Академический Документы
Профессиональный Документы
Культура Документы
Pulmonary Atresia With Ventricular Septal Defect: Systematic Review
Загружено:
Ivan VeriswanОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pulmonary Atresia With Ventricular Septal Defect: Systematic Review
Загружено:
Ivan VeriswanАвторское право:
Доступные форматы
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.
99]
REVIEW ARTICLE
PULMONARY ATRESIA WITH VENTRICULAR SEPTAL
DEFECT: SYSTEMATIC REVIEW
1
Duraisamy Balaguru, M.D.; 2Muhammad Dilawar, M.D.
1
Tufts University School of Medicine, Boston, MA, USA; 2Cardiology and Cardiovascular Surgery
Department, Hamad Medical Corporation, Doha, Qatar
Introduction
ulmonary atresia with ventricular septal therefore it remains multifactorial in nature.
P defect (PA-VSD) is synonymous with
Tetralogy of Fallot-pulmonary atresia and this
defect may be considered as an extreme form of
Baltimore-Washington infant study provides us
with some pointers to the etiology of Tet-PA. In
BWIS3, 73.3% of patients with PA-VSD did not
classic Tetralogy of Fallot. Classic Tetralogy of have any associated extra-cardiac
Fallot consists of right ventricular outflow tract abnormalities. The remaining 26.7% of the
stenosis, malaligned ventricular septal defect, patients with PA-VSD had chromosomal
overriding of aorta and right ventricular abnormality, a recognizable syndrome, or other
hypertrophy. In contrast, PA-VSD consists of single organ defects. PA-VSD occurs more
atresia of right ventricular outflow tract along with often with DiGeorge syndrome and associated
remaining three features of classic Tetralogy of with Chromosome 22q11 microdeletion. Other
Fallot. Other synonyms for this defect are Type IV recognizable syndromes associated with this
truncus and Pseudotruncus. PA-VSD has been lesion include VACTER, CHARGE and Alagille
proposed by the international nomenclature syndromes. Chromosomal anomalies such as
committee of Congenital Heart Surgery Trosomy 13, Trisomy 21 and Deletion 5p have
Nomenclature and Database Project as a unifying also been reported in babies with PA-VSD. A
term1. The variabilities of pulmonary blood supply in ten-fold higher incidence of PA-VSD has been
PA-VSD make this defect heterogeneous and reported in infants of diabetic mothers
challenging for surgical repair. Relatively poorer compared to non-diabetic mothers and the
outcome for PA-VSD compared to classic incidence is 20-fold higher if diabetes was
Tetralogy of Fallot stems from the complexity of its severe enough to need treatment with insulin.
pulmonary blood supply. Strategies combining Maternal intake of benzodiazepines was
catheter-based therapies for rehabilitation of associated with congenital heart disease with an
pulmonary arteries with appropriately-timed Odds ratio of 2.15.
surgical repair have helped to achieve better
results in recent years2. III. Natural History of the disease
I. Epidemiology Early natural history reports did not address PA-
VSD separate from Tetralogy of Fallot. Limited
Baltimore-Washington Infant Study 3 (BWIS) natural history information is available for PA-VSD
recorded 4390 infants with cardiovascular group from two recent reports, though some
malformations from 1981 – 1989. Of this, 296 patients in these studies underwent surgical
(6.7%) were reported to be Tetralogy of Fallot. repair. A cohort study of 26 adults managed at
Sixty of 296 (20%) infants in the Tetralogy group UCLA (UCLA adult congenital heart disease
were Tet-PA. Tet-PA accounted for 1.4% of all registry 1978 – 1992) was studied for outcome
forms of congenital heart disease and 0.07 per during a 14 year period4. At the time of referral as
100 live births. adults, 16 of them did not have any prior surgery
and the remaining 10 have had some palliative
II. Etiology surgery (mainly systemic to pulmonary artery
shunting). All patients were symptomatic at the
Genetic, environmental, and familial factors play time of referral with cyanosis or functional
a causative role in etiology of PA-VSD and limitation.
1. Assistant Professor of Pediatrics, Tufts University School of Medicine, Boston, MA, USA.
2. Consultant Pediatric Cardiologist, Cardiology & Cardiovascular Surgery Dept. Hamad Medical Corporation & Assistant
professor of Pediatrics Weil Cornell Medical College, Doha, Qatar
Corresponding address: Duraisamy Balaguru MD, MRCP (UK), FAAP, FACC, Children's Heart Center, Children's Hospital of
New Jersey at Newark Beth Israel Medical Center, 201 Lyons Avenue, Newark, NJ 07112. dbalaguru@sbhcs.com
52 HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
Twenty of these patients had aortic IV. Pathology
regurgitation by echocardiogram and 10 of them
were classified as moderate or severe by semi- Description of pathology of this defect falls under
quantitative echocardiography. None of the two categories namely intracardiac anatomy and
patients survived beyond the third decade. This pulmonary blood supply.
is a small group of self or naturally selected
group of patients who have survived to IV.1: Intracardiac anatomy
adulthood with cyanosis and pulmonary blood
supply supported by collateral arteries. PA-VSD is characterized by atresia of both the
A recent European study5 documents the pulmonary valve and a variable length of main
outcome in 218 patients who were treated in two pulmonary artery (MPA). Ventricular septal
leading cardiac centers in London over a period defect (VSD) is an integral part of the lesion and
of 26 years (1965 – 1991) and followed up to 40 is typically large, malaligned, membranous type
years of age. This study sheds light on the and can occasionally be of the infundibular type.
course of the disease modified by state of the art There is variable degree of aortic override, and
surgical management that was available during right ventricle (RV) hypertrophy develops as a
the study period. It is notable that cardiac consequence of hemodynamic effects.
surgical therapy and catheterization techniques It should be noted that PA-VSD is different
and the understanding of the disease itself had from pulmonary atresia-intact ventricular septum
greatly improved during this study period. This (PA -IVS) in that the latter lesion has no VSD and
study however helps to set the goals for future is generally associated with hypoplastic tricuspid
management planning. valve and RV, or dilated and dysfunctional RV
Overall, 60% of infants survived to 1 year with regurgitant tricuspid valve. Generally,
highlighting the greatest attrition that occurs pulmonary artery abnormalities are not seen in
during infancy with or without palliation. Of the PA-IVS. Moreover, presence of coronary
patients who survived to 1 year, 65% lived to 10 sinusoids is a significant issue in PA-IVS. Unlike
years. Only 16% of these patients who lived up tetralogy of Fallot, coronary arteries in
to 10 years were alive at 35 years of age. PA-VSD are usually normal with a prominent
Cardiovascular complications included infective conal branch.
endocarditis (n = 17), stroke (n = 15) and RV
failure (n = 16). Aortic regurgitation has been IV.2: Pulmonary blood supply
recognized in 62% of patients by the age of 30
years. Thirty one percent of patients who Abnormalities in pulmonary artery anatomy and
underwent definitive surgical repair died within pulmonary blood supply are significant features
30 days of surgery and thirty eight percent of of PA-VSD that sets it apart from classic
them died by 3 months. There was no difference Tetralogy of Fallot. Variations in pulmonary blood
in survival up to 2 years between the patients supply makes each patient unique and warrant
who underwent definitive repair versus no individualized planning of surgical and catheter-
definitive repair. A difference was only noted based strategies. Complexity in the management
after 5 years from definitive surgery. of Tet-PA stems from the complexity of
Thus, the overall outcome in the first 3 pulmonary blood flow. The discussion of
decades of surgical approach to this lesion has pulmonary blood flow in PA-VSD includes the
not been encouraging despite significant extent of MPA atresia, patent ductus arteriosus,
progress in treatment of other complex native pulmonary arteries, aortopulmonary
congenital heart lesions. The survivors after collaterals and distal pulmonary vascular
definitive repair remain functionally well and are arborization.
less symptomatic than the non-repaired Extent of pulmonary valve atresia varies from
patients. Evolution of newer management only a plate-like atresia of the pulmonary valve to
strategies in the past two decades appears to absence of both valve and a variable length of
have considerably improved outcome. All MPA. Extension of MPA atresia to its bifurcation
patients face periodic re-operations and results in non-confluent central pulmonary
therapeutic catheterization procedures arteries (PAs). Presence or absence of confluent
throughout their life time after complete repair, PAs significantly influences surgical outcome. At
for replacement of RV – PA conduit and for birth, PDA becomes an essential source of
correction of any residual obstruction in RVOT. pulmonary blood flow when confluent pulmonary
HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61 53
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
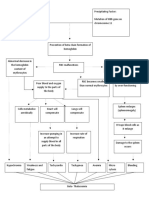
Fig.1 (Type A, B, C): Classification of PA - VSD according to the status of native pulmonary arteries (NPAs), aorto-pulmonary
collaterals (APCs) and patent ductus arteriosus (PDA).
Type A: Native pulmonary arteries present, no APCs.
Type B: Native pulmonary arteries and APCs present.
Type C: No native pulmonary arteries, only APCs maintain pulmonary blood flow.
arteries are present. In PA-VSD, PDA typically age. Color Doppler flow studies have been
originates from either the undersurface of the shown to be reliable in making this distinction
arch (67%) or from the undersurface of the between PDA and APCs based on the direction
innominate artery (33%). Unilateral PDA is of blood flow in the proximal mediastinal
usually associated with confluent PAs, while PDA segment of PAs6. Furthermore, PDA is straight
can be bilateral as is usual with non-confluent and do not branch while APCs in general, are
PAs. When PDA is present, PAs are confluent in tortuous and may branch.
80% of cases. All patients with PDA have central
PAs6. Notably, PDA is absent in 1/3 of cases and V. Classification
is associated with absent central PAs6.
Aortopulmonary collaterals (APCs) are The anatomic spectrum varies from atresia of
muscular arteries until they enter the lung pulmonary valve, presence of MPA and
parenchyma, but the muscular layer is gradually confluent normal sized PAs that are supplied by
replaced by elastic lamina that resembles true a PDA; to atresia of MPA with diminutive and/or
pulmonary arteries. APCs are seen in 30 – 65% non-confluent PAs, absent PDA and pulmonary
of patients with PA - VSD7 and are usually 2 – 6 blood supply solely provided by multiple APCs
in number. Known sites of origin of APCs include and bronchial arteries. There are several
descending thoracic aorta at the level of carina, degrees of severity in between these two
subclavian arteries, abdominal aorta, and extremes of the spectrum. Consequently, it has
coronary arteries. Sixty percent of APCs have been difficult to classify this lesion and compare
stenosis either at diagnosis or it develops over a the outcome. A practical classification has been
period of time during follow up. proposed by Congenital Heart Surgeons Society
The differentiation between PDA and APCs is based on complexity of pulmonary blood supply
important in newborns, who have balanced which in turn indicates the complexity of surgical
pulmonary blood flow and therefore, are repair1 (Figure 1).
candidates for a relatively late definitive repair. In Type A: Native PAs present, pulmonary
such patients, a reliable source of pulmonary vascular supply through PDA and no APCs.
blood flow is necessary until cardiac repair is Type B: Native PAs and APCs present
performed. PDA is considered a less reliable Type C: No native PAs, pulmonary blood
source beyond the first few days of life due to its supply through APCs only.
tendency to close. Though APCs are also prone Surgical approach for type B and C is similar
for stenosis over a period of weeks to months, except that more extensive unifocalization of
they remain patent more reliably than PDA until APCs will be needed in Type C, before the total
surgical repair is performed at few months of repair is achieved.
54 HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
VI. Evaluation of a child with PA-VSD the newborn gets older and leads to heart failure.
These infants may have only mild cyanosis and
VI.1: Clinical presentation escape recognition until later.
There is yet another subset of patients with
Approximately 65% of Tet-PA patients present to adequate and “balanced” pulmonary blood flow
a cardiac center during infancy. The remainder throughout early infancy and may present during
presents later presumably because of high late infancy. Such patients may present with a
enough pulmonary blood flow which lead to heart murmur that was heard during routine
clinically undetectable cyanosis during the early physical examination and cyanosis or heart
months of life. Overall, the modes of failure was not clinically obvious. As a general
presentation in Tet-PA consisted of cyanosis rule, in complete mixing lesions such as
(50%), heart failure (25%) or murmur with mild pulmonary atresia, systemic oxygen saturation
cyanosis with or without failure to thrive (25%)5. of 85% is achieved by Qp/Qs of at least 2.5
Newborns present with cyanosis with or (mixed venous saturation 60%). Symptoms of
without a heart murmur. Such newborns have heart failure in childhood imply a Qp/Qs ≥ 4. The
duct dependent pulmonary circulation. The so-called “balanced circulation” with
presentation occurs when the duct starts to asymptomatic infants occurs when Qp/Qs
constrict. Severe hypoxia, acidosis and shock ranges between 2.5 and 4 during infancy5.
ensues closure of PDA. If the babies had gone Failure to thrive in the absence of heart failure
home by this time, they present to the has been reported as a presenting symptom but
emergency department in extreme shock and the mechanism is unclear and can be secondary
acidosis. Typical age of presentation in this to underlying genetic abnormality.
group is 3 – 7 days. Sepsis, congenital adrenal Adult patients, either unoperated since they
hyperplasia, other duct-dependent congenital were deemed inoperable or had undergone only
heart diseases or severe illnesses affecting a palliative procedure, are infrequently seen in
other systems comprise the differential the current era. In a recent report of 26 adult
diagnosis. patients4, all were cyanotic (mean oxygen
There may or may not be a murmur which is saturation of 85%) and polycythemic (mean
typically continuous in nature representing hematocrit 57%) at presentation. They were all
aortopulmonary collateral artery flow if present. symptomatic with signs of heart failure such as
Immediate resuscitation with prostaglandin E1 effort dyspnea or decreased exercise tolerance
(PGE1) infusion will help to stabilize the patient. and were NYHA functional class II or III.
This is the type with good-sized native PAs
which are supplied by a duct. Usually, these VI.2: Physical examination
patients do not require unifocalization and are
good candidates for neonatal repair with right The severity of cyanosis depends upon the
ventricle to pulmonary artery (RV-PA) conduit. amount of pulmonary blood flow. Close clinical
However, babies with more complex pulmonary follow up with regular measurement of oxygen
blood flow tend to be less dependent on ductal saturations is essential until surgical repair is
flow since the proportion of pulmonary blood flow accomplished. On the other hand, fall of
derived via native PAs is much less than that pulmonary vascular resistance during early
derived via the APCs. If the pulmonary blood infancy allows increase in pulmonary blood flow
flow is adequate and well-balanced, these leading to heart failure and present with feeding
babies will only have mild cyanosis and will difficulty, failure to thrive, signs of respiratory
escape detection as a newborn. distress, tachypnea, tachycardia and
Presentation in early infancy occurs when the hepatomegaly. A bounding pulse in these infants
baby has “balanced circulation” with adequate is usual and signified large pulmonary blood flow
pulmonary blood flow via APCs. These babies with run-off from systemic arteries through
often present after 4 – 6 weeks of age either with APCs. Auscultation reveals the absence of
increasing cyanosis or signs of heart failure. pulmonary component of second heart sound
Development of stenosis in APCs progressively and therefore, a single S2. Continuous bruit of
reduces pulmonary blood flow causing the flow through APCs could be heard over the
progressive cyanosis. Alternatively, pulmonary chest wall. As the infancy progresses, cyanosis
over circulation occurs from the physiologic usually worsens and polycythemia and clubbing
reduction in pulmonary vascular resistance as may develop.
HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61 55
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
VI.3: Chest X ray blood flow. In newborns, presence of right
ventricular hypertrophy differentiates it from PA-
Boot shaped heart: The left heart border on chest IVS which has diminutive RV forces in the
X-ray from above downwards is constituted of anterior chest leads. However, there is less
aortic arch, main pulmonary artery, left atrial emphasis on EKG findings in the era of
appendage and left ventricular apex. In Tetralogy advanced echocardiographic technology.
of Fallot with or without pulmonary atresia, the
main pulmonary artery segment is small or VI.5: Echocardiography
absent creating a concavity below the aortic arch.
The right ventricular hypertrophy leads to upward Echocardiography is the key diagnostic modality
pointing of the cardiac apex from the right dome for the diagnosis of congenital heart diseases.
of the diaphragm. The combination of concavity While echocardiography has supplanted
at the upper mid part of the left heart border with diagnostic catheterization studies to a
the uplifting of the cardiac apex creates a boot considerable extent in the evaluation of infants
shape appearance of the cardiac silhouette on with PA-VSD, creative use of other non-invasive
chest X-ray. Right aortic arch (25 – 50%), is more modalities such as computed tomography (CT)
common in this lesion than classic Tetralogy of and magnetic resonance imaging (MRI) are
Fallot (20 – 25%) and can be diagnosed on chest increasingly used to define pulmonary blood flow.
X-ray and more precisely by echocardiogram. Echocardiography is the gold standard to
Pulmonary vascular markings have a typical delineate intracardiac defects but has limitations
reticular pattern when there are multiple for the extracardiac vascular structures. Direction
collaterals supplying the lungs. Overall extent of of blood flow in central PAs helps to differentiate
pulmonary vascular markings will depend on the PDA from APCs. The blood flow by color Doppler
extent of pulmonary blood flow. typically is antegrade if the source is PDA since
PDA joins the PA in the mediastinum while the
VI.4: Electrocardiogram collateral arteries join PAs in the lung hilum, and
hence, the flow in the central PAs will be
The EKG findings depends on the age of the retrograde. In general, if there is evidence of
patient. Right axis deviation, right ventricular significant APCs, a diagnostic catheterization
hypertrophy and possibly right atrial enlargement angiography or CT/MR angiography is generally
are usual features. Biventricular hypertrophy is performed to define the precise anatomy and
noted in patients with increased pulmolnary distribution of blood flow in the APCs.
Fig.2 (A, B): PA-VSD with confluent native pulmonary arteries (NPAs) and aortopulmonay collaterals (APCs).
A: Aortic arch angiography by pigtail in anteroposterior (AP) view showing confluent NPAs and APCs.
B: Selective left lung collateral angiography using Judkins right catheter in AP view showing retrograde filling of NPAs via the
APC that originates from descending thoracic aorta.
56 HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
VI.6: Cardiac Catheterization been closely correlated with surgical outcome. At
least 10 – 16 lung segments need to be
The technological advances in connected to the RV-PA conduit in order to have
echocardiography with color Doppler imaging satisfactory hemodynamic result after complete
over the past 2-3 decades, have diminished repair9. If the central native PAs were not
the indications for diagnostic catheterization. identified on echo, it is prudent to demonstrate
The focus of catheterization has shifted from them angiographically. Furthermore, a
making the diagnosis to filling in missing simultaneous contrast injection into the proximal
information in the diagnosis such as the stump of the pulmonary artery and the
hemodynamic data regarding pulmonary blood pulmonary vein wedge injection will help to
supply. Other specific questions unanswered define the length of discontinuity that need to be
by echocardiography such as: 1) coronary “bridged” surgically during repair10.
anatomy; 2) aorto-pulmonary collateral arteries Preoperative evaluation of adequacy of
(number, size, distribution, any stenosis and pulmonary artery size is difficult because of
blood pressure in each collateral vessel) under filling of PAs and therefore, the potential
(Figure 2: A, B); 3) confirmation of presence or size of these PAs after surgical repair is
absence of native PAs and a retrograde unpredictable. However, several pulmonary
pulmonary vein wedge injection if needed to artery indices have been developed by several
identify their presence if not clear on investigators:
aortography; 4) number of lung segments 1) McGoon's ratio: McGoon's ratio is
connected to native Pas; and 5) lung segments calculated by dividing the sum of the diameters
with dual blood supply. of RPA (at the level of crossing the lateral margin
of vertebral column on angiogram) and LPA (just
VI.7: CT / MR angiography proximal to its upper lobe branch), divided by the
diameter of aorta at the level above the
CT/MR angiography provides an alternative diaphragm [DRPA /DDTAO)+( DLPA / DDTAO)].
modality to conventional angiography to define An average value of 2.1 was noted in normal
RVOT, MPA, branch PAs and APCs8. subjects. Ratio above 1.2 is associated with
acceptable postoperative RV systolic pressure in
VI.8: Nuclear perfusion scan Tetralogy of Fallot. Ratio below 0.8 is deemed
inadequate for complete repair of PA – VSD.
Quantitative lung perfusion scan using nuclear VSD closure is deferred in such patients at the
scintigraphy is useful in defining relative time of repair or they underwent aortopulmonary
distribution of RV output to each lung and to shunt procedure as first stage11,12. However, this
individual lung segments. Such lung perfusion ratio tends to overestimate the adequacy of the
scans help to guide and gauge interventional size of PAs since this is derived using the
catheterization therapy during pulmonary arterial diameter of descending thoracic aorta at the
rehabilitation postoperatively and is generally not level of diaphragm which is frequently smaller in
helpful preoperatively in the presence of APCs. patients with PA-VSD.
2) Nakata index: Nakata PA index is
VI.9: Evaluation of adequacy of calculated from the diameter of PAs measured
pulmonary arteries immediately proximal to the origin of upper lobe
branches of the respective branch PAs13. The
The complexity of pulmonary blood supply sum of the cross sectional area (CSA) of right
determines the extent of surgical exploration and left PAs is divided by the body surface area
necessary to perform unifocalization. Eligibility of the patient [Nakata index = CSA of RPA
for complete repair is dependent on this since (mm2) + CSA of LPA (mm2)/ BSA (m2)]. A
the RV-PA conduit needs to be placed to the Nakata index of >150 mm2/m2 is acceptable for
vessel which is connected to maximum possible complete repair without prior palliative shunt14.
pulmonary vascular bed. Furthermore, closing While Nakata index is widely used in
the VSD at the time of placement of RV – PA preoperative assessment of adequacy of
conduit needs to be determined. Adequacy of pulmonary vascular bed, it is not useful in
the pulmonary vascular bed and the pulmonary patients with multifocal pulmonary blood supply,
vascular resistance are the determinants of who are evaluated for single-stage repair of PA -
postoperative RV pressure which in turn has VSD. UCSF group had proposed a total Neo-
HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61 57
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
pulmonary artery index for use in patients with vessels only. The nature of the distal pulmonary
such complex lesions. vascular bed and pulmonary vascular resistance
3) Total Neo-pulmonary artery index (TNPAI): are not expressed in these calculations. Since
Nakata index is of limited use for evaluation of these latter factors play an important role in
the adequacy of PAs in single stage repair postoperative RV pressure and in turn the
strategy where unifocalization of several APCs is hemodynamic outcome of surgical repair, an
followed by total repair at the same operation. In intraoperative method to assess the adequacy of
Nakata index, there is no provision for the pulmonary vascular bed has been proposed15.
additional vascular bed that will be added by
unifocalization. A composite index of native PAs VII. Management
and the APCs that will be unifocalized was
needed, in order to determine whether the VSD VII.1: General principles of surgical therapy of
could be closed at surgery. PA-VSD: Heterogeneity of pulmonary blood
The UCSF group proposed TNPAI in order to supply in PA-VSD precludes uniformally
help preoperative planning in these patients15. applicable management to all the patients.
Nakata PA index was measured as described However, certain guiding principles of
above. Then, APCs index was calculated by management have evolved over the past 3
addition of CSA of all significant APCs divided by decades based on earlier observations in these
the BSA. CSA of each APC was calculated from patients. Connecting as many lung segments as
diameter of the respective vessels measured on possible to the blood flow from RV during early
preoperative cineangiogram. The sum of total infancy is essential since early attrition of these
APC index and PA index is called TNPAI. A patients occurs during infancy and significant
TNPAI index >200 mm2/m2 correlated well with histologic changes occurs in pulmonary
low postoperative RV/LV pressure ratio and vasculature during young age5,9. Development of
identified patients who were clear candidates for pulmonary vascular occlusive disease from
VSD closure at the time of single-stage surgical unrestricted pulmonary blood flow from APCs
repair. These indices are limited in value since can develop as early as 4 weeks16. Recruitment
they are based on the size of the proximal of lung segments into RV-PA conduit supply is
more successful when blood flow to it is restored
early in life and complete repair should be
attempted within weeks to months during
infancy. Therapeutic catheterization procedures
such as balloon angioplasty help to rehabilitate
pulmonary arteries with stenosis and should be
combined with surgical repairs to optimize the
overall outcome.
VII.2: Components of surgical repair:
Regardless of the surgical strategy that is used
for a given patient, the components of total repair
of PA-VSD consist of (a) placement of RV - PA
conduit, (b) unifocalization of APCs and (c) VSD
closure. These components are performed in
one-stage, or at different operations depending
on the anatomy and institutional policy.
a) RV – PA conduit placement: Typically a
cadaveric, cryopreserved homograft is used to
connect right ventricle to available central
pulmonary arteries. In complex cases, where a
central pulmonary artery is absent or the
pulmonary blood flow is multifocal,
unifocalization of the diminutive native
pulmonary arteries and APCs will be performed
Fig.3: Cartoon showing repaired Pulmonary atresia - before RV – PA conduit is placed (Figure 3).
Ventricular septal defect. Right ventricle to pulmonary
artery (RV - PA) conduit is shown, VSD patch not shown in b) Unifocalization of APCs: It was shown in
the cartoon. the mid seventies that unifocalization will enable
58 HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
connecting more lung segments to central when applicable. When VSD closure is deferred
Pas17,18, and the current practice is to unifocalize at initial repair, it is surgically closed after 6 - 12
significant APCs during the first 3 months of life. months, if and when left to right shunt is
Median sternotomy is the preferred method established via the VSD with Qp/Qs exceeding
especially if single stage repair is planned. In 2:1 by catheter evaluation15.
multi stage surgical approach, unifocalization is
done through lateral thoracotomies. During VIII. Multi-stage versus single-stage
unifocalization, APCs are ligated at the origin approach
and mobilized to maximize their length with
creative rerouting. Such mobilized vessels are VIII.1: Multi-stage approach: A multi-stage
anastomosed in the mediastinum before being correction evolved from the early surgical
connected to RV-PA conduit. experiences. Inevitably, the strategy changed
c) VSD closure: Closure of VSD at the time of based on individual patient's anatomy and clinical
initial repair is desirable in order to avoid the need features. Traditional approach consisted of a
for further surgery. However, if there were any palliative shunt in all patients (patients with “good
concerns about the adequacy of the pulmonary size”, confluent central PA in particular) during
vascular bed, it is customary to defer VSD neonatal period or early infancy to relieve
closure. Leaving the VSD unrepaired, helps to cyanosis and allow for growth of distal pulmonary
avoid supra-systemic RV pressure in the arteries. However, with diminutive PAs, RV – PA
immediate postoperative period by allowing RV to continuity is established by placing a RV – PA
decompress through the VSD. Over a period of conduit. This provides catheter access to
months, pulmonary vascular development occurs peripheral PAs to perform balloon angioplasty of
and the VSD can be closed safely with sub- the pulmonary arteries. The VSD is typically left
systemic RV pressure. The strategy of delayed open at this first stage. Any possible
VSD closure has reduced the operative mortality. unifocalization of APCs will also be performed.
With the single stage surgical repair strategy it A subsequent operation will be done to close
is important to ensure that pulmonary the VSD, relieve any residual right ventricular
vasculature is adequate, both in diameter of outflow tract obstruction and place a valved
proximal pulmonary vessels and development of conduit. With absent mediastinal PAs, the
distal pulmonary vascular bed, for the safe surgical approach is further complicated. Two
closure of VSD. Preoperative PA indices modified Blalock Taussig shunts are performed
mentioned earlier help to assess the adequacy to each PA via bilateral thoracotomies.
of PA size and the nature of distal pulmonary Unifocalization of any significant APCs will be
vascular bed that is connected to central PAs. preformed. Each thoracotomy is done during the
However when a single-stage repair strategy same hospitalization but separated by few days.
is adopted with unifocalization of APCs at the This will relieve cyanosis and allow growth of
same operation, preoperatively-determined PA native pulmonary arteries. The babies would
indices will not be able to predict the level of have catheter evaluation prior to next operation.
pulmonary vascular bed added by unifocalization The second operation will consist of RV – PA
of APCs. Therefore, an intraoperative method to homograft, connection of all branches of PA with
evaluate adequacy of pulmonary vascular bed or without VSD closure. Modifications to above
was proposed by the UCSF group15. After mentioned generalized outlines will be made
completion of unifocalization and distal dependent upon individual patient's condition.
anastamosis of RV - PA conduit, a perfusion VIII.2: Single-stage approach: Current
cannula and a PA catheter are inserted from the surgical approach attempts to perform APCs
proximal end of the conduit and left atrial vent is unifocalization and cardiac repair at the same
placed. The conduit is connected to the bypass operation, through median sternotomy. The
machine. The bypass machine is run at choice between multi-stage and single-stage
increasing flow rates to 2.5 L/min/m2 and the PA repair is dependent on various factors: Nature of
pressure is monitored. VSD is closed if the mean PAs (small vs. good size), (duct-dependent or
conduit pressure is < 25 mmHg, and left open if collateral-dependent PBF), age of the patient at
it is higher. Alternative strategy in borderline presentation, status of APCs, and availability of
cases is to close the VSD with a fenestrated surgical skills and results of the institution.
patch and the fenestration can be closed later Newborns with no PDA and adequate collateral
either by surgery or transcatheter technique, dependent pulmonary blood supply with
HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61 59
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
acceptable systemic oxygen saturations, are the Aortic regurgitation (AR) develops in a significant
typical candidates for elective single-stage number of patients with or without complete
unifocalization and cardiac repair that is surgical repair. Development of AR occurs more
performed at about 3 months of age. often with patients who had palliative shunts only
VIII.3: Comparison of outcome between multi since they add to the LV volume overload and
and single-stage repair: Several theoretical therefore LV dilatation. The resultant aortic
advantages of the single-stage approach over the annular dilatation worsens aortic regurgitation.
more traditional multi-stage approach exist. Single Infective endocarditis affecting aortic valve is
stage repair allows for early normalization of another mechanism of AR. Progressive LV
cardiovascular physiology by recruitment of all dilatation due to volume overload from AR,
possible lung segments into RV derived circulation systemic to pulmonary artery shunt or collateral
as early in life as possible. This alleviates cyanosis flow eventually leads to LV dysfunction.
and polycythemia during infancy. Early repair also In patients who have had complete repair, there
preserves pulmonary vascular bed and avoids is a gradual deterioration of conduit function23 from
development of pulmonary vaso-occlusive disease loss of luminal diameter, calcification, peel
in the lung segments exposed to systemic formation and from the deterioration of valve
pressure via APCs, and hypoplasia of the distal function. The valve in the conduit is prone for
pulmonary vasculature in under-perfused lung calcification, stenosis and regurgitation.
segments. There is also evidence to suggest that Pulmonary regurgitation worsens with any residual
long term cardiac function is preserved by avoiding stenosis in distal pulmonary arteries. While
ventricular dysfunction from prolonged cyanosis pulmonary regurgitation is well tolerated for years,
and arrhythmias19. When we compare outcome RV dilatation and hypertrophy eventually ensues
between patients treated in same surgical era20, 21, leading to RV dysfunction24. There is evidence that
the ultimate results are comparable but patients in RV dilatation with dysfunction can eventually
the single stage group undergo one or two impact LV function by ventricle-ventricle
operations less than the patients in multi-stage interaction. However, optimal timing of re-
group do. operation either to replace the deteriorated conduit
or implantation of pulmonary valve to stop
IX. Complementary role of pulmonary regurgitation is still unclear.
interventional catheterization Development of ventricular arrhythmias has been
documented after tetralogy repair. This is thought
Interventional catheterization has assumed an to account for the relatively high incidence of
important complementary role in rehabilitation of sudden deaths noted in patients long after
pulmonary arteries in the management of tetralogy repair. Co-existing poor hemodynamic
patients with PA - VSD by the use of balloon parameters such as high RV pressure is thought to
angioplasty and stent placements 22. be a risk factor for arrhythmias. Correction of
Catheterization helped avoiding surgery in case hemodynamic abnormalities by pulmonary valve
of stenosis in proximal segments of the PAs and implantation or replacement of RV – PA conduit is
by being able to reach distal stenosis within lung expected to help reduce this risk25. The outcome
parenchyma that are inaccessible to the from the current modified approach combining
surgeon. Coil occlusion of APCs, stent surgery and therapeutic cardiac catheterization
placement in RVOT and palliative stenting of techniques has improved the outcome and long
stenotic APCs are some of the other procedures term studies in future will provide proof of such
that interventional catheterization has to offer to improved outcome.♦
the patients with PA – VSD.
References:
X. Long term sequelae/outcome
1. Tchervenkov CI, Roy N. Congenital heart
Many of the long term sequelae have been disease nomenclature and database project:
mentioned earlier under the natural history Pulmonary atresia - ventricular septal defect. Ann
section. Patients who were unsuitable for Thoracic Surg 2000; 69:S97-S105.
complete surgical repair and therefore were 2. McElhinney DB; Reddy MV; Hanley FL.
palliated with systemic to pulmonary artery Tetralogy of Fallot with major aortopulmonary
shunts only, develop progressive cyanosis and collaterals: Early total repair. Pediatric Cardiology
polycythemia as they survive into adulthood. 1998;19:289-296.
60 HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61
[Downloaded free from http://www.heartviews.org on Tuesday, October 30, 2018, IP: 114.6.181.99]
Pulmonary Atresia with Ventricular Septal Defect: Systematic Review
3. Malformations of the cardiac outflow tract, in 215-234.
Ferencz C, Loffredo CA, Correa-Villasenor A, 15. Reddy MV, Petrossian E, McElhinney DB, Moore
Nathan PD (eds): Genetic, environmental risk P, Teitel DF, Hanley FL: One stage complete
factors for major cardiovascular malformations. unifocalization in infants: When should the
The Baltimore-Washington Infant Study 1981- ventricular septal defect be closed? J Thorac
1989. Armonk,NY, Futura Publishing Company, Cardiovasc Surg 1997;113:858-868.
1997, pp 59-102. 16. Reddy MV, Wong J, Liddicoat JR, et al.: Altered
4. Marelli AJ, Perloff JK, Child JS, Laks H. endothelium dependent responses in lambs with
Pulmonary atresia with ventricular septal defect pulmonary hypertension and increased
in adults. Circulation 1994;89:243-251. pulmonary blood flow. American Journal of
5. Bull C, Somerville J; Ty E, Spiegelhalter D: Physiology 1996;271:H562-H570.
Presentation and attrition in complex pulmonary 17. Haworth SG, Macartney FJ: Growth and
atresia. J AM COLL CARDIOL 1995;25:491-499. development of pulmonary circulation in
6. Acherman RJ, Smallhorn JF, Freedom RM. pulmonary atresia with ventricular septal defect
Echocardiographic assessment of pulmonary and major aortopulmonary collateral arteries. Br
blood supply in patients with pulmonary atresia Heart J 1980;44:14-24.
and ventricular septal defect. J AM COLL 18. Haworth SG, Rees PG, Taylor JFN, et al.:
CARDIOL 1996;28:1308-1313. Pulmonary atresia with ventricular septal defect
7. Hofbeck M, Sunnegardh J, Burrows PE, et al.: and major aortopulmonary collateral arteries. Br
Analysis of survival in patients with pulmonic Heart J 1981;45:133-141.
valve atresia and ventricular septal defect. Am J 19. Joffe H, Georgakopoulos D, Celermajer DS, et
Cardiol 1991;67:737-743. al.: Late ventricular arrhythmia is rare after early
8. Holmqvist C, Hochberg P, Bjorkhem G, Laurin S. repair of tetralogy of Fallot.[see comments]. J Am
Pre-operative evaluation with MR in tetralogy of Coll Cardiol 1994;23:1146.
Fallot and pulmonary atresia with ventricular 20. Tchervenkov CI, Salasidis G, Cecere R, Beland
septal defect. Acta Radiologica 2001;42:63-69. MJ, Jutras L, Paquet M, Dobell ARC: One-stage
9. Shimazaki Y, Tokusan Y, Lio M, Nakano S, et al. midline unifocalization and complete repair in
Pulmonary artery pressure and resistance late infancy versus multiple-stage unifocalization
after repair of tetralogy of Fallot with pulmonary followed by repair for complex heart disease with
atresia. J Thorac Cardiovasc Surg 1990;100:425- major aortopulmonary collaterals. J Thorac
440. Cardiovasc Surg 1997;114:727-737.
10. Liao P-K, Edwards WD, Julsrud PR, Puga FJ, 21. Murthy KS, Rao SG, Krishnanaik S, Coelho R,
Danielson GK, Feldt RH: Pulmonary blood Krishnan US, Cherian KM: Evolving surgical
supply in patients with pulmonary atresia and management for ventricular septal defect, pulmonary
ventricular septal defect. J Am Coll Cardiol atresia, and major aortopulmonary collateral arteries.
1985;6:1343-1350. Ann Thoracic Surg 1999;67:760-764.
11. Piehler JM, Danielson GK, McGoon DC, Wallace 22. Interventional cardiac catheterization in the
RB, Fulton RE, Mair DD. Management of management of pulmonary atresia with
pulmonary atresia with ventricular septal defect ventricular septal defect and aorto-pulmonary
and hypoplastic pulmonary arteries by right collaterals. Radtke,W., Balaguru, D. Cardiology
ventricular outflow construction. J Thorac in the Young 2000; 10 (Suppl 2): 48.
Cardiovasc Surg 1980;80:552-567. 23. Salim MA, DiSessa TG, Alpert BS, Arheart KL,
12. Blackstone EH, Kirklin JK, Bertranou EG, Labrosse Novick WM, Watson DC: The fate of homograft
CJ, Soto B, Bargeron Jr. LM. Preoperative conduits in children with congenital heart
prediction from cineangiograms of postrepair right disease: An angiographic study. Ann Thoracic
ventricular pressure in Tetralogy of Fallot. J Thorac Surg 1995;59:67-73.
Cardiovasc Surg 1979;78:542-552. 24. Ovaert C, Caldarone CA, McCrindle BW,
13. Nakata S, Imai Y, Takanashi Y, Kurosawa H, Nykanen DG, Freedom RM, Coles JG, Williams
Tezuka K, Nakazawa M, Ando M, Takao A: A WG, Benson LN: Endovascular stent
new method for the quantitative standardization implantation for the management of
of cross-sectional area of the pulmonary arteries postoperative right ventricular outflow tract
in congenital heart diseases with decreased obstruction: Clinical efficacy. J Thorac
pulmonary blood flow. J Thorac Cardiovasc Surg Cardiovasc Surg 1999;118:886 - 893.
1984;88:610-619. 25. Therrien J, Siu SC, Harris L, Dore A, Niwa K,
14. AnonymousTetralogy of Fallot., in Castaneda Janousek J, Williams WG, Webb GD, Gatzoulis
AR, Jonas RA, Mayer JE, Hanley FL (eds): MA: Impact of pulmonary valve replacement on
Cardiac surgery of the neonate and infant. arrhythmia propensity late after repair of Tetralogy
Philadelphia, W.B.Saunders Company, 1994, pp of Fallot. Circulation 2002;103:2489-2494.
HEART VIEWS VOLUME 8 NO.2 JUNE–AUGUST 2005:52–61 61
Вам также может понравиться
- Problem-based Approach to Gastroenterology and HepatologyОт EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisОценок пока нет
- Hereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- CPG Managment of Neonatal Jaundice (Second Edition) NewДокумент62 страницыCPG Managment of Neonatal Jaundice (Second Edition) NewHafiz HamidiОценок пока нет
- Albendazole in PediatricsДокумент38 страницAlbendazole in PediatricsKishore ChandkiОценок пока нет
- Oral Cases Study Guide - PediatricsДокумент68 страницOral Cases Study Guide - PediatricsJohn100% (1)
- Masalah Gastrointestinal KolestasisДокумент21 страницаMasalah Gastrointestinal KolestasisMuthi'ah Ramadhani AgusОценок пока нет
- Ob SGDДокумент88 страницOb SGDFerdinand Luis SuarezОценок пока нет
- Hepatitis VirusДокумент37 страницHepatitis Virusapi-19916399Оценок пока нет
- Necrotizing Enterocolitis ProtocolДокумент3 страницыNecrotizing Enterocolitis Protocoleddy riachyОценок пока нет
- Neonatal Hepatitis SyndromeДокумент18 страницNeonatal Hepatitis Syndromeenny_rommyОценок пока нет
- DiarrheaДокумент38 страницDiarrheaSTEPHANIE SOR100% (1)
- Renal Failure and Pancytopenia Linked to HyperparathyroidismДокумент3 страницыRenal Failure and Pancytopenia Linked to HyperparathyroidismIvan VeriswanОценок пока нет
- Hemorrhagic Conditions in Neonates: DR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUДокумент27 страницHemorrhagic Conditions in Neonates: DR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUAbdisalan hassanОценок пока нет
- Celiac Disease in ChildrenДокумент59 страницCeliac Disease in Childrend-fbuser-57045067Оценок пока нет
- The Effectiveness of Educational Program On Nurses' Competencies Regarding Pre-Eclampsia Care in Three Hospitals in Sudan2021Документ6 страницThe Effectiveness of Educational Program On Nurses' Competencies Regarding Pre-Eclampsia Care in Three Hospitals in Sudan2021International Journal of Innovative Science and Research Technology100% (1)
- Beta ThalassaemiaДокумент10 страницBeta ThalassaemiaJoyce TeoОценок пока нет
- Henoch Schonlein Purpura REVДокумент42 страницыHenoch Schonlein Purpura REVBayu Kurniawan100% (1)
- Clinical Management: PGI Eileen Andres PediatricsДокумент9 страницClinical Management: PGI Eileen Andres PediatricsMichael BonillaОценок пока нет
- Stevens Johnson DiseaseДокумент5 страницStevens Johnson DiseaseShammy RNОценок пока нет
- VOD - SOS in HSCTДокумент25 страницVOD - SOS in HSCTKim-Thinh Nguyen ThiОценок пока нет
- Approach To Neonatal HyperbilirubinemiaДокумент34 страницыApproach To Neonatal HyperbilirubinemiaNilesh HatzadeОценок пока нет
- Shoulder DystociaДокумент11 страницShoulder DystociaYulvina IjieОценок пока нет
- Congenital and Childhood Atrioventricular Blocks: Pathophysiology and Contemporary ManagementДокумент14 страницCongenital and Childhood Atrioventricular Blocks: Pathophysiology and Contemporary ManagementIvan VeriswanОценок пока нет
- Pediatric History TemplateДокумент3 страницыPediatric History TemplateJoel TamayoОценок пока нет
- Case Presentation-ChickenpoxДокумент41 страницаCase Presentation-ChickenpoxShaliniОценок пока нет
- CPG Childhood ImmunizationДокумент25 страницCPG Childhood ImmunizationLady Nur StarkОценок пока нет
- Pediatrics in Review 2013 Friedman 328 30Документ5 страницPediatrics in Review 2013 Friedman 328 30Enrique CaballéОценок пока нет
- Preterm Prelabour Rupture of MembranesДокумент12 страницPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanОценок пока нет
- Care for Babies with ABO IncompatibilityДокумент56 страницCare for Babies with ABO IncompatibilityJonathan DiazОценок пока нет
- Detecting Dengue Hemorrhagic FeverДокумент4 страницыDetecting Dengue Hemorrhagic FeverPatrick DeeОценок пока нет
- Newborn NotesДокумент44 страницыNewborn NotesHaziq KamardinОценок пока нет
- Approach To The Child With Anemia - UpToDateДокумент41 страницаApproach To The Child With Anemia - UpToDateDaniel Enrique CardenasОценок пока нет
- Neonatal Sepsis Diagnosis and TreatmentДокумент18 страницNeonatal Sepsis Diagnosis and TreatmentFãhâd Õró ÂhmédОценок пока нет
- 1 - Presentation - Management of Preclamplsia, Mild and ModerateДокумент22 страницы1 - Presentation - Management of Preclamplsia, Mild and ModeratesharonОценок пока нет
- Abruptio Placenta B-1Документ29 страницAbruptio Placenta B-1drsachinhОценок пока нет
- Ovarian Cysts and Cancer in PregnancyДокумент15 страницOvarian Cysts and Cancer in Pregnancykarina100% (1)
- IntussusceptionДокумент33 страницыIntussusceptionNovendi RizkaОценок пока нет
- Are Viruses Living or Non-Living Organisms?Документ8 страницAre Viruses Living or Non-Living Organisms?Sydney Cloyce NagalОценок пока нет
- Pediatrics 2 LaboratoryДокумент40 страницPediatrics 2 LaboratoryAmaetenОценок пока нет
- Causes and Symptoms of Beta-ThalassemiaДокумент1 страницаCauses and Symptoms of Beta-ThalassemiaAngie LamoОценок пока нет
- Oral Revalida Im Cases Dec. 12 and 13 2020Документ16 страницOral Revalida Im Cases Dec. 12 and 13 2020Bea Y. Bas-ongОценок пока нет
- Anemia of PrematurityДокумент14 страницAnemia of PrematurityMariel HuamancayoОценок пока нет
- Vitamin K Shot Prevents Bleeds in BabiesДокумент11 страницVitamin K Shot Prevents Bleeds in BabiesLucky PuspitasariОценок пока нет
- Neonatal Cholestasis GuideДокумент28 страницNeonatal Cholestasis GuideHafsaJabbarОценок пока нет
- Malnutrition in Children For PDR III - PediaДокумент24 страницыMalnutrition in Children For PDR III - PediaJaniel King100% (1)
- Neonatalhypoglycemia: Is There A Sweet Spot?Документ14 страницNeonatalhypoglycemia: Is There A Sweet Spot?karisman kadirОценок пока нет
- Idiophatic Thrombocytopenic Purpura (ITP) in PregnancyДокумент27 страницIdiophatic Thrombocytopenic Purpura (ITP) in PregnancyAdietya Bima PrakasaОценок пока нет
- Congenital Rubella Syndrome-Case ReportДокумент4 страницыCongenital Rubella Syndrome-Case ReportErlina WahyuОценок пока нет
- POLYCYTHEMIAДокумент29 страницPOLYCYTHEMIAFaizan KhanОценок пока нет
- Graves' Disease Symptoms and TreatmentДокумент29 страницGraves' Disease Symptoms and Treatmentanon_414347743Оценок пока нет
- Congenital Adrenal HyperplasiaДокумент29 страницCongenital Adrenal HyperplasiaMohan RaoОценок пока нет
- Anatomic Disorders of Female Reproductive SystemДокумент42 страницыAnatomic Disorders of Female Reproductive SystemNelly AstikaОценок пока нет
- Neurological Deseases in PregnancyДокумент6 страницNeurological Deseases in PregnancyOdi KaiОценок пока нет
- Kawasaki Disease DiagnosisДокумент5 страницKawasaki Disease DiagnosisFranz SalazarОценок пока нет
- Epilepsy in Pregnancy JatuДокумент57 страницEpilepsy in Pregnancy Jatuninjahattori1Оценок пока нет
- Approach To FeverДокумент80 страницApproach To FeverRaditia AbrahamОценок пока нет
- Vitamin B12 Deficiency and A Patient Case StudyДокумент36 страницVitamin B12 Deficiency and A Patient Case Studynherm6425100% (1)
- PreeclampsiaДокумент14 страницPreeclampsiaHenny NovitasariОценок пока нет
- Maternal Collapse During PregnancyДокумент57 страницMaternal Collapse During PregnancytapayanaОценок пока нет
- TMP 18829-E354.full91399039Документ7 страницTMP 18829-E354.full91399039Cordova ArridhoОценок пока нет
- High-Dose Oral Ibuprofen in Treatment of Patent Ductus Arteriosus in Full-Term NeonatesДокумент5 страницHigh-Dose Oral Ibuprofen in Treatment of Patent Ductus Arteriosus in Full-Term NeonatesIvan VeriswanОценок пока нет
- Neonatal Hypoglycemia: Jane E. Mcgowan, MDДокумент12 страницNeonatal Hypoglycemia: Jane E. Mcgowan, MDIvan VeriswanОценок пока нет
- Renal Failure and Pancytopenia Linked to HyperparathyroidismДокумент3 страницыRenal Failure and Pancytopenia Linked to HyperparathyroidismIvan VeriswanОценок пока нет
- Piis0002934313005986 PDFДокумент2 страницыPiis0002934313005986 PDFIvan VeriswanОценок пока нет
- Reference Range Values For Pediatric Care-2nd PDFДокумент202 страницыReference Range Values For Pediatric Care-2nd PDFIvan Veriswan67% (3)
- SDQ Behavioral ScreeningДокумент7 страницSDQ Behavioral ScreeningIvan VeriswanОценок пока нет
- English ReportДокумент29 страницEnglish ReportWasuchon ChaichanОценок пока нет
- Hipertensi Pada AnakДокумент21 страницаHipertensi Pada AnakRanti Apriliani PutriОценок пока нет
- Piis0002934313005986 PDFДокумент2 страницыPiis0002934313005986 PDFIvan VeriswanОценок пока нет
- Hhs Public Access: Non-Ige Mediated Food Allergy SyndromesДокумент7 страницHhs Public Access: Non-Ige Mediated Food Allergy SyndromesIvan VeriswanОценок пока нет
- The Role of Echocardiography in Diagnosis, Monitoring Closure and Post Procedural Assessment of Patent Foramen OvaleДокумент9 страницThe Role of Echocardiography in Diagnosis, Monitoring Closure and Post Procedural Assessment of Patent Foramen OvaleIvan VeriswanОценок пока нет
- Etiology of Hemoptysis in Children PDFДокумент4 страницыEtiology of Hemoptysis in Children PDFAnantaBenvenutoОценок пока нет
- Evaluation and Treatment of Functional.24Документ17 страницEvaluation and Treatment of Functional.24Asri RachmawatiОценок пока нет
- American Journal of GastroenterologyДокумент6 страницAmerican Journal of GastroenterologyIvan VeriswanОценок пока нет
- TSC 1Документ36 страницTSC 1Ivan VeriswanОценок пока нет
- Guidelines For HMD Design: April 2009Документ45 страницGuidelines For HMD Design: April 2009Ivan VeriswanОценок пока нет
- Casie Mcginness Chelsie Michael Wenatchee High SchoolДокумент22 страницыCasie Mcginness Chelsie Michael Wenatchee High SchoolAbd AphedОценок пока нет
- Mehta2009 PDFДокумент18 страницMehta2009 PDFIvan VeriswanОценок пока нет
- Jurding 3-Fecal MicrobiotaДокумент9 страницJurding 3-Fecal MicrobiotaYessi OktaviantiОценок пока нет
- Pediatric Constipation in The EmergencyДокумент7 страницPediatric Constipation in The EmergencyIvan VeriswanОценок пока нет
- Tuberous Sklerosis Pada Anak: Sandra Ayamiseba Pieter L. SulingДокумент6 страницTuberous Sklerosis Pada Anak: Sandra Ayamiseba Pieter L. SulingIvan VeriswanОценок пока нет
- Nihms 630882Документ16 страницNihms 630882ika yunidasariОценок пока нет
- WHO CG Annex 1Документ2 страницыWHO CG Annex 1DaychiОценок пока нет
- Mehta2009 PDFДокумент18 страницMehta2009 PDFIvan VeriswanОценок пока нет
- Tuberous Sklerosis Pada Anak: Sandra Ayamiseba Pieter L. SulingДокумент6 страницTuberous Sklerosis Pada Anak: Sandra Ayamiseba Pieter L. SulingIvan VeriswanОценок пока нет
- Roach 2004Документ8 страницRoach 2004Ivan VeriswanОценок пока нет
- Liver InjuryДокумент10 страницLiver InjuryIvan VeriswanОценок пока нет
- Congenital and Childhood Atrioventricular Blocks: Pathophysiology and Contemporary ManagementДокумент14 страницCongenital and Childhood Atrioventricular Blocks: Pathophysiology and Contemporary ManagementIvan VeriswanОценок пока нет
- 2015 SVT Toolkit ReferenceCardДокумент2 страницы2015 SVT Toolkit ReferenceCardbonne_ameОценок пока нет
- Cardiac arrest outcomes in COVID-19 patientsДокумент13 страницCardiac arrest outcomes in COVID-19 patientsyuni ayu lestariОценок пока нет
- Fibrilacioni Atrial Trajtimi Dhe Diagnoza e TijДокумент8 страницFibrilacioni Atrial Trajtimi Dhe Diagnoza e TijMarsiano QendroОценок пока нет
- The Ehra Book of Intervntional Electrophysiology - OxfordДокумент321 страницаThe Ehra Book of Intervntional Electrophysiology - Oxfordmorris njageОценок пока нет
- Eaton County Apparent Drowning Death UnidentifiedДокумент5 страницEaton County Apparent Drowning Death UnidentifiedFergus BurnsОценок пока нет
- Understanding The Dimensions in EchocardiographyДокумент10 страницUnderstanding The Dimensions in EchocardiographyGeorge ThomasОценок пока нет
- PATHOLOGY LE3-mergedДокумент18 страницPATHOLOGY LE3-mergedNdor BariboloОценок пока нет
- Electrical Safety TestsДокумент29 страницElectrical Safety TestsJaniceMujah100% (1)
- Seminar On Mobile Coronary Care UnitДокумент11 страницSeminar On Mobile Coronary Care UnitASIR DHAYANI95% (19)
- Bob BACK Protocol PDFДокумент53 страницыBob BACK Protocol PDFMihaela VasilutaОценок пока нет
- Seeking Closure For Pda - Neonatal Care UpdateДокумент46 страницSeeking Closure For Pda - Neonatal Care Updateapi-602288180Оценок пока нет
- Fluid and Electrolytes Case StudyДокумент2 страницыFluid and Electrolytes Case StudyJamie Wiebe100% (8)
- Pathologt of The HeartДокумент40 страницPathologt of The HeartJudithОценок пока нет
- Effect of Vedic Mantra Treatment in Reduction of Depressive Syndrome and AnxietyДокумент4 страницыEffect of Vedic Mantra Treatment in Reduction of Depressive Syndrome and AnxietymaninagaОценок пока нет
- Powerpoint The HeartДокумент13 страницPowerpoint The HeartjavadkollamОценок пока нет
- Vimalraj Bogana Shanmugam, 2015Документ11 страницVimalraj Bogana Shanmugam, 2015Tony Santos'sОценок пока нет
- Nice 2016Документ85 страницNice 2016Diana ToroОценок пока нет
- Soal Imspq 2015Документ9 страницSoal Imspq 2015AgungBudiPamungkasОценок пока нет
- RevolutionДокумент32 страницыRevolutiondoggy2178100% (4)
- Heart Failure with Normal Ejection FractionДокумент19 страницHeart Failure with Normal Ejection FractionFarhan HasbiОценок пока нет
- Respiration, Muscles and The Internal EnvironmentДокумент11 страницRespiration, Muscles and The Internal Environmentmii chanrОценок пока нет
- Anatomy of Chest PDFДокумент61 страницаAnatomy of Chest PDFRizwan QureshiОценок пока нет
- 4th Term - G8 Daily Test (Biology) - MSДокумент17 страниц4th Term - G8 Daily Test (Biology) - MSMatthew EdbertОценок пока нет
- The Living Embryo and Making of Whole Mounts 72Документ7 страницThe Living Embryo and Making of Whole Mounts 72joemark_narsico5796100% (1)
- Shazia Kazi ResumeДокумент2 страницыShazia Kazi Resumeshazia kaziОценок пока нет
- SS1 1ST Term Animal Husbandry E-NoteДокумент29 страницSS1 1ST Term Animal Husbandry E-Notekanajoseph2009Оценок пока нет
- FEU Review Pre Board Exam 2016 NeoPediaДокумент9 страницFEU Review Pre Board Exam 2016 NeoPediaDharlyn MungcalОценок пока нет
- Biology-Igcse FULL NotesДокумент63 страницыBiology-Igcse FULL NotesSameer Abu Munshar100% (5)
- Pulmonary EdemaДокумент2 страницыPulmonary EdemaMuhammad Bayu Zohari HutagalungОценок пока нет
- Clinical Case 1Документ31 страницаClinical Case 1reginaОценок пока нет
- 24 de AgostoДокумент7 страниц24 de Agostoapi-626131140Оценок пока нет