Академический Документы
Профессиональный Документы
Культура Документы
Incident Open-Angle Glaucoma and Blood Pressure
Загружено:
meikisirmanОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Incident Open-Angle Glaucoma and Blood Pressure
Загружено:
meikisirmanАвторское право:
Доступные форматы
Incident Open-Angle Glaucoma and Blood Pressure
M. Cristina Leske, MD, MPH; Suh-Yuh Wu, MA; Barbara Nemesure, PhD; Anselm Hennis, MRCP(UK),
PhD; for the Barbados Eye Studies Group
Background: The risk of open-angle glaucoma (OAG) may be incidence was 0.7%, increasing to 18.3% with IOP
related to low blood pressure (BP) relative to in-traocular greater than 25 mm Hg, for a 25-fold increase in RR.
pressure (IOP), ie, to low perfusion pressure (PP). However, OAG developed throughout the IOP range
Alternatively, systemic hypertension may increase OAG risk. and two thirds of incident cases had baseline IOP less
than 25 mm Hg. Baseline hypertension was associated
Objective: To clarify these possible relationships by with a halving of the RR of OAG (RR, 0.49; 95% confi-
evaluating hypertension and PP (where PP=BP−IOP) as dence interval [CI], 0.29-0.85); the RR also tended to
risk factors for incident OAG in a black population. decrease as systolic BP increased (P = .07). Consistent
with these findings, a lower baseline PP increased RR
Design: Population-based cohort study (85% partici- (systolic PP 101 mm Hg, 2.6 [95% CI, 1.3-4.9]; dias-
pation); simple random sample of residents of Barba-dos, tolic PP 55 mm Hg, 3.2 [95% CI, 1.6-6.6]; mean PP 42
West Indies, aged 40 years and older. mm Hg, 3.1 [95% CI, 1.6-6.0]).
Participants: Two thousand nine hundred eighty-nine Conclusions: As baseline IOP increased, the risk of OAG
black participants at risk; 67 developed OAG after 4 years substantially increased. In contrast, persons with sys-temic
(2.2% incidence). hypertension at baseline had half the RR, suggest-ing that
hypertension does not increase (and may de-crease) the 4-
Main Outcome Measure: Adjusted relative risk (RR) of year risk of OAG. Lower PP at baseline increased RR
OAG from logistic regression analyses. approximately 3-fold, a result consistent with the vascular
hypothesis of OAG pathogenesis.
Results: The 4-year risk increased markedly with base-line
IOP. With an IOP less than or equal to 17 mm Hg, Arch Ophthalmol. 2002;120:954-959
I N THE LAST 10 YEARS, several large prevalence
studies of open-angle glaucoma (OAG)
have been conducted.1-10 While they have
between high BP and OAG might be ex-
pected. These conflicting scenarios re-
garding the possible effect of high or low
BP levels on OAG risk have not been clari-
confirmed the relationship of fied. Elucidating this relationship is im-
OAG to age, high intraocular pressure portant to understand the factors affect-ing
(IOP), family history, and African ances- OAG development as well as having
try, no other major risk factors have been clinical implications given the high preva-
From the School of Medicine,
identified consistently. Vascular factors lence of hypertension and use of BP-
University of New York at
Stony Brook, Stony Brook have been investigated,11-19 with particu-lar lowering treatment among older adults.
(Drs Leske, Nemesure, attention to blood pressure (BP) and One obstacle to clarifying the issue is
Hennis, and Ms Wu; the perfusion pressure (PP), where PP = BP − the dearth of population-based cohort studies
Ministry of Health, Barbados, IOP. According to the vascular hy-pothesis to measure incidence, ie, the risk of
West Indies (Dr Hennis); the of OAG pathogenesis, a low BP relative to developing OAG in a given period. Such
School of Clinical Medicine IOP could lead to low PP, thus impairing longitudinal studies allow the most valid
and Research, University of perfusion of the optic nerve and causing inferences by recording BP at baseline be-fore
the West Indies, Barbados,
glaucomatous loss of the visual field. On the onset of OAG, and following the cohort to
(Dr Hennis); and the School of
the other hand, systemic hyper-tension may identify incident cases that de-velop over
Medicine, The Johns Hopkins
University, Baltimore, Md. The increase risk by damaging the small vessels time. The magnitude of the BP effect can be
members of the Barbados Eye of the optic disc; further-more, BP and IOP quantified by calculating rela-tive risks (RR$),
Studies Group are listed on levels which compare the inci-dence of OAG at
page 958. various BP levels.21 Avail-
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
954
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
Table 1. Four-year Incidence of Open-Angle
Glaucoma and RR by IOP at Baseline*
METHODS
Incidence
The Barbados Eye Studies, funded by the National IOP at Baseline,
Eye Institute (Bethesda, Md), are investigating the mm Hg n % RR (95% CI)†
prevalence, incidence, and risk factors for major 17 9/1313 0.7 1.0
causes of visual loss in a large, predominantly 17-19 8/716 1.1 1.59 (0.61-4.16)
African-origin population. The baseline prevalence 19-21 15/559 2.7 3.97 (1.72-9.20)
study, the BES, was based on a simple random 21-23 6/167 3.6 4.76 (1.64-13.83)
sample of Bar-badian-born citizens, aged 40 to 84 23-25 7/102 6.9 10.50 (3.76-29.38)
years, with 84% participation.1 After 4 years, the 25 22/120 18.3 24.69 (10.55-57.79)
surviving cohort members were invited for a follow-
up visit as par-ticipants in BISED and 85% of the *RR indicates relative risk; IOP, intraocular pressure; and CI,
confidence interval.
4040 eligible par-ticipants were reexamined
†Logistic regression adjusting for age, sex,
(N=3427: 3193 black; 139 mixed, 95 white/other).22 hypertension, and IOP-lowering treatment.
As detailed previously,1,22 baseline and fol-low-up
data were collected using standardized pro-tocols,
including ophthalmic and other measure-ments, able reports, however, are based on cross-sectional data
tonometry, Humphrey automated perimetry (Zeiss- from clinic-based or prevalence studies, which do not al-
Humphrey Systems, Dublin, Calif), lens grad-ings, 30° low the determination of incidence or RR.
color stereo fundus photography of the disc and macula, Recently, incidence rates of OAG were obtained by
and an interview. A 10% systematic sample and the Barbados Incidence Study of Eye Diseases (BISED),
persons with specific findings (best-corrected visual 1992-1997,22,23 which reexamined the population-based
acuity 20/30, visual field defects, IOP 21 mm Hg,
history of major eye diseases or dia-betes, family cohort of the Barbados Eye Study (BES), 1988-1992.1 To
history of glaucoma, and inability to have perimetry, assess the potential role of BP, this report evalu-ates
fundus photographs, or lens gradings) were referred for systemic hypertension and PP as risk factors for the 4-year
a comprehensive ophthalmologic exami-nation. The incidence of OAG in black BISED participants while
definition of OAG1,22 required the pres-ence of both controlling for pertinent variables. Since persons of Af-
visual field defects and optic disc dam-age after rican descent have high prevalences of OAG and hyper-
ophthalmologic exclusion of other possible causes. tension, this evaluation has important public health im-
Intraocular pressure was not considered in this plications and makes associations easier to detect.
definition. Visual field defects were determined by
specific criteria based on automated perimetric data.1,22
Optic disc damage was ascertained by the study
ophthalmologist and by masked photo-graphic gradings
at a reading center.
Of the 3193 black BISED participants, 2989 did not have
Three applanation tonometry measurements were OAG at baseline. After 4 years, 67 of these participants
recorded and IOP for a person was defined as the (2.2%) met the criteria for incident OAG.22 Incidence was
highest mean value in either eye. Blood pressure was higher with age, in men, and in those with higher IOP. 22
measured twice with the Hawksley (Hawksley & Sons The 67 incident cases, therefore, were older than the rest of
Ltd, Lancing, Sussex, England) random zero the cohort (median age at baseline, 64 years vs 55 years),
sphygmomanometer, following the Hypertension De- tended to have more males (49% vs 41%), and had higher
tection and Follow-up protocol,24 and the average was IOP (median IOP at baseline, 21.3 mm Hg vs 17.7 mm
used in the analysis. Quality control was main-tained by Hg). At baseline, 10.4% of the incident cases reported IOP-
monitoring digit preference and conduct-ing replicate
measurements. Hypertension was de-fined as a systolic lowering treatment vs 1.1% of the other cohort members. 22
BP (SBP) greater than or equal to 140 mm Hg and/or a As presented in Table 1, the 4-year incidence in-
diastolic BP (DBP) greater than or equal to 90 mm Hg, creased from 0.7% with IOP less than or equal to 17 mm
and/or using BP-lowering treat-ment, following current Hg to 3.6% at IOP 21 to 23 mm Hg, reaching 18.3% at
guidelines.25 Perfusion pres-sure was evaluated by IOP greater than 25 mm Hg. The adjusted RR con-firms
systolic (SBP −IOP), diastolic (DBP − IOP), and mean the strong association between IOP and the inci-dence of
PP (2⁄3 mean arterial pres-sure – IOP, where mean OAG. Compared with IOP less than or equal to 17 mm
arterial pressure=DBP+ 1⁄3 [SBP – DBP]). Blood Hg, the 4-year risk of developing OAG was about 5
pressure and PP were stratified by quartiles of the times higher, with IOP between 21 to 23 mm Hg, and
population distribution and also used as continuous about 25 times higher, with IOP greater than 25 mm Hg,
variables. Associations were evalu-ated by logistic after adjusting for age, sex, IOP-lowering treatment, and
regression analyses, which con-trolled for age, sex, and systemic hypertension status.
other relevant IOP and BP variables. Results are
reported as adjusted RR with 95% confidence intervals. Systemic hypertension was frequent, affecting about
Tests for trend used a 4-cat-egory variable denoting BP 52% of black participants at baseline; about half of these
and PP quartiles in the logistic regression models. All participants with hypertension used BP-lowering medi-
analyses were per-formed with SAS software (SAS cations. Table 2 presents OAG incidence and adjusted RR
Institute, Cary, NC). for hypertension and BP-lowering treatment at base-line.
Persons with hypertension had a statistically sig-nificant
decreased risk of OAG (P = .01), with about half
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
955
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
Table 2. Fo ur-Year Incidence of Open-Angle Table 4. Relative Risk (RR) of Open-Angle Glaucoma
Glaucoma and Relative Risk by Hypertension by Blood Pressure and Treatment Categories at Baseline*
and Blood Pressure Treatment at Baseline*
Incidence
Incidence BP and Treatment Categories No. (%) RR (95% CI)†
No. (%) RR (95% CI)†
SBP, mm Hg
Hypertension SBP 140; no BP-lowering 34/1504 (2.3) 1.0
(SBP/DBP 140/90 mm Hg treatment
or treatment) SBP 140; with BP-lowering 7/373 (1.9) 0.7 (0.29-1.66)
No 34/1420 (2.4) 1.0 treatment
Yes 33/1526 (2.1) 0.49 (0.29-0.85)‡ SBP 140; no BP-lowering 15/619 (2.4) 0.5 (0.26-1.03)
BP-lowering medication treatment
No 49/2125 (2.3) 1.0 SBP 140; with BP-lowering 11/483 (2.3) 0.5 (0.23-1.08)
Yes 18/856 (2.1) 0.74 (0.41-1.33) treatment
DBP, mm Hg
*RR indicates relative risk; CI, confidence interval; SBP, DBP 90; no BP-lowering 41/1785 (2.3) 1.0
systolic BP; and DBP, diastolic BP. treatment
†RRs for BP-lowering treatment or hypertension were adjusted DBP 90; with BP-lowering 10/535 (1.9) 0.5 (0.26-1.17)
for age, sex, IOP, and IOP-lowering treatment. treatment
‡P = .01. DBP 90; no BP-lowering 8/338 (2.4) 0.6 (0.26-1.43)
treatment
DBP 90; with BP-lowering 8/321 (2.5) 0.9 (0.40-2.04)
Table 3. Four-Year Incidence of Open-Angle Glaucoma and treatment
Relative Risk by Quartiles of Blood Pressure at Baseline*
*BP indicates blood pressure; CI, confidence interval; SBP,
systolic BP; and DBP, diastolic BP.
Incidence †Adjusting for age, sex, I0P, and I0P-lowering treatment.
BP Quartiles No. (%) RR (95% CI)†
SBP, mm Hg‡
SBP 119 16/725 (2.2) 1.0 Table 4 presents comparisons of OAG incidence and
119 SBP 132 16/763 (2.1) 0.81 (0.38-1.72) RR with various combinations of BP and treatment sta-tus.
132 SBP 148 14/723 (1.9) 0.63 (0.29-1.38)
Compared with persons without elevated BP, all RRs for
SBP 148 21/775 (2.7) 0.51 (0.23-1.12)
DBP, mm Hg‡ elevated SBP and DBP were less than 1, denoting lower
DBP 73 17/736 (2.3) 1.0 risks. For the subgroup with SBP greater than or equal to
73 DBP 80 17/655 (2.6) 1.20 (0.58-2.48) 140 mm Hg and no treatment, the RR was decreased to one
80 DBP 88 12/779 (1.5) 0.60 (0.28-1.33) half (RR, 0.5; P = .06); a similar result was found for the
DBP 88 21/816 (2.6) 0.94 (0.47-1.89) subgroup with treated but uncontrolled SBP (RR, 0.5; P =
.08). Comparably low RRs were observed for treated and
*RR indicates relative risk; BP, blood pressure; CI, confidence
interval; SBP, systolic BP; and DBP, diastolic BP.
controlled DBP and for DBP of 90 mm Hg and no treat-
†Adjusting for age, sex, intraocular pressure (IOP), and ment (RR, 0.5 and 0.6, respectively).
IOP- or BP-lowering treatment. As presented in Table 5, OAG incidence was high-est
‡Test for trend: P = .07 for SBP; P = .52 for DBP. with low PP. Persons with lower systolic PP (SPP), ie,
lower than the first quartile ( 101.3 mm Hg), had a
the risk (RR, 0.49) of persons with lower BP. Users of significant, more than 21⁄2-times increased RR of devel-
BP-lowering treatment had about three fourths (RR, oping OAG (RR, 2.6). Persons with moderately low SPP
0.74) the risk of nonusers but the RR was not (101.3-114.4 mm Hg) also tended to have an increased RR
statistically sig-nificant. Analyses of age-specific RR (RR, 1.5), whereas persons with moderately high SPP
showed the same pat-tern, with decreased RR in every (114.4-129.8 mm Hg) had similar a RR (RR, 0.9) as those
age group (data not shown). with higher SPP. A similar pattern was found for dias-tolic
Despite the almost 10-year older age of the OAG PP (DPP), where lower DPP ( 55 mm Hg) more than tripled
group, their baseline BP levels (median SBP and DBP, 133 the RR of OAG (RR, 3.2). While lower mean PP (MPP) (
mm Hg and 79 mm Hg, respectively) resembled those of 41.9 mm Hg) also tripled the RR (RR, 3.1), there was a
the remaining cohort members (median SBP and DBP, 132 nonsignificant decreased RR at moderately high MPP (RR,
mm Hg and 80 mm Hg, respectively). Table 3 pre-sents 0.4), a result based on 4 incident cases. All tests for trend
results for SBP and DBP, stratified by quartiles of the were statistically significant (SPP, P = .003; DPP, P .001;
distribution. The crude OAG incidence rates had no MPP, P .001), confirming the negative association between
consistent pattern across SBP and DBP categories, pos- PP and OAG risk. Stratify-ing the analyses by presence or
sibly reflecting the relatively small size of these catego-ries absence of hypertension treatment was unrevealing owing
and their differences in age, sex, IOP, and treat-ment. After to small sample size.
adjusting for these confounding variables, the RR tended to Separate analyses were conducted to evaluate asso-
decrease as SBP increased (0.81 for SBP 119-132 mm Hg; ciations in the subgroup of cases with higher tensions (IOP
0.63 for SBP 132 to 148 mm Hg; 0.51 for SBP greater than 21 mm Hg at follow-up; n=48). These analyses yielded
or equal to 148 mm Hg). The test for trend was consistent similar results to those in Tables 2 through 5. The RRs for
with lower risks at higher SBP (P = .07); no trends were hypertension, SPP, and DPP were of similar mag-nitude
seen for DBP (P = .52). (RR, 0.44, 2.49, and 2.74, respectively) and sta-
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
956
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
tistically significant (P .05). Additional analyses using
Table 5. Four-Year Incidence of Open-Angle Glaucoma
BP and PP as continuous rather than categorical vari-
and Relative Risk by Perfusion Pressure at Baseline*
ables did not materially alter the results.
Incidence
No. (%) RR (95% CI)†
SPP, mm Hg‡
Consistent with these findings, low PP at base-line
SPP 101.3 24/740 (3.2) 2.6 (1.3-4.9)
approximately tripled the RR of OAG, suggesting that low BP 101.3 SPP 114.4 15/748 (2.0) 1.5 (0.7-3.1)
relative to IOP increases RR (Table 5). This find-ing is in 114.4 SPP 129.8 11/743 (1.5) 0.9 (0.4-1.9)
accord with the vascular hypothesis of OAG patho-genesis, SPP 129.8 17/745 (2.3) 1.0
that a low PP would contribute to the develop-ment of visual DPP, mm Hg‡
field defects. The same results were found in the subgroup of DPP 55 33/729 (4.5) 3.2 (1.6-6.6)
55 DPP 62.3 12/723 (1.7) 1.3 (0.6-3.1)
persons with OAG and IOP greater than 21 mm Hg,
62.3 DPP 70.3 11/763 (1.4) 1.2 (0.5-2.7)
suggesting that these results also apply to cases with higher DPP 70.3 11/761 (1.4) 1.0
IOP and are not limited to “normal-tension” OAG. These MPP, mm Hg‡
results suggest the involvement of vascular factors in OAG MPP 41.9 33/750 (4.4) 3.1 (1.6-6.0)
development, with a possible “protec-tive” effect of 41.9 MPP 47.7 16/739 (2.2) 1.5 (0.7-3.3)
hypertension in maintaining an adequate PP. 47.7 MPP 53.6 4/743 (0.5) 0.4 (0.1-1.1)
MPP 53.6 14/744 (1.9) 1.0
OAG AND BASELINE IOP *RR indicates relative risk; PP, perfusion pressure; CI, confidence
interval; SPP, systolic PP; DPP, diastolic PP; and MPP, mean PP.
An important contribution of this study is to provide a †Adjusting for age, sex, intraocular pressure (IOP), and IOP-
population-based measurement of the 4-year risk of or blood pressure–lowering treatment.
‡Test for trend: P = .003 for SPP; P .001 for DPP; P .001 for MPP.
OAG at various IOP levels. Although OAG developed
through-out the IOP range, risk increased steadily with
increas-ing IOP (Table 1). While high IOP was a major visual field loss had developed after treatment of sys-temic
risk fac-tor, one fourth of new OAG arose in persons hypertension.26 In BISED, the use of BP-lowering
with baseline IOP in the 13 to 19 mm Hg range; about treatment tended to decrease, not increase, the risk of OAG
half developed with IOP less than or equal to 21 mm development (Tables 2 and 4). These results are consis-tent
Hg, and two thirds developed with IOP less than or with those of our Long Island case-control study, which
equal to 25 mm Hg. Still, the magnitude of the relative found similar use of antihypertensives drugs among OAG
and attribut-able22 risks associated with high IOP cases, ocular hypertensive cases, and controls. 17
substantiate its ma-jor role in OAG development. While BISED found that hypertension decreased RR,
some studies have reported cross-sectional associations of
OAG AND BASELINE BP OAG with high BP.13,14,17-19 In the Rotterdam and Egna-
Neumarkt prevalence studies, significantly (P .05) more
A new finding from BISED is that hypertension seemed to hypertension was found in persons with high-tension OAG,
halve the RR of OAG during 4 years of follow-up; similar but not in normal-tension OAG.18,19 Similarly, cases with
results were suggested for higher SBP (Tables 2 and 3). high-tension OAG in the Long Island study had higher
These findings are consistent with the hypothesis that hy- DBP than controls17; however, after controlling for IOP, an
pertension has a protective effect on early OAG develop- in-dependent association of OAG with high BP/
ment since it maintains an adequate PP for the optic nerve. hypertension was not confirmed, thus casting doubts on the
A decrease in RR with higher DBP was not evident across role of high BP itself as a risk factor. In other case-control
the quartiles of the DBP distribution (Table 2); however, a studies of high-tension OAG that included black
decreased RR was suggested in persons with DBP of 90 participants, one study found uncontrolled systolic hy-
mm Hg and no treatment (Table 3), which is consistent pertension to be a major risk factor,13 a result not verified
with the SBP results. Since our current report reflects risk in BISED (Table 3). In another study, DBP was positively
at 4 years, further follow-up of the cohort will be valuable related to OAG, but SBP tended to have a negative rela-
to detect any changes in the relationships of BP and OAG tionship14; the latter outcome is similar to BISED find-ings.
over time. For example, long-standing hypertension may This variability in results is not surprising since the
dam-age the small vessels and eventually impair PP. relationship of BP and OAG is complex and may be af-
Another important result is that antihypertensive treat- fected by many factors, such as IOP and BP levels; extent
ment did not increase OAG risk. Such a hypothesis was of vascular damage; duration of hypertension and OAG;
advanced several years ago, based on various reports that use of BP- and IOP-lowering medications; inclusion of IOP
in the OAG definitions; hypertension definitions; selec-
tion; and other biases. As such, cross-sectional studies may
yield different results depending on the distribution of these
variables in their populations and the degree to which
analy-ses adjust for contributory factors.
If high BP were positively associated with OAG, this
relationship would be easier to detect in black popula-tions,
which have an increased prevalence of systemic hy-
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
957
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
independent effects of high IOP and low BP, which are not
explained by the contribution of the other. An additional issue
to consider is that PP can be affected by BP- and IOP-lowering
Principal Investigator
treatment, and few analyses have accounted for these effects.
M. Cristina Leske, MD, MPH Our longitudinal results, which adjusted for confounding
Coordinating Center factors, help to clarify these issues by sup-porting the role of
low PP in the development of early OAG. From our analyses,
University of New York at Stony Brook, Stony Brook, NY:
M. Cristina Leske, MD, MPH; Barbara Nemesure, PhD, the risk attributable to low PP in the multivariate model28 was
Suh-Yuh Wu, MA; Leslie Hyman, PhD; Xiaowei Li, PhD, about 30% to 40% (28% for SPP, 32% for MPP, and 41% for
Shu-Hong Xie, MS, Lixin Jiang, MS, Kasthuri Sarma, DPP), meaning that this factor could explain a substantial
Melinda Santoro, Koumudi Manthani. Data Collection portion of the OAG risk in the cohort. Possibly, persons with
Center: Ministry of Health, Bridgetown, Barbados, West OAG may have a loss of the usual balance between BP and
In-dies: Anthea M. S. Connell, FRCS, FRCOphth; Anselm IOP; in fact, an impair-ment of vascular autoregulation
Hennis, MRCP(UK), PhD, Ann Bannister, MB, BS, DO, mechanisms has been pos-tulated in these patients, with
Muthu A. Thangaraj, MB, BS, DO, Coreen Barrow; Pa- considerable clinical and ex-perimental evidence to this
tricia Basdeo, Kim Bayley, Anthanette Holder. Fundus
effect.26,29-32 The RRs for high IOP are of considerable
Pho-tography Reading Center: The Johns Hopkins
University, Baltimore, MD: Andrew P. Schachat, MD; magnitude (Table 1) and the at-tributable risks are also high22;
Judith A. Al-exander; Noreen B. Javornik, MS; Cheryl J. it is likely that both me-chanical and vascular factors play a
Hiner; Debo-rah A. Phillips; Reva Ward; Terry W. George. role.
A major strength is the BISED cohort design, based
on a population-based, nationwide random sample with
high participation. Cohort studies are the only types of
pertension and OAG. However, our baseline evalua-tions epidemiologic studies to directly measure risk and the
of the Barbados cohort, based on 302 black participants strongest type of design to detect causal relationships. 21
with prevalent OAG, found no significant associations with While losses to follow-up may lead to biased estimates of
SBP, DBP, or hypertension.16 In the Bal-timore Eye risk in cohort studies, BISED achieved a high (85%)
Survey, which included white and black par-ticipants, age- participation, with losses being mainly due to death. Aside
and race-adjusted results suggested a small association of from the older age and lower education of nonpartici-pants,
higher SBP and prevalent OAG but re-sults were not no significant differences in demographics or ma-jor
statistically significant.15 While there was no overall diagnoses were noted in participation rates; addition-ally,
association with hypertension, younger per-sons ( 60 years no differences in incidence estimates were observed after
old) with OAG tended to have less hy-pertension than adjusting for nonparticipation.22 In sum, a good rep-
controls, which was similar to our BISED results; the resentation of the original cohort was achieved, thus de-
reverse trend was only seen in persons 80 years and older. creasing the possibility of nonparticipation biases.
Possibly, this trend for a protective effect of hypertension While our 67 new cases represent the largest num-
at younger ages reflects the inclusion of per-sons with ber of population-based incident OAG cases reported as
early, recently developed OAG, who may be more far as we know, this number may not allow the detec-
comparable with the BISED incident cases than the elderly tion of modest effects and estimates based on subgroups
cases with longer disease duration. No age trends were may have high variability. These sample size issues can
evident in the BISED incidence data. Based on BISED lead to difficulties in interpreting the results of nonsig-
results, systemic hypertension does not increase (and in nificant statistical tests. As such, examination of consis-
fact decreases) the RR and is unlikely to explain the high tent trends in the data may be more revealing than rely-
OAG frequency in persons of African descent. ing on statistical significance alone.
Because this study was based on an Afro-Caribbean
OAG AND PP population with high OAG risk, questions can be raised as
to the general applicability of BISED findings. Current
A strong relationship was found between lower PP and concepts concerning racial differences in disease support
OAG risk (Table 5). These BISED results were similar to environmentally related explanations (including gene-
our previous BES findings, among which persons with low environment interactions) rather than genetic explana-tions
BP/IOP differences or low BP/IOP ratios were up to 5.5 alone.33 Investigations in populations at high risk thus offer
times more likely to have OAG than others.16 In 1983, we a special opportunity to advance knowledge on cau-
also reported that Framingham Eye Study participants with sation.23 If a disease is more frequent in a population, the
field defects had significantly low BP/IOP ratios; persons determining factors should be more common as well, thus
with definite defects had lower ratios than those with sus- making associations easier to detect. These underlying as-
pect defects or no defects.11 Low PP was also an OAG risk sociations should generally apply to the disease across eth-
factor in the Baltimore and Egna-Neumarkt prevalence nic groups since similar etiologic mechanisms would per-
studies, the Long Island case-control study, and the Bar- tain.23 In fact, no major ethnic/racial differences in OAG
bados Family Study, further confirming these find- risk factors have been reported,34 supporting the general
ings.15,17,19,27 One issue in interpreting these results is that relevance of our results.
a low PP could be explained by high IOP alone.17 How- This 4-year longitudinal study confirms the strong
ever, the analyses controlled for IOP and found a signifi- influence of high IOP on the incidence of OAG. It is im-
cantly low RR for hypertension. Our results indicate strong portant to note, however, that two thirds of cases arose
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
958
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
with IOP less than 25 mm Hg at baseline, emphasizing lence of glaucoma in a rural East African population. Invest
Ophthalmol Vis Sci. 2000;41:40-48.
the limitations of IOP as a predictor of risk. In addition 11. Leske MC, Podgor MJ. Intraocular pressure, cardiovascular risk variables,
to IOP, results support the involvement of vascular fac- and visual field defects. Am J Epidemiol. 1983;118:280-287.
tors in the risk of early OAG, with systemic hyperten- 12. Bengtsson B. The prevalence of glaucoma. Br J Ophthalmol. 1981;65:46-49.
sion having a protective effect by presumably maintain- 13. Wilson MR, Hertzmark E, Walker AM, Childs-Shaw K, Epstein DL. A
ing perfusion. Systemic hypertension at baseline case-control study of risk factors in open angle glaucoma. Arch
Ophthalmol. 1987; 105:1066-1071.
approximately halved the RR and, consistent with this
14. Katz J and Sommer A. Risk factors for primary open angle glaucoma.
finding, low PP approximately tripled the RR. There Am J Prev Med. 1988;4:110-114.
was no evidence to support the hypothesis that 15. Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC. Hypertension, perfusion pres-sure and
antihyper-tensive treatment increases OAG risk. primary open-angle glaucoma. Arch Ophthalmol. 1995;113:216-221.
16. Leske MC, Connell AMS, Wu S-Y, Hyman L, Schachat AP, and the Barbados Eye Study Group.
Further follow-up of the cohort will provide esti- Risk factors for open-angle glaucoma: The Barbados Eye Study.
mates of 9-year risk of OAG as well as evaluations of pos- Arch Ophthalmology. 1995;113:918-924.
sible changes in BP and IOP relationships over time. This 17. Leske MC, Warheit-Roberts L, Wu S-Y, and the Long Island
and future reports may assist our understanding of the Glaucoma Case-control Study Group. Open-angle glaucoma and
mechanisms leading to OAG development, with a view ocular hypertension: the Long Island Glaucoma Case-control Study
Group. Ophthalmol Epidemiol. 1996;3: 85-96.
toward preventive interventions to lower risk.
18. Dielemans I, Vingerling JR, Algra D, Hofman A, Grobbee DE, de
Jong PT. Pri-mary open-angle glaucoma, intraocular pressure, and
Submitted for publication May 31, 2001; final revision re- systemic blood pressure in the general elderly population: the
ceived September 25, 2001; accepted October 26, 2001. Rotterdam Study. Ophthalmology. 1995; 102:54-60.
This study was supported by grants EYO7625 and 19. Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto MD.
Vascular risk factors for primary open angle glaucoma: the Egna-
EYO7617 from the National Eye Institute, Bethesda, Md. Neumarkt Study. Oph-thalmology. 2000;107:1287-1293.
We thank the Barbados Eye Studies participants 20. Wu S-Y, Leske MC and the Barbados Eye Study Group.
and the Ministry of Health, Barbados, West Indies, for Associations with intraocular pressure in the Barbados Eye Study.
their role in the study. Arch Ophthalmol. 1997;115: 1572-1576.
Corresponding author and reprints: M. Cristina Leske, 21. Leske MC. Case-control and cohort studies. In: Johnson GJ,
Minassian DC, Weale RA, eds. The Epidemiology of Eye Disease.
MD, MPH, Department of Preventive Medicine, University of London, England: Chapman & Hall Ltd; 1998.
New York at Stony Brook, L3 HSC Room 086, Stony Brook, 22. Leske MC, Connell A, Wu S, et al. Incidence of open-angle
NY 11794-8036 (e-mail: cleske@notes.cc.sunysb.edu). glaucoma. Arch Oph-thalmol. 2001;119:89-95.
23. Musch DC. Insights from incidence, the Barbados Eye Studies. Arch
Ophthal-mol. 2001;119:117-118.
24. Hypertension Detection and Follow-up Program Cooperative Group. Race, edu-
cation and prevalence of hypertension. Am J Epidemiol. 1977;106:351-361.
1. Leske MC, Connell AMC, Schachat A, Hyman L, and the Barbados 25. The sixth report of the Joint National Committee on prevention,
Eye Study Group. The Barbados Eye Study: prevalence of open- detection, evalu-ation, and treatment of high blood pressure. Arch
angle glaucoma. Arch Ophthal-mol. 1994;112:821-829. Intern Med. 1997;157:2413-2445.
2. Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, Javitt J. 26. Drance SM. Glaucoma: a look beyond intraocular pressure. Am J
Racial variations in the prevalence of primary open-angle glaucoma: Ophthalmol. 1997;123:817-819.
the Baltimore Eye Survey. JAMA. 1991;266:369-374. 27. Leske MC, Nemesure B, He Q, et al Patterns of Open-Angle Glaucoma in
3. Klein B, Klein R, Sponsel WE, et al. Prevalence of glaucoma: the the Bar-bados Family Study. Ophthalmology. 2001;108:1015-1022.
Beaver Dam Study. Ophthalmology. 1992;99:1499-1504. 28. Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C. Estimating the
4. Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P. Prevalence of population attributable risk for multiple risk factors using case-control
glaucoma in the west of Ireland. Br J Ophthalmol. 1993;77:17-21. data. Am J Epide-miol. 1985;122:904-914.
5. Dielemans I, Vingerling JR, Wolfs RCW, Hofman A, Grobee DE, deJong 29. Gherghel D, Orgu¨l S, Gugleta K, Gekkieva M, Flammer J. Relationship between
PTVM. The prevalence of primary open-angle glaucoma in a population- ocular perfusion pressure and retrobulbar blood flow in patients with glaucoma
based study in the Netherlands. Ophthalmology. 1994;101:1851-1855. with progressive damage. Am J Ophthalmol. 2000;130:597-605.
6. Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia: the 30. Findl O, Rainer G, Dallinger S, et al. Assessment of optic disk blood flow in
Blue Mountains Eye Study. Ophthalmology. 1996;103:1661-1669. pa-tients with open-angle glaucoma. Am J Ophthalmol. 2000;130:589-596.
7. Cedrone C, Culasso F, Cesareo M, Zapelloni A, Cedrone P, Cerulli 31. Kerr J, Nelson P, O’Brien C. A comparison of ocular blood flow in
L. Prevalence of glaucoma in Ponza, Italy: a comparison with other untreated pri-mary open-angle glaucoma and ocular hypertension.
studies. Ophthal Epide-miol. 1997;4:59-72. Am J Ophthalmol. 1998; 126:42-51.
8. Wensor MD, McCarty CA, Stanislavsky YL, Livingston PM, Taylor 32. Drance SM, Sweeney VP, Morgan RW. Studies of factors involved in the
HR. The preva-lence of glaucoma in the Melbourne Visual pro-duction of low tension glaucoma. Ophthalmology. 1973;89:457-465.
Impairment Project. Ophthalmology. 1998;105:733-739. 33. Goodman AH. Why genes don’t count (for racial differences in
9. Shiose Y, Kitazawa Y, Tsukahara S, et al. Epidemiology of glaucoma in Japan: a health). Am J Public Health. 2000;90:1699-1702.
nationwide glaucoma survey. Jpn J Ophthalmol. 1991;35:133-155. 34. Wilson MR. Epidemiological features of glaucoma. Int Ophthalmol
10. Buhrmann RR, Quigley HA, Barron Y, West SK, Oliva MS, Mmbaga BBO. Preva- Clin. 1990; 30:153-160.
(REPRINTED) ARCH OPHTHALMOL / VOL 120, MAR 2002 WWW.ARCHOPHTHALMOL.COM
959
©2002 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/ophth/6811/ on 02/02/2017
Вам также может понравиться
- Episode 6: Deductive and Inductive Methods of Teaching: My Learning Episode OverviewДокумент10 страницEpisode 6: Deductive and Inductive Methods of Teaching: My Learning Episode OverviewJustine Elle Vijar85% (13)
- Iop HT 7Документ9 страницIop HT 7Peer TutorОценок пока нет
- Role of Hypertension As A Risk Factor OAGДокумент9 страницRole of Hypertension As A Risk Factor OAGAndhika PutraОценок пока нет
- Prospective Study of Fasting Blood Glucose and Intracerebral Hemorrhagic RiskДокумент7 страницProspective Study of Fasting Blood Glucose and Intracerebral Hemorrhagic Riskhidayatul rahmoОценок пока нет
- Chest: Postgraduate Education CornerДокумент10 страницChest: Postgraduate Education Cornerdimas adjie pangestuОценок пока нет
- Hypertensionaha 118 11819-2Документ2 страницыHypertensionaha 118 11819-2Sari RakhmawatiОценок пока нет
- What Is NTGДокумент4 страницыWhat Is NTGSonia RogersОценок пока нет
- Bjophthalmol 2018 311897.fullДокумент8 страницBjophthalmol 2018 311897.fullKrisnaОценок пока нет
- I1552 5783 60 14 4548 PDFДокумент8 страницI1552 5783 60 14 4548 PDFNetflix DheaОценок пока нет
- Accepted Manuscript: YprrvДокумент27 страницAccepted Manuscript: YprrvTiara Grhanesia DenashuryaОценок пока нет
- Ibyt 13 I 4 P 659Документ10 страницIbyt 13 I 4 P 659Sadhira GitaОценок пока нет
- Current Incidence and Outcome of The Acute Respiratory Distress SyndromeДокумент6 страницCurrent Incidence and Outcome of The Acute Respiratory Distress Syndromedarius2311Оценок пока нет
- CKD HT 3Документ8 страницCKD HT 3Peer TutorОценок пока нет
- Heart Volume Issue 2017 (Doi 10.1136 - Heartjnl-2017-312112) Ruwald, Martin H - Syncope andДокумент3 страницыHeart Volume Issue 2017 (Doi 10.1136 - Heartjnl-2017-312112) Ruwald, Martin H - Syncope andZauzaОценок пока нет
- Anemia in Heart FailureДокумент8 страницAnemia in Heart FailuremardianrnОценок пока нет
- Dci 210017Документ3 страницыDci 210017Gloria WuОценок пока нет
- A Correlational Study of Systemic Blood Pressure and IOP HL SITHOLEДокумент6 страницA Correlational Study of Systemic Blood Pressure and IOP HL SITHOLESurya Nirmala DewiОценок пока нет
- Primary Aldosteronism, Aldosterone, and Extracellular VesiclesДокумент9 страницPrimary Aldosteronism, Aldosterone, and Extracellular VesiclesYo MeОценок пока нет
- E001559 FullДокумент10 страницE001559 FullMohammad Chandra dwi pОценок пока нет
- Hypertensionaha 108 190329 PDFДокумент19 страницHypertensionaha 108 190329 PDFRJ CabaОценок пока нет
- Pulmonary Arterial Hypertension in Infants With Chronic Lung Disease: Will We Ever Understand It?Документ5 страницPulmonary Arterial Hypertension in Infants With Chronic Lung Disease: Will We Ever Understand It?Adrian KhomanОценок пока нет
- Barst RJ 2011 Pulmonary Arterial Hypertension A Comparison Between Children and AdultsДокумент13 страницBarst RJ 2011 Pulmonary Arterial Hypertension A Comparison Between Children and Adultsdr.herusetiawanОценок пока нет
- HHS Public Access: Pulmonary Hypertension in ChildrenДокумент44 страницыHHS Public Access: Pulmonary Hypertension in ChildrenLina María CañónОценок пока нет
- International Journal of Pharma and Bio Sciences: BiochemistryДокумент5 страницInternational Journal of Pharma and Bio Sciences: BiochemistryAkbar LimpoОценок пока нет
- Kent, Et Al. 2020 - StrokeДокумент5 страницKent, Et Al. 2020 - StrokeCARLOS SANTIAGO PEREZ RODRIGUEZОценок пока нет
- Chadsvasc and HasbledДокумент4 страницыChadsvasc and HasbledPGI AnaesthesiaОценок пока нет
- Oxidative Stress and Lipid Profile Among Hypertensive Patients at A Tertiary Centre in Kano, Northwest, NigeriaДокумент9 страницOxidative Stress and Lipid Profile Among Hypertensive Patients at A Tertiary Centre in Kano, Northwest, NigeriaidiОценок пока нет
- Chest: Cardiovascular Comorbidity in COPDДокумент16 страницChest: Cardiovascular Comorbidity in COPDAndry Wahyudi AgusОценок пока нет
- Hypertensive Disorders of Pregnancy and Long-Term Risk of Maternal Stroke-A Systematic Review and Meta-AnalysisДокумент21 страницаHypertensive Disorders of Pregnancy and Long-Term Risk of Maternal Stroke-A Systematic Review and Meta-AnalysisprofnutrialecuriОценок пока нет
- Control of Hypertension and Risk of Stroke Recurrence: Gary Friday, MD, MPH Milton Alter, MD, PHD Sue-Min Lai, PHD, MsДокумент7 страницControl of Hypertension and Risk of Stroke Recurrence: Gary Friday, MD, MPH Milton Alter, MD, PHD Sue-Min Lai, PHD, MsDeudeu Durotun NafisahОценок пока нет
- Traducir NeurologiaДокумент23 страницыTraducir Neurologiaclara aquino mayangaОценок пока нет
- The Journal For Nurse Practitioners: Jacqueline O'Toole, MSC, NP, Irene Gibson, Ma, RGN, Gerard T. Flaherty, MDДокумент4 страницыThe Journal For Nurse Practitioners: Jacqueline O'Toole, MSC, NP, Irene Gibson, Ma, RGN, Gerard T. Flaherty, MDGina GuisamanoОценок пока нет
- 2001 Relationship of Blood Pressure To 25-Year Mortality Due To Coronary Heart Disease, Cardiovascular Diseases, and All Causes in Young Adult MenДокумент8 страниц2001 Relationship of Blood Pressure To 25-Year Mortality Due To Coronary Heart Disease, Cardiovascular Diseases, and All Causes in Young Adult MencarlosОценок пока нет
- Prognostic Factors in Pulmonary Arterial Hypertension: Literature ReviewДокумент5 страницPrognostic Factors in Pulmonary Arterial Hypertension: Literature Reviewhuda riyambodoОценок пока нет
- Hajiaghajani 2021Документ13 страницHajiaghajani 2021Camilo HernándezОценок пока нет
- Blood Pressure and OxygenationДокумент7 страницBlood Pressure and OxygenationRoberto ZelayaОценок пока нет
- Prognostic Value of Admission Blood Glucose in Diabetic and Non-Diabetic Patients With Intracerebral HemorrhageДокумент7 страницPrognostic Value of Admission Blood Glucose in Diabetic and Non-Diabetic Patients With Intracerebral HemorrhageNur Irma SafitriОценок пока нет
- Sleep and HypertensionДокумент10 страницSleep and HypertensionPutraОценок пока нет
- Obstructive Sleep Apnoea Syndrome As A Risk Factor For Hypertension: Population StudyДокумент4 страницыObstructive Sleep Apnoea Syndrome As A Risk Factor For Hypertension: Population StudyNelson OlivarОценок пока нет
- Anemia in Heart Failure: Still Relevant?Документ8 страницAnemia in Heart Failure: Still Relevant?Hedya Nadhrati SururaОценок пока нет
- Postgradmedj 96 525Документ5 страницPostgradmedj 96 525Huda TrisenaОценок пока нет
- Latest Strategy in Renal Anemia Management in Peritoneal Dialysis PatientsДокумент5 страницLatest Strategy in Renal Anemia Management in Peritoneal Dialysis PatientsMamad TrihatmowidjoyoОценок пока нет
- Mapaennios Aha Hypertension2008Документ20 страницMapaennios Aha Hypertension2008Mr. ShadenfreudeОценок пока нет
- Pubmed 3Документ11 страницPubmed 3Adam PrabataОценок пока нет
- Chronicsubdural Hematoma: Epidemiology and Natural HistoryДокумент6 страницChronicsubdural Hematoma: Epidemiology and Natural HistoryalgoОценок пока нет
- NeldamДокумент10 страницNeldamdini hanifaОценок пока нет
- Dose-Response Association Between Physical Activity and Incident HypertensionДокумент8 страницDose-Response Association Between Physical Activity and Incident HypertensionRirin Van GobelОценок пока нет
- NTG Practical ApproachДокумент6 страницNTG Practical ApproachRasha Mounir Abdel-Kader El-TanamlyОценок пока нет
- Ooa 00229Документ4 страницыOoa 00229fatma522Оценок пока нет
- Risk Factors For Incident Retinopathy in A Diabetic and Nondiabetic Population - The Hoorn StudyДокумент8 страницRisk Factors For Incident Retinopathy in A Diabetic and Nondiabetic Population - The Hoorn StudyspaceОценок пока нет
- ArticleДокумент7 страницArticleQuentin LISANОценок пока нет
- Jurnal HTДокумент8 страницJurnal HTseruniallisaaslimОценок пока нет
- Hypertension and Hemodialysis: Pathophysiology and Outcomes in Adult and Pediatric PopulationsДокумент12 страницHypertension and Hemodialysis: Pathophysiology and Outcomes in Adult and Pediatric PopulationsinaОценок пока нет
- Righi (2016)Документ6 страницRighi (2016)PelagyalОценок пока нет
- 49 FullДокумент7 страниц49 FullPetru GlavanОценок пока нет
- PPHNДокумент6 страницPPHNHarish SudarsananОценок пока нет
- Controlled Level and Variability of Systolic Blood Pressure On TheДокумент7 страницControlled Level and Variability of Systolic Blood Pressure On TheJeanette LuevanosОценок пока нет
- Seminar: Epidemiology and Risk FactorsДокумент17 страницSeminar: Epidemiology and Risk FactorsNelly ElizabethОценок пока нет
- Effects of Different Antihypertensive Drug Combinations On Blood Pressure and Arterial StiffnessДокумент6 страницEffects of Different Antihypertensive Drug Combinations On Blood Pressure and Arterial StiffnessbimaОценок пока нет
- Hipertensión SitémicaДокумент12 страницHipertensión SitémicaIván Alejandro Trejo ValdiviezoОценок пока нет
- Modern Management of Obstructive Sleep ApneaОт EverandModern Management of Obstructive Sleep ApneaSalam O. SalmanОценок пока нет
- Nutrition in Pregnancy Royal College of Obstetricians and GynaecologistДокумент7 страницNutrition in Pregnancy Royal College of Obstetricians and GynaecologistmeikisirmanОценок пока нет
- AKP 1.2.B.2 Formulir Deteksi Dini Covid 19Документ1 страницаAKP 1.2.B.2 Formulir Deteksi Dini Covid 19meikisirmanОценок пока нет
- Jurnal Reading Retinopati Diabetik Stase MataДокумент16 страницJurnal Reading Retinopati Diabetik Stase MatameikisirmanОценок пока нет
- Refrat: Osteoarthrisis Desti Omega, S.Ked Meiki Permatasari, S.KedДокумент10 страницRefrat: Osteoarthrisis Desti Omega, S.Ked Meiki Permatasari, S.KedmeikisirmanОценок пока нет
- I Am A Filipino by Carlos RomuloДокумент7 страницI Am A Filipino by Carlos RomuloKimberly NgОценок пока нет
- AIKINS v. KOMMENDAДокумент6 страницAIKINS v. KOMMENDAMENSAH PAULОценок пока нет
- Blood TestsДокумент3 страницыBlood TestsMarycharinelle Antolin MolinaОценок пока нет
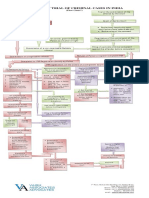
- Process of Trial of Criminal Cases in India (Flow Chart)Документ1 страницаProcess of Trial of Criminal Cases in India (Flow Chart)Arun Hiro100% (1)
- CVT / TCM Calibration Data "Write" Procedure: Applied VehiclesДокумент20 страницCVT / TCM Calibration Data "Write" Procedure: Applied VehiclesАндрей ЛозовойОценок пока нет
- Italian Companies Eastern China - JAN 2014Документ139 страницItalian Companies Eastern China - JAN 2014AndresОценок пока нет
- Coin Operated Short Movie AnalysisДокумент17 страницCoin Operated Short Movie AnalysisA 29 Nathaniela Devany MiramaОценок пока нет
- 6 Cathay vs. VazquezДокумент2 страницы6 Cathay vs. VazquezErwin BernardinoОценок пока нет
- Theory of Design 2Документ98 страницTheory of Design 2Thirumeni MadavanОценок пока нет
- JBL Tune 115TWS HeadphoneДокумент2 страницыJBL Tune 115TWS HeadphoneTimiОценок пока нет
- Assignment # (02) : Abasyn University Peshawar Department of Computer ScienceДокумент4 страницыAssignment # (02) : Abasyn University Peshawar Department of Computer ScienceAndroid 360Оценок пока нет
- Comics Trip MasterpiecesДокумент16 страницComics Trip MasterpiecesDaniel Constantine100% (2)
- Medical and Health Care DocumentДокумент6 страницMedical and Health Care Document786waqar786Оценок пока нет
- Untitled PresentationДокумент23 страницыUntitled Presentationapi-543394268Оценок пока нет
- MEM Companion Volume Implementation Guide - Release 1.1Документ23 страницыMEM Companion Volume Implementation Guide - Release 1.1Stanley AlexОценок пока нет
- 659.69 BM67 2018-02-06 02 Im Beu-UsaДокумент88 страниц659.69 BM67 2018-02-06 02 Im Beu-UsaIrakli JibladzeОценок пока нет
- Agricultural LocationДокумент26 страницAgricultural LocationPrince MpofuОценок пока нет
- Shanu Return Ticket To Sobani HostelДокумент1 страницаShanu Return Ticket To Sobani HostelTamseel ShahajahanОценок пока нет
- SMEC01 CBRS Guide For NBC Reports - v1.1Документ53 страницыSMEC01 CBRS Guide For NBC Reports - v1.1phal sovannarithОценок пока нет
- Form Seven PlacementsДокумент26 страницForm Seven PlacementsRL Iroga100% (4)
- Welcome To UnixДокумент14 страницWelcome To UnixSrinivas KankanampatiОценок пока нет
- PolygonsДокумент23 страницыPolygonsPietrelle Liana PuruggananОценок пока нет
- Huawei Videoconferencing MCU VP9600 Series Data SheetДокумент2 страницыHuawei Videoconferencing MCU VP9600 Series Data SheetIsaac PiresОценок пока нет
- Argumentative Essay-2Документ4 страницыArgumentative Essay-2api-385385980Оценок пока нет
- Room Air Conditioner: Service ManualДокумент68 страницRoom Air Conditioner: Service Manualervin0% (1)
- MVP Teacher 12Документ6 страницMVP Teacher 12Ivan ChuОценок пока нет
- Jaringan Noordin M. TopДокумент38 страницJaringan Noordin M. TopgiantoОценок пока нет
- Pineapple Working PaperДокумент57 страницPineapple Working PaperAnonymous EAineTiz100% (7)
- Prgm-Sminr Faculties Identified Through FIP NIRCДокумент9 страницPrgm-Sminr Faculties Identified Through FIP NIRCDonor CrewОценок пока нет