Академический Документы
Профессиональный Документы
Культура Документы
Henoch-Schonlein Purpura A Review Article
Загружено:
rezaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Henoch-Schonlein Purpura A Review Article
Загружено:
rezaАвторское право:
Доступные форматы
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/6127285
Henoch-Schönlein Purpura: A Review Article
Article in Southern Medical Journal · September 2007
DOI: 10.1097/SMJ.0b013e3180f62d0f · Source: PubMed
CITATIONS READS
58 3,449
6 authors, including:
Paul Roberts Thomas Waller
Mayo Foundation for Medical Education and Research Mayo Foundation for Medical Education and Research
3 PUBLICATIONS 71 CITATIONS 6 PUBLICATIONS 74 CITATIONS
SEE PROFILE SEE PROFILE
Jerry Sayre
Mayo Clinic
7 PUBLICATIONS 83 CITATIONS
SEE PROFILE
All content following this page was uploaded by Thomas Waller on 23 August 2018.
The user has requested enhancement of the downloaded file.
Review Article
Henoch-Schönlein Purpura: A Review Article
Paul F. Roberts, MD, Thomas A. Waller, MD, Todd M. Brinker, MD, Izabela Z. Riffe, MD,
Jerry W. Sayre, MD, and Robert L. Bratton, MD
America, Caucasians have the highest incidence, and African
Abstract: Henoch-Schönlein purpura (HSP) is the most common
vasculitis of childhood. Although HSP is typically a disease of chil-
Americans have the lowest incidence. Although the cause of
dren, adult cases have been described. HSP can affect multiple or-
HSP is unknown, it commonly follows an upper respiratory
gans with a characteristic rash present in all patients. Most cases
tract infection. As a result, the disease is more common in
resolve with symptomatic treatment, but serious complications can
January through March.7,9
occur such as renal failure. Primary care physicians should be well
The overall incidence in children has been estimated to
aware of the disease because the true incidence is probably under-
be 13.5 cases per 100,000.10 In 2002, a survey was published
estimated.
on the frequency and ethnic variation of childhood vasculitic
syndromes. The survey had been sent monthly to subspecial-
Key Words: children, Henoch-Schönlein purpura, rash, renal dis- ists and family physicians in the United Kingdom for 3 years.
ease The survey results revealed that the HSP incidence was higher
than previously expected, at 22.1 cases per 100,000 popula-
tion.11 The true incidence is probably underestimated because
H enoch-Schönlein purpura (HSP), a vasculitis of the small
vessels, is the most common vasculitis of childhood.
First described in 1801 by William Heberden,1,2 it was orig-
cases are often not reported to public health agencies.
inally known as Heberden-Willan disease. In 1837, Johann Pathophysiology
Lukas Schönlein recognized the association between purpura HSP is a systemic vasculitis characterized by the tissue
and arthritis.1,3 Edouard Heinrich Henoch later reported a deposition of IgA-containing immune complexes. The depo-
case that also included abdominal pain, bloody diarrhea, and sition of IgA and occasionally IgG in the mesangial region of
renal involvement.1,2 Many believe that HSP is what led to the kidney is the prominent feature by fluorescence micros-
Wolfgang Amadeus Mozart’s death in 1791,4,5 although this copy.12,13 On histologic examination, the appearance of renal
supposition cannot be confirmed. lesions varies from mild focal mesangial proliferation to cres-
The cause of HSP is unclear; however, it may occur after centic glomerulonephritis.14 The pathogenesis of this disease
an upper respiratory infection. HSP is characterized by non- is similar to that of IgA nephropathy, which has the same
thrombocytopenic palpable purpura, abdominal pain, arthri- histologic findings in the kidney.13,15
tis, and glomerulonephritis. It is treated with supportive care HSP has a prominent cutaneous component with skin
and is usually self-limited, although it can cause glomerulo- lesions consisting of subepidermal hemorrhages and necro-
nephritis and death. The prognosis is excellent in those cases tizing vasculitis of the small vessels of the dermis.16 IgA is
without renal disease. also present in these vessels. The vasculitis can also occur in
other organs, such as the gastrointestinal tract.
Epidemiology
HSP is typically a disease of children between the ages of Clinical Manifestations
3 and 10 years. Although adult cases have been described, HSP usually presents with a classic tetrad of rash, pol-
50% of all cases occur at or before the age of 5 years.6,7 yarthralgias, abdominal pain, and renal disease.2,7 The rash,
Males are affected twice as often as females.7,8 In North
Key Points
• Henoch-Schönlein purpura (HSP) is the most com-
From the Department of Family Medicine, Mayo Clinic, Jacksonville, Flor-
ida; and the Department of Family Medicine, Mayo Clinic, Scottsdale, mon vasculitis of childhood.
Arizona. • HSP can affect multiple organs, with a rash present in
Reprint requests to Dr. Paul F. Roberts, Mayo Clinic, Department of Family all cases.
Medicine, 4500 San Pablo Road, Jacksonville, FL 32224. Email:
roberts.paul@mayo.edu • Treatment of HSP is usually symptomatic, but serious
Accepted March 20, 2007. complications can occur.
Copyright © 2007 by The Southern Medical Association • The true incidence of HSP is probably underestimated.
0038-4348/0⫺2000/10000-0821
Southern Medical Journal • Volume 100, Number 8, August 2007 821
Roberts et al • Henoch-Schönlein Purpura
Fig. Palpable purpura on the legs
of a child.
which occurs in all patients, is characterized clinically as Diagnosis
palpable purpura (Fig.). The lesions are typically nonblanch- The presence of palpable purpura with the other compo-
ing, as they represent extravasation of blood into the skin,14 nents of the tetrad makes the diagnosis straightforward. How-
and they often occur in groups that can persist for 3 to 10 ever, other systemic autoimmune diseases must be consid-
days. They can occur anywhere on the skin but are often ered, such as other forms of vasculitis or juvenile rheumatoid
concentrated on the lower legs and arms. In children, local arthritis. Few laboratory tests are useful for diagnosis. Often
angioedema may precede the development of the purpura. mild leukocytosis with a normal platelet count is found. Oc-
The polyarthralgias are present in more than 80% of patients. casionally, eosinophilia is present. In some studies, throat
They most commonly affect the knees and ankles and are swabs for group A hemolytic streptococcus were positive in
often associated with edema. These findings resolve after a more than 50% of patients.12,19 However, other studies have
few days and leave no permanent damage.16 The abdominal found no increased incidence of group A hemolytic strepto-
pain, occurring in more than half of the patients, is often coccus infection in children with HSP.12 Elevation of IgA in
colicky-type pain. It frequently develops within 8 days of the the blood occurs in 50% of patients, and a definitive diagno-
appearance of the rash. The pain is usually associated with sis is confirmed by a biopsy specimen of the skin or kidney
nausea, vomiting, and diarrhea, or perhaps constipation, and that shows IgA deposition.7,20
blood and mucus are frequently present with stool passage. A In 1990, the American College of Rheumatology devel-
rare complication is intussusception.14,17 The renal disease, oped criteria for the diagnosis of HSP21 (Table 1). According
which occurs in about 40 to 50% of patients, often presents as to the criteria and for the purpose of classification, a patient
mild glomerulonephritis. This produces proteinuria, micro- is said to have HSP if at least 2 of the 4 criteria are present.
scopic hematuria, and often red blood cell casts. Fortunately, The presence of 2 or more of the criteria yields a sensitivity
this renal involvement usually resolves spontaneously.13,16 of 87.1% and a specificity of 87.7%.21
However, a progressive renal condition may develop, and
those with persistent proteinuria will likely have worsening Treatment
renal damage.13,18 Renal failure is the most common cause of The acute, active phase of HSP resolves spontaneously in
death in patients who die with HSP. 94% of children and 89% of adults,6 and the primary goal of
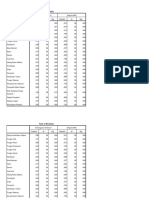
Table 1. American College of Rheumatology criteria for classification of Henoch-Schönlein purpura
Criterion Definition
1. Palpable purpura Slightly raised “palpable” hemorrhagic skin lesions; not related to thrombocytopenia
2. Age ⱕ20 years at disease onset Patient age ⱕ20 years at onset of symptoms
3. Bowel angina Diffuse abdominal pain, worse after meals, or the diagnosis of bowel ischemia, usually including bloody diarrhea
4. Wall granulocytes on biopsy Histologic changes showing granulocytes in the walls of arterioles and venules
From Mills et al.3 Used with permission.
822 © 2007 Southern Medical Association
Review Article
Table 2. Suggested management of various manifestations of Henoch-Schönlein purpura
Short-term Corticosteroids plus
Supportive oral IV IV pulse immunosuppressive
HSP manifestation care only NSAIDs corticosteroids corticosteroids corticosteroids drugs Plasmapheresis
Mild symptoms X
Rash and arthritis X X
Rash and mild edema X
Rash and severe edema X X
Severe colicky abdominal X X
pain
Any abdominal pain with X X
nausea and vomiting
Scrotal or testicular X X
involvement
Nephrotic range proteinuria X X
Rapidly progressive X X X
nephritis
Pulmonary hemorrhage X X X
From Gedalia.7 Used with permission.
HSP, Henoch-Schönlein purpura; IV, intravenous; NSAID, nonsteroidal anti-inflammatory drug.
the patient’s physician is to reassure the patient and the pa- maturia with proteinuria and deterioration of renal function,
tient’s parents of the benign nature of the disease and to then consultation with a pediatric nephrologist is necessary.
provide symptomatic treatment for the patient. The patient Renal biopsy may be necessary to predict prognosis and guide
should be monitored for rare but more serious complications, therapy.3,10,16 Crescentic nephritis discovered by renal biopsy
such as hemorrhagic involvement of the renal, pulmonary, has a poor prognosis, with 1% of affected patients progress-
gastrointestinal, genitourinary, and central nervous systems ing to end-stage renal disease.16 Treatment options for severe
or the joints, which usually occurs within 4 weeks of initial renal involvement by HSP include the following:
presentation but may occur as late as 8 weeks.16 Serious renal
• high-dose corticosteroids, either alone or combined
complications necessitate referral to a pediatric nephrologist.
with immunosuppressive agents such as azathioprine,
The patient (especially a child) may need to be hospitalized
cyclophosphamide, or cyclosporine;
for acute monitoring purposes and hydration. Milder cases
• high-dose IV immunoglobulins;
may be managed at home if the physician has a good rela-
• plasma exchange or plasmapheresis;
tionship with the patient’s parents, and follow-up is assured.
• corticosteroids combined with urokinase and warfarin;
Joint pain and painful soft tissue edema usually respond to
• renal transplant.3,10,16
acetaminophen or nonsteroidal anti-inflammatory drugs,22 but
The suggested management of the various manifestations
oral prednisone, 1 to 2 mg/kg per day, may be necessary to
of HSP is summarized in Table 2.3
hasten their resolution.16 Anti-inflammatory agents should be
Thirty percent of patients who recover from HSP may
avoided in patients with extensive renal involvement. Several
have recurrent symptoms as late as 7 years after the acute
anecdotal reports suggest dapsone may hasten the resolution
phase, and those with renal involvement may have lifelong
of the palpable rash.16
problems. The patient’s physician, therefore, needs to moni-
No placebo-controlled prospective studies have been con-
tor for complications.16
ducted on the use of corticosteroids in treating HSP abdom-
inal pain; however, a few retrospective analyses and multiple Conclusion
case reports suggest that corticosteroids may lead to rapid HSP is the most common vasculitis of childhood, and the
resolution of abdominal pain within 24 hours without serious true incidence is probably underestimated because the num-
complications.3,10 In addition, a few studies have suggested ber of cases is underreported. HSP can affect multiple organ
factor XIII replacement therapy to treat severe gastrointesti- systems, and the characteristic palpable purpuric rash is
nal tract bleeding complications.16 present in all patients. The vast majority of cases resolve
Although most physicians who treat children agree on spontaneously, but the patients should be monitored for rare
the acute treatment of HSP, the treatment of the pulmonary, but serious complications.
neurologic, and renal complications remains controversial.23
Renal involvement is common in patients with HSP, but the References
majority of patients maintain normal renal function.13 Corti-
1. Matteson EL. Notes on the history of eponymic idiopathic vasculitis: the
costeroid therapy does not prevent the development of pro- diseases of Henoch and Schönlein, Wegener, Churg and Strauss, Horton,
gressive renal disease.3,16 If there is evidence of marked he- Takayasu, Behçet and Kawasaki. Arthritis Care Res 2000;13:237–245.
Southern Medical Journal • Volume 100, Number 8, August 2007 823
Roberts et al • Henoch-Schönlein Purpura
2. Ballinger S. Henoch-Schönlein purpura. Curr Opin Rheumatol 2003;15: 13. Fervenza FC. Henoch-Schönlein purpura nephritis. Int J Dermatol 2003;
591–594. 42:170–177.
3. Mills JA, Michel BA, Bloch DA, et al. The American College of Rheu- 14. Saulsbury FT. Henoch-Schönlein purpura. Curr Opin Rheumatol 2001;
matology 1990 criteria for the classification of Henoch-Schönlein pur- 13:35–40.
pura. Arthritis Rheum 1990;33:1114–1121. 15. Cotran RS, Kumar V, Collins T, editors. Robbins pathologic basis of
4. Davies PJ. Mozart’s death: a rebuttal of Karhausen: further evidence for disease, 6th ed. Philadelphia, Saunders, 1999.
Schönlein-Henoch syndrome. J R Soc Med 1991;84:737–740. 16. Rostoker G. Schönlein-Henoch purpura in children and adults: diagno-
5. Kubba AK, Young M. Wolfgang Amadeus Mozart: a case report. J R sis, pathophysiology and management. BioDrugs 2001;15:99–138.
Coll Surg Edinb 1996;41:44–47. 17. Leung AK, Chan KW. Evaluating the child with purpura. Am Fam Physi-
6. Blanco R, Martinez-Taboada VM, Rodriguez-Valverde V, et al. He- cian. 2001;64:419–428. Erratum in: Am Fam Physician 2002;65:1751.
noch-Schönlein purpura in adulthood and childhood: two different ex- 18. Saulsbury FT. Henoch-Schönlein purpura in children: report of 100
pressions of the same syndrome. Arthritis Rheum 1997;40:859–864. patients and review of the literature. Medicine (Baltimore) 1999;78:395–
7. Gedalia A. Henoch-Schönlein purpura. Curr Rheumatol Rep 2004;6: 409.
195–202. 19. Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-
8. Agraharkar M, Gokhale S, Le L, et al. Cardiopulmonary manifestations Schönlein purpura. J Paediatr Child Health 1998;34:405–409.
of Henoch-Schönlein purpura. Am J Kidney Dis 2000;35:319–322. 20. Halling SF, Soderberg MP, Berg UB. Henoch Schönlein nephritis: clin-
9. Robson WL, Leung AK. Henoch-Schönlein purpura. Adv Pediatr 1994; ical findings related to renal function and morphology. Pediatr Nephrol
41:163–194. 2005;20:46–51. Epub 2004 Oct 22.
10. Szer IS. Henoch-Schönlein purpura. Curr Opin Rheumatol 1994;6:25–31. 21. Bailey M, Chapin W, Licht H, et al. The effects of vasculitis on the gas-
11. Gardner-Medwin JM, Dolezalova P, Cummins C, et al. Incidence of trointestinal tract and liver. Gastroenterol Clin North Am 1998;27:747–782.
Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in 22. Giangiacomo J, Tsai CC. Dermal and glomerular deposition of IgA in
children of different ethnic origins. Lancet 2002;360:1197–1202. anaphylactoid purpura. Am J Dis Child 1977;131:981–983.
12. Saulsbury FT. Epidemiology of Henoch-Schönlein purpura. Cleveland 23. Kraft DM, Mckee D, Scott C. Henoch-Schönlein purpura: a review. Am
Clin J Med 2002;69:SII-87–SII-9. Fam Physician 1998;58:405–408.
We make a living by what we get, we make a life by
what we give.
—Sir Winston Churchill
824 © 2007 Southern Medical Association
View publication stats
Вам также может понравиться
- Positive Options for Antiphospholipid Syndrome (APS): Self-Help and TreatmentОт EverandPositive Options for Antiphospholipid Syndrome (APS): Self-Help and TreatmentРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Henoch Schoenlein PurpuraДокумент10 страницHenoch Schoenlein PurpuraAlberto Kenyo Riofrio PalaciosОценок пока нет
- Brief: Henoch-Schönlein PurpuraДокумент5 страницBrief: Henoch-Schönlein PurpuraAdrian KhomanОценок пока нет
- Henoch-Schonlein PurpuraДокумент5 страницHenoch-Schonlein PurpuraPramita Pramana100% (1)
- Henoch Schonlein Purpura (IgA Vasculitis)Документ15 страницHenoch Schonlein Purpura (IgA Vasculitis)Emily Eresuma100% (1)
- Eosinophilia and RashДокумент3 страницыEosinophilia and RashmikelОценок пока нет
- Henoch Schonlein Purpura HSP Case ReportДокумент3 страницыHenoch Schonlein Purpura HSP Case ReportResearch ParkОценок пока нет
- Uk HSP1Документ3 страницыUk HSP1Ery RadiyantiОценок пока нет
- Whipple S DiseaseДокумент12 страницWhipple S DiseaseGrifanda HumairahОценок пока нет
- All Rights Reserved Vol. 114, No. 3: American Journal of EpidemiologyДокумент12 страницAll Rights Reserved Vol. 114, No. 3: American Journal of EpidemiologyMaisury LadjidjiОценок пока нет
- Mills 2010Документ8 страницMills 2010JOAO CARLOS BATISTA LIZОценок пока нет
- Henoch-Schonlein Purpura: An Update: Nutan Kamath, Suchetha RaoДокумент7 страницHenoch-Schonlein Purpura: An Update: Nutan Kamath, Suchetha RaoManjunath VaddambalОценок пока нет
- Diagnostic Criteria For Systemic Lupus ErythematosusДокумент9 страницDiagnostic Criteria For Systemic Lupus ErythematosusarifbudipraОценок пока нет
- HSP 508Документ6 страницHSP 508As-sifa KharismaОценок пока нет
- Hyperhidrosis: A Common Problem: Reventive AreДокумент11 страницHyperhidrosis: A Common Problem: Reventive AreAfiqah RahahОценок пока нет
- Westjmed00082 0031Документ8 страницWestjmed00082 0031Engga Swari RatihОценок пока нет
- Clinical Practice Diagnosis and Management of HenoДокумент9 страницClinical Practice Diagnosis and Management of HenoHosne araОценок пока нет
- Prevalence of Idiopathic Normal Pressure Hydrocephalus: A Prospective, Population-Based StudyДокумент11 страницPrevalence of Idiopathic Normal Pressure Hydrocephalus: A Prospective, Population-Based StudyNovrianda Eka PutraОценок пока нет
- Pediatric VasculitisДокумент17 страницPediatric VasculitisRam PadronОценок пока нет
- Henoch-Schonlein Purpura Associated With Bee Sting Case Report PDFДокумент7 страницHenoch-Schonlein Purpura Associated With Bee Sting Case Report PDFjoshkelОценок пока нет
- Anatomy & Medicine MCQs April 14Документ21 страницаAnatomy & Medicine MCQs April 14sb medexОценок пока нет
- Education and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemДокумент11 страницEducation and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemKhalvia KhairinОценок пока нет
- 2022 Hepatic EncephalopathyДокумент22 страницы2022 Hepatic Encephalopathykarina hernandezОценок пока нет
- IJP - Volume 3 - Issue 6.2 - Pages 1097-1101Документ5 страницIJP - Volume 3 - Issue 6.2 - Pages 1097-1101Ash mohamedОценок пока нет
- Causes of DysphagiaДокумент23 страницыCauses of DysphagiaDe WiqОценок пока нет
- ManagementДокумент9 страницManagementanka_mihaelaОценок пока нет
- Final Paper Rheumatic Heart DiseaseДокумент16 страницFinal Paper Rheumatic Heart DiseasePrincess TumambingОценок пока нет
- Hereditary SpherocytosisДокумент39 страницHereditary SpherocytosisjoannaОценок пока нет
- Eosinofilia 2022Документ24 страницыEosinofilia 2022raymundo lopez silvaОценок пока нет
- 1271 HSP .FullДокумент8 страниц1271 HSP .FulldonkeyendutОценок пока нет
- Significance of Family History in Homoeopathic PrescribingДокумент8 страницSignificance of Family History in Homoeopathic PrescribingHomoeopathic Pulse50% (2)
- Johne's Disease and Crohn's Disease, Report in BriefДокумент2 страницыJohne's Disease and Crohn's Disease, Report in BriefNational Academies of Science, Engineering, and MedicineОценок пока нет
- Chediak - HigashisyndromeLessonsfromasingle CentrecaseseriesДокумент6 страницChediak - HigashisyndromeLessonsfromasingle CentrecaseseriesHeitor DambiskiОценок пока нет
- Henoch-Schonlein Purpura Clinical Presentation History, Physical Examination, ComplicationsДокумент19 страницHenoch-Schonlein Purpura Clinical Presentation History, Physical Examination, ComplicationsResty SukurОценок пока нет
- Jessica Reid-Adam: Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, NYДокумент3 страницыJessica Reid-Adam: Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, NYAnastasia Widha SylvianiОценок пока нет
- EtiologyДокумент2 страницыEtiologyJan JeweyОценок пока нет
- Epilepsy 2Документ6 страницEpilepsy 2fikaОценок пока нет
- Hant PDFДокумент6 страницHant PDFRodrigo AriasОценок пока нет
- Sydenham Chorea 2019Документ3 страницыSydenham Chorea 2019Hajrin PajriОценок пока нет
- 2015 PsoriasisДокумент12 страниц2015 PsoriasispablopabloortizortizОценок пока нет
- Am Fam Physician. 1998 Aug 1 58 (2) :405-408.: Clinical Presentation RashДокумент6 страницAm Fam Physician. 1998 Aug 1 58 (2) :405-408.: Clinical Presentation RashAnastasia Widha SylvianiОценок пока нет
- Renal Calculi: An Unusual Presentation of T-Cell Acute Lymphoblastic LeukemiaДокумент6 страницRenal Calculi: An Unusual Presentation of T-Cell Acute Lymphoblastic LeukemiaHussein KhalifehОценок пока нет
- Infectious Mononucleosis: A Case ReportДокумент3 страницыInfectious Mononucleosis: A Case ReportSerghei CojocariОценок пока нет
- 2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CДокумент4 страницы2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CPratyay HasanОценок пока нет
- Dicaprio 2014Документ10 страницDicaprio 2014Montserrat SantiagoОценок пока нет
- Angiolupus 4Документ2 страницыAngiolupus 4AlisОценок пока нет
- Acute Hypotonia in An Infant (2017)Документ3 страницыAcute Hypotonia in An Infant (2017)nikos.alexandrОценок пока нет
- Infantile Hemangiomas: From Pathogenesis To Clinical FeaturesДокумент10 страницInfantile Hemangiomas: From Pathogenesis To Clinical FeaturesIfadahОценок пока нет
- 5 Psoriasis ManagementДокумент10 страниц5 Psoriasis ManagementrioОценок пока нет
- Echevarria Jonille S. BS-Pharmacy 2 November 03, 2020: 1. Comment in House M.D. "Hunting"Документ3 страницыEchevarria Jonille S. BS-Pharmacy 2 November 03, 2020: 1. Comment in House M.D. "Hunting"Jonille EchevarriaОценок пока нет
- Behçet's SyndromeДокумент12 страницBehçet's SyndromeFernando Franco VargasОценок пока нет
- p1319 PDFДокумент4 страницыp1319 PDFSyairodhiОценок пока нет
- Psoriasis 2 Epidemiology and Clinical Spectrum: Difficulties in Defining Psoriasis FrequencyДокумент7 страницPsoriasis 2 Epidemiology and Clinical Spectrum: Difficulties in Defining Psoriasis FrequencyMiguel Martin DiazОценок пока нет
- Polyserositis: A Diagnostic Challenge: Polyserositis Diagnosis Is ChallengingДокумент7 страницPolyserositis: A Diagnostic Challenge: Polyserositis Diagnosis Is ChallengingAarathi raoОценок пока нет
- The SLE Review Series: Working For A Better Standard of CareДокумент8 страницThe SLE Review Series: Working For A Better Standard of CareCamilo TovarОценок пока нет
- International Journal of Health Sciences and ResearchДокумент4 страницыInternational Journal of Health Sciences and Researchmamal malikaОценок пока нет
- Reviews: Henoch-Schönlein Purpura Nephritis in ChildrenДокумент11 страницReviews: Henoch-Schönlein Purpura Nephritis in ChildrenRivqa Rati InggitОценок пока нет
- Henoch Scholein PurpuraДокумент2 страницыHenoch Scholein PurpuraPhil Adit RОценок пока нет
- Czlonkowska 2019 WDДокумент44 страницыCzlonkowska 2019 WDMartinaAstMonОценок пока нет
- Gastroparesis Dan Dumping SyndromeДокумент12 страницGastroparesis Dan Dumping SyndromeBela RonaldoeОценок пока нет
- Toorthj 6 28 PDFДокумент8 страницToorthj 6 28 PDFrezaОценок пока нет
- C Spine LectureДокумент57 страницC Spine LecturerezaОценок пока нет
- CervicalspineanatomyДокумент15 страницCervicalspineanatomyrezaОценок пока нет
- CervicalspineanatomyДокумент15 страницCervicalspineanatomyrezaОценок пока нет
- CervicalspineanatomyДокумент15 страницCervicalspineanatomyrezaОценок пока нет
- CervicalspineanatomyДокумент15 страницCervicalspineanatomyrezaОценок пока нет
- Arterial Wall InjuryДокумент2 страницыArterial Wall InjuryrezaОценок пока нет
- DigestiveДокумент13 страницDigestiverezaОценок пока нет
- TongueДокумент54 страницыTongueishak_alsophОценок пока нет
- Full Paper ATCSAДокумент16 страницFull Paper ATCSArezaОценок пока нет
- Kompetensi Yang Harus Dikuasai Spesialis Bedah Umum, (Lama) 2Документ5 страницKompetensi Yang Harus Dikuasai Spesialis Bedah Umum, (Lama) 2Ikhsan HidayatОценок пока нет
- Clinical, Pathological and Prognostic AspectsДокумент87 страницClinical, Pathological and Prognostic AspectsrezaОценок пока нет
- Appendiceal Abscess Ef FixДокумент24 страницыAppendiceal Abscess Ef FixrezaОценок пока нет
- Emergency Operation ReportДокумент2 страницыEmergency Operation ReportrezaОценок пока нет
- Respiratory Medicine Case Reports: Regina Monteiro, José Carlos Carneiro, Claúdia Costa, Raquel DuarteДокумент4 страницыRespiratory Medicine Case Reports: Regina Monteiro, José Carlos Carneiro, Claúdia Costa, Raquel DuarterezaОценок пока нет
- Tests of Normality BanaДокумент10 страницTests of Normality BanarezaОценок пока нет
- Tests of Normality BanaДокумент10 страницTests of Normality BanarezaОценок пока нет
- Tests of Normality BanaДокумент10 страницTests of Normality BanarezaОценок пока нет
- Duplication Cyst of The Pylorus: A Case Report: Sefta Jaka, Dastamuar Shalita, Saksono SinduДокумент1 страницаDuplication Cyst of The Pylorus: A Case Report: Sefta Jaka, Dastamuar Shalita, Saksono SindurezaОценок пока нет
- BMI Lap CholeДокумент7 страницBMI Lap CholerezaОценок пока нет
- Meconium IleusДокумент2 страницыMeconium IleusrezaОценок пока нет
- Brain AbscessДокумент3 страницыBrain AbscessrezaОценок пока нет
- Peritonitis and Intraabdominal InfectionДокумент71 страницаPeritonitis and Intraabdominal InfectionrezaОценок пока нет
- Ward Report 4-5-2017Документ9 страницWard Report 4-5-2017rezaОценок пока нет
- Perforasi GasterДокумент29 страницPerforasi GasterrezaОценок пока нет
- Laporan Jaga Bangsal 3-5-2017Документ9 страницLaporan Jaga Bangsal 3-5-2017rezaОценок пока нет
- Ward Report Thursday, February 23 2017Документ3 страницыWard Report Thursday, February 23 2017rezaОценок пока нет
- Ward Report 22-2-2017Документ4 страницыWard Report 22-2-2017Afkar30Оценок пока нет
- United General Hospital ICU Expansion Case StudyДокумент7 страницUnited General Hospital ICU Expansion Case StudyTeddy Les Holladayz25% (4)
- Female Sexual DysfunctionДокумент18 страницFemale Sexual DysfunctionRisky SetiawanОценок пока нет
- Acute Renal FailureДокумент1 страницаAcute Renal FailureSonia Letran Singson100% (1)
- HEPADNAVIRIDAEДокумент14 страницHEPADNAVIRIDAEnur qistina humaira zulkarshamsiОценок пока нет
- Pelayanan PaliatifДокумент43 страницыPelayanan PaliatifBety RindaОценок пока нет
- Assessment of Knowledge and Attitude Towards Patient-Centered Care Among UndergraduateДокумент13 страницAssessment of Knowledge and Attitude Towards Patient-Centered Care Among UndergraduateKIU PUBLICATION AND EXTENSIONОценок пока нет
- BeraДокумент20 страницBeraMuhamad SyaifulОценок пока нет
- Icd X: Diagnose ICD Diagnosa ICDДокумент33 страницыIcd X: Diagnose ICD Diagnosa ICDannisa statiraОценок пока нет
- Salubris Medical Center: National Highway, Brgy. Roxas, Solano, Nueva VizcayaДокумент10 страницSalubris Medical Center: National Highway, Brgy. Roxas, Solano, Nueva Vizcayajulie ann afanОценок пока нет
- Case Study Week 1 Community Acquired Pneumonia 1Документ6 страницCase Study Week 1 Community Acquired Pneumonia 1Yuuki Chitose (tai-kun)Оценок пока нет
- Investigatory Project On AnalgesicsДокумент30 страницInvestigatory Project On AnalgesicsAnurag Singh100% (1)
- UntitledДокумент14 страницUntitledsyntacs skОценок пока нет
- Approach To Nursing Assessment 1Документ5 страницApproach To Nursing Assessment 1Taiye OkondoОценок пока нет
- Laboratory Investigation ReportДокумент7 страницLaboratory Investigation ReportAmarjeetОценок пока нет
- Aapc 2016Документ92 страницыAapc 2016Ravi Pal75% (4)
- The Hong Kong College of Anaesthesiologists Final Fellowship Examination March/May 2006 Examiners ReportДокумент10 страницThe Hong Kong College of Anaesthesiologists Final Fellowship Examination March/May 2006 Examiners ReportJane KoОценок пока нет
- 1translation and MedicineДокумент202 страницы1translation and MedicineMNОценок пока нет
- New Techniques in Chelonian Shell RepairДокумент8 страницNew Techniques in Chelonian Shell RepairChecko LatteОценок пока нет
- Rachael Stanton Resume Rachael Stanton LVT 1 2Документ2 страницыRachael Stanton Resume Rachael Stanton LVT 1 2api-686124613Оценок пока нет
- Fulmer SPICES: An Overall Assessment Tool For Older AdultsДокумент2 страницыFulmer SPICES: An Overall Assessment Tool For Older AdultsSteve GarrettОценок пока нет
- Case Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)Документ4 страницыCase Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)john dave rougel ManzanoОценок пока нет
- Inroduction To Homoeopathic Materia Medica 2023Документ10 страницInroduction To Homoeopathic Materia Medica 2023mahitha sujithОценок пока нет
- Kedaruratan THT I: Dr. Sri Utami Wulandari, SPTHT-KLДокумент24 страницыKedaruratan THT I: Dr. Sri Utami Wulandari, SPTHT-KLEvi Liana BahriahОценок пока нет
- Aga Khan University Postgraduate Medical Education (Pgme) Induction Frequently Asked QuestionsДокумент15 страницAga Khan University Postgraduate Medical Education (Pgme) Induction Frequently Asked QuestionsRamzan BibiОценок пока нет
- Home Study Course-HomeopathДокумент155 страницHome Study Course-HomeopathAzad Ansari67% (6)
- Louis Kuhne - Neo-Naturopathy (New Science of Healing) (1917)Документ313 страницLouis Kuhne - Neo-Naturopathy (New Science of Healing) (1917)Școala Solomonară / The Solomonary School100% (16)
- Resilient Health Care (2013)Документ297 страницResilient Health Care (2013)Pepi RamosОценок пока нет
- Mock Congress Bill Research EssayДокумент9 страницMock Congress Bill Research Essayapi-302890064Оценок пока нет
- Chapter 34 Emergency Cardiovascular SystemДокумент24 страницыChapter 34 Emergency Cardiovascular SystemDharlyn MungcalОценок пока нет
- Patient Education and NegotiationДокумент7 страницPatient Education and NegotiationSammy ChegeОценок пока нет