Академический Документы
Профессиональный Документы
Культура Документы
Pathophysiology of Lumbar Disc Degeneration: A Review of The Literature
Загружено:
Nafiys Reeven TeergovОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pathophysiology of Lumbar Disc Degeneration: A Review of The Literature
Загружено:
Nafiys Reeven TeergovАвторское право:
Доступные форматы
Neurosurg Focus 13 (2):Article 1, 2002, Click here to return to Table of Contents
Pathophysiology of lumbar disc degeneration: a review of
the literature
MICHAEL D. MARTIN, M.D., CHRISTOPHER M. BOXELL, M.D., F.A.C.S.,
AND DAVID G. MALONE, M.D.
Department of Neurological Surgery, University of Oklahoma, Oklahoma City; and Oklahoma Spine
and Brain Institute, Tulsa, Oklahoma
Lumbar disc degeneration occurs because of a variety of factors and results in a multitude of conditions. Alterations
in the vertebral endplate cause loss of disc nutrition and disc degeneration. Aging, apoptosis, abnormalities in colla-
gen, vascular ingrowth, loads placed on the disc, and abnormal proteoglycan all contribute to disc degeneration. Some
forms of disc degeneration lead to loss of height of the motion segment with concomitant changes in biomechanics of
the segment. Disc herniation with radiculopathy and chronic discogenic pain are the result of this degenerative process.
KEY WORDS • lumbar • disc • degeneration • pathophysiology • review •
anatomy
Lumbar disc degeneration occurs commonly in humans. sion and is a stronger ligament than the PLL. The PLL is
There are a variety of factors that contribute to this condi- not as strong as the ALL, but it provides a tension band to
tion. The disc itself is active tissue that contains signif- resist flexion forces. The PLL strongly attaches to the anu-
icant mechanisms for self-repair.26 Reviewing the available lus fibrosis, and frequently is torn in cases of free frag-
literature concerning the normal and abnormal physiology ment disc herniation.
of the disc is useful in understanding why degeneration A meningeal branch of the spinal nerve, better known
occurs, why certain conditions are painful, and which as the recurrent sinuvertebral nerve, innervates the area
mechanisms can be used to prevent further degeneration. around the disc space (Fig. 2). This nerve exits from the
dorsal root ganglion and enters the foramen, where it then
ANATOMY OF THE INTERVERTEBRAL DISC divides into a major ascending and lesser descending
branch.6 It has been shown in animal studies that further
The intervertebral disc is composed of at least three ele- afferent innervation to the sinuvertebral nerve arises via
ments. The central portion of the disc contains the nucle- the rami communicantes from multiple superior and infe-
us pulposus, which is composed of cells from the primi- rior dorsal root ganglia.43 In both human and animal stud-
tive notochord. The outer portion of the disc is the anulus ies, the outer anular regions are innervated, but the inner
fibrosis, and it is composed of concentric layers of inter- regions and nucleus pulposus are not innervated.37,48 In
twined anular bands. These anular bands are arranged in a addition studies have demonstrated that the ALL also re-
specific pattern to resist forces placed on the lumbar spine. ceives afferent innervation from branches that originate in
The anular bands are subdivided into inner fibers, which the dorsal root ganglion.7 The PLL is richly innervated by
are connected to the cartilaginous endplate, and outer nociceptive fibers from the major ascending branch of the
Sharpy fibers, which are attached to the VB (Fig. 1). The sinuvertebral nerve. These nerves also innervate the adja-
ALL and PLL further strengthen the disc space. The ALL cent outer layers of the anulus fibrosis.7,37 Degenerated hu-
attaches more strongly to the VB edges than to the anulus. man lumbar discs have been shown to contain more nerve
It provides a tension band to resist forces applied in exten- tissue and to be more vascular than normal discs.9,12,48
Abbreviations used in this paper: ALL = anterior longitudinal PROTEOGLYCAN AND WATER CONTENT
ligament; IL = interleukin; MMP = matrix metalloproteinase; NO =
nitric oxide; PG = prostaglandin; PGE = prostaglandin E; PLL = The strength of the lumbar disc is related to the fluid
posterior longitudinal ligament; VB = vertebral body. and proteoglycan content of the disc. Proteoglycan is a
Neurosurg. Focus / Volume 13 / August, 2002 1
M. D. Martin, C. M. Boxell, and D. G. Malone
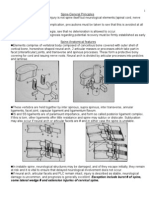
Fig. 1. Artist's illustration showing the vascular supply to the
disc space from the cartilaginous endplate. 1 = segmental radicu-
lar artery; 2 = interosseous artery; 3 = capillary tuft; and 4 = disc
anulus.
Fig. 2. Artist's illustration showing innervation of the PLL and
the disc anulus; 1 = ascending branch of the sinuvertebral nerve;
2 = dorsal root ganglion; 3 = descending branch of the sinuverte-
hydrophilic, negatively charged, branched chain molecule bral nerve; 4 = disc anulus; 5 = PLL.
composed of a protein attached to an oligosaccharide. Pro-
teoglycans are also known as glycosaminoglycans and
include such structures as chondroitin and collagen. The
negative charge on the branched chains and the hydro- change with increasing age that is characterized by a pro-
philic nature of proteoglycan internally pressurize the disc portional increase in its glycoprotein form, which lacks
by drawing water via osmosis into the nucleus pulposus. keratin sulfate.61
Unfortunately, proteoglycan and therefore water content
in the disc tend to decrease with age.1-3,51,65 Additionally VASCULARITY OF THE DISC
the amount of hydration within the disc is inversely pro-
portional to applied stress, suggesting that applied spinal The disc itself has a low metabolic rate and receives
loads lead to a loss of hydration and proteoglycan in the most of its nutrition by diffusion.26 Bulk transport con-
disc.65 Interestingly, proteoglycan, and thus water content, tributes somewhat to nutrition of the disc and this is facil-
has also been shown to be low throughout the entire spine itated by spinal motion.25 The majority of disc nutrition
in patients with degenerated discs.51 Studies have shown is supplied via the capillary beds of the cartilaginous VB
that applied stress produces degenerative change in the endplate.10 Blood flow to these capillary beds is under hu-
disc; however, it remains unclear whether degeneration in moral control, which increases with application of acetyl-
vivo is the result of stress applied to an already biochem- choline.68 Early research suggests muscarinic receptors
ically altered disc or a response to stress by an otherwise exist on the cartilaginous endplate, implying a possible
normal disc. Disc degeneration may have a genetic basis; mechanism of the negative effects of nicotine on the end-
Sahlman, et al.,59 have shown that mice that are heterozy- plate.68 These capillary beds receive blood flow from the
gotes for the knockout gene, Col2a1, related to Type II distal branches of the interosseous arteries supplying the
collagen, had 4% shorter spines and a decreased concen- VB. Disruption of the cartilaginous endplate leads to for-
tration of glycosaminoglycans in their endplates, verte- mation of Schmoral nodes.54 Vascular and lymphatic tis-
brae, and anuli fibrosis. sue is present in the anulus of patients who are as old as
Degenerated discs have been demonstrated to vary spe- age 20 years; however, lymphatics and blood vessels are
cifically in the degree of sulfation of chondroitin.27 De- not present in the nucleus pulposus at any age.56 The con-
generated discs lacked adequate sulfation of chondroitin centration of oxygen has been found to be greatest at the
when compared with controls, and the degree of degen- disc edge, and the concentration of lactate is greatest in the
eration was greater in higher grade degeneration. The center, which is the portion of the disc farthest from the
specific disaccharide involved was chondroitin sulfate,6 blood supply.4 Although the concentrations of oxygen and
which had been reduced to unsulfated chondroitin in de- lactate vary widely from person to person, they do not
generated sections. This study suggested a possible mech- seem to change in pathological states.4
anism for the increased incidence of posterior failure of Changes in the vascular supply appear in disc degener-
the disc, because the degree of undersulfation was accen- ation. Normal anastomotic arteries on the anterolateral
tuated in the nucleus pulposus as well as the posterior surface are obliterated and replaced by small, tortuous
central segment of the anulus fibrosis. Another specific arteries in degenerated anuli.33 The arterial changes occur
anular proteoglycan, fibromodulin, exhibits a structural before the degenerative process and may be related to the
2 Neurosurg. Focus / Volume 13 / August, 2002
Pathophysiology of lumbar disc degeneration
ingrowth of vessels from osteophyte formation.33 This im- parent that an inappropriate disc matrix is produced in
plies a relationship between nutrition to the disc and sub- degenerated lumbar discs.20 This inappropriate matrix
sequent disease. Some authors believe that neovascularity may isolate cells in the disc and lead to apoptosis. Further
occurs in response to injury as an attempt to supply the experimentation has indicated that apoptosis occurs at a
damaged portion of the disc with nutrients.66 Others sug- higher rate in cases of free disc fragments compared with
gest that vascularization of the anulus occurs in response contained disc herniations.50 This increased rate of apop-
to trauma and that the new vessels are associated with en- tosis in free disc herniations may be a possible mechanism
dothelial cells, fibroblasts, and mononuclear cells.53 Sur- of resorption and remodeling of the extruded material.
gical specimens have been compared with those from In vitro evidence suggests that certain cytokines, namely
normal cadaveric disc and it has been found that the vas- insulin-like growth factor-1 and platelet-derived growth
culature of normal discs was not associated with addition- factor, can inhibit apoptosis in cell cultures of disc materi-
al cells, but instead with an inactive collagen matrix.53 al.21 In vivo experiments indicate that disc tissue responds
Both macrophages and blood vessels have been found to in an autocrine fashion; that is, the cells release substances
be prominent in herniated disc fragments, but the presence to which the cells themselves respond.31,36,49 This has been
or absence of these entities could not be correlated with shown to be different in degenerated compared with nor-
the timing of radicular pain.67 mal disc tissue, and it has been hypothesized that these
substances can lead to disc degeneration.36,49 These stud-
ies all indicate that the disc is much more active biologi-
COLLAGEN DISTRIBUTION cally than previously thought, and further research may
Collagen is a widely distributed proteoglycan in the provide pharmacological means to change the natural his-
body. Type I collagen is usually found in skin, bone, ten- tory of disc degeneration.
don, and dentin. Types II and IX are normally found in hy-
aline cartilage and vitreous humor. Type III collagen can
be found in skin and blood vessels. Type VI is found in MECHANICAL STRESS AND INFLAMMATORY
most interstitial tissues. Type I collagen is found in the COMPONENTS
nucleus pulposus and anulus fibrosis in both normal and
pathologically degenerated discs, whereas Type II and IX Authors of multiple studies have evaluated mechanical
collagen are found to be increased in areas of minor stress as applied to the intervertebral disc. Disc degenera-
degeneration but absent in areas of more advanced dis- tion is related to mechanical stresses. Degeneration may
ease.44 In contrast, Lotz, et al.,40 found that Type II colla- begin in early adulthood and may change the disc in such
gen is decreased at all levels of applied mechanical stress. a way that herniation is imminent.23 The levels most com-
In another study the total amount of collagen was found to monly affected are L4-5 and L5-S1. Although degenera-
be highest in patients 5 to 15 years of age, and in this study tion at one of these two levels is correlated with disease
the amount of denatured Type II was decreased in degen- at the other, there is no correlation with disease in facet
erated discs.2,3 Types III and VI were increased in areas of joints.17 Disease in either the facet joints or the disc is not
degeneration regardless of the degree.44 A marker of oxi- reliably correlated with patient age. Stress in the vertebral
dative stress related to modification of the protein struc- column is transmitted mostly to the endplates of the VB
ture of collagen, N-(carboxymethyl)lysine, has been and less to the core of the body.39 In healthy individuals
shown to increase with advancing degenerative disease.45 the stress is transmitted from the center of the endplate,
Additional studies of the collagen composition of the whereas in a degenerative state, stress is transmitted more
disc have revealed the importance of collagen crosslinks to the peripheral rather than the central aspects of the VB.
to the mechanical stability of the intervertebral disc. A This is thought to be due to the loss of hydration of the
decrease in the presence of pyridinoline and an increase in nucleus pulposus that accompanies aging.39
pentosidine within the disc are associated with aging.52 Other biomechanical studies have focused on the effect
The concentration of pyridinoline found in patients older of applied stress. A study in which cadaveric disc was
than 65 years was approximately 50% of that found in used and with motion was applied in flexion-extension,
younger people. Decreases in pyridinoline crosslinks lead axial rotation, and lateral bending showed that the laxity
to alterations in the collagen matrix of the disc. Cells in of a degenerated disc is increased and the range of motion
the disc have the potential to produce a matrix that is inap- is decreased.41 Spine flexibility and, thus range of motion,
propriate for the mechanical stresses placed on it.20 was shown to be reduced in degeneration because of the
It has also been suggested that matrix degeneration increasing size of the endplate and the decreasing height
within the nucleus may result from the increase in certain of the intervertebral disc space. The increased laxity of the
proteinases that do not appear in the normal disc. Leuko- motion segment was found to be due to decreased disc
cyte elastase, which is normally found in the VB, may be height of the nucleus with resultant loss of tension of the
at least partially responsible for the degeneration of the surrounding ligaments.41 When intradiscal pressure is
extracellular matrix in the anulus, nucleus, and endplate.13 increased, degenerated discs herniate at lower pressures
than normal discs.28 It may be possible that a certain criti-
cal pressure exists above which the stressed anulus is
unable to counteract the force applied, resulting in rup-
ROLE OF APOPTOSIS ture.28 Umehara, et al.,64 reported that the anulus in degen-
Apoptosis is programmed cell death and occurs in both erated discs is abnormal and that its elastic modulus is
normal and pathological states. The role of apoptosis in lowest in the posterolateral section of the disc. The same
lumbar disc degeneration is not fully understood. It is ap- group demonstrated that symmetry and regularity of the
Neurosurg. Focus / Volume 13 / August, 2002 3
M. D. Martin, C. M. Boxell, and D. G. Malone
elastic modulus decrease as the grade of degeneration in- although the number of macrophages is known to be in-
creases. Others have shown that the degenerated disc had creased.22,34
reduced ability to withstand applied stress and that the
section of anulus most responsible for this is the middle
portion.14 DISC HERNIATION
Applied stress may trigger certain biochemical events It has been widely held that symptoms of lumbar disc
within the disc. Degenerated discs have higher than nor- disease are the result of either herniation of the nucleus
mal concentrations of fibronectin, which may be elevated pulposus through a mechanically weak anulus fibrosis or
as part of the response to injury.47 This may translate to an from tearing of the anulus itself. This can lead to radicu-
increase in proteolytic activity.47 Mechanical stress has lopathy from nerve root compression or an inflammatory
also been shown to increase the activity of MMPs 2 and 9 process affecting nerve roots or the spinal cord. Herniation
in articular cartilage, indicating an increase in tissue turn- is thought to be the result of a defect in the anulus fibro-
over that has the potential to weaken the disc.5 Increases sis, most likely the result of excessive stress applied to the
in MMPs, NO, PGE-2, and IL-6 are also seen in herniat- disc.15 Histological evaluation has revealed that whatever
ed discs.32 Cathespin G, a proteinase with a wide variety the cause of the tear, the extruded portion always involves
of biochemical actions, has been shown to be increased in material from the nucleus pulposus.42 Herniation most
the anulus of degenerated discs.38 It has also been sug- often occurs on the posterior or posterolateral aspect of the
gested that applied stress may decrease the expression of disc.28 Morphological characteristics, namely the arrange-
Type II collagen and result in disorganization of the anu- ment of the anular fiber bundles, seem to contribute to the
lus fibrosus.40 propensity for disc herniation on the posterior aspect of
The herniated disc also induces an inflammatory re- the disc. This directs the herniation toward the exiting and
sponse. In a dog model with autologous implantation of traversing nerve roots.63
both nucleus and anulus, Hasegawa and colleagues24 The degree of disease in the lumbar spine is character-
showed that nucleus fragments induce an inflammatory ized by the location of the abnormal portion of the disc.30
reaction. The number of lymphocytes, macrophages, and A disc bulge is a symmetrical extension of the disc beyond
fibroblasts was markedly increased in samples from older the endplates, whereas a protrusion is a focal area of ex-
dogs.24 Others have examined human samples, finding tension still attached to the disc.16,30 An extruded fragment
that macrophages are the most commonly found cell type is one that is no longer connected to the disc, and a
in both acute and chronic herniation.19,22,29 Despite this sequestered fragment is contained within the PLL.16,30
finding, evidence of macrophage infiltration does not cor-
relate with clinical symptoms in humans.55 Interestingly,
the presence of inflammation in patients does correlate CONCLUSIONS
with a better postoperative outcome when compared with The lumbar discs most often affected by degeneration
those with herniated discs showing no inflammation.69 A that leads to herniation are L4-5 and L5-S1, most proba-
study in rats revealed an increase in the expression of IL- bly because of a combination of longstanding degenera-
1, IL-6, and NO synthetase 1 week after implantation of tion and a subsequent change in the ability of the disc to
nucleus fragments.35 Further progression of the inflamma- resist applied stress. Discs that are degenerated show ab-
tory response may be caused by IL-1; the addition of this normal vascularity, and abnormal distribution of collagen
cytokine to normal disc tissue in vitro causes an increase and collagen crosslinks. They also show an abnormal and
in MMPs, IL-6, PGE-2, and NO.32 Degradation of the pro- nonuniform elastic modulus that distributes stress to criti-
teins in the extracellular matrix of the disc may also be cal portions of the disc. Radicular pain is often associated
caused by MMP's. Other inflammatory mediators, such as with disc herniation, which may be due, in part, to an in-
IL-1␣ and tumor necrosis factor-, are also present in the flammatory response to the portion of nucleus that has
herniated disc and may in crease the amount of PGE-2.62 been extruded. This inflammation is characterized by an
The painful disc may be the result of the effect of PGE-2, increase in the number of macrophages and an increase in
and, in fact, a positive straight-leg raise result has been IL-1, with a subsequent release of PGE-2. Although the
correlated with the amount of PGE-2.46 Some controversy relative importance of these diverse pathological changes
exists as to whether levels of tumor necrosis factor-␣ is unclear, it is clear that lumbar disc degeneration and
and phospholipase A2 are increased in the herniated herniation are multifactoral processes and that both mech-
disc.11,18,57,58 anical and biochemical derangements exist.
In addition to the inflammatory mediators already men-
tioned, authors of one study found that two thirds of pa-
tients with lumbar disc disease and radicular symptoms References
had an increase in antiglycosphingolipid antibodies, sug-
gesting an autoimmune component to lumbar disc dis- 1. Adams MA, McNally DS, Dolan P: 'Stress' distributions inside
ease.8 Another group of authors showed that there are an- intervertebral discs. The effects of age and degeneration. J
tigen-antibody complexes present in the herniated disc, Bone Joint Surg Br 78:965–972, 1996
2. Antoniou J, Goudsouzian NM, Heathfield TF, et al: The human
although no conclusions were made regarding their clini- lumbar endplate. Evidence of changes in biosynthesis and de-
cal significance.60 The theory that there is an autoimmune naturation of the extracellular matrix with growth, maturation,
component to lumbar disc disease is controversial; oth- aging, and degeneration. Spine 21:1153–1161, 1996
ers authors have demonstrated a lack of cells that were 3. Antoniou J, Steffen T, Nelson F, et al: The human lumbar inter-
expected in an antigen-specific inflammatory response, vertebral disc: evidence for changes in the biosynthesis and de-
4 Neurosurg. Focus / Volume 13 / August, 2002
Pathophysiology of lumbar disc degeneration
naturation of the extracellular matrix with growth, maturation, 27. Hutton WC, Elmer WA, Boden SD, et al: Analysis of chondroi-
ageing, and degeneration. J Clin Invest 98:996–1003, 1996 tin sulfate in lumbar intervertebral discs at two different stages
4. Bartels EM, Fairbank JC, Winlove CP, et al: Oxygen and lac- of degeneration as assessed by discogram. J Spinal Disord 10:
tate concentrations measured in vivo in the intervertebral discs 47–54, 1997
of patients with scoliosis and back pain. Spine 23:1–8, 1998 28. Iencean SM: Lumbar intervertebral disc herniation following
5. Blain EJ, Gilbert SJ, Wardale RJ, et al: Up-regulation of matrix experimental intradiscal pressure increase. Acta Neurochir
metalloproteinase expression and activation following cyclical 142:669–676, 2000
compressive loading of articular cartilage in vitro. Arch Bio- 29. Ikeda T, Nakamura T, Kikuchi T, et al: Pathomechanism of
chem Biophys 396:49–55, 2001 spontaneous regression of the herniated lumbar disc: histologic
6. Bogduk N: The anatomy of the lumbar intervertebral disc syn- and immunohistochemical study. J Spinal Disord 9:136–140,
drome. Med J Aust 1:878–881, 1976 1996
7. Bogduk N, Tynan W, Wilson AS: The nerve supply to the hu- 30. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al: Mag-
man lumbar intervertebral discs. J Anat 132:39–56, 1981 netic resonance imaging of the lumbar spine in people without
8. Brisby H, Balague F, Schafer D, et al: Glycosphingolipid anti- back pain. N Engl J Med 331:69–73, 1994
bodies in serum in patients with sciatica. Spine 27:380–386, 31. Kang JD, Georgescu HI, McIntyre-Larkin L, et al: Herniated
2002 lumbar intervertebral discs spontaneously produce matrix met-
9. Coppes MH, Marani E, Thomeer RT, et al: Innervation of alloproteinases, nitric oxide, interleukin-6, and prostaglandin
"painful" lumbar discs. Spine 22:2342–2350, 1997 E2. Spine 21:271–277, 1996
10. Crock HV, Goldwasser M: Anatomic studies of the circulation 32. Kang JD, Stefanovic-Racic M, McIntyre LA, et al: Toward a
in the region of the vertebral end-plate in adult Greyhound biochemical understanding of human intervertebral disc degen-
dogs. Spine 9:702–706, 1984 eration and herniation. Contributions of nitric oxide, interleu-
11. Doita M, Kanatani T, Harada T, et al: Immunohistologic study kins, prostaglandin E2, and matrix metalloproteinases. Spine
of the ruptured intervertebral disc of the lumbar spine. Spine 22:1065–1073, 1997
21:235–241, 1996 33. Kauppila LI: Ingrowth of blood vessels in disc degeneration.
12. Freemont AJ, Peacock TE, Goupille P, et al: Nerve ingrowth Angiographic and histological studies of cadaveric spines. J
into diseased intervertebral disc in chronic back pain. Lancet Bone Joint Surg Am 77:26–31, 1995
350:178–181, 1997 34. Kawaguchi S, Yamashita T, Yokogushi K, et al: Immunophe-
13. Fujita K, Nakagawa T, Hirabayashi K, et al: Neutral proteinases notypic analysis of the inflammatory infiltrates in herniated in-
in human intervertebral disc. Role in degeneration and probable tervertebral discs. Spine 26:1209–1214, 2001
origin. Spine 18:1766–1773, 1993 35. Kawakami M, Matsumoto T, Kuribayashi K, et al: mRNA
14. Fujita Y, Duncan NA, Lotz JC: Radial tensile properties of the expression of interleukins, phospholipase A2, and nitric oxide
lumbar annulus fibrosus are site and degeneration dependent. J synthase in the nerve root and dorsal root ganglion induced by
Orthop Res 15:814–819, 1997 autologous nucleus pulposus in the rat. J Orthop Res 17:
15. Gordon SJ, Yang KH, Mayer PJ, et al: Mechanism of disc rup- 941–946, 1999
ture. A preliminary report. Spine 16:450–456, 1991 36. Kohyama K, Saura R, Doita M, et al: Intervertebral disc cell
16. Greenberg MS: Handbook of Neurosurgery, ed 5. New York: apoptosis by nitric oxide: biological understanding of interver-
Thieme, 2001, p 289 tebral disc degeneration. Kobe J Med Sci 46:283–295, 2000
17. Gries NC, Berlemann U, Moore RJ, et al: Early histologic 37. Kojima Y, Maeda T, Arai R, et al: Nerve supply to the posterior
changes in lower lumbar discs and facet joints and their corre- longitudinal ligament and the intervertebral disc of the rat ver-
lation. Eur Spine J 9:23–29, 2000 tebral column as studied by acetylcholinesterase histochem-
18. Gronblad M, Virri J, Ronkko S, et al: A controlled biochemi- istry. I. Distribution in the lumbar region. J Anat 169:237–246,
cal and immunohistochemical study of human synovial-type 1990
(Group II) phospholipase A2 and inflammatory cells in macro- 38. Konttinen YT, Kaapa E, Hukkanen M, et al: Cathepsin G in de-
scopically normal, degenerated, and herniated human lumbar generating and healthy discal tissue. Clin Exp Rheumatol 17:
disc tissues. Spine 21:2531–2538, 1996 197–204, 1999
19. Gronblad M, Virri J, Tolonen J, et al: A controlled immunohis- 39. Kurowski P, Kubo A: The relationship of degeneration of the
tochemical study of inflammatory cells in disc herniation tissue. intervertebral disc to mechanical loading conditions on lumbar
Spine 19:2744–2751, 1994 vertebrae. Spine 11:726–731, 1986
20. Gruber HE, Hanley EN Jr: Analysis of aging and degeneration 40. Lotz JC, Colliou OK, Chin JR, et al: Compression-induced de-
of the human intervertebral disc. Comparison of surgical spec- generation of the intervertebral disc: an in vivo mouse model
imens with normal controls. Spine 23:751–757, 1998 and finite-element study. Spine 23:2493–2506, 1998
21. Gruber HE, Norton HJ, Hanley EN Jr: Anti-apoptotic effects of 41. Mimura M, Panjabi MM, Oxland TR, et al: Disc degenera-
IGF-1 and PDGF on human intervertebral disc cells in vitro. tion affects the multidirectional flexibility of the lumbar spine.
Spine 25:2153–2157, 2000 Spine 19:1371–1380, 1994
22. Habtemariam A, Gronblad M, Virri J, et al: A comparative im- 42. Moore RJ, Vernon-Roberts B, Fraser RD, et al: The origin and
munohistochemical study of inflammatory cells in acute-stage fate of herniated lumbar intervertebral disc tissue. Spine 21:
and chronic-stage disc herniations. Spine 23:2159–2166, 1998 2149–2155, 1996
23. Hadjipavlou AG, Simmons JW, Pope MH, et al: 43. Morinaga T, Takahashi K, Yamagata M, et al: Sensory inner-
Pathomechanics and clinical relevance of disc degeneration and vation to the anterior portion of lumbar intervertebral disc.
annular tear: a point-of-view review. Am J Orthop Spine 21:1848–1851, 1996
28:561–571, 1999 44. Nerlich AG, Boos N, Wiest I, et al: Immunolocalization of
24. Hasegawa T, An HS, Inufusa A, et al: The effect of age on major interstitial collagen types in human lumbar intervertebral
inflammatory responses and nerve root injuries after lumbar discs of various ages. Virchows Arch 432:67–76, 1998
disc herniation: an experimental study in a canine model. Spine 45. Nerlich AG, Schleicher ED, Boos N: 1997 Volvo Award win-
25:937–940, 2000 ner in basic science studies. Immunohistologic markers for age-
25. Holm S, Nachemson A: Variations in the nutrition of the canine related changes of human lumbar intervertebral discs. Spine
intervertebral disc induced by motion. Spine 8:866–874, 1983 22:2781–2795, 1997
26. Humzah MD, Soames RW: Human intervertebral disc: struc- 46. O'Donnell JL, O'Donnell AL: Prostaglandin E2 content in her-
ture and function. Anat Rec 220:337–356, 1988 niated lumbar disc disease. Spine 21:1653–1656, 1996
Neurosurg. Focus / Volume 13 / August, 2002 5
M. D. Martin, C. M. Boxell, and D. G. Malone
47. Oegema TR Jr, Johnson SL, Aguiar DJ, et al: Fibronectin and 60. Satoh K, Konno S, Nishiyama K, et al: Presence and distribu-
its fragments increase with degeneration in the human interver- tion of antigen-antibody complexes in the herniated nucleus
tebral disc. Spine 25:2742–2747, 2000 pulposus. Spine 24:1980–1984, 1999
48. Palmgren T, Gronblad M, Virri J, et al: An immunohistochem- 61. Sztrolovics R, Alini M, Mort JS, et al: Age-related changes in
ical study of nerve structures in the anulus fibrosus of human fibromodulin and lumican in human intervertebral discs. Spine
normal lumbar intervertebral discs. Spine 24:2075–2079, 1999 24:1765–1771, 1999
49. Park JB, Chang H, Kim KW: Expression of Fas ligand and 62. Takahashi H, Suguro T, Okazima Y, et al: Inflammatory cyto-
apoptosis of disc cells in herniated lumbar disc tissue. Spine 26: kines in the herniated disc of the lumbar spine. Spine 21:
618–621, 2001 218–224, 1996
50. Park JB, Kim KW, Han CW, et al: Expression of Fas receptor 63. Tsuji H, Hirano N, Ohshima H, et al: Structural variation of the
on disc cells in herniated lumbar disc tissue. Spine 26:142–146, anterior and posterior anulus fibrosus in the development of
2001 human lumbar intervertebral disc. A risk factor for interverte-
51. Pearce RH, Grimmer BJ, Adams ME: Degeneration and the bral disc rupture. Spine 18:204–210, 1993
chemical composition of the human lumbar intervertebral disc. 64. Umehara S, Tadano S, Abumi K, et al: Effects of degeneration
J Orthop Res 5:198–205, 1987 on the elastic modulus distribution in the lumbar intervertebral
52. Pokharna HK, Phillips FM: Collagen crosslinks in human lum- disc. Spine 21:811–820, 1996
bar intervertebral disc aging. Spine 23:1645–1648, 1998 65. Urban JP, McMullin JF: Swelling pressure of the lumbar inter-
53. Repanti M, Korovessis PG, Stamatakis MV, et al: Evolution of vertebral discs: influence of age, spinal level, composition, and
disc degeneration in lumbar spine: a comparative histological degeneration. Spine 13:179–187, 1988
study between herniated and postmortem retrieved disc speci- 66. Virri J, Gronblad M, Savikko J, et al: Prevalence, mor-
mens. J Spinal Disord 11:41–45, 1998 phology, and topography of blood vessels in herniated disc
54. Roberts S, Menage J, Urban JP: Biochemical and structural tissue. A comparative immunocytochemical study. Spine 21:
properties of the cartilage end-plate and its relation to the inter- 1856–1863, 1996
vertebral disc. Spine 14:166–174, 1989 67. Virri J, Sikk S, Gronblad M, et al: Concomitant immunocyto-
55. Rothoerl RD, Woertgen C, Holzschuh M, et al: Is there a clini- chemical study of macrophage cells and blood vessels in disc
cal correlate to the histologic evidence of inflammation in her- herniation tissue. Eur Spine J 3:336–341, 1994
niated lumbar disc tissue? Spine 23:1197–1201, 1998 68. Wallace AL, Wyatt BC, McCarthy ID, et al: Humoral reg-
56. Rudert M, Tillmann B: Lymph and blood supply of the human ulation of blood flow in the vertebral endplate. Spine 19:
intervertebral disc. Cadaver study of correlations to discitis. 1324–1328, 1994
Acta Orthop Scand 64:37–40, 1993 69. Woertgen C, Rothoerl RD, Brawanski A: Influence of macro-
57. Saal JS: The role of inflammation in lumbar pain. Spine 20: phage infiltration of herniated lumbar disc tissue on outcome
1821–1827, 1995 after lumbar disc surgery. Spine 25:871–875, 2000
58. Saal JS, Franson RC, Dobrow R, et al: High levels of inflam-
matory phospholipase A2 activity in lumbar disc herniations.
Spine 15:674–678, 1990 Manuscript received June 24, 2002.
59. Sahlman J, Inkinen R, Hirvonen T, et al: Premature vertebral Accepted in final form July 3, 2002.
endplate ossification and mild disc degeneration in mice after Address reprint requests to: David G. Malone, M.D., Oklahoma
inactivation of one allele belonging to the Col2a1 gene for Type Spine and Brain Institute, 1919 South Wheeling, Tulsa, Oklahoma
II collagen. Spine 26:2558–2565, 2001 74104. email: xmalone@cox.net.
6 Neurosurg. Focus / Volume 13 / August, 2002
Вам также может понравиться
- Posterior Cruciate Ligament Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPosterior Cruciate Ligament Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Trochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandTrochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Spinal StenosisДокумент14 страницSpinal Stenosisshwampa100% (3)
- Degenerative Spine DiseaseДокумент17 страницDegenerative Spine DiseasekidrocksbodydblОценок пока нет
- Prolapsed Disc SignsДокумент14 страницProlapsed Disc SignsMartin Sage100% (1)
- Orthopaedic Surgeon's Guide to Spine Problems and TreatmentsДокумент65 страницOrthopaedic Surgeon's Guide to Spine Problems and TreatmentsDenuna EnjanaОценок пока нет
- San Antonio Scoliosis Houston Scoliosis Treatment Spine and Scoliosis Center Central TexasДокумент7 страницSan Antonio Scoliosis Houston Scoliosis Treatment Spine and Scoliosis Center Central TexasequijanocОценок пока нет
- Red Flag: MSK Services Pathway - Shoulder PathologyДокумент11 страницRed Flag: MSK Services Pathway - Shoulder PathologyMuhammed ElgasimОценок пока нет
- Common Shoulder Pathologies and Causes of Shoulder PainДокумент33 страницыCommon Shoulder Pathologies and Causes of Shoulder PainjermaineОценок пока нет
- Ijspt-Biomechanics and Pathomechanics of The Patellofemoral JointДокумент11 страницIjspt-Biomechanics and Pathomechanics of The Patellofemoral JointDevi MigiekaОценок пока нет
- Low Back PainДокумент8 страницLow Back PainLev KalikaОценок пока нет
- Postural Assessment (Mia)Документ9 страницPostural Assessment (Mia)im. EliasОценок пока нет
- Scapular Dyskinesis PDFДокумент24 страницыScapular Dyskinesis PDFPablo Sentis DiazОценок пока нет
- Scoliosis: Degenerative & IdiopathicДокумент34 страницыScoliosis: Degenerative & IdiopathicClaudia MariscaОценок пока нет
- Rotator Cuff Tears Orthoinfo - Aaos.org TopicДокумент7 страницRotator Cuff Tears Orthoinfo - Aaos.org TopicMontserrat LandaОценок пока нет
- Achilles RuptureДокумент23 страницыAchilles RupturePhysiotherapist AliОценок пока нет
- Chaptar 30 Degenerative Spine DiseaseДокумент9 страницChaptar 30 Degenerative Spine DiseaseAbraham SaldañaОценок пока нет
- Assessment of Posture: Prepared By: Floriza P. de Leon, PTRPДокумент17 страницAssessment of Posture: Prepared By: Floriza P. de Leon, PTRPFloriza de Leon100% (1)
- Lower Back Pain Causes and TreatmentsДокумент19 страницLower Back Pain Causes and TreatmentsGavin TessierОценок пока нет
- Static Palpation of The Spine FINALДокумент13 страницStatic Palpation of The Spine FINALPrathap KumarОценок пока нет
- KyphosisДокумент32 страницыKyphosisBeniamin CostinașОценок пока нет
- Anatomy of ScoliosisДокумент6 страницAnatomy of ScoliosisDaniel MañalacОценок пока нет
- De Novo Scoliosis: Ashish Patel Frank Schwab Jean-Pierre FarcyДокумент9 страницDe Novo Scoliosis: Ashish Patel Frank Schwab Jean-Pierre Farcymetasoniko81Оценок пока нет
- Featured Applied Radiology Article - Diagnostic Imaging of Spinal Fusion and ComplicationsДокумент11 страницFeatured Applied Radiology Article - Diagnostic Imaging of Spinal Fusion and ComplicationsradRounds Radiology NetworkОценок пока нет
- Shoulder Impingement SyndromeДокумент21 страницаShoulder Impingement SyndromeivannaOctavianiОценок пока нет
- Department of Orthopaedic and Traumatology Faculty of Medicine - Hasanuddin University Makassar 2017Документ24 страницыDepartment of Orthopaedic and Traumatology Faculty of Medicine - Hasanuddin University Makassar 2017aritrisnawatiОценок пока нет
- Degenerative Spinal DisordersДокумент47 страницDegenerative Spinal Disordersasad1912Оценок пока нет
- Coxa ValgaДокумент7 страницCoxa Valgachitz.14Оценок пока нет
- Suplemen AmputeeДокумент59 страницSuplemen Amputeewahyu_sitaОценок пока нет
- Cauda Equina and Conus Medullaris Syndromes Clinical PresentationДокумент9 страницCauda Equina and Conus Medullaris Syndromes Clinical PresentationhoneyworksОценок пока нет
- Clinical Signs - NamedДокумент9 страницClinical Signs - NamedsprapurОценок пока нет
- F16 Physiotherapy After Stroke - 0Документ15 страницF16 Physiotherapy After Stroke - 0Mohammad Reyaz AhmadОценок пока нет
- Lower Extremity DisordersДокумент25 страницLower Extremity DisordersJameson87Оценок пока нет
- Aetiology of Idiopathic Scoliosis. Current Concepts, BurwellДокумент34 страницыAetiology of Idiopathic Scoliosis. Current Concepts, BurwellJeanne MalizardОценок пока нет
- Cervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandCervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Exception Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical SpineДокумент29 страницException Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical Spinebhavesh jain100% (2)
- B 756 Vertebris GB III10Документ44 страницыB 756 Vertebris GB III10Lukasz Bartochowski100% (1)
- Understanding ACL Injuries and SurgeryДокумент38 страницUnderstanding ACL Injuries and SurgerySzilvia MartonosОценок пока нет
- Effectiveness of Mulligan's Mobilization Technique Versus Eccentric Exercises On Pain, Hand Grip Strength and Function in Subjects With Lateral EpicondylitisДокумент8 страницEffectiveness of Mulligan's Mobilization Technique Versus Eccentric Exercises On Pain, Hand Grip Strength and Function in Subjects With Lateral EpicondylitisInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Therapybook Interferencial TherapyДокумент34 страницыTherapybook Interferencial TherapyBrian RaymondОценок пока нет
- Rehabilitation Protocol For ACLДокумент9 страницRehabilitation Protocol For ACLgb tradeОценок пока нет
- Achilles Tendon RuptureДокумент6 страницAchilles Tendon RuptureBn Wahyu AjiОценок пока нет
- Entrapment Neuropathies Conversion-GateДокумент76 страницEntrapment Neuropathies Conversion-GateRam ReddyОценок пока нет
- Intervertebral Disc Degeneration Prevalence, Risk Factors and Treatments MasudДокумент297 страницIntervertebral Disc Degeneration Prevalence, Risk Factors and Treatments MasudAlban KrasniqiОценок пока нет
- Jurnal Shoulder Dislocation - PendekДокумент84 страницыJurnal Shoulder Dislocation - PendekCliff LewisОценок пока нет
- Alingment in TKRДокумент3 страницыAlingment in TKRdeepak100% (1)
- Tendon TransferДокумент1 страницаTendon TransferPandi Smart VjОценок пока нет
- Interferential Therapy Sept 08Документ8 страницInterferential Therapy Sept 08api-19753815100% (1)
- Physical Therpay Protocols For Conditions of Neck RegionДокумент74 страницыPhysical Therpay Protocols For Conditions of Neck Regionjrpsaavedra4599Оценок пока нет
- The Wrist Common Injuries and ManagementДокумент36 страницThe Wrist Common Injuries and ManagementDan RollorataОценок пока нет
- Physical Therapy Protocols For Conditions of Thorax RegionДокумент52 страницыPhysical Therapy Protocols For Conditions of Thorax RegionVytautas PilelisОценок пока нет
- Flexor Tendon Injuries SeminarДокумент75 страницFlexor Tendon Injuries SeminarAmit GoyalОценок пока нет
- OMT Workshop Techniques - HohnerДокумент43 страницыOMT Workshop Techniques - Hohnerstudentdoc440100% (1)
- Libro IsicoДокумент111 страницLibro Isicoiguija6769Оценок пока нет
- Cervical Spine CYRIAXДокумент16 страницCervical Spine CYRIAXCarlos TavaresОценок пока нет
- The Kinetic Chain Approach To PainДокумент4 страницыThe Kinetic Chain Approach To PaincharbelhannaОценок пока нет
- Pediatric Rehab 2001-2009Документ221 страницаPediatric Rehab 2001-2009beekerdogОценок пока нет
- Shoulder ArthroplastyДокумент53 страницыShoulder ArthroplastyWijaya X PutriОценок пока нет
- Clinical Neurodynamics and Sports Medicine: Origins and DevelopmentДокумент8 страницClinical Neurodynamics and Sports Medicine: Origins and DevelopmentWahid NasrudinОценок пока нет
- Leaflet TbchivДокумент2 страницыLeaflet TbchivNafiys Reeven TeergovОценок пока нет
- Fullpapers Bik376117be181fullДокумент6 страницFullpapers Bik376117be181fullIGusti Ngurah AgungОценок пока нет
- Hubungan Kadar Hbco Dengan Kapasitas Vital ParuДокумент5 страницHubungan Kadar Hbco Dengan Kapasitas Vital ParuKukuh Iman Putra RaharjaОценок пока нет
- WHO Growth Chart Boys (Weight For Age) 0-5 YearsДокумент1 страницаWHO Growth Chart Boys (Weight For Age) 0-5 YearsHendry HuangОценок пока нет
- Regurgitasi AortaДокумент10 страницRegurgitasi AortaNafiys Reeven TeergovОценок пока нет
- Fenton2013growthchartcolor Girls PDFДокумент1 страницаFenton2013growthchartcolor Girls PDFNafiys Reeven TeergovОценок пока нет
- Umn LMNДокумент2 страницыUmn LMNNafiys Reeven TeergovОценок пока нет
- Nomenclature and Classification of Lumbar Disk PathologyДокумент21 страницаNomenclature and Classification of Lumbar Disk PathologyYasemen KОценок пока нет
- WHO Diabetes Definition and DiagnosisДокумент50 страницWHO Diabetes Definition and DiagnosisDavidОценок пока нет
- Legends and Lairs - Elemental Lore PDFДокумент66 страницLegends and Lairs - Elemental Lore PDFAlexis LoboОценок пока нет
- Unit 14 Ergonomics Design: AND ProductДокумент24 страницыUnit 14 Ergonomics Design: AND ProductRämêşh KątúřiОценок пока нет
- Rubric 5th GradeДокумент2 страницыRubric 5th GradeAlbert SantosОценок пока нет
- GP Rating GSK Exit ExamДокумент108 страницGP Rating GSK Exit ExamMicle VM100% (4)
- Individual Performance Commitment and Review Form (Ipcrf) : Mfos Kras Objectives Timeline Weight Per KRAДокумент4 страницыIndividual Performance Commitment and Review Form (Ipcrf) : Mfos Kras Objectives Timeline Weight Per KRAChris21JinkyОценок пока нет
- The Smith Generator BlueprintsДокумент36 страницThe Smith Generator BlueprintsZoran AleksicОценок пока нет
- Allan S. Cu v. Small Business Guarantee and FinanceДокумент2 страницыAllan S. Cu v. Small Business Guarantee and FinanceFrancis Coronel Jr.Оценок пока нет
- Guia de Usuario GPS Spectra SP80 PDFДокумент118 страницGuia de Usuario GPS Spectra SP80 PDFAlbrichs BennettОценок пока нет
- Pfr140 User ManualДокумент4 страницыPfr140 User ManualOanh NguyenОценок пока нет
- Felizardo C. Lipana National High SchoolДокумент3 страницыFelizardo C. Lipana National High SchoolMelody LanuzaОценок пока нет
- Mil STD 2154Документ44 страницыMil STD 2154Muh SubhanОценок пока нет
- ArДокумент26 страницArSegunda ManoОценок пока нет
- Unr Ece R046Документ74 страницыUnr Ece R046rianteri1125Оценок пока нет
- Paradigms of ManagementДокумент2 страницыParadigms of ManagementLaura TicoiuОценок пока нет
- LIST OF ENROLLED MEMBERS OF SAHIWAL CHAMBER OF COMMERCEДокумент126 страницLIST OF ENROLLED MEMBERS OF SAHIWAL CHAMBER OF COMMERCEBASIT Ali KhanОценок пока нет
- The Service Marketing Plan On " Expert Personalized Chef": Presented byДокумент27 страницThe Service Marketing Plan On " Expert Personalized Chef": Presented byA.S. ShuvoОценок пока нет
- Evaluative Research DesignДокумент17 страницEvaluative Research DesignMary Grace BroquezaОценок пока нет
- 2018 NAMCYA CHILDREN'S RONDALLA ENSEMBLE GuidelinesДокумент3 страницы2018 NAMCYA CHILDREN'S RONDALLA ENSEMBLE GuidelinesJohn Cedrick JagapeОценок пока нет
- CBT For BDDДокумент13 страницCBT For BDDGregg Williams100% (5)
- Correlation Degree Serpentinization of Source Rock To Laterite Nickel Value The Saprolite Zone in PB 5, Konawe Regency, Southeast SulawesiДокумент8 страницCorrelation Degree Serpentinization of Source Rock To Laterite Nickel Value The Saprolite Zone in PB 5, Konawe Regency, Southeast SulawesimuqfiОценок пока нет
- Financial Analysis of Wipro LTDДокумент101 страницаFinancial Analysis of Wipro LTDashwinchaudhary89% (18)
- A Reconfigurable Wing For Biomimetic AircraftДокумент12 страницA Reconfigurable Wing For Biomimetic AircraftMoses DevaprasannaОценок пока нет
- Training Customer CareДокумент6 страницTraining Customer Careyahya sabilОценок пока нет
- Sinclair User 1 Apr 1982Документ68 страницSinclair User 1 Apr 1982JasonWhite99Оценок пока нет
- Listening Exercise 1Документ1 страницаListening Exercise 1Ma. Luiggie Teresita PerezОценок пока нет
- HVAC Master Validation PlanДокумент51 страницаHVAC Master Validation Plannavas197293% (30)
- Price List PPM TerbaruДокумент7 страницPrice List PPM TerbaruAvip HidayatОценок пока нет
- Kalley Ltdn40k221twam Chassis msd6308 SM PDFДокумент49 страницKalley Ltdn40k221twam Chassis msd6308 SM PDFjulio cesar calveteОценок пока нет
- Why Choose Medicine As A CareerДокумент25 страницWhy Choose Medicine As A CareerVinod KumarОценок пока нет