Академический Документы
Профессиональный Документы
Культура Документы
Pediatric Evaluation
Загружено:
api-420919156Исходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pediatric Evaluation
Загружено:
api-420919156Авторское право:
Доступные форматы
OCCUPATIONAL THERAPY EVALUATION REPORT
CONFIDENTIAL
NAME “XXX”
DATE OF BIRTH XXX X, XXXX
AGE 3 years 8 months
EVALUATION DATE October 3, 2017
REASON FOR Sensory, Behavior
REFERRAL
MEDICATION(S) None – Vitamins
Allergies None
Diagnosis wNone
Occupational Profile
v Client Report: Background and History
wHealth status & XXX is a 3 year, 8 month old boy that was self-referred to the Life Skills
medical history Clinic by his mother for evaluation and treatment of sensory and
wCurrent concerns behavior issues. XXX is a strong and healthy boy with a very active life
related to preference. XXX has had his adenoids removed due to them interfering
engagement in daily with breathing while sleeping. XXX’s mother reports concerns about
life activities XXX being too strong and often uses that strength to lash out at others
when aggravated. In addition, mother reports that XXX does not know
how to interact with others and play well with others while in daycare.
XXX’s mother would like to see improvement with behavioral
regulation, self-regulation strategies, and peer interaction.
wOccupations/Activities XXX is very coordinated and accomplishes motor tasks well. XXX is
where they are very interested in his environment and enjoys elements that are going
successful on around him. He is very successful in hard work activities. XXX is
wBarriers affecting very strong and likes to use it in his activities. XXX enjoys taking toys
success taking things apart due to his curiosity. XXX enjoys cars, music,
dancing, and animals - especially horses. He participates in activities
and occupations well when one-on-one basis is provided; however
other classmates or individuals interrupting can cause a barrier to his
success. When being interrupted, XXX often lashes out, hits,
scratches, or bites. In addition, he knows his limits when it comes to
sensory stimuli; however, his response to these stimuli are affecting
participation in a variety of activities.
wPersonal/Family XXX’s mom and dad enjoy the outdoors and sharing these types of
interests & values experiences with XXX. Education is important to the family. Most
importantly, mother wants XXX to be a well-rounded child. The family
values social interaction and relationships. They want XXX to get along
well with others.
wOccupational History XXX was born in Ethiopia and abandoned at a young age. A farmer
& Life experiences found him and raised him for a short time before giving him to an
orphanage. XXX was adopted at 18 months old by the XXX family. Due
to XXX’s unknown past, birth date is an approximation of the doctor’s
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
examination. Developmental milestones prior to 18 months are
unknown. He did not meet all milestones at the age of 18 months. At 24
months, an occupational therapy evaluation was completed; however,
he did not qualify for services. XXX currently attends preschool at
Bright Horizons. Today was his first day at Bright Horizons. Prior to
Bright Horizons, XXX attended daycare and preschool at a different
daycare but was removed due to aggressive behavior toward
classmates.
w Performance patterns XXX’s daily routine is consistent on most days. His morning routine
of engagement (i.e. involves waking up, dressing for the day, and breakfast before school.
routines, roles & His school routine consists of a variety of activities and nap time. XXX
habits) does not take naps which often interferes with the class’ routine. Once
picked up in the afternoon, the afternoon consists of playing outside
and indoors, dinner, bath (if needed), story time, and bed. When
parents are engaging in house management, XXX enjoys helping with
sweeping and washing windows. When the typical routine is broken;
XXX does not respond well, as he struggles with transitioning.
XXX has a role of a son.
XXX will be raised in the cultural rituals of his adopted family.
vClient environmental factors
Supports Barriers
wPhysical (e.g. furniture, A safe and consistent home is Bed. This is the location where
pets) provided for XXX. he most often engages in head
Environment
banging.
XXX lacks the abilities to properly
initiate contact.
wSocial (e.g. parents, XXX has a few close friends and XXX struggles with the ability to
spouse, friends, supportive parents. work in social groups.
caregivers) XXX is starting a new preschool.
wCultural (e.g. customs, Parents believe that their child XXX will not learn the customs
beliefs) should be raised to be well and beliefs of the culture in that
rounded for all areas of life. which he was born.
XXX will not be raised within the
culture he was born.
wPersonal (e.g. age, Young, able to develop new skills XXX has been removed from a
gender, SES, education) and adaptive behaviors and previous daycare due to
Context
further increase his aggressive behaviors toward
independence. peers.
wTemporal (e.g. stage of XXX is still developing, which XXX has had multiple traumatic
life, time, year) means neuroplasticity is easier experiences up until the age of
and will assist in developing the 18 months.
proper social skills he needs.
XXX is also beginning a new
preschool.
wvirtual (e.g. chat, email, N/A N/A
remote monitoring)
vClient Goals and Priorities
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
COPM: Canadian Occupational Performance Measure
XXX’ mother completed the Canadian Occupational Performance Measure (COPM), which is an
assessment that identifies top priorities for goals and outcomes as well as the perception of the current
performance, and performance over time in each specified area. The following items were indicated as
highest areas of concern (in order of most important to least important):
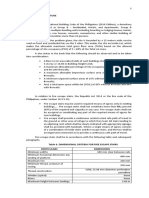
OCCUPATIONAL Impt PERFORMANCE SATISFACTION
PERFORMANCE PRIORITIES (On a scale of 1-10; 1=not (On a scale of 1-10; 1=not
performing, 10=performing satisfied, 10=highly
independently) satisfied)
Socialization – Aggressive Behavior 1 1
Socialization – Initiating Contact 1 1
Play/Education - Transitioning 1 1
Rest and Sleep - Head Banging 3 3
TOTAL 6 6
Average Scores 1.5 1.5
OCCUPATIONAL PERFORMANCE ANALYSIS:
XXX was accompanied to this evaluation by both his mother. The evaluation was conducted in quiet,
relatively distraction-free treatment rooms of the Life Skills Clinic. Standardized and non-standardized
clinical observations of various structured and unstructured fine and gross motor activities, as well as
review of medical charts were used to assess overall abilities and limitations. The following is a summary
of evaluation results.
ASSESSMENTS:
INFORMAL CLINICAL OBSERVATION EVALUATION:
(All Items/sections may or may not be applicable)
CHILD’S MODE OF COMMUNICATION
Verbal
Gestural (pointing, waving, moving body to, etc.)
Other/Additional Comments (echolalic speech; few word phrases; receptive/expressive language;
follows single/mutli-step directions, etc.):
SELF-CARE SKILLS
Dressing Independent Requires Assistance: Min A w/shirt – Dependent/shoes &socks
Toileting Independent Requires Assistance: With wiping with bowel movement
Grooming/Hygiene Independent Requires Assistance: Brushing teeth, combing hair.
Self-care Mother reports that XXX can take on and off his pants and underwear I. For his
observations and shirt, she just help hold the sleeves and he can put it on the rest of the way (Min
additional A). XXX is dependent on socks and shoes.
comments There was a time when XXX did not tolerate changing clothes, mother reports
that this has improved and no longer seems to be an issue. XXX does not enjoy
brushing his hair. Brushing teeth is a struggle but progressing.
FEEDING –
Self-Feeding Independent Requires Assistance:
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
Spoon Use Independent Requires Assistance:
Fork Use Independent Requires Assistance:
Picky Eater? Yes No
If yes, preferred foods/brands/textures:
If yes, foods/brands/textures avoided:
Feeding Food insecurities were present for a while. If food was not on the table when XXX
observations and walked in the room he would panic.
additional Mom reports no concerns related to feeding at this time.
comments
FORMAL ASSESSMENTS:
Sensory Profile-2
The Sensory Profile 2, was administered as a part of a comprehensive assessment to determine whether
aspects of sensory processing might be contributing to performance challenges in daily life of XXX.
XXX’s mom completed the Sensory Profile Caregiver Questionnaire. The Sensory Profile is an 86 item
questionnaire designed to build a picture of a child’s sensory functioning throughout the day. Items are
rated on a 5-point scale, from “almost always” to “almost never”, and scores are compared to same age
peers. XXX’s scores are as follows:
Quadrants
Just Like the Much More Than
Raw Score Total More Than Others
Majority of Others Others
Seeking/Seeker 59/95 X
Avoiding/Avoider 69/100 X
Sensitivity/Sensor 42/95 X
Registration/
42/110 X
Bystander
Sensory Sections
Auditory 16/40 X
Visual 18/30 X
Touch 26/55 X
Movement 19/40 X
Body Position 18/40
Oral 18/50 X
Behavioral Sections
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
Conduct 33/45 X
Social Emotional 47/70 X
Attentional 27/50 X
XXX obtained scores that indicate typical performance in the following sections:
• Auditory Processing
• Oral Sensory Processing
Typical performance within these areas indicate that XXX is using his sensory
inputs successfully. XXX is able to satisfactorily use auditory processing in order
to appropriately interact with what is going on around him. In addition, XXX is
able to use oral sensory to gather information from his mouth.
XXX obtained scores above the typical average (more than others) in the
following sections:
• Visual Processing
• Touch Processing
• Movement Processing
• Body Positioning Processing
XXX may find these areas difficult to meaningfully use this type of sensory
information. XXX visually becomes involved with everything going on around him,
losing focus on the task at hand as seen through observation.
XXX obtained scores above the typical average (more than others) in the
following section:
• Attentional Behavior
Interpretation of XXX may have difficulties with attentional behavior due to him always wanting to
Sensory Profile know what is going on around him.
XXX demonstrates difficulty (much more than others) in the following sections:
• Conduct
• Emotional Behavior
XXX score in Emotional Behavior indicates that he may become frustrated or
upset easily. His emotional responses may be due to his attempt to
overwhelming sensory input. In addition, his Conduct score indicates that he
struggles to meet other’s expectations.
Within the Quadrants, XXX obtained scores that indicate typical performance in
the following section:
• Sensitivity
• Registration
Typical performance in these areas indicate that XXX is detecting sensory and
registering those senses successfully.
XXX obtained a score in Seeking above the typical average (more than others).
This means that XXX often seeks out more sensory input than other typical
children his ages. This indicates that XXX has a high threshold for sensory
information.
Lastly, XXX scored much more than others in Avoiding. Children with Avoiding
patterns often are bothered much more than other children to stimuli. XXX’s
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
score indicates that he struggles with the need to control the amount and type of
sensations available to him at any time. This indicates that XXX has a low
threshold for sensory information.
When considering XXX’s scores in Seeking and Avoiding, his scores seem
contradictory. Looking more in depth into the assessment, results demonstrate
that XXX tends to seek out movements. XXX has a high threshold to movement,
indicating that he needs more input in order to receive input with this sensory
section. In terms of Avoiding, XXX’s scores indicate that he avoids social
interactions. XXX has a low threshold to social interactions, indicating that he has
a difficulty time regulating sensory stimuli associated to verbal and physical
interaction with others.
Comments
Performance Summary & Analysis:
Performance Deficits
Physical, cognitive and/or Activity Limitations and/or participation restrictions
psychosocial skill deficits resulting from deficits
Emotional Regulation XXX in unable to successfully participate in school with his
peers because he cannot regulate his emotions. Instead of
communicating, he often acts out through aggression by hitting,
scratching, or biting.
Initiating Contact When XXX wants to play with new friends he often goes up and
hits them because he does not understand how to appropriately
initiate contact. This is interfering with him developing
friendships.
Transitioning XXX is unable to transition between activities in school without
acting out.
Social Interaction Skills Overall, XXX lacks the skills needed in order to participate in
activities with peers and develop appropriate relationships.
Treatment Options:
1. Sensory Integration, modulation and processing techniques & strategies to facilitate
attention to task, motor coordination & planning, and self -regulation skills to promote
independence and participation with play, mobility, self-care, education and social
participation.
2. Behavior Acquisitional, facilitated learning and developmental sequencing techniques &
strategies to facilitate sequential task and motivational skills to promote independence and
participation with play, mobility, self-care, education and social participation
3. Social Participation, create positive interactions and establish routine to encourage habits of
social interaction and improve relationships & teach self-regulation of emotions to show
social behaviors appropriately to promote independence and participation with play, self-care,
education and social participation.
Summary:
A comprehensive evaluation using standardized and non-standardized clinical observations of
various structured and unstructured fine and gross motor activities resulted in XXX demonstrating
performance deficits with sensory processing, social skills, and self-regulation limiting his ability to
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
participate and function independently in age appropriate social and self-care activities at home and
school. Moderate task and environmental adaptations were required, such as visual timer and verbal
prompts, in order to effectively complete evaluation tasks and activities. XXX demonstrates age
appropriate fine and gross motor skills.
Recommendations (POC):
Occupational therapy services are recommended 1x/ week for 6 months in order to achieve the following
goals and objectives.
Goals:
1. Within 6 months, XXX will demonstrate improved regulation of behaviors through expressing
emotion, acknowledgement, and speaking clearly in order to socially interact with peers at
preschool with Mod A from teacher through self-regulation strategies in 4/5 data collection days.
2. Within 6 months, XXX will independently demonstrate improved initiation of contact and
emotional regulation in order to display no more than one aggressive behaviors toward a peer
when being approached by the peer when he is interacting with a teacher in 4/5 data collection
days.
3. Within 6 months, XXX will improve emotional regulation in order to independently transition
between school activities with no emotional outbursts through use of a visual timer in 4/5 data
collection days.
4. Within 6 months, mom will self-report that XXX demonstrates improved emotional regulation in
order to decrease head banging 80% of the time with Min A and use of proper adaptive sensory
strategies in 4/5 data collection days.
Assessment Completed By: , OTS
Assessment Reviewed By: Dr.
Division of Occupational Therapy’s LIFE SKILLS CLINIC
540 Arapeen Drive Suite 200
Main Clinic Number 801-585-6837—FAX 801-585-6813—
www.LifeSkillsClinic@utah.edu
Вам также может понравиться
- Raising Kids With Sensory Processing Disorders: A Week-by-Week Guide to Helping Your Out-of-Sync Child With Sensory and Self-Regulation IssuesОт EverandRaising Kids With Sensory Processing Disorders: A Week-by-Week Guide to Helping Your Out-of-Sync Child With Sensory and Self-Regulation IssuesОценок пока нет
- Occupational Therapy Goals and Obj BankДокумент16 страницOccupational Therapy Goals and Obj Bankadelitaperez94% (18)
- Category Ot Goals.Документ11 страницCategory Ot Goals.adelitaperez100% (3)
- Pediatric Treatment PlanДокумент11 страницPediatric Treatment PlanKayla Jensen100% (1)
- Template Evaluation Report For Sensory Profile Data1Документ4 страницыTemplate Evaluation Report For Sensory Profile Data1Sarah Levoy80% (10)
- Occupational Therapy Ia Sample ReportsДокумент11 страницOccupational Therapy Ia Sample Reportssneha duttaОценок пока нет
- Sensory Profile School Companion 2Документ2 страницыSensory Profile School Companion 2Calvin Lester M. Leorna75% (4)
- Functional Intervention Occupational Therapy Kit DescriptionДокумент3 страницыFunctional Intervention Occupational Therapy Kit Descriptionapi-404615775Оценок пока нет
- Ot Goals NuevoДокумент157 страницOt Goals NuevoElbania PerezОценок пока нет
- Double Time Docs Sample Evaluation OT SchoolДокумент10 страницDouble Time Docs Sample Evaluation OT SchoolAlyssa Balverde100% (1)
- Ot Guidelines Child SpecificДокумент34 страницыOt Guidelines Child Specific健康生活園Healthy Life Garden100% (1)
- Occupational Therapy AssessmentДокумент3 страницыOccupational Therapy AssessmentEllySaleh100% (1)
- Occupational Therapy Evaluation Report and Initial Intervention PlanДокумент12 страницOccupational Therapy Evaluation Report and Initial Intervention Planapi-488383880100% (1)
- Occupational Therapy - Adolescence and Executive SkillsДокумент3 страницыOccupational Therapy - Adolescence and Executive SkillsAnnbe BarteОценок пока нет
- SensoryProfile2 CaseStudy PDFДокумент4 страницыSensoryProfile2 CaseStudy PDFEvelina LamsodieneОценок пока нет
- School Companion Sample ReportДокумент15 страницSchool Companion Sample ReportCarolina Recio100% (11)
- OT Services in Classroom PresentationДокумент46 страницOT Services in Classroom PresentationHusainiОценок пока нет
- Ot Assessment Template - SelpaДокумент5 страницOt Assessment Template - Selpaapi-417867603100% (1)
- Sensory Diet DocumentsДокумент7 страницSensory Diet Documentspratibhaumrariya100% (1)
- Goals Editable PDFДокумент140 страницGoals Editable PDFManuel Ascanio67% (3)
- Occupational-Therapy ICD 10Документ2 страницыOccupational-Therapy ICD 10Amaliyah67% (3)
- CO OP AOTA - July - 2020Документ10 страницCO OP AOTA - July - 2020Ana Claudia GomesОценок пока нет
- Sample OT Reports Adult AllДокумент22 страницыSample OT Reports Adult AllDanielle Stella N'Luca50% (2)
- Sensory DietДокумент11 страницSensory Dietbarbarasanjose100% (7)
- OT Practice FrameworkДокумент12 страницOT Practice Frameworkenrico_aguila100% (2)
- Updated Activity Analysis Using The Occupational Therapy Practice Framework IIIДокумент49 страницUpdated Activity Analysis Using The Occupational Therapy Practice Framework IIIIan Russ Bautista100% (2)
- PEDI CAT Manual 1 3 6 PDFДокумент162 страницыPEDI CAT Manual 1 3 6 PDFSari Nm100% (2)
- Executive Function Occupational Therapy SkillsДокумент3 страницыExecutive Function Occupational Therapy SkillsRachel100% (10)
- OYH Assessment ManualДокумент53 страницыOYH Assessment ManualLizPattison9275% (12)
- Pediatric Occupational TherapyДокумент13 страницPediatric Occupational TherapyGeetha Priya Setty100% (3)
- Occupational Therapy Assessments Quick TableДокумент5 страницOccupational Therapy Assessments Quick Tableredsmartie100% (3)
- BOT-2 Complete Form Sample ReportДокумент12 страницBOT-2 Complete Form Sample Reportkonna4539100% (3)
- Sensory Profile: Submitted By-Amandeep Kaur M.O.T-Neuro, Sem 3 ENROLLMENT NO - A138141620004 Guided by - Ruby Ma'AmДокумент42 страницыSensory Profile: Submitted By-Amandeep Kaur M.O.T-Neuro, Sem 3 ENROLLMENT NO - A138141620004 Guided by - Ruby Ma'Amamandeep kaurОценок пока нет
- School Function AssessmentДокумент8 страницSchool Function AssessmentPaulina Vergara67% (3)
- OT Theories (In A Nutshell)Документ8 страницOT Theories (In A Nutshell)TaraJane House100% (1)
- Occupational Therapy Resource Pack For School Aged ChildrenДокумент66 страницOccupational Therapy Resource Pack For School Aged ChildrenDamayanti ThapaОценок пока нет
- Copm PDFДокумент4 страницыCopm PDFAlina Zagorodniuc100% (4)
- Student Treatment Session Soap 8Документ9 страницStudent Treatment Session Soap 8api-340625860100% (1)
- GMFMscoresheetДокумент6 страницGMFMscoresheetAbdur RasyidОценок пока нет
- Short Sensory: ProfileДокумент2 страницыShort Sensory: Profilediyanr_275% (4)
- Fine Motor and Handwriting Skills ActivitiesДокумент4 страницыFine Motor and Handwriting Skills Activitiesehopkins5_209Оценок пока нет
- Occupational Therapy in Neonatal Services and Early Intervention PDFДокумент152 страницыOccupational Therapy in Neonatal Services and Early Intervention PDFLauren100% (1)
- Caregiver Sensory ProfileДокумент6 страницCaregiver Sensory ProfileRomysah Farooq100% (1)
- Living With An Autism Spectrum Disorder (ASD) : The High School YearsДокумент2 страницыLiving With An Autism Spectrum Disorder (ASD) : The High School YearsThe American Occupational Therapy AssociationОценок пока нет
- Occupational Therapy Manual For The EASA ModelДокумент48 страницOccupational Therapy Manual For The EASA Modellolocy L100% (2)
- Sensory Profile Sample ReportДокумент22 страницыSensory Profile Sample ReportCarolina Recio100% (2)
- Occupational TherapyДокумент373 страницыOccupational TherapyInnova TO95% (19)
- Wilbarger ProtocolДокумент7 страницWilbarger Protocolcharisseleyba67% (3)
- Occupational Profile & Intervention PlanДокумент19 страницOccupational Profile & Intervention Planapi-262531856100% (1)
- Occupational Therapy Using A Sensory Integration-Based Approach With Adult PopulationsДокумент2 страницыOccupational Therapy Using A Sensory Integration-Based Approach With Adult PopulationsThe American Occupational Therapy Association75% (4)
- M-FUN Assessment ReviewДокумент4 страницыM-FUN Assessment ReviewKishan RamtohulОценок пока нет
- CO-OP PediatriaДокумент17 страницCO-OP PediatriaCarol Alvarado100% (2)
- VMIpdfДокумент6 страницVMIpdfRidwan HadiputraОценок пока нет
- Building Blocks for Learning Occupational Therapy Approaches: Practical Strategies for the Inclusion of Special Needs in Primary SchoolОт EverandBuilding Blocks for Learning Occupational Therapy Approaches: Practical Strategies for the Inclusion of Special Needs in Primary SchoolОценок пока нет
- Occupational Therapy Handbook: Practice Education, TheОт EverandOccupational Therapy Handbook: Practice Education, TheРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Senior Occupational Therapist: Passbooks Study GuideОт EverandSenior Occupational Therapist: Passbooks Study GuideОценок пока нет
- Morocco FinalДокумент87 страницMorocco Finalapi-420919156Оценок пока нет
- LW Reflective DiaryДокумент4 страницыLW Reflective Diaryapi-420919156Оценок пока нет
- CC DischargeДокумент4 страницыCC Dischargeapi-420919156Оценок пока нет
- Pediatric SpaДокумент11 страницPediatric Spaapi-420919156100% (2)
- Jurong Junior College: Preliminary Examination 2009Документ16 страницJurong Junior College: Preliminary Examination 2009cjcsucksОценок пока нет
- Civil & Structural Designer'S Data Pack: Section 7: MasonryДокумент5 страницCivil & Structural Designer'S Data Pack: Section 7: MasonryMirea Florentin0% (1)
- Vishay Load Cell Calibration System - ENДокумент3 страницыVishay Load Cell Calibration System - ENSarhan NazarovОценок пока нет
- 3949-Article Text-8633-1-10-20180712Документ10 страниц3949-Article Text-8633-1-10-20180712Volodymyr TarnavskyyОценок пока нет
- Briefing Evaluation: Yes / No High / Low Yes / No High / Low Good / Inferior Yes / NoДокумент4 страницыBriefing Evaluation: Yes / No High / Low Yes / No High / Low Good / Inferior Yes / NoAmmarah AzharОценок пока нет
- Normal DistributionДокумент23 страницыNormal Distributionlemuel sardualОценок пока нет
- Transient Thermal Conduction ExampleДокумент14 страницTransient Thermal Conduction ExampleDevendra BangarОценок пока нет
- Data Structures and Algorithms AssignmentДокумент25 страницData Structures and Algorithms Assignmentعلی احمد100% (1)
- Dossat PrinciplesOfRefrigerationДокумент554 страницыDossat PrinciplesOfRefrigerationHernan CobaОценок пока нет
- 1.1. CHILLER 1.2. Centrifugal: 5.2.hrizontalДокумент2 страницы1.1. CHILLER 1.2. Centrifugal: 5.2.hrizontalShah ArafatОценок пока нет
- 33392-01 Finegayan Water Tank KORANDO PDFДокумент3 страницы33392-01 Finegayan Water Tank KORANDO PDFShady RainОценок пока нет
- Hydrology: Dua'a Telfah PH.D, Civil Engineering Department Jadara UniversityДокумент104 страницыHydrology: Dua'a Telfah PH.D, Civil Engineering Department Jadara UniversityFaris AlmomaniОценок пока нет
- ACFrOgDVly789-6Z8jIbi7pBoLupubEgMyOp7PczEvUguHoW3uj oR2PKzDvuhRzzkIhacYjxXRrU6iA7sHt t6MhtpZFq0t uZL2pF5Ra NNZ kmcl5w7BCQeUegKhjRhNuou88XxLodzWwbsrДокумент14 страницACFrOgDVly789-6Z8jIbi7pBoLupubEgMyOp7PczEvUguHoW3uj oR2PKzDvuhRzzkIhacYjxXRrU6iA7sHt t6MhtpZFq0t uZL2pF5Ra NNZ kmcl5w7BCQeUegKhjRhNuou88XxLodzWwbsrJohn Steven LlorcaОценок пока нет
- Discussion 2: OOA: Case Study Robot in MazeДокумент17 страницDiscussion 2: OOA: Case Study Robot in MazeArmmetОценок пока нет
- Dynamic Analysis of Synchronous Reluctance Motor Drives Based On Simulink and Finite Element ModelДокумент5 страницDynamic Analysis of Synchronous Reluctance Motor Drives Based On Simulink and Finite Element ModelenmnabilОценок пока нет
- Load Dwe Eigh Ing D Devi Ice: For R Elev Vators SДокумент28 страницLoad Dwe Eigh Ing D Devi Ice: For R Elev Vators SNaren AnandОценок пока нет
- Layers of The EarthДокумент26 страницLayers of The EarthLoo DrBrad100% (1)
- Employment Under Dubai Electricity & Water AuthorityДокумент6 страницEmployment Under Dubai Electricity & Water AuthorityMominur Rahman ShohagОценок пока нет
- Investigation: Present By:Shivam Ranabhat Project Title: Esport Players Recruit SystemДокумент18 страницInvestigation: Present By:Shivam Ranabhat Project Title: Esport Players Recruit Systemjames chhetriОценок пока нет
- Getting Started in Steady StateДокумент24 страницыGetting Started in Steady StateamitОценок пока нет
- Imarest 2021 Warship Development 1997Документ43 страницыImarest 2021 Warship Development 1997nugrohoОценок пока нет
- Recruitment and SelectionДокумент50 страницRecruitment and SelectionAmrita BhatОценок пока нет
- DESBLOQUEADO Synesis Erik Hollnagel 2022Документ81 страницаDESBLOQUEADO Synesis Erik Hollnagel 2022Tribu de SSOОценок пока нет
- Pism Pub Line Up - Jul-Dec - 2022Документ1 страницаPism Pub Line Up - Jul-Dec - 2022Yus CeballosОценок пока нет
- Embargoed: Embargoed Until April 24, 2019 at 12:01 A.M. (Eastern Time)Документ167 страницEmbargoed: Embargoed Until April 24, 2019 at 12:01 A.M. (Eastern Time)Las Vegas Review-JournalОценок пока нет
- Comparison of Plate Count Agar and R2A Medium For Enumeration of Heterotrophic Bacteria in Natural Mineral WaterДокумент4 страницыComparison of Plate Count Agar and R2A Medium For Enumeration of Heterotrophic Bacteria in Natural Mineral WaterSurendar KesavanОценок пока нет
- C1 L2D Quadratic FormulaДокумент3 страницыC1 L2D Quadratic FormulaJo-Amver Valera ManzanoОценок пока нет
- FC Exercises3Документ16 страницFC Exercises3Supertj666Оценок пока нет
- 01 Gyramatic-Operator Manual V2-4-1Документ30 страниц01 Gyramatic-Operator Manual V2-4-1gytoman100% (2)
- A Research Paper On DormitoriesДокумент5 страницA Research Paper On DormitoriesNicholas Ivy EscaloОценок пока нет