Edition Ebook PDFДокумент61 страницаApplied Statics and Strength of Materials 6th Edition Ebook PDFteri.sanborn87695% (44)
- The Dominant Regime Method - Hinloopen and Nijkamp PDFДокумент20 страницThe Dominant Regime Method - Hinloopen and Nijkamp PDFLuiz Felipe GuaycuruОценок пока нет
- eHMI tool download and install guideДокумент19 страницeHMI tool download and install guideNam Vũ0% (1)
- Cableado de TermocuplasДокумент3 страницыCableado de TermocuplasRUBEN DARIO BUCHELLYОценок пока нет
- Iphoneos 31Документ159 страницIphoneos 31Ivan VeBoОценок пока нет
- Equilibruim of Forces and How Three Forces Meet at A PointДокумент32 страницыEquilibruim of Forces and How Three Forces Meet at A PointSherif Yehia Al MaraghyОценок пока нет
- Strategies For StartupДокумент16 страницStrategies For StartupRoshankumar BalasubramanianОценок пока нет
- Alternate Tuning Guide: Bill SetharesДокумент96 страницAlternate Tuning Guide: Bill SetharesPedro de CarvalhoОценок пока нет
- Role of PAOДокумент29 страницRole of PAOAjay DhokeОценок пока нет
- TJUSAMO 2013-2014 Modular ArithmeticДокумент4 страницыTJUSAMO 2013-2014 Modular ArithmeticChanthana ChongchareonОценок пока нет
- Evil Days of Luckless JohnДокумент5 страницEvil Days of Luckless JohnadikressОценок пока нет
- Speed Reducer GearboxДокумент14 страницSpeed Reducer Gearboxعبد للهОценок пока нет
- Nokia CaseДокумент28 страницNokia CaseErykah Faith PerezОценок пока нет
- Cell Organelles ColoringДокумент2 страницыCell Organelles ColoringThomas Neace-FranklinОценок пока нет
- Emergency Management of AnaphylaxisДокумент1 страницаEmergency Management of AnaphylaxisEugene SandhuОценок пока нет
- Cab&Chaissis ElectricalДокумент323 страницыCab&Chaissis Electricaltipo3331100% (13)
- Bula Defense M14 Operator's ManualДокумент32 страницыBula Defense M14 Operator's ManualmeОценок пока нет
- STS Prelim ExamДокумент2 страницыSTS Prelim ExamMychie Lynne MayugaОценок пока нет
- Marshall Stability Test AnalysisДокумент5 страницMarshall Stability Test AnalysisZick Zickry50% (2)
- Listening Exercise 1Документ1 страницаListening Exercise 1Ma. Luiggie Teresita PerezОценок пока нет
- Damcos Mas2600 Installation UsermanualДокумент26 страницDamcos Mas2600 Installation Usermanualair1111Оценок пока нет
- Technical Specification of Heat Pumps ElectroluxДокумент9 страницTechnical Specification of Heat Pumps ElectroluxAnonymous LDJnXeОценок пока нет
- Techniques in Selecting and Organizing InformationДокумент3 страницыTechniques in Selecting and Organizing InformationMylen Noel Elgincolin ManlapazОценок пока нет
- AtlasConcorde NashДокумент35 страницAtlasConcorde NashMadalinaОценок пока нет
- Form 4 Additional Mathematics Revision PatДокумент7 страницForm 4 Additional Mathematics Revision PatJiajia LauОценок пока нет
- Cot 2Документ3 страницыCot 2Kathjoy ParochaОценок пока нет
- Seminar Course Report ON Food SafetyДокумент25 страницSeminar Course Report ON Food SafetyYanОценок пока нет