Академический Документы
Профессиональный Документы
Культура Документы
Enucleation Surgery-Orbital Implants and Surgical Techniques - 1
Загружено:
Satria Adi MarhendraИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Enucleation Surgery-Orbital Implants and Surgical Techniques - 1
Загружено:
Satria Adi MarhendraАвторское право:
Доступные форматы
Enucleation
Enucleation Surgery—Orbital Implants and Surgical Techniques
Yacoub A Yousef
Department of Surgery, King Hussein Cancer Center, Amman, Jordan
DOI: http://doi.org/10.17925/USOR.2016.09.01.46
Abstract
Enucleation consists of surgical removal of the entire eye globe with preservation of the conjunctiva, extraocular muscles, orbital fat, and optic
nerve. This surgical procedure is generally accepted treatment for intraocular malignancies, blind painful eye, severely traumatized eye, phthisis
bulbi, and to improve cosmetic appearance. Once the eye is removed, orbital volume enhancement typically requires implantation of spherical
materials that can be classified into two major groups: non-porous and porous orbital implants. Different surgical techniques have been
described in the literature, including muscle imbrication technique and the myoconjunctival enucleation technique (both with a non-integrated
implant) and the more recent integrated orbital implants technique that results in less implant-migration and improved prosthesis movement.
In this review, we discuss indications, orbital implant choices and the main enucleation surgical techniques reported in the literature.
Keywords
Enucleation, porous orbital implant, rectus muscle, tumor
Disclosure: Yacoub A Youssef has nothing to declare in relation to this article. No funding was received in the publication of this article.
Open Access: This article is published under the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, adaptation, and
reproduction provided the original author(s) and source are given appropriate credit.
Received: February 9, 2016 Accepted: February 17, 2016 Citation: US Ophthalmic Review, 2016;9(1):46–8
Correspondence: Yacoub A Yousef, Consultant Ocular Oncologist, King Hussein Cancer Centre, Queen Rania Street, PO Box 1269 Al-Jubeiha, Amman 11941 Jordan.
E: yyousef@khcc.jo
Enucleation, or surgical removal of the entire eye globe, was described Types of Implants and Enucleation
by Bartisch in 1583, and was described in combination with orbital Surgical Techniques
volume replacement (implant) by Mules in 1585.1–3 In the US, trauma is the In the modern era, several types of orbital implants are available for
leading indication for enucleation (40.9% of cases), followed by tumors volume replacement after removal of the eye. They can be classified
(28% of cases).4,5 Other indications include painful blind eye, phthisis into two major groups: non-integrated orbital implants (primarily
with degeneration, congenital anophthalmia, severe microphthalmia, polymethylmethacrylate [PMMA]) and integrated porous orbital implants
unresponsive endophthalmitis, and for improvement of cosmesis (typically plastic, bone, or coral).18–24 The difference between these two
in a blind eye.4 major groups is that integrated implants allow fibrovascular invasion or
incorporation into the living orbit. Graue and Finger demonstrated that on
Various materials may be used to create orbital implants, including positron emission tomography (PET)/computed tomography (CT) imaging,
cartilage, bone, fat, gold, silver, cork, rubber, aluminum, ivory, silk, porous orbital implants absorb 18-fluorodeoxyglucose contrast, indicating
wool, petroleum jelly, acrylics, silicone, glass, titanium, quartz, and metabolic activity within the implanted device.25 That fibrovascular
porous materials such as hydroxyapatite (HA) and polyethylene.6–15 invasion does not occur with non-integrated implants.
Unfortunately, however, several reports describe the associated
complications of using such materials, such as exposure, displacement, Surgical Techniques
extrusion, and orbital infection.7,14,16 Enucleation surgery is usually done under general anesthesia. First, the
surgeon resects the conjunctiva from the surgical limbus (periotomy),
The orbital implant and overlying prosthesis work together to allow followed by dissection of the Tenon’s capsule (tenotomy). Then the four
excellent overall cosmesis and eye movement after enucleation. Most recti muscles (with or without the two oblique muscles) need to be
patients are pleased with the result and few require secondary cosmetic isolated, tied by 6–0 absorbable suture, followed by muscle resection
surgery. After healing, the appearance of the anophthalmic patient’s from the insertion, and homeostasis. Then the eye globe should be
affected eye should be similar in all aspects to their other, normal eye.17 pulled anteriorly (either from the stump of the medial rectus, assisted
Herein, we briefly review the main types of orbital implants, and the main by cryotherapy, or by sutures at the limbus from two sites), followed by
enucleation surgical techniques reported in the literature. resection of the optic nerve (the length should be 8–12 mm in cases of
TOU CH ME D ICA L ME D IA
46
Yousef_FINAL.indd 46 30/03/2016 23:23
Enucleation Surgery—Orbital Implants and Surgical Techniques
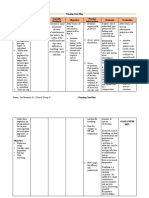
Table 1: The Differences Between the Three Main Enucleation Surgical Techniques
Imbrication Technique20,24,26 Integrated Implant Technique12–15,27,28 Mycoconjunctival Technique29,30
Type of implant Non-integrated Integrated (porous) Non-integrated
Implant material (commonly used) PMMA or silicone Hydroxyapatite or polyethylene PMMA
Need for mesh around the implant No Yes No
Repositioning the rectus muscles Superior rectus imbricated with inferior Muscles directly sutured to the scleral Recti muscles sutured just short of the
rectus, and medial rectus imbricated with cap or the mesh around the implant in respective fornices with sutures passing
lateral rectus a location corresponding to muscle through the anterior Tenon’s-conjunctival
insertion complex
Repositioning the oblique muscles No Yes No
Postoperative care Eye patch for 2–5 days and prophylactic systemic and topical antibiotics for 2 weeks
Main complications Implant displacement and extrusion Persistent infection, and implant exposure Implant extrusion
Cost Cheap Expensive Cheap
PMMA = polymethylmethacrylate.
retinoblastoma). Then a plastic or metallic dummy implant can be used and conjunctiva, the mechanical efficiency of transmission of movement
to check the best size for the orbital implant (i.e. the maximum size that from the implant to the prosthesis is suboptimal. In addition to that,
fills the orbit and allows adequate suturing of the anterior layers without imbrication of the recti over the smooth surface of nonintegrated implants
tension). Once the required size is identified, the selected implant should can result in implant displacement and migration.12–15
be inserted deep in the socket (with or without implant injector), and
deeper than the posterior Tenon’s layer. Table 1 illustrates the differences Integrated porous implants have been used for more than two decades
between the three main enucleation surgical techniques. now and they provide better implant movement than the traditional
non-integrated implants because of direct attachment of extraocular
After fixation of the implant in the correct site and attachment of the muscles to the implant,33 and they are associated with less migration
muscles according to technique, the posterior and anterior parts of and extrusion.5,33 Custer et al.34 reported that there was no difference in
the Tenon’s capsule will be sutured by absorbable interrupted sutures implant movement when sclera-wrapped non-integrated implants and
(5–0 or 6–0) separately, followed by closure of the conjunctiva by running sclera-wrapped integrated implants were compared, thus indicating that
6–0 absorbable suture. In the case of the myoconjunctival technique, then the implant material itself may not have a bearing on implant movement,
the exteriorized muscle sutures are tied onto the conjunctival surface and as long as the muscles are attached directly or indirectly to the implant.
the suture knot left exposed. Although the porous implants have been reported to offer improved
implant movement,35 these are more expensive and intrusive, requiring
To maintain the fornices and to prepare them for prosthesis fitting wrapping, and also are prone to implant exposure.33
(usually six weeks after enucleation), a conformer of adequate size
(small, medium, or large) needs to be inserted anterior to the sutured The cosmetic appearance of the prosthesis36,37 and implant migration and
conjunctiva, with topical antibiotic and tight patching of the eye for two to extrusion37,38 are subjective outcome measures, while implant and prosthesis
five days. An alternative to the conformer is immediate painted prosthesis movement are objective, and hence were used as the primary outcome
insertion at the time of the surgery, or early prosthesis insertion at the measure in a randomized controlled trial by Shome et al.,30 who compared
time of patch removal, to allow for cosmetic rehabilitation and improved the differences in implant and prosthetic movement after myoconjunctival
quality of life. This prosthesis may need to be replaced by a custom-made enucleation (with non-integrated PMMA implant) with those of two other
one after six weeks.31,32 standard techniques: the traditional muscle imbrication technique (with
non-integrated PMMA implant) and enucleation with integrated porous
Discussion polyethylene implant. They found that myoconjunctival PMMA implant
An ideal orbital implant and surgical technique should yield excellent movement was better than the traditional PMMA implant, and was
prosthesis motility and cosmesis, with very few complications. similar to that of the porous polyethylene implant. Even more, prosthesis
The technique includes choosing an appropriately sized implant, movement with the myoconjunctival PMMA implant was better than that
positioning the implant deeply in the orbit, meticulously closing the Tenon with either the traditional PMMA or porous polyethylene implants.30
capsule over the implant, and securing the conjunctiva over the implant
without tension. An important aspect of implant movement is the contraction of the rectus
muscles. According to the Starling hypothesis,39 muscle contraction is
Imbrication of the rectus muscles over a non-integrated implant compromised by undue stretching beyond its original length, and this is
traditionally was thought to impart movement to the implant and believed to have been responsible for the decreased implant movement
prosthesis. Like a ball-and-socket joint, when the implant moves, the after the traditional imbrication technique. This poor implant movement
prosthesis on surface moves. However, because the so-called ball and in turn leads to poor prosthesis movement because spherical implants
socket are separated by layers of Tenon’s capsule, imbricated muscles, impart movement to the prosthesis by providing a smooth pivotal surface
US OPH THAL MIC REVIE W
47
Yousef_FINAL.indd 47 30/03/2016 23:23
Enucleation
over which the prosthesis glides passively. This probably accounted for HA implants range from 0% to 22%,15,30–44 while it is almost (0%) for silicone
the poorer prosthesis movement in the traditional PMMA group compared implants.45 Buettner and Bartley42 proposed that exposure of HA implants
with the myoconjunctival technique, where each muscle is sutured to is related to the inflammatory reaction incited by the implant or by delayed
the respective fornix, thus avoiding stretching. One more reason for that fibrous ingrowth. Goldberg et al.46 suggested that use of HA implants, even
difference is that the muscle imbrication over the anterior surface of the with exposure, was less likely to lead to extrusion or infection compared
implant is associated with higher rate of implant displacement, while the with exposure with silicone or acrylic implants. Shields et al.47 described
deep orbital placement of the implant, the secure posterior Tenon’s capsule 100 cases of HA implants, among which they reported six patients with
over it, and the suturing of the extraocular muscles to the fornices in the excessive postoperative orbital pain, two patients with wound edema, and
myoconjunctival PMMA implant technique might have helped implant one patient with erosion. In another report of 250 cases they described
centration better.26,29 eight patients with conjunctival thinning, four patients with erosions, and
one with orbital infection.48
The prosthesis movement associated with the myoconjunctival PMMA
implant was better than with the integrated porous polyethylene implant. Conclusion
That is possibly because the attachment of the extraocular muscle to the In conclusion, orbital implants have been used for more than a
fornices causes exaggerated deepening and shallowing of the fornices century. Serious complications can occur, but they do so infrequently.
when the patient attempts to look in different directions, thereby causing Different surgical techniques were described in the literature; both the
further enhanced prosthesis movement. myoconjunctival enucleation technique (with non-integrated implant)
and the integrated porous orbital implant technique result in better
Unfortunately, many complications are associated with integrated implant and prosthesis movement than the traditional muscle imbrication
implants. Rates of exposure and postoperative inflammation of integrated enucleation technique with a PMMA implant. ■
1. Soares IP, França VP, Evisceration and enucleation, Semin Instruments, Philadelphia: Blakiston, 1910:457–77. 34. Custer PL, Trinkaus KM, Fornoff J, Comparative motility
Ophthalmol, 2010;25:94–7. 19. Anderson RL, Thiese SM, Nerad JA, et al., The universal orbital of hydroxyapatite and alloplastic enucleation implants,
2. Luce CM, A short history of enucleation, Int Ophthalmol Clin, implant: indications and methods, Adv Ophthalmic Plast Ophthalmology, 1999;106:513– 6.
1970;10:681–7. Reconstr Surg, 1990;8:88–99. 35. Jordan DR, Chan S, Mawn L, et al., Complications associated
3. Gougelman HP, The evolution of the ocular motility implant, Int 20. Beard C, Remarks on historical and newer approaches to orbital with pegging hydroxyapatite orbital implants, Ophthalmology,
Ophthalmol Clin, 1970;10:689–711. implants, Ophthalmic Plast Reconstr Surg, 1995;11:89–90. 1999;106:505–12.
4. Shah RD, Singa RM, Aakalu VK, Setabutr P, Evisceration and 21. Girard LJ, Eguez I, Soper JW, et al., Buried quasi-integrated 36. Goldberg RA, Dresner SC, Braslow RA, et al., Animal model
enucleation: a national survey of practice patterns in the United enucleation implant of Proplast II: a preliminary report, of porous polyethylene orbital implants, Ophthalmic Plast
States, Ophthalmic Surg Lasers Imaging, 2012;43:425–30. Ophthalmic Plast Reconstr Surg, 1990;6:141–3. Reconstr Surg, 1994;10:104–9.
5. Moshfeghi DM, Moshfeghi AA, Finger PT, Enucleation, Surv 22. Karesh JW, Dresner SC, High-density porous polyethylene 37. Karcioglu ZA, al-Mesfer SA, Mullaney PB, Porous polyethylene
Ophthalmol, 2000;44:277–301. (Medpor) as a successful anophthalmic socket implant, orbital implant in patients with retinoblastoma, Ophthalmology,
6. Chaudhry IA, AlKuraya HS, Shamsi FA, et al., Current indications Ophthalmology, 1994;101:1688–95; discussion 1695–6. 1998;105:1311– 6.
and resultant complications of evisceration, Ophthalmic 23. Migliori ME, Putterman AM, The domed dermis-fat graft orbital 38. Soll DB, The anophthalmic socket, Ophthalmology,
Epidemiol, 2007;14(2):93–7. implant, Ophthalmic Plast Reconstr Surg, 1991;7:23–30. 1982;89:407–23.
7. Anderson RL, Thiese SM, Nerad JA, et al., The Universal orbital 24. Hornblass A, Biesman BS, Eviatar JA, Current techniques of 39. Nunery WR, Hetzler KJ, Improved prosthetic motility following
implant: indications and methods, Adv Ophthal Plast Reconstr enucleation: a survey of 5,439 intraorbital implants and a review enucleation, Ophthalmology, 1983;90:1110–15.
Surg, 1990;888–99. of the literature, Ophthalmic Plast Reconstr Surg, 1995;11:77– 40. De Potter P, Shields CL, Shields JA, Singh AD, Use of the
8. Tyers AG, Collin JR, Baseball orbital implants: a review of 39 86; discussion 87–8. hydroxyapatite ocular implant in the pediatric population, Arch
patients, Br J Ophthalmol, 1985;69:438–42. 25. Graue GF, Finger PT, Physiologic positron emission tomography/ Ophthalmol, 1994;112:208–12.
9. Helms HA, Zeiger HE Jr, Callahan A, Complications following CT imaging of an integrated orbital implant, Ophthal Plast 41. Hornblass A, Biesman BS, Eviatar JA, Current techniques of
enucleation and implantation of multiple glass spheres in the Reconstr Surg, 2012;28:e4–6. enucleation: a survey of 5,439 intraorbital implants and a
orbit, Ophthal Plast Reconstr Surg, 1987;387–9. 26. Allen L, The argument against imbricating the rectus review of the literature, Ophthal Plast Reconstr Surg,
10. Hornblass A, Herschorn BJ, Double sphere orbital implantation muscles over spherical orbital implants after enucleation, 1995;11:77–88.
in enucleation and evisceration, Ophthal Plast Reconstr Surg, Ophthalmology, 1983;90:1116 –20. 42. Buettner H, Bartley GB, Tissue breakdown and exposure
1985;165–8. 27. Shields CL, Shields JA, Eagle RC, De Potter P, Histopathologic associated with orbital hydroxyapatite implants, Am J
11. Jacob-LaBarre JT, DiLoreto DA, Total integration of an ocular evidence of fibrovascular ingrowth four weeks after Ophthalmol, 1992;113:669–73.
implant/prosthesis: preliminary in vivo study of a new design, implantation of the hydroxyapatite orbital implant, Am J 43. Kaltreider SA, Newman SA, Prevention and management of
Ophthal Plast Reconstr Surg, 1995;11200–8. Ophthalmol, 1991;111:363–6. complications associated with the hydroxyapatite implants,
12. Karesh JW, Dresner SC, High density porous polyethylene 28. Sires BS, Holds JB, Archer CR, et al., Histological and radiological Ophthal Plast Reconstr Surg, 1996;1218–31.
(Medpor) as a successful anophthalmic socket implant, analyses of hydroxyapatite orbital implants in rabbits, Ophthal 44. Oestreicher JH, Liu E, Berkowitz M, Complications of
Ophthalmology, 1994;101:1688–96. Plast Reconstr Surg, 1995;11:273–7. hydroxyapatite orbital implants: a review of 100 consecutive
13. Morax S, Use of GORE-TEX (polytetrafluoroethylene) in the 29. Nunery WR, Chen WP, Enucleation and evisceration. In: cases and a comparison of Dexon mesh (polyglycolic acid) with
anophthalmic socket, Adv Ophthalmic Plast Reconstr Surg, Bosniak SL, ed., Principles and Practice of Ophthalmic Plastic scleral wrapping, Ophthalmology, 1997;104:324–9.
1990;882–7. and Reconstructive Surgery, vol. 2, Philadelphia: Saunders, 45. Nunery WR, Heinz GW, Bonnin JM, et al., Exposure rate
14. Perry AC, Integrated orbital implants, Adv Ophthal Plast 1996;1035– 45. of hydroxyapatite spheres in the anophthalmic socket:
Reconstr Surg, 1990;875–81. 30. Shome D, Honavar SG, Raizada K, Raizada D, Implant and histopathologic correlation and comparison with silicone
15. Remulla HD, Rubin PA, Shore JW et al., Complications of porous prosthesis movement after enucleation: a randomized sphere implants, Ophthal Plast Reconstr Surg, 1993;996–104.
spherical orbital implants, Ophthalmology, 1995;102,586–93. controlled trial, Ophthalmology, 2010;117:1638–44. 46. Goldberg RA, Holds JB, Ebrahimpour J, Exposed hydroxyapatite
16. Shields CL, Shields JA, De Potter P, Singh AD, Problems with the 31. Chin K, Margolin CB, Finger PT, Early ocular prosthesis orbital implants: report of six cases, Ophthalmology,
hydroxyapatite orbital implant: experience with 250 consecutive insertion improves quality of life after enucleation, Optometry, 1992;99:831–6.
cases, Br J Ophthalmol, 1994;78:702–6. 2006;77:71–5. 47. Shields CL, Shields JA, De Potter P, Hydroxyapatite orbital
17. Schaefer DP, Rocca RC, Enucleation. In: Nesi FA, Lisman RD, 32. Vincent AL, Webb MC, Gallie BL, Héon E, Prosthetic conformers: implant after enucleation: experience with initial 100
Levine MR, eds., Smith’s Ophthalmic Plastic and Reconstructive a step towards improved rehabilitation of enucleated children, consecutive cases, Arch Ophthalmol, 1992;110:333–8.
Surgery, 2nd ed. St. Louis, MO: Mosby, 1998;1015–52. Clin Experiment Ophthalmol, 2002;30:58–9. 48. Shields CL, Shields JA, De Potter P, Singh AD, Lack of
18. Beard CH, Ophthalmic Surgery: A Treatise on Surgical 33. Shields CL, Shields JA, De Potter P, Singh AD, Problems with the complications of the hydroxyapatite orbital implant in
Operations Pertaining to the Eye and Its Appendages, with hydroxyapatite orbital implant: experience with 250 consecutive 250 consecutive cases, Trans Am Ophthalmol Soc,
Chapters on Para-Operative Technique and Management of cases, Br J Ophthalmol, 1994;78:702–6. 1993;91:177–95.
48 U S OPH TH A LMIC RE VIE W
Yousef_FINAL.indd 48 30/03/2016 23:23
Вам также может понравиться
- Aromatherapy For Professionals ENGДокумент593 страницыAromatherapy For Professionals ENGcamelia100% (3)
- Implants in Maxillofacial Prosthodontics PDFДокумент50 страницImplants in Maxillofacial Prosthodontics PDFankita50% (2)
- Lesson Plan Renal CalculiДокумент17 страницLesson Plan Renal CalculiAmrita Dean71% (7)
- Evisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsДокумент6 страницEvisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsSaraelsy MonterrosoОценок пока нет
- Acfs 2019 00605 PDFДокумент5 страницAcfs 2019 00605 PDFChandra BudiОценок пока нет
- Regional Anesthesia and Eye SurgeryДокумент7 страницRegional Anesthesia and Eye SurgeryharumОценок пока нет
- Hyperostosing Sphenoid Wing Meningiomas: Surgical Outcomes and Strategy For Bone Resection and Multidisciplinary Orbital ReconstructionДокумент10 страницHyperostosing Sphenoid Wing Meningiomas: Surgical Outcomes and Strategy For Bone Resection and Multidisciplinary Orbital ReconstructionPanggea Ghiyats SabrianОценок пока нет
- 9Документ7 страниц9Soal KoasОценок пока нет
- The Role of Arthroscopy in Instability of The Elbow 2023 JSES InternationalДокумент6 страницThe Role of Arthroscopy in Instability of The Elbow 2023 JSES Internationaligor gayosoОценок пока нет
- Successful Treatment of Intraorbital Lymphangioma With Tissue Fibrin GlueДокумент3 страницыSuccessful Treatment of Intraorbital Lymphangioma With Tissue Fibrin GlueIRAОценок пока нет
- Piis2058534917300604 PDFДокумент7 страницPiis2058534917300604 PDFirvan rahmanОценок пока нет
- Bone Transport Distraction Osteogenesis 1Документ31 страницаBone Transport Distraction Osteogenesis 1Euginia YosephineОценок пока нет
- Corneal TransplantationДокумент10 страницCorneal TransplantationKabelo MaruvaОценок пока нет
- Cabigas, Mary Rose (Manuscript) CRANIOPLASTYДокумент5 страницCabigas, Mary Rose (Manuscript) CRANIOPLASTYMa. Ydela MeradoresОценок пока нет
- Immediate One-Stage Postextraction Implant: A Human Clinical and Histologic Case ReportДокумент6 страницImmediate One-Stage Postextraction Implant: A Human Clinical and Histologic Case ReportBagis Emre GulОценок пока нет
- J Neurosurg Pediatr Article p701Документ4 страницыJ Neurosurg Pediatr Article p701mirmasottОценок пока нет
- Oculofacial Plastic and Orbital SurgeryДокумент14 страницOculofacial Plastic and Orbital SurgeryTakwinОценок пока нет
- Novel Surgical Technique For Clavicle Graft HarvestДокумент5 страницNovel Surgical Technique For Clavicle Graft Harvestsanchaita kohliОценок пока нет
- Comminuted Intraarticular Fractures of The Tibial Plateau Lead To Posttraumatic Osteoarthritis of The Knee: Current Treatment ReviewДокумент7 страницComminuted Intraarticular Fractures of The Tibial Plateau Lead To Posttraumatic Osteoarthritis of The Knee: Current Treatment ReviewGustavoBecerraОценок пока нет
- SwithcingДокумент6 страницSwithcingKyoko CPОценок пока нет
- Arthroscopy of The Inferior Compartment of The Temporomandibular Joint - A New PerspectiveДокумент5 страницArthroscopy of The Inferior Compartment of The Temporomandibular Joint - A New PerspectiveFatima Karoline DultraОценок пока нет
- 2016 Periumbilical Fat Auto-Graft Associated To A Porous Orbital Implant For Socket Reconstruction After EnucleationДокумент7 страниц2016 Periumbilical Fat Auto-Graft Associated To A Porous Orbital Implant For Socket Reconstruction After EnucleationDimitris RodriguezОценок пока нет
- Vol 17 Issues 4 Anterior Segment CompliДокумент97 страницVol 17 Issues 4 Anterior Segment CompliScerbatiuc CristinaОценок пока нет
- Document PDFДокумент4 страницыDocument PDFBagis Emre GulОценок пока нет
- Conventional - Extracapsular - Cataract - Extraction - and CirugiaДокумент4 страницыConventional - Extracapsular - Cataract - Extraction - and CirugiaPedro PeredaОценок пока нет
- Modified Incision For Maxillectomy: Our ExperienceДокумент4 страницыModified Incision For Maxillectomy: Our Experiencedarmayanti ibnuОценок пока нет
- Crawley 2015Документ6 страницCrawley 2015Eduardo HernándezОценок пока нет
- Artroscopia Yang Paper Cirugia Maxilofacial AtmДокумент6 страницArtroscopia Yang Paper Cirugia Maxilofacial AtmAna Clara BiscottiОценок пока нет
- Experimental Alveolar Ridge Augmentation by Distraction Osteogenesis Using A Simple Device That Permits Secondary Implant PlacementДокумент8 страницExperimental Alveolar Ridge Augmentation by Distraction Osteogenesis Using A Simple Device That Permits Secondary Implant PlacementBagis Emre GulОценок пока нет
- Osteoarthritis and Osteoporosis 2Документ38 страницOsteoarthritis and Osteoporosis 2tarikeopsОценок пока нет
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumДокумент6 страницComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinОценок пока нет
- Aaos Elbow Surgical Approaches-1Документ9 страницAaos Elbow Surgical Approaches-1Mossa SultanyОценок пока нет
- Immediate Prostheses On One Piece Trans Mucosal Implants in Flapless Surgical Procedures Case Series Report Part I Full Arch RehabilitationsДокумент6 страницImmediate Prostheses On One Piece Trans Mucosal Implants in Flapless Surgical Procedures Case Series Report Part I Full Arch RehabilitationsSalem Fathi BermawiОценок пока нет
- Retromandibular Approach JournalДокумент4 страницыRetromandibular Approach JournalAldo AguilarОценок пока нет
- Kyung 2013Документ4 страницыKyung 2013thompson sousa thompsonОценок пока нет
- Case Report: The Prosthetic Management of A Case of Epulis Fissuratum by A Novel TechniqueДокумент6 страницCase Report: The Prosthetic Management of A Case of Epulis Fissuratum by A Novel TechniqueMichelle VelezОценок пока нет
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumДокумент6 страницComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinОценок пока нет
- FDP AvulsionДокумент8 страницFDP AvulsionNico BrantesОценок пока нет
- DownloadДокумент14 страницDownloadhasan nazzalОценок пока нет
- Management of Odontogenic Tumors / Orthodontic Courses by Indian Dental AcademyДокумент82 страницыManagement of Odontogenic Tumors / Orthodontic Courses by Indian Dental Academyindian dental academyОценок пока нет
- Acromioclavicular Fracture Dislocation Fixation TeДокумент7 страницAcromioclavicular Fracture Dislocation Fixation TeMinh ChíОценок пока нет
- Corneal Transplantation in Modern EraДокумент16 страницCorneal Transplantation in Modern Eraसुनन्दन भट्टОценок пока нет
- Holy Angel University: Enucleation of The GlobeДокумент4 страницыHoly Angel University: Enucleation of The GlobeRennel EscotoОценок пока нет
- CLG PterygiumДокумент3 страницыCLG PterygiumMichael HumiantoОценок пока нет
- JC - Endoscopic Techniques in OralДокумент33 страницыJC - Endoscopic Techniques in OralNarla SusheelОценок пока нет
- PM 070 E0Документ23 страницыPM 070 E0Radu HarliscaОценок пока нет
- Cabello 2015Документ22 страницыCabello 2015Vannia BautistaОценок пока нет
- ArticlДокумент6 страницArticlAhmadОценок пока нет
- Journal 3Документ6 страницJournal 3Maulida HalimahОценок пока нет
- Corso 1995Документ6 страницCorso 1995Matei RazvanОценок пока нет
- Surgical Outcome of Blowout Fractures of Floor of Orbit A Case Series Of5 Patients 2155 9570 1000518Документ5 страницSurgical Outcome of Blowout Fractures of Floor of Orbit A Case Series Of5 Patients 2155 9570 1000518Luqman HakimОценок пока нет
- (123doc) Opthalmic Microsurgical Suturing Techniques Part 9Документ15 страниц(123doc) Opthalmic Microsurgical Suturing Techniques Part 9TEODORA MIHAELA PELEASAОценок пока нет
- Cid 13008Документ10 страницCid 13008snkidОценок пока нет
- Comparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationДокумент7 страницComparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationvikrizkaОценок пока нет
- Basic Knee Arthroscopy Part 4Документ2 страницыBasic Knee Arthroscopy Part 4Diego BellingОценок пока нет
- Mandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyДокумент10 страницMandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyFerenc NagyОценок пока нет
- Rectangular Loop Suture To Correct Iris Capture of The Posterior Chamber Intraocular LensДокумент5 страницRectangular Loop Suture To Correct Iris Capture of The Posterior Chamber Intraocular LensHuang WanjingОценок пока нет
- Proptosis FTOZДокумент9 страницProptosis FTOZMohab MohamedОценок пока нет
- Reyneke2015.pdf-Bsso Steps PDFДокумент10 страницReyneke2015.pdf-Bsso Steps PDFBenjie LawОценок пока нет
- Surgical Outcome of Primary Intradural Surgical Outcome of Primary IntraduralДокумент6 страницSurgical Outcome of Primary Intradural Surgical Outcome of Primary Intraduralmazen alkarrasОценок пока нет
- Alterations in Thickness of Macula After Uncomplicated Cataract SurgeryДокумент14 страницAlterations in Thickness of Macula After Uncomplicated Cataract SurgeryInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Endoscopic Procedures on the SpineОт EverandEndoscopic Procedures on the SpineJin-Sung KimОценок пока нет
- PDFДокумент228 страницPDFSatria Adi MarhendraОценок пока нет
- Analysis of Base Apex Lead Electrocardiograms of Normal Dairy CowsДокумент8 страницAnalysis of Base Apex Lead Electrocardiograms of Normal Dairy CowsSatria Adi MarhendraОценок пока нет
- 23936-Article Text-73375-1-10-20181031Документ2 страницы23936-Article Text-73375-1-10-20181031Satria Adi MarhendraОценок пока нет
- Two Cases of Dipylidiasis (Dog Tapeworm Infection) in Children: Update On An Old ProblemДокумент6 страницTwo Cases of Dipylidiasis (Dog Tapeworm Infection) in Children: Update On An Old ProblemSatria Adi MarhendraОценок пока нет
- Surgical Management of Aural Hematoma in Dog: December 2017Документ5 страницSurgical Management of Aural Hematoma in Dog: December 2017Satria Adi MarhendraОценок пока нет
- Clinical Usefulness of Propofol As An Anesthetic Induction Agent in Dogs and CatsДокумент3 страницыClinical Usefulness of Propofol As An Anesthetic Induction Agent in Dogs and CatsSatria Adi MarhendraОценок пока нет
- Clinical Assessment of Repeated Propofol-Associated Anesthesia in CatsДокумент7 страницClinical Assessment of Repeated Propofol-Associated Anesthesia in CatsSatria Adi MarhendraОценок пока нет
- Mechanisms in Hyperkalemic Renal Tubular AcidosisДокумент4 страницыMechanisms in Hyperkalemic Renal Tubular AcidosisSatria Adi MarhendraОценок пока нет
- UretrotomyДокумент10 страницUretrotomySatria Adi MarhendraОценок пока нет
- Canine Prostatic Diseases: Reproduction and Periparturient CareДокумент13 страницCanine Prostatic Diseases: Reproduction and Periparturient CareSatria Adi MarhendraОценок пока нет
- Feed Additives, Antibodies, Poultry Vaccines 2023.3Документ6 страницFeed Additives, Antibodies, Poultry Vaccines 2023.3Bruce YangОценок пока нет
- Pathomorphology MCQSДокумент191 страницаPathomorphology MCQSNana BentilОценок пока нет
- Anatomy and Physiology Laboratory: Exercise: Digestive SystemДокумент4 страницыAnatomy and Physiology Laboratory: Exercise: Digestive SystemLouise Mica LeeОценок пока нет
- Carvalho-2016-About AssesmentДокумент19 страницCarvalho-2016-About AssesmentChiriac Andrei TudorОценок пока нет
- US - Inggris 2017Документ5 страницUS - Inggris 2017SmabaitulhikmahОценок пока нет
- Drug Related Problem (DRP)Документ10 страницDrug Related Problem (DRP)ERONADIAULFAH SUGITO50% (2)
- Dorothea Orem: Self-Care TheoryДокумент16 страницDorothea Orem: Self-Care TheoryHazel LezahОценок пока нет
- Psychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Документ21 страницаPsychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Eduardo Aguirre DávilaОценок пока нет
- Salmon Dna: Introducing Scientific Breaktrough From JapanДокумент6 страницSalmon Dna: Introducing Scientific Breaktrough From JapanLeonardo100% (1)
- Invos System Improving Patient Outcomes Cerebral Somatic Oximetry BrochureДокумент6 страницInvos System Improving Patient Outcomes Cerebral Somatic Oximetry Brochuremihalcea alinОценок пока нет
- Coronavirus Disease (COVID-19) : Case Investigation FormДокумент2 страницыCoronavirus Disease (COVID-19) : Case Investigation FormJudeLaxОценок пока нет
- Introduction of The Topic: Nano-BiotechnologyДокумент7 страницIntroduction of The Topic: Nano-BiotechnologyAbhishek YadavОценок пока нет
- What Is Rheumatoid ArthritisДокумент16 страницWhat Is Rheumatoid ArthritisDurge Raj GhalanОценок пока нет
- Fever of Unknown OriginДокумент26 страницFever of Unknown OriginFiona Yona Sitali100% (1)
- DMC FinalsДокумент64 страницыDMC Finalskaye agustinОценок пока нет
- Nursing Care PlanДокумент13 страницNursing Care PlanJan DamesОценок пока нет
- Dr. Marcelia Suryatenggara, Sp. S - How To Choose Your AnalgeticsДокумент9 страницDr. Marcelia Suryatenggara, Sp. S - How To Choose Your AnalgeticsFreade AkbarОценок пока нет
- Scenihr o 046Документ116 страницScenihr o 046Ana NicoletaОценок пока нет
- Causes of Metabolic AcidosisДокумент10 страницCauses of Metabolic AcidosisKimberly Anne SP PadillaОценок пока нет
- Science: Modified Strategic Intervention MaterialsДокумент28 страницScience: Modified Strategic Intervention Materialskotarobrother23Оценок пока нет
- SAM 350P User ManualДокумент40 страницSAM 350P User ManualkristiaОценок пока нет
- Effectiveness of Psychoeducation For Relapse, Symptoms, Knowledge, Adherence and Functioning in Psychotic Disorders: A Meta-AnalysisДокумент14 страницEffectiveness of Psychoeducation For Relapse, Symptoms, Knowledge, Adherence and Functioning in Psychotic Disorders: A Meta-AnalysisPatty IzquierdoОценок пока нет
- Pros and Cons EuthanasiaДокумент3 страницыPros and Cons EuthanasiaMirantika Audina100% (1)
- Timed Up and Go Test RalanДокумент1 страницаTimed Up and Go Test RalanBagus Andi PramonoОценок пока нет
- Group Assignment Population EconomicsДокумент7 страницGroup Assignment Population EconomicsSayed Abdullah Shah SadaatОценок пока нет
- Documents 34-51Документ3 страницыDocuments 34-51api-575141270Оценок пока нет
- Antibiotic Resistance Lesson Plan Final ProjectДокумент10 страницAntibiotic Resistance Lesson Plan Final Projectapi-436796283Оценок пока нет
- Analytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajДокумент7 страницAnalytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajyusufОценок пока нет