Академический Документы
Профессиональный Документы
Культура Документы
Osteosarcoma
Загружено:
Ahmad Syahmi YZАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Osteosarcoma
Загружено:
Ahmad Syahmi YZАвторское право:
Доступные форматы
Osteosarcoma
About
• Malignant tumor arise within bone & spreading rapidly outward to periosteum & surrounding soft
tissue
• 2nd most common tumor in orthopedic
• Highly malignant primary bone tumor
Most common
• Most common age group: Children, young adult (15 – 25 years old)
• Most common musculoskeletal tumor in children & young adult
• Most common site: Long bone metaphysis such as
» Lower end of femur (Most common)
» Upper end of tibia (Common)
» Upper end of humerus (Less common)
• Why osteosarcoma most common in metaphysis?
» Growth based on Johnson’s theory of field selection, proliferative primitive spindle cells lodged in
metaphysis
History
• Bone pain (75%) – 1st symptom, constant, boring in nature, worse at night, increase severity
• Swelling (lump) – 2nd symptoms (Most common 100%)
• History of trauma
• Pathological fracture – rare
Examination
• Swelling at metaphysis
• Local tenderness
• Palpable mass (late presentation)
• Skin over swelling is shiny + prominent veins
• Warm swelling
• Inflamed overlying tissue
Pathology
• Osteosarcoma: Malignant tumor of mesenchymal cells characterized by formation of osteoid or bone
by tumor cells
Gross morphology Histopathology
1. Osteoblastic type
• Greyish white, hard, gritty architecture
2. Chondroid type
• Opalescent, bluish grey
3. Fibroblastic type
• Typical fish flesh sarcomatous appearance
4. Telangiectatic
• Large area of tumor necrosis
• Blood filled spaces within tumor mass
Classification
Clinical Classification Histopathology classification
1. Primary Osteosarcoma 1. Osteoblastic
• Most common • High bone formation
• Age group: 15 – 25 years old 2. Chondroid
• No pre-malignant conditions • Malignant cell is cartilage cell
• More malignant than secondary osteosarcoma 3. Fibroblastic
2. Secondary Osteosarcoma • Malignant cell is fibroblast
• Less common 4. Telangiectatic or Osteolytic
• Age group: > 45 years old • Predominantly lytic tumor
• Pre malignant lesions: Paget’s disease, Multiple • Most agressive
endochromatosis, Fibrous dysplasia, Irradiation
to bone, Multiple osteochondroma
• Treatment: Same as primary osteosarcoma
Metastasis
• Hematogenous (through blood)
• 1st organ to metastasize: Lung
• Most common Bone metastasis – Vertebra
• Lymph node involvement: Uncommon
• Osteosarcoma rarely invade epiphyseal plate
Investigation
Investigation Reasons Expected indings
FBC Monitoring • WBC
ESR Monitoring • ESR
Serum Alkaline Useful for follow-up case; • Serum Alkaline phosphatase
phosphatase (SAP) Indicator of recurrence or
metastasis
Bone X-ray Diagnosis • Area of irregular destruction in metaphysis
• New bone formation in tumor matrix
• Bone cortex is eroded
• Irregular periosteal reaction (elevation)– tumor
lift periosteum
• Codman’s triangle (typical)
• Sun-ray appearance (Pathognomonic) – due to
calcification along periosteal blood vessel
• Pathological fracture
Core needle biopsy Gold standard in diagnosis • Confirm diagnosis by gross morphology &
Open Biopsy histopathology by pathologist
FNAC • Core needle biopsy is ideal – because less
bleeding, minimum contamination
• Diagnostic: Presence of malignant osteod
Chest X-ray Metastasis • Multiple lung nodule (lung metastasize)
• Lung is the 1st site of metastasis
Chest CT-scan Metastasis • If Chest X-ray not clear
• To detect micro metastasis
• More sensitive than Chest X-ray
• 10% patient have lung metastasis when
diagnosis is made
Bone scan Metastasis • To detect intra-medullary spread (Skip lesions)
MRI Metastasis • To detect soft tissue spread
• Best investigation for local staging
CT-scan Metastasis • To detect soft tissue spread
Confirm diagnosis
Open biopsy (Gold standard)
Clinical + Radiological (If biopsy unsure)
How to suspect osteosarcoma clinically?
• Young age group – 15 – 25 years old
• No joint involvement, but may have extra-articular restriction
• No constitutionals ymptoms
Treatment
“It is important to eradicate the primary lesion completely; the mortality rate after local recurrence is far
worse than following effective ablation at the first encounter” Apley concise orthopaedic
Stage & Treatment
Stage Description Treatment
IA Intracompartmental low grade Limb-saving surgery (Radical excision)
IB Extracompartmental low grade Amputation
II A Intracompartmental high grade Limb-saving surgery (Radical excision)
II B Extracompartmental high grade Amputation
(Most common stage 70%)
III Metastasis (Common stage 30%) Palliative ablation/ Chemo/ Radiotherapy
1. Local control (Surgical removal)
(1) Amputation (mainstay treatment) (2) Limb-saving surgery (Radical excision)
Site Level Commonly perform
Lower end femur • Mid thigh amputation For early diagnosis
(early lesion) After 8 – 12 weeks of pre-surgery (neo adjuvant)
• Hip disarticulation chemotherapy
Upper end femur • Hip disarticulation No skip lesions
(early lesion) Tumor is resectable
• Hindquarter
amputation Perform radical excision
Upper end tibia • Mid thigh amputation
Bone defect after surgery is filled with bone graft
Upper end humerus • Forequarter or prosthesis
amputation
Post-surgery Chemotherapy
(3) Radiotherapy
Indication:
• Tumor found at surgically inaccessible site
• Patient refuse surgery
2. Control distant macro or micro-metastasis
• Majority cases, micro-metastasis occur when diagnosis is made
(1) Neoadjuvant Chemotherapy (2) Immunotherapy
• Given pre or post-surgery • Not yet practice as its new treatment
• High dose: Methotrexate, Citrovorum factor, • Principle: Portion of tumor (donor) is implanted
Endoxan, Cisplastinum into sarcoma survivor (recipient) & the tumor
• Highly toxic, need to manage adverse effect removed after 14 days. Sensitized lymphocytes
• Give for 8 – 12 weeks from survivor then infused into patient to kill the
cancer cells
Prognosis
• Without treatment, death occur within 2 years ~ usually within 6 months if there is micro-metastasis
• 20% survive with Surgery
• 70% survive with Surgery + Adjuvant Chemotherapy
• Worst prognosis: Telangiectatic osteosarcoma
Course of osteosarcoma if not treated
• It breaches the cortex and the soft tissues interior of muscles, nerves, vascular structures and distant
metastasis and not by lymphatics. This is because bone has no lymphatics.
Difference between Osteosarcoma & Ewing sarcoma
Osteosarcoma Ewing sarcoma
Location Appendicular skeleton 50% axial skeleton
50% appendicular skeleton
Constitutional symptoms Absent Present
Вам также может понравиться
- Sba MedicineДокумент19 страницSba MedicineAhmad Syahmi YZ100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Acute Otitis MediaДокумент1 страницаAcute Otitis MediaAhmad Syahmi YZОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Paediatrics SbaДокумент34 страницыPaediatrics SbaAhmad Syahmi YZ100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- OBSTETRICS AND GYNAECOLOGY CollectionДокумент12 страницOBSTETRICS AND GYNAECOLOGY CollectionAhmad Syahmi YZОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- SBA SurgeryДокумент9 страницSBA SurgeryAhmad Syahmi YZОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Panic DisorderДокумент3 страницыPanic DisorderAhmad Syahmi YZОценок пока нет
- CC PsychosisДокумент6 страницCC PsychosisAhmad Syahmi YZОценок пока нет
- Q&A ENT EmergencyДокумент9 страницQ&A ENT EmergencyAhmad Syahmi YZОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Psychotic Disorder PsychosisДокумент3 страницыPsychotic Disorder PsychosisAhmad Syahmi YZОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Generalized Anxiety DisorderДокумент3 страницыGeneralized Anxiety DisorderAhmad Syahmi YZОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Seminar DementiaДокумент63 страницыSeminar DementiaAhmad Syahmi YZОценок пока нет
- Psychiatry Shelf ReviewДокумент11 страницPsychiatry Shelf ReviewAhmad Syahmi YZ75% (4)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Panic DisorderДокумент3 страницыPanic DisorderAhmad Syahmi YZОценок пока нет
- GMT 409 Psychiatry Student Guide BookДокумент43 страницыGMT 409 Psychiatry Student Guide BookAhmad Syahmi YZ100% (1)
- CPG MDDДокумент11 страницCPG MDDAhmad Syahmi YZОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- HO Ortho NotesДокумент13 страницHO Ortho NotesAhmad Syahmi YZОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Treatment For ESRDДокумент9 страницTreatment For ESRDpunpen ngorsakun100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- CataractДокумент292 страницыCataractTiffany Clementson100% (1)
- HEGUДокумент2 страницыHEGUSee Hing Kok100% (1)
- PDDPharmacyprojectДокумент22 страницыPDDPharmacyprojectGeeta G. Kulkarni100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Antioxidant and Antimicrobial Activities of Pink Guava Leaves and SeedsДокумент10 страницAntioxidant and Antimicrobial Activities of Pink Guava Leaves and SeedsRobbyОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1091)
- Drug StudyДокумент21 страницаDrug StudyShyla Garnace JavillonarОценок пока нет
- Cancer ChemotherapyДокумент79 страницCancer ChemotherapyDanii-Boo InspiraОценок пока нет
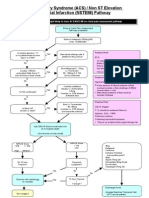
- ACS NSTEMI Clinical PathwayДокумент3 страницыACS NSTEMI Clinical PathwayXtiaRОценок пока нет
- Gastrointestinal DrugsДокумент27 страницGastrointestinal DrugsKer YehunОценок пока нет
- Effect of Crew Resource ManagementДокумент10 страницEffect of Crew Resource ManagementoguzatikОценок пока нет
- Sputum ExaminationДокумент9 страницSputum ExaminationDr. Ashish JawarkarОценок пока нет
- Yellow Card 20 MedicДокумент2 страницыYellow Card 20 MedicLeonardo AlcotaОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Cardiac OutputДокумент37 страницCardiac OutputIndrashish Chakravorty100% (1)
- Admission NUHДокумент2 страницыAdmission NUHDanny WidjajaОценок пока нет
- JMRB Resume - FinalДокумент3 страницыJMRB Resume - Finalapi-280548809Оценок пока нет
- CAT Intervention FormДокумент3 страницыCAT Intervention FormVictoria Perreault QuattrucciОценок пока нет
- Floppy BabyДокумент13 страницFloppy BabyJorge JhgОценок пока нет
- Salzmann Evaluation IndexДокумент4 страницыSalzmann Evaluation IndexRissa Septi RahardiniОценок пока нет
- Patient Care Classification SystemДокумент8 страницPatient Care Classification SystemWin AndangОценок пока нет
- Welch Allyn Atlas Patient Monitor - Service Manual 2007 PDFДокумент225 страницWelch Allyn Atlas Patient Monitor - Service Manual 2007 PDFGeorge LunaОценок пока нет
- Pi Is 0025619616308187Документ13 страницPi Is 0025619616308187Anthony M CaballeroОценок пока нет
- ME210 Gastrointestinal TimetableДокумент6 страницME210 Gastrointestinal TimetableEka Irina Akma KamaruddinОценок пока нет
- Critical Review On Pentazocine AbuseДокумент10 страницCritical Review On Pentazocine Abuseאדיטי פאווארОценок пока нет
- NehaДокумент20 страницNehaRecorders RndОценок пока нет
- Medical Spas in Los Angeles, CA (Report by Harrison Gordon)Документ182 страницыMedical Spas in Los Angeles, CA (Report by Harrison Gordon)Leon ParsaudОценок пока нет
- Rekap MJSДокумент6 страницRekap MJSRidho SaputraОценок пока нет
- Disruption of Radiologist WorkflowДокумент6 страницDisruption of Radiologist WorkflowChrisОценок пока нет
- Sindh Nurses Examination Board Karachi: Center Supervisor: S.No Name School Name RemarksДокумент1 страницаSindh Nurses Examination Board Karachi: Center Supervisor: S.No Name School Name RemarksAyazОценок пока нет
- Consequence Maps With CitationsДокумент4 страницыConsequence Maps With Citationsapi-247044545Оценок пока нет
- Periorbital Paederus DermatitisДокумент3 страницыPeriorbital Paederus DermatitisWanly SyahrizalОценок пока нет