Академический Документы
Профессиональный Документы
Культура Документы
Peptic Ulcer Disease
Загружено:
Chino Paolo SamsonОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Peptic Ulcer Disease
Загружено:
Chino Paolo SamsonАвторское право:
Доступные форматы
GROUP
C2
Physiology Laboratory
Small Group Discussion
Output
March 9, 2016
[PEPTIC ULCER DISEASE]
By: ASUBARIO, Olufunmilola Omonike; BALADAD, Alvin Byron; DE JESUS, Chrislou; GURUNG, Man
Bahadur; KALANYEG, Kristie; MAHALEE, Naphitcharak; MONTHATHONG, Thanapol; PANLASIGUI,
Rikkimae Maria; SAMSON, Chino Paolo; SOLONIO, Natalie Keith; VALDEZ, Gregorio
PEPTIC ULCER DISEASE
Peptic ulcer disease (PUD), also known
as a peptic ulcer or stomach ulcer, is a break in
the lining of the stomach, first part of the small
intestine, or occasionally the lower esophagus. An
ulcer in the stomach is known as a gastric
ulcer while that in the first part of the intestines is
known as a duodenal ulcer. The most common
symptoms are waking at night with upper
abdominal pain or upper abdominal pain that
improves with eating. The pain is often described
as a burning or dull ache. Other symptoms include
Deep gastric ulcer belching, vomiting, weight loss, or poor appetite.
About a third of older people have no symptoms.
Complications may include bleeding, perforation,
and blockage of the stomach. Bleeding occurs in
as many as 15% of people.
EPIDEMIOLOGY
In the United States, PUD affects approximately 4.5 million people annually.
Approximately 10% of the US population has evidence of a duodenal ulcer at some
time. Of those infected with H pylori, the lifetime prevalence is approximately 20%. Only
about 10% of young persons have H pylori infection; the proportion of people with the
infection increases steadily with age.
Overall, the incidence of duodenal ulcers has been decreasing over the past 3-4
decades. Although the rate of simple gastric ulcer is in decline, the incidence of
complicated gastric ulcer and hospitalization has remained stable, partly due to the
concomitant use of aspirin in an aging population. The hospitalization rate for PUD is
approximately 30 patients per 100,000 cases.
The prevalence of PUD has shifted from predominance in males to similar
occurrences in males and females. Lifetime prevalence is approximately 11-14% in men
and 8-11% in women. Age trends for ulcer occurrence reveal declining rates in younger
men, particularly for duodenal ulcer, and increasing rates in older women. Trends reflect
complex changes in risk factors for PUD, including age-cohort phenomena with the
prevalence of H pylori infection and the use of NSAIDs in older populations.
Physiology Laboratory Small Group Discussion Output | Peptic Ulcer Disease 1
International statistics
The frequency of PUD in other countries is variable and is determined primarily
by association with the major causes of PUD: H pylori and NSAIDs
SIGNS & SYMPTOMS
An ulcer may or may not have symptoms. When symptoms occur, they may include:
A gnawing or burning pain in the middle or upper stomach between meals or at
night
Bloating
Heartburn
Nausea or vomiting
In severe cases, symptoms can include:
Dark or black stool (due to bleeding)
Vomiting blood (that can look like "coffee-grounds")
Weight loss
Severe pain in the mid to upper abdomen
CAUSES
Different factors can cause the lining of the stomach, the esophagus, and the small
intestine to break down. These include:
Helicobacter pylori (H. pylori): a bacteria that can cause a stomach infection and
inflammation
frequent use of aspirin, ibuprofen, and other anti-inflammatory drugs (risk associated
with this behavior increases in women and people over the age of 60)
smoking
drinking too much alcohol
radiation therapy
stomach cancer
PATHOPHYSIOLOGY
Peptic ulcers result from an imbalance between factors that can damage the
gastroduodenal mucosal lining and defense mechanisms that normally limit the injury.
Aggressive factors include gastric juice (including hydrochloric acid, pepsin, and bile
salts refluxed from the duodenum), H pylori, and NSAIDs.
Physiology Laboratory Small Group Discussion Output | Peptic Ulcer Disease 2
Mucosal defenses comprise a mucus bicarbonate layer secreted by surface
mucus cells forming a viscous gel over the gastric mucosa; the integrity of tight
junctions between adjacent epithelial cells; and the process of restitution, whereby any
break in the epithelial lining is rapidly filled by adjacent epithelial and mucosal stromal
cells migrating and flattening to fill the gap. Mucosal defenses depend on an adequate
blood supply and on formation within the gastric mucosa.
In general, duodenal ulcers are the result of hypersecretion of gastric acid related
to H pylori infection (the majority of cases), whereas secretion is normal or low in
patients with gastric ulcers.
In duodenal ulcers, chronic H pylori infection confined mainly to the gastric
antrum leads to impaired secretion of somatostatin and consequently increased gastrin
release, resulting in gastric acid hypersecretion. In Zollinger-Ellison syndrome, a
gastrin-secreting neuro-endocrine tumour is the stimulus for high rates of gastric acid
secretion.
In gastric ulcers, longstanding H pylori infection throughout the stomach
accompanied by severe inflammation results in gastric mucin degradation, disruption of
tight junctions between gastric epithelial cells, and the induction of gastric epithelial cell
death. NSAIDs cause injury directly (involving trapping hydrogen ions) and indirectly (a
systemic effect involving the inhibition of cyclo-oxygenases, especially COX-1) and
increase bleeding risk through anti-platelet actions. Chronic gastric ischaemia underlies
the stress ulcers of patients in intensive care.
DIAGNOSIS:
Tests for H. pylori- Your doctor may recommend tests to determine whether the
bacterium H. pylori is present in your body. Tests can test for H. pylori using:
> Blood
> Breath
> Stool
Endoscopy- using a scope to examine your upper digestive system.During
endoscopy, your doctor passes a hollow tube equipped with a lens (endoscope)
down your throat and into your esophagus, stomach and small intestine. Using
the endoscope, your doctor looks for ulcers. If your doctor detects an ulcer, small
tissue samples (biopsy) may be removed for examination in a lab. A biopsy can
also identify the presence of H. pylori in your stomach lining. Your doctor is more
likely to recommend endoscopy if you are older, have signs of bleeding, or have
experienced recent weight loss or difficulty eating and swallowing
Physiology Laboratory Small Group Discussion Output | Peptic Ulcer Disease 3
X-ray of your upper digestive system- sometimes called a barium swallow or
upper gastrointestinal series, this series of X-rays creates images of your
esophagus, stomach and small intestine. During the X-ray, you swallow a white
liquid (containing barium) that coats your digestive tract and makes an ulcer
more visible.
TREATMENT & MANAGEMENT:
Treatment for peptic ulcers depends on the cause. Treatments can include:
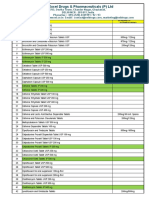
Antibiotic medications to kill H. pylori. If H. pylori is found in your digestive tract, your
doctor may recommend a combination of antibiotics to kill the bacterium.
Proton pump inhibitors reduce stomach acid by blocking the action of the parts of
cells that produce acid. These drugs include the prescription and over-the-counter
medications omeprazole (Prilosec), lansoprazole (Prevacid), rabeprazole (Aciphex),
esomeprazole (Nexium) and pantoprazole (Protonix).
Acid blockers — also called histamine (H-2) blockers — reduce the amount of
stomach acid released into your digestive tract, which relieves ulcer pain and
encourages healing.
Antacids that neutralize stomach acid. Antacids neutralize existing stomach acid and
can provide rapid pain relief. Side effects can include constipation or diarrhea,
depending on the main ingredients.
In some cases, your doctor may prescribe medications called cytoprotective agents
that help protect the tissues that line your stomach and small intestine. Options
include the prescription medications sucralfate (Carafate) and misoprostol (Cytotec).
Another nonprescription cytoprotective agent is bismuth subsalicylate (Pepto-
Bismol).
PROGNOSIS
When the underlying cause is addressed, the prognosis is excellent. Most
patients are treated successfully with eradication of H pylori infection, avoidance of
NSAIDs, and the appropriate use of antisecretory therapy. Eradication of H
pyloriinfection changes the natural history of the disease, with a decrease in the ulcer
recurrence rate from 60-90% to approximately 10-20%. However, this is a higher
recurrence rate than previously reported, suggesting an increased number of ulcers not
caused by H pylori infection.
Physiology Laboratory Small Group Discussion Output | Peptic Ulcer Disease 4
With regard to NSAID-related ulcers, the incidence of perforation is
approximately 0.3% per patient year, and the incidence of obstruction is approximately
0.1% per patient year. Combining both duodenal ulcers and gastric ulcers, the rate of
any complication in all age groups combined is approximately 1-2% per ulcer per year.
The mortality rate for PUD, which has decreased modestly in the last few
decades, is approximately 1 death per 100,000 cases. If one considers all patients with
duodenal ulcers, the mortality rate due to ulcer hemorrhage is approximately 5%. Over
the last 20 years, the mortality rate in the setting of ulcer hemorrhage has not changed
appreciably despite the advent of histamine-2 receptor antagonists (H2RAs) and proton
pump inhibitors (PPIs). However, evidence from meta-analyses and other studies has
shown a decreased mortality rate from bleeding peptic ulcers when intravenous PPIs
are used after successful endoscopic therapy.[19, 20, 21, 22]
Emergency operations for peptic ulcer perforation carry a mortality risk of 6-30%.
Factors associated with higher mortality in this setting include the following:
Shock at the time of admission
Renal insufficiency
Delaying the initiation of surgery for more than 12 hours after presentation
Concurrent medical illness (eg, cardiovascular disease, diabetes mellitus
Age older than 70 years
Cirrhosis
Immunocompromised state
Location of ulcer (mortality associated with perforated gastric ulcer is twice that
associated with perforated
References:
1. Guyton, AC; Hall, JE: Textbook of Medical Physiology, 11th edition. Elsevier Inc.
2006.
2. Koeppen, BM; Stanton, BA: Berne and Levy Physiology, 6 th edition. Elsevier Inc.
2010.
3. en.wikipedia.org
4. http://www.webmd.com/digestive-disorders/digestive-diseases-peptic-ulcer-disease
Physiology Laboratory Small Group Discussion Output | Peptic Ulcer Disease 5
Вам также может понравиться
- Stomach Ulcers (Peptic Ulcers)Документ25 страницStomach Ulcers (Peptic Ulcers)Irtza MajeedОценок пока нет
- "Peptic Ulcer": Presented By, Archana Devi M.Sc. (N) 1 Year EconДокумент27 страниц"Peptic Ulcer": Presented By, Archana Devi M.Sc. (N) 1 Year EconArchana VermaОценок пока нет
- Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer DiseaseДокумент9 страницPeptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer DiseaseRhesky Noer FhadillahОценок пока нет
- Peptic Ulcer Disease: "Something Is Eating at Me"Документ37 страницPeptic Ulcer Disease: "Something Is Eating at Me"bobtaguba100% (1)
- Perforated Gastric UlcerДокумент15 страницPerforated Gastric UlcerNorshahidah IedaОценок пока нет
- Evidence-Based Treatment of Peptic Ulcer DiseaseДокумент9 страницEvidence-Based Treatment of Peptic Ulcer DiseaseRandi AnugerahОценок пока нет
- By Amente J. (B.Pharm, MSC) : For Clinical Pharmacy Students (4 Year)Документ38 страницBy Amente J. (B.Pharm, MSC) : For Clinical Pharmacy Students (4 Year)Mohamed IsmaelОценок пока нет
- Peptic Ulcer Disease - EMEDICINE.2020Документ47 страницPeptic Ulcer Disease - EMEDICINE.2020qayyum consultantfpsc100% (1)
- Abdominal Pain Causes and CharacteristicsДокумент2 страницыAbdominal Pain Causes and CharacteristicsChris RayОценок пока нет
- Comprehensive Resume On Hepatitis AДокумент9 страницComprehensive Resume On Hepatitis AGeoffrey MasyhurОценок пока нет
- Peptic Ulcer Disease GuideДокумент5 страницPeptic Ulcer Disease GuideJake MillerОценок пока нет
- Ulkus PeptikДокумент26 страницUlkus PeptikKang MunirОценок пока нет
- Peptic Ulcer Disease - Need PicturesДокумент5 страницPeptic Ulcer Disease - Need PicturesAriana ValenciaОценок пока нет
- Peptic Ulcer Symptoms and Diagnosis GuideДокумент10 страницPeptic Ulcer Symptoms and Diagnosis Guidemiz uОценок пока нет
- Peptic Ulcer Symptoms, Causes and TreatmentsДокумент14 страницPeptic Ulcer Symptoms, Causes and Treatmentslagas_ralphОценок пока нет
- Complication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaДокумент76 страницComplication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaBrajesh MouryaОценок пока нет
- Peptic UlcerДокумент7 страницPeptic UlcerMarielle Adey Magcawas RNОценок пока нет
- Helicobacter Pylori: Gastric and Duodenal Ulcers: A Gastric Ulcer Would GiveДокумент5 страницHelicobacter Pylori: Gastric and Duodenal Ulcers: A Gastric Ulcer Would Giveleslie_08Оценок пока нет
- Definition, Etiology, Epidemiology PepticДокумент3 страницыDefinition, Etiology, Epidemiology Pepticalfira andiniОценок пока нет
- Peptic Ulcer 2017 SiteДокумент54 страницыPeptic Ulcer 2017 Sitelungu eduardОценок пока нет
- Definition, Etiology, Epidemiology PepticДокумент4 страницыDefinition, Etiology, Epidemiology Pepticalfira andiniОценок пока нет
- Tugas Ppdi + TerjemahanДокумент14 страницTugas Ppdi + TerjemahanAnggii WidyОценок пока нет
- Peptic Ulcer Disease: Causes, Symptoms, and TreatmentДокумент3 страницыPeptic Ulcer Disease: Causes, Symptoms, and TreatmentleahraizaОценок пока нет
- MD Guide to the Stomach and DuodenumДокумент27 страницMD Guide to the Stomach and Duodenumraed faisalОценок пока нет
- Gastrointestinal Diseases - Part 1: Symptoms, Causes and Treatments of Common GI DisordersДокумент27 страницGastrointestinal Diseases - Part 1: Symptoms, Causes and Treatments of Common GI Disordersglenn johnstonОценок пока нет
- BRIEF HISTORY OF PEPTIC ULCER DISEASEДокумент17 страницBRIEF HISTORY OF PEPTIC ULCER DISEASEJon Corpuz AggasidОценок пока нет
- Peptic Ulcer 2Документ38 страницPeptic Ulcer 2tarekОценок пока нет
- Gastro-Oesophageal Reflux Disease: EpidemiologyДокумент6 страницGastro-Oesophageal Reflux Disease: EpidemiologyRehan RiyazОценок пока нет
- Part 1 Introduction AДокумент6 страницPart 1 Introduction Ajay5ar5jamorabon5torОценок пока нет
- Everything You Need to Know About Peptic UlcersДокумент8 страницEverything You Need to Know About Peptic UlcersSyazmin KhairuddinОценок пока нет
- Gastric UlcerДокумент2 страницыGastric Ulcersaby abbyОценок пока нет
- Seminar ON Peptic Ulcer: Presented By: Ms. Sweta SinghДокумент26 страницSeminar ON Peptic Ulcer: Presented By: Ms. Sweta Singhshweta singhОценок пока нет
- Hematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewДокумент6 страницHematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewWahyu Agung PribadiОценок пока нет
- Peptic ulcer symptoms and causesДокумент6 страницPeptic ulcer symptoms and causesIlyes FerenczОценок пока нет
- Brief Summary of Peptic UlcersДокумент3 страницыBrief Summary of Peptic UlcersruguОценок пока нет
- 01 Gastritis & PUDxxДокумент51 страница01 Gastritis & PUDxxTor Koang ThorОценок пока нет
- Peptis Ulcer-Bs TâmДокумент27 страницPeptis Ulcer-Bs TâmÁnh PhạmОценок пока нет
- Peptic Ulcer DiseaseДокумент7 страницPeptic Ulcer DiseaseDiriba FedasaОценок пока нет
- Part 1 Introduction AДокумент6 страницPart 1 Introduction AGeevee Naganag VentulaОценок пока нет
- Nursing Management OF Git Problems Gastric and Duodenal DisordersДокумент109 страницNursing Management OF Git Problems Gastric and Duodenal DisorderstantanbaragoОценок пока нет
- Presentation On Gastric Ulcer-1Документ37 страницPresentation On Gastric Ulcer-1Roshan GhimireОценок пока нет
- Part 1 Introduction AДокумент6 страницPart 1 Introduction AGeevee Naganag VentulaОценок пока нет
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsОт EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsРейтинг: 5 из 5 звезд5/5 (1)
- Duodenum Esophagus Stomach Meckel's Diverticulum: Pylori. Infection Usually Persists For ManyДокумент3 страницыDuodenum Esophagus Stomach Meckel's Diverticulum: Pylori. Infection Usually Persists For ManyKim Andrew SantosОценок пока нет
- Gastritis Diagnosis and Treatment GuideДокумент18 страницGastritis Diagnosis and Treatment GuideBeatrice Sandra ChelaruОценок пока нет
- Peptic Ulcer PresentationДокумент46 страницPeptic Ulcer Presentationmaryam ijazОценок пока нет
- Acute gastritis overviewДокумент13 страницAcute gastritis overviewFalaudin LaksanaОценок пока нет
- A Peptic UlcerДокумент7 страницA Peptic UlcerjenilyndchavezОценок пока нет
- Unit 3 Gastrointestinal Disorders P2 Peptic UlcerДокумент43 страницыUnit 3 Gastrointestinal Disorders P2 Peptic UlcerShashidharan MenonОценок пока нет
- Peptic UlcermazherДокумент49 страницPeptic UlcermazherjawaidakramОценок пока нет
- Peptic UlcerДокумент2 страницыPeptic UlcerluvvemulleОценок пока нет
- 2 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionДокумент11 страниц2 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionKylle AlimosaОценок пока нет
- Peptic Ulcer DiseaseДокумент5 страницPeptic Ulcer DiseasecookieОценок пока нет
- Patho AssignmentДокумент17 страницPatho AssignmentKevser UnalОценок пока нет
- Causes and Diagnosis of Gastric PerforationДокумент4 страницыCauses and Diagnosis of Gastric PerforationChiki CacaОценок пока нет
- Gastrointestinal Health: The Self-Help Nutritional Program That Can Change the Lives of 80 Million AmericansОт EverandGastrointestinal Health: The Self-Help Nutritional Program That Can Change the Lives of 80 Million AmericansОценок пока нет
- CASE PRESENTATION ON PUD: PEPTIC ULCER DISEASEДокумент28 страницCASE PRESENTATION ON PUD: PEPTIC ULCER DISEASEAntoОценок пока нет
- Gastric Ulcer Causes, Symptoms, Diagnosis and TreatmentДокумент16 страницGastric Ulcer Causes, Symptoms, Diagnosis and TreatmentTabada NickyОценок пока нет
- Duodenal Ulcer-1Документ43 страницыDuodenal Ulcer-1Roshan GhimireОценок пока нет
- Abct Journal ReadingsДокумент9 страницAbct Journal ReadingsJane Arian BerzabalОценок пока нет
- PathologyДокумент306 страницPathologyhevenpapiya100% (1)
- Female Physiology Before PregnancyДокумент81 страницаFemale Physiology Before PregnancyChino Paolo SamsonОценок пока нет
- PathologyДокумент306 страницPathologyhevenpapiya100% (1)
- Important Patho Tables, Morphology, and Key Concepts: Chapter 1 - CellДокумент15 страницImportant Patho Tables, Morphology, and Key Concepts: Chapter 1 - CellChino Paolo SamsonОценок пока нет
- 9 Annual Review in Internal Medicine: GastroenterologyДокумент26 страниц9 Annual Review in Internal Medicine: GastroenterologyChino Paolo SamsonОценок пока нет
- Acquired Prothrombin Complex DeficiencyДокумент7 страницAcquired Prothrombin Complex DeficiencyChino Paolo SamsonОценок пока нет
- Airway ManagementДокумент45 страницAirway ManagementChino Paolo SamsonОценок пока нет
- Case Digests 3Документ14 страницCase Digests 3Chino Paolo SamsonОценок пока нет
- Protein-Calories, Malnutrition & Nutritional DeficienciesДокумент14 страницProtein-Calories, Malnutrition & Nutritional DeficienciesChino Paolo SamsonОценок пока нет
- MCQs in Pathology: Key ConceptsДокумент69 страницMCQs in Pathology: Key Conceptsfadiawwad100% (4)
- BIOENERGETICS Trans - IncДокумент3 страницыBIOENERGETICS Trans - IncChino Paolo SamsonОценок пока нет
- Carbs CCДокумент18 страницCarbs CCChino Paolo SamsonОценок пока нет
- Hypo Thyroid Is MДокумент14 страницHypo Thyroid Is MChino Paolo SamsonОценок пока нет
- Protein-Calories, Malnutrition & Nutritional DeficienciesДокумент15 страницProtein-Calories, Malnutrition & Nutritional DeficienciesChino Paolo SamsonОценок пока нет
- Obstructive Pulmonary DiseaseДокумент6 страницObstructive Pulmonary DiseaseChino Paolo SamsonОценок пока нет
- Hemolytic DiseaseДокумент10 страницHemolytic DiseaseChino Paolo SamsonОценок пока нет
- Where Will We Hold OnДокумент1 страницаWhere Will We Hold OnChino Paolo SamsonОценок пока нет
- Obesity 123Документ12 страницObesity 123Chino Paolo SamsonОценок пока нет
- Acute Renal FailureДокумент10 страницAcute Renal FailureChino Paolo SamsonОценок пока нет
- Cushing DiseaseДокумент17 страницCushing DiseaseChino Paolo SamsonОценок пока нет
- Fluid & Electrolyte ImbalanceДокумент11 страницFluid & Electrolyte ImbalanceChino Paolo SamsonОценок пока нет
- Your WordДокумент1 страницаYour WordChino Paolo SamsonОценок пока нет
- Breastfeeding EssentialsДокумент22 страницыBreastfeeding EssentialsChino Paolo SamsonОценок пока нет
- Adrenal Insufficiency & Addison'S Disease: April 13, 2016Документ6 страницAdrenal Insufficiency & Addison'S Disease: April 13, 2016Chino Paolo SamsonОценок пока нет
- Cushing Syndrome Signs, Causes, Diagnosis in 40 CharactersДокумент8 страницCushing Syndrome Signs, Causes, Diagnosis in 40 CharactersChino Paolo SamsonОценок пока нет
- Cardiac ArrhythmiasДокумент11 страницCardiac ArrhythmiasChino Paolo SamsonОценок пока нет
- CHF: Congestive Heart Failure Signs, Causes, PathophysiologyДокумент15 страницCHF: Congestive Heart Failure Signs, Causes, PathophysiologyChino Paolo SamsonОценок пока нет
- Examination in Hematology: NameДокумент1 страницаExamination in Hematology: NameChino Paolo SamsonОценок пока нет
- Long-Term Safety Analysis of Dengue Vaccine CandidateДокумент3 страницыLong-Term Safety Analysis of Dengue Vaccine CandidateChino Paolo SamsonОценок пока нет
- International Journal of Pharmtech Research: Sweety Saini, Chandana Majee, Gunosindhu Chakraborthy, SalahuddinДокумент14 страницInternational Journal of Pharmtech Research: Sweety Saini, Chandana Majee, Gunosindhu Chakraborthy, SalahuddinHarshadbhai S.PrajapatiОценок пока нет
- Medication MathДокумент48 страницMedication MathAlice Choi100% (1)
- 2016 ATC Index With DDDДокумент317 страниц2016 ATC Index With DDDSi CentilОценок пока нет
- Gazette 2022-03-15 Price Revision of 60 Varieties of Medicinal DrugsДокумент10 страницGazette 2022-03-15 Price Revision of 60 Varieties of Medicinal DrugsAda Derana100% (1)
- Formularium PDFДокумент63 страницыFormularium PDFGuntur Marganing100% (1)
- Manage Barrett's Esophagus with Endoscopy, MedicationДокумент21 страницаManage Barrett's Esophagus with Endoscopy, MedicationLyka DimayacyacОценок пока нет
- Ray Pharma Marketing PlanДокумент82 страницыRay Pharma Marketing PlanAndrea Buccarella100% (1)
- NCLEX Cram SheetДокумент2 страницыNCLEX Cram SheetSarah Plunkett100% (1)
- Sample - Drug Index DatabaseДокумент12 страницSample - Drug Index DatabaseEubert John VenturinaОценок пока нет
- Health Teaching For B.P.U.D.Документ10 страницHealth Teaching For B.P.U.D.Jule SantoyaОценок пока нет
- Difference Between GERD and PUDДокумент7 страницDifference Between GERD and PUDOla Adel ShabeebОценок пока нет
- Formulariun UPDATE 25 FEB 2022Документ349 страницFormulariun UPDATE 25 FEB 2022RISKA.SILVIAОценок пока нет
- Vee Excel Drugs & Pharmaceuticals product catalogДокумент10 страницVee Excel Drugs & Pharmaceuticals product catalogSingh PushpanjaliОценок пока нет
- Proton Pump Inhibitors - The Beginning of The End or The End of The Beginning PDFДокумент8 страницProton Pump Inhibitors - The Beginning of The End or The End of The Beginning PDFbravohr98Оценок пока нет
- Helicobacter Pylori:: SymptomsДокумент6 страницHelicobacter Pylori:: SymptomsZaid AbdulqadirОценок пока нет
- Stress-Related Mucosal Disease: Mitchell J. Spirt, MDДокумент11 страницStress-Related Mucosal Disease: Mitchell J. Spirt, MDnur hidayatОценок пока нет
- Registered Medicine List 2014 FMHACAДокумент162 страницыRegistered Medicine List 2014 FMHACASindy ElfasОценок пока нет
- Pharmacy Training - Gastro Intestinal TractДокумент56 страницPharmacy Training - Gastro Intestinal TractDylanSalam100% (1)
- Night Time Gastric Acid Suppression by Tegoprazan Compared To Vonoprazan orДокумент9 страницNight Time Gastric Acid Suppression by Tegoprazan Compared To Vonoprazan orDhruvin KapadiaОценок пока нет
- A Review On Delivery of Drugs Used For Acid Reflux Treatment Using Buccal DrugДокумент18 страницA Review On Delivery of Drugs Used For Acid Reflux Treatment Using Buccal DrugAnjali Sahil MittalОценок пока нет
- Omeprazole: Drugs For Drug Class Brand Name Contains Dosage Form Manufacturer Price (TK .)Документ15 страницOmeprazole: Drugs For Drug Class Brand Name Contains Dosage Form Manufacturer Price (TK .)Sabbir PrinceОценок пока нет
- Esomeprazole Mag. Trihydrate Pellets 22.5%Документ5 страницEsomeprazole Mag. Trihydrate Pellets 22.5%Life Pearl100% (1)
- MNT 1 Nfs 3250 Gerd Case Study PaperДокумент25 страницMNT 1 Nfs 3250 Gerd Case Study Paperapi-302042358100% (2)
- HESI Pharmacology Exam PracticeДокумент11 страницHESI Pharmacology Exam PracticeEkОценок пока нет
- DHM Collection-Instructions Urea-Breath-Test 201902 - UnknownДокумент2 страницыDHM Collection-Instructions Urea-Breath-Test 201902 - Unknownjohn mewОценок пока нет
- 5 Natural Heartburn RemediesДокумент12 страниц5 Natural Heartburn RemediesanafagulhaОценок пока нет
- Debunking The Evergreening Patents MythДокумент3 страницыDebunking The Evergreening Patents Mythjns198Оценок пока нет
- Case PresentationДокумент29 страницCase PresentationLeezhaj VargasОценок пока нет
- Dyspepsia CPG (NICE)Документ322 страницыDyspepsia CPG (NICE)NiñoTanОценок пока нет