Академический Документы
Профессиональный Документы
Культура Документы
Engelman - 2016 - Skin NTDs PDF
Загружено:
owusuesselОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Engelman - 2016 - Skin NTDs PDF
Загружено:
owusuesselАвторское право:
Доступные форматы
Opinion
Opportunities for Integrated
Control of Neglected Tropical
Diseases That Affect the Skin
Daniel Engelman,1,2,* L. Claire Fuller,3,4 Anthony W. Solomon,5
James S. McCarthy,6 Roderick J. Hay,4,7 Patrick J. Lammie,8
and Andrew C. Steer1,2
Many neglected tropical diseases (NTDs) affect the skin, causing considerable
Trends
disability, stigma, and exacerbation of poverty. However, there has been rela-
Skin manifestations are a major contri-
tively little investment into laboratory research, epidemiology, diagnostic tools butor to the disability and stigma of
or management strategies to control tropical skin disease. Integration may neglected tropical diseases.
advance the control of skin disease across a range of domains, including Integration of control efforts for tropical
mapping, diagnosis, clinical management, and community control measures skin diseases may facilitate advance-
such as mass drug administration. Examples of successful integration strate- ment in the understanding and control
of this diverse group of diseases.
gies include programs targeting scabies, impetigo, yaws, and diseases causing
lymphoedema. Future strategies should build on these experiences and the Integration of mapping, surveillance,
clinical diagnosis, and management
experience of integration of other NTDs, strengthen existing health systems,
has been achieved in a limited range
and contribute toward the attainment of Universal Health Coverage. Strong of settings and disease groupings, but
partnerships and political support and will be necessary to achieve these goals. its potential has not yet been fully
realized.
NTDs of the Skin – Redefining an Ancient Problem Integration of mass drug administration
NTDs are a group of conditions sharing common features – they cause considerable morbidity could allow treatment and control of
and disability, and affect the poorest, most disadvantaged populations with notable geo- multiple conditions for a greater overall
benefit, with increased cost-effective-
graphic clustering. Although these diseases have afflicted humans for millennia, and affect ness compared to single disease
more than 1 billion people, they were largely neglected in terms of funding, advocacy, research, programs.
and drug development during the 20th century [1,2]. Since 2003 the World Health Organization
(WHO) and international research and implementation partners have made considerable
advances in the control of some NTDs. Targets for control, elimination, and eradication
1
now exist for many diseases, as established by the 2012 London Declaration (unitingtocom- Centre for International Child Health,
University of Melbourne, Melbourne,
batntds.org/resource/london-declaration) and the WHO NTD roadmap (apps.who.int/iris/ Australia
handle/10665/70809) endorsed by the World Health Assembly in 2013 (apps.who.int/iris/ 2
Group A Streptococcal Research,
handle/10665/150163). Murdoch Childrens Research Institute,
Melbourne, Australia
3
Chelsea and Westminster Hospital,
However, one underappreciated dimension of the NTD grouping is that many of the diseases London, UK
4
affect the skin, either as the primary manifestation or as an associated clinical feature. Until now International Foundation for
Dermatology, London, UK
the skin morbidity of individual NTDs has not been a prominent driver for the control agenda. 5
Department of Control of Neglected
However, reconceptualizing the collective morbidity of skin disease caused by the NTDs as a Tropical Diseases, World Health
group reveals a much greater burden. Skin manifestations are highly visible (Figure 1, Key Organization, Geneva, Switzerland
6
Queensland Institute of Medical
Figure), and therefore are major contributors to the disability, stigma, and exacerbation of Research Berghofer Medical Research
poverty associated with NTDs [3]. When considered in parallel with the relatively low activity Institute, University of Queensland,
in laboratory and operational research, and the major deficiencies in our understanding and tools Brisbane, Australia
7
King's College London, King's
to combat some of these diseases, there is a strong case for further investment in research and College Hospital National Health
the development of control strategies. While this investment appears unlikely to be forthcoming Service Trust, London, UK
Trends in Parasitology, November 2016, Vol. 32, No. 11 http://dx.doi.org/10.1016/j.pt.2016.08.005 843
© 2016 Elsevier Ltd. All rights reserved.
8
Key Figure Centers for Disease Control and
Prevention, Atlanta, GA, USA
Neglected Tropical Diseases Affecting the Skin
*Correspondence:
Daniel.Engelman@rch.org.au
(A) (B) (D. Engelman).
(C) (D)
Figure 1. (A) Cutaneous leishmaniasis. (B) Scabies. (C) Nodular chromoblastomycosis. (D) Mycetoma. Images courtesy of:
Regional Dermatology Training Centre, Moshi, Tanzania (A,C); Daniel Mason (B); and Roderick Hay (D).
for individual skin diseases in the foreseeable future, integration provides an opportunity to
leverage funding for the control of multiple NTDs that affect the skin.
Models of Integration
We define integration here to mean combining activities for two or more diseases, at the same
time, and in the same communities, with the aim of increasing effectiveness and/or efficiency.
This is in contrast to coordination, where stakeholders and implementing partners for discrete
programs communicate and work in a way that avoids conflict and competition, but without
sharing resources and personnel. While both strategies are important, and either may be
appropriate in specific contexts, we focus specifically on integration. The importance of inte-
gration at national and international levels to improve effectiveness and efficiency is emphasized
within the commitments of the London Declaration.
Opportunities for integration are numerous and include mapping, training, clinical diagnosis and
management, and community control. Integration strategies could be developed at various levels,
including among the NTDs affecting the skin; with skin conditions that have existing control or
elimination programs; with the broader NTD control movement; and within the global framework
of development outlined in the Sustainable Development Goals and associated targets. Integra-
tion can be delivered either through a national NTD program, overseeing and coordinating
844 Trends in Parasitology, November 2016, Vol. 32, No. 11
campaigns using a vertical model, or a more truly horizontal approach where programs are
embedded into routine healthcare delivery and prevention systems [4]. The major burden of NTDs
exists in areas where health systems are fragile and under-resourced. Therefore, integration
should facilitate the development of more resilient health systems and advance work toward the
alleviation of poverty, rather than remaining limited by disease-specific program goals.
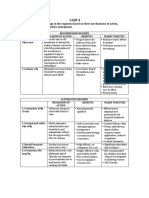
The Spectrum and Burden of Skin Disease Caused by NTDs
Nine of the WHO's main list of 17 NTDs have important skin manifestations. In addition, several
other skin conditions, consistent with the features of NTDs, appear on the NTD lists of WHO
regional offices [5] or the Public Library of Science [6] (Table 1). The list comprises a diverse
group of conditions. Some have advanced control or elimination strategies, backed by World
Health Assembly resolutions, and others (e.g., scabies, podoconiosis, and mycetoma) have to
date struggled to attract global attention and have been referred to as the most ‘neglected of the
neglected’ [2,7–10].
The global burden of many NTDs affecting the skin remains largely unknown. The Global Burden
of Disease (GBD) 2010 study estimated skin conditions as a whole to be the 18th leading cause
of health burden worldwide, and one of the top-10 causes of non-fatal disability [11]. These data,
particularly estimates of disability, have limitations and are likely to underestimate the true
burden, owing to the relative lack of data and the way in which GBD study methodology
assigns disability weights. These diseases frequently coexist with other NTDs and other health
conditions, and may not be the primary health problem affecting an individual. Therefore
ascribing burden between discrete diseases and their sequelae is methodologically challenging.
Skin conditions are among the most frequent complaints affecting communities in resource-
limited areas. They account for a large proportion of health-clinic presentations [12] and, because
prevalence is underestimated by self-reporting compared to clinical examination [13], the real
burden is likely to be even greater. Many conditions disproportionately affect children, and the vast
majority are eminently treatable [14]. The most prevalent skin NTDs globally are scabies and
bacterial skin infections (Box 1). Many of the conditions that cause a breach in the skin barrier
predispose to bacterial skin infection. This is most notably associated with scabies [15,16], related
to breakdown of the skin by scratching and factors specific to the scabies mite [17]. Superficial
bacterial infections, particularly with group A Streptococcus, further predispose to severe,
invasive infection and autoimmune sequelae affecting the heart and kidneys, and cause hundreds
of thousands of deaths annually [18]. Some diseases are concentrated in distinct geographic
areas: for example, paracoccidioidomycosis in tropical Latin America; tinea imbricata in Southeast
Asia, the South Pacific, and Latin America [19]; and podoconiosis in high-altitude, volcanic areas
of tropical Africa, Central America, and North India [10].
Many other skin conditions are not considered to be NTDs and are beyond the scope of this
review [20]. Common infectious diseases affecting the skin in tropical areas include dermato-
phyte and yeast infections, insect bites, molluscum contagiosum, warts (human papilloma virus),
herpes simplex virus, and Kaposi sarcoma (human herpesvirus 8). Many viruses causing
systemic infection, including measles, varicella, rubella, dengue, chikungunya, and zika, also
present with rash. Important non-infectious skin conditions include ulcers due to diabetes
mellitus and chronic venous stasis, itch, acne vulgaris, atopic dermatitis (eczema), skin cancer,
snakebite, trauma, and burns.
Opportunities and Challenges of Integration
Integrated Disease Mapping and Surveillance
A primary barrier to the control of many of the NTDs affecting the skin is a paucity of
epidemiological data. Therefore mapping is arguably the most pressing issue. Control of several
Trends in Parasitology, November 2016, Vol. 32, No. 11 845
Table 1. Neglected Tropical Diseases Affecting the Skin
Condition Major skin manifestations WHO NTD Estimated Refs
list and global
road map burden
Buruli ulcer Slow-growing, painless ulcer, with undermined Yes NDa
edge, mainly lower limb
Chromoblastomycosis Papules, nodules, and plaques with superficial black ND
dots
Cutaneous lava migrans Serpiginous, itching lesions, occasional blistering ND
Dracunculiasis (guinea worm) Burning, itching, blisters, ulceration Yes Nearing [83]
eradication
Endemic systemic mycoses Coccidioidomycosis: papules, plaques, ulcers, ND
abscess, erythema nodosum
Histoplasmosis: papules, pustules, nodules,
erythema nodosum
Paracoccidioidomycosis: painful ulcerated lesions
particularly affecting the mouth and face.
Talaromyces marneffei: umbilicated papules and
mucosal lesions
Endemic treponematoses Primary papules and papillomata (‘mother yaw’), Yes 2.5 million [75]
(yaws) multiple secondary papules, ulcers, patches, and
plaques
Human African Itch during the hemolymphatic stage, then primary Yes 37 thousand [84]
trypanosomiasis (sleeping chancre (painful, red lesion with ulcers) symptomatic
sickness)
Impetigo/cellulitis/skin abscess Pustules, blisters, ulcers with crusts, erythema, 141 million [11]
(bacterial skin diseases) folliculitis, abscesses with impetigo
Leishmaniasis (cutaneous) Plaques, painless ulcers on exposed areas Yes 10 million [84]
Leprosy Hypopigmented macules, plaques, neuropathic Yes 189 000
ulcers, lepra reactions
Lymphatic filariasis Limb swelling, nodules, acute lymphangitis Yes 120 million [84]
infected;
36 million with
lymphoedema/
hydrocele
Mycetoma Swelling and fibrosis with overlying sinus ND
discharging grains
Myiasis (fly larva infection) Nodules with overlying punctum ND
Onchocerciasis Itch, macules, papules, nodules, plaques, Yes 30 million [84]
depigmentation
Pediculosis (head, body, Itch, papules ND
pubic lice)
Podoconiosis Limb swelling, nodules, hyperkeratotic surface 4 million [85]
roughness (‘mossy change’), acute lymphangitis
Scabies Severe itch, papules, burrows, secondary infection 100 million [11]
Schistosomiasis Wheals, nodules, itch Yes 30 million [84]
Strongyloidiasis Itchy papules and vesicles (site of penetration); 30–100 million [86]
severe itch, linear urticarial rash (larva currens)
Tropical ulcer (including Ulcers, particularly lower limbs ND
Fusobacterium ulcerans)
Tungiasis (sand flea disease) Papules on extremities, itch, pain, secondary ND
infection
a
ND, no data.
846 Trends in Parasitology, November 2016, Vol. 32, No. 11
Box 1. Scabies Case Study
Scabies is a parasitic skin condition affecting people of all ages in every country; however, the burden of disease is most
pronounced in tropical regions. Scabies disproportionately affects children and the disadvantaged. The disease burden
is conservatively estimated at 100 million cases at any time [11], but prevalence data from most regions remain patchy.
Outbreaks in institutions and refugee and displaced persons camps are common. In the Pacific region the prevalence in
children is around 20–30% [16]. The severe itch and rash cause sleep disturbance, stigma, and economic costs to
families. In addition, scabies predisposes to bacterial skin infections, which in turn cause serious complications and
considerable mortality as a result of invasive infections, as well as autoimmune disease leading to chronic kidney disease
and possibly rheumatic heart disease [18]. Although fulfilling the criteria for an NTD, scabies is not currently included on
the WHO NTD list, limiting the visibility of the problem and hindering access to funding. Scabies is recognized as a priority
NTD by some regional offices [5]. Clinical diagnosis can be challenging, particularly in individuals with dark skin, and there
are several differential diagnoses [76]. There is no available diagnostic test or consensus case definition for epidemiologic
surveys, although preliminary work is underway in both areas [18].
Current case-and-contact treatment strategies are limited by adherence to messy topical treatments, especially in
contacts, and reinfestation is common [77]. By contrast, community mass treatment programs, in particular using oral
ivermectin, appear to be highly effective at reducing the prevalence of scabies and secondary impetigo in island
communities [78,79]. However, long-term effectiveness in diverse settings has not yet been demonstrated, and a study
from Australia did not show a significant impact, possibly owing to lower baseline prevalence, a highly mobile population,
and the presence of individuals with highly-infectious crusted scabies [80]. Important operational research questions
remain – including dosing strategy and effectiveness in preventing severe complications such as invasive infections,
kidney disease, and rheumatic heart disease.
There are several examples of integrating scabies with existing NTD control programs and operational research to further
the scabies control agenda. Successful mapping and coadministration of mass treatment studies have been conducted
in the Solomon Islands, integrating with existing programs for trachoma and yaws [81]. Further integrated activities are
planned as part of research assessing the impact of triple-drug treatment for LF [49]. Additional major challenges to a
mass treatment program include the expense of treatments. The Mectizan Donation Program for ivermectin is limited to
onchocerciasis and LF programs, and there is currently no donation pathway for topical treatments for small children or
pregnant women who cannot take ivermectin. The development of moxidectin, a macrocyclic lactone similar to
ivermectin, but with a much longer half-life, for the treatment of human scabies is encouraging [82].
Two countries (Ethiopia and Fiji) with extensive experience in NTD control are currently developing comprehensive
scabies control programs, and an international alliance has formed to advance collaboration [18]. Further research
demonstrating the burden of disease, and the effectiveness and safety of control strategies, may increase the visibility of
scabies control within the global health agenda and attract the attention of international agencies and donors.
diseases is constrained by the present scenario in which funding is not available to undertake
robust epidemiological research to demonstrate disease burden, but, without a sound under-
standing of burden and geographic distribution, it is not possible to advocate for required
resources or develop control strategies. Integration of mapping with existing, funded ventures
offers a way forward.
For example, in the Global Trachoma Mapping Project (GTMP), completed in December 2015,
population-based prevalence surveys were completed for >1500 suspected endemic districts
for trachoma across 29 countries, and over 2.6 million people were examined [21]. The GTMP
was an enormous undertaking, involving the mobilization of more than 500 teams to perform
clinical examination in often very remote communities, and received considerable funding (more
than £16 million from the UK Department for International Development and the US Agency for
International Development). In addition to the major achievements specific to trachoma, the
GTMP achieved successful integration with yaws mapping in the Solomon Islands [22] and
guinea worm case finding in Sudan and Ethiopia. Mapping of schistosomiasis, soil-transmitted
helminths, and lymphatic filariasis (LF) was also coordinated in parts of Africa. However, these
examples represent only a few of the > 1500 GTMP districts. It is unlikely that the level of funding
provided for the GTMP will be made available for other single-disease mapping projects. Future
exercises should again pursue integration to fully leverage the available resources, workforce,
and infrastructure to advance understanding of multiple NTDs.
Trends in Parasitology, November 2016, Vol. 32, No. 11 847
Two disease programs are currently undertaking or planning large survey projects to assess the
impact of community treatment interventions: transmission assessment surveys (TAS) for LF
[23], and impact and surveillance surveys for the global trachoma program, using the Tropical
Data platform (www.tropicaldata.org). These large-scale projects represent tremendous oppor-
tunities for integrated mapping. Guidelines already exist for integrating the assessment of
prevalence of helminth infections within TAS.
There are several prerequisites for successful integration of data collection between
NTDs. First, regional co-endemicity must be established. Second, the epidemiologic pro-
tocols and rigor required for each specific disease must be compatible. For example, if
population-based prevalence estimates of skin NTDs are required, they may be more readily
integrated with trachoma surveys than with school-based surveys for schistosomiasis
and soil-transmitted helminths. Third, training and assessment protocols for each disease
need to be agreed and compatible. Consensus case definitions for epidemiologic
surveys are required, such as those existing for Buruli ulcer and podoconiosis [9], but
which are currently lacking for scabies and tropical ulcer. Fourth, and perhaps most
challenging, there must be political, donor, and partner support for integrated fieldwork.
Ethical dimensions for each disease, including privacy for skin exposure for clinical exami-
nation, and provision of information, referral, and treatment of suspected cases must also be
considered.
The distribution and clustering of NTDs by age, gender, and geography means that some
diseases are more suitable for integrated mapping. For example, integrated data collection on
podoconiosis and LF may be appropriate within the known, endemic regions for podoco-
niosis, as successfully shown in Ethiopia [24]. Integrated mapping is more likely to succeed if
the same ages are targeted. For diseases that affect the whole lifespan, but with a predomi-
nance of cases in children, such as scabies and impetigo, protocols that limit data collection
to targeted age-ranges may better facilitate integration. For example, focusing on school-
going children may enable integration with mapping of soil-transmitted helminths. Likewise,
integration of skin NTD mapping with existing maternal and child health services, immuniza-
tion programs, malaria indicator surveys, or demographic and health surveys may be feasible
in some settings. Integration may be more challenging where conditions require vastly
different assessment procedures, such as a lengthy clinical assessment or complex collection
of specimens.
Program goals need to be considered, whether control, elimination, or eradication [25]. Pro-
grams aiming to eliminate transmission or eradicate infection are obliged to sustain efforts to
achieve a very low or zero threshold, including reaching populations in the most geographically
or politically difficult areas. However, for many other NTDs affecting the skin, disease control may
be a more appropriate goal, and data collection could be initially limited to more-accessible
locations and populations. The stage of a program, whether mapping at baseline or undertaking
surveys to assess the impact of an intervention, may also affect integration feasibility. Therefore
defining the control priorities for each region is a key task.
In the longer term, emerging techniques such as multiplex bead array serological assays on
dried bloodspots have the potential to allow integrated, large-scale sero-surveys of several
skin NTDs, which could be integrated with surveys for other NTDs as well as for malaria
or vaccine-preventable diseases. The technique has now been evaluated for yaws, LF,
onchocerciasis, and strongyloidiasis [26,27], and further development for other skin NTDs
would be a major advance. It may be possible to apply nucleic acid diagnostic methods such
as loop-mediated isothermal amplification [28] as the understanding of organism genomes
increases [29].
848 Trends in Parasitology, November 2016, Vol. 32, No. 11
Integrated Clinical Diagnosis
Few skin NTDs have diagnostic tests, and therefore clinical examination will remain the corner-
stone of diagnosis, for at least the medium term. Training health workers in the diagnosis of
individual diseases during vertical NTD programs is inefficient. By contrast, brief, integrated
training programs, utilizing syndrome-based assessment tools, have been developed for many
skin conditions including scabies, bacterial skin infections, and leprosy [30–32] and could be
incorporated into non-skin NTD training programs. Teledermatology collaborations can also
enhance the reach of more-specialized dermatological services into remote areas and margin-
alized populations [33]. Brief dermatological training, when integrated into primary healthcare
services, can result in improvements in diagnosis, management, and reduction in prescription
costs [34,35]. Early diagnosis of chronic skin NTDs such as Buruli ulcer and mycetoma is likely to
lead to improved outcomes.
However, despite the theoretical appeal of all-encompassing integrated training and diagnosis
for NTDs and skin disease, it is vital to keep teaching and health system processes simple.
Complicated assessment protocols may not be appropriate for all levels of health workers [4],
and future integrated training schemes should be assessed for validity. The lack of validated
diagnostic criteria for many skin NTDs remains a challenge, and may need to be region-specific.
For example, a patient with itch and papules in the South Pacific may have a high likelihood of
scabies, but, because onchocerciasis can also present with these symptoms, a more-nuanced
approach to diagnosis is required in onchocerciasis-endemic areas [36].
Integrated Community Control Using Mass Drug Administration
While the largest NTD control programs all commenced as disease-specific interventions,
resource limitations led to consideration of integration in areas where diseases overlap, particu-
larly Sub-Saharan Africa and Latin America [37]. There is now more than a decade of experience
in the integration of NTD control. Lessons, including successes and failures, provide a strong
basis for the design of future integration efforts [4,38–40]. Integration of preventative chemo-
therapy for seven of the most prevalent NTDs, through the creation of ‘rapid impact packages’ of
multiple drugs, distributed using a coordinated, community-based system, can provide con-
siderable cost-savings. Estimates that up to seven major NTDs could be controlled for as little as
$0.50 per person (in large part due to drug donation programs) has proved powerful for
advocacy for control of those diseases [41].
The drug ivermectin is one of the major tools in the control of NTDs. It is highly effective at killing
microfilariae in patients with onchocerciasis and LF, and billions of doses have been given to
prevent these conditions [42]. The immense benefits of ivermectin to human health were
acknowledged by the award of the 2015 Nobel Prize for Medicine to William Campbell and
-
Satoshi Omura [43]. Ivermectin is also the drug of choice for treatment of strongyloidiasis, and is
active against several skin parasites including scabies, pediculosis, and cutaneous larva migrans
[44]. Thus, there is mounting evidence suggesting that mass drug administration (MDA) using
ivermectin may be highly effective in the control of several skin NTDs. Selective MDA using
ivermectin in Brazil considerably reduced the prevalence of numerous coexisting parasitic
infections [45]. Ivermectin MDA has been shown to improve skin health from non-target
diseases, particularly scabies, as part of the African Program for Onchocerciasis [46] and
the Global Programme to Eliminate LF [42]. Indirect measurement of the impact of annual
ivermectin MDA for LF in Zanzibar showed a dramatic decrease in clinic presentations for
scabies [47].
The off-target effects of ivermectin in reducing itch and treating skin conditions are major drivers
of community adherence to MDA [48]. These factors will become increasingly important as LF
and onchocerciasis programs approach the elimination endpoint, and maximizing adherence
Trends in Parasitology, November 2016, Vol. 32, No. 11 849
becomes crucial. Furthermore, as these two successful programs begin stopping MDA in
selected regions, the effects of ivermectin on skin diseases have become more apparent.
For example, there are reports of a resurgence of scabies cases in Ecuador in communities
where ivermectin MDA for onchocerciasis has been discontinued (C. Mackenzie, personal
communication).
The current investigation of a triple drug combination (ivermectin, albendazole, and diethylcar-
bamazine citrate, DEC) for LF [49] represents another major opportunity to gather epidemiologic
data and to investigate the effects on skin NTDs in a variety of settings. The potential addition of
ivermectin to LF programs in regions that currently use albendazole and DEC could increase
community acceptance and MDA coverage though the treatment of skin conditions, resulting in
reduced program duration and treatment cycles to achieve elimination [50]. Integration with
broader public health programs such as vitamin A and micronutrient supplementation, distri-
bution of insecticide-treated nets, and health education is also feasible in some settings, as is
integration with the major global programs of AIDS, tuberculosis, and malaria [51], particularly if
MDA is employed as part of malaria eradication efforts [52].
Despite the opportunities of integrated MDA, there are numerous challenges. For many skin
NTDs the optimal MDA strategy is unknown – how many doses should be given, how often, and
for how many rounds is uncertain. There are differences in the recommended doses for skin
NTDs and other diseases. For example, the recommended dose of ivermectin for onchocercia-
sis is 150 mg/kg, but higher for scabies at 200 mg/kg, with a second dose repeated at 7–14 days.
Similarly, azithromycin for trachoma is administered at 20 mg/kg (maximum 1 g), whereas for
yaws the recommended dose is higher at 30 mg/kg (maximum 2 g) [53]. Despite these differ-
ences, initial evidence suggests that the lower-dose MDA regimens for onchocerciasis and
trachoma have considerable effect on the corresponding skin diseases [47,54]. Operational
research is required to address the optimal dose and comparative effectiveness of alternative
strategies. A further issue is that ivermectin is currently not recommended in young children or
pregnant women, necessitating additional treatments with topical permethrin for community
control of scabies in these groups. Pharmacokinetic and safety studies could further facilitate
integration of MDA.
Another barrier is the possible risk of drug coadministration for multiple diseases. Safety
considerations are paramount for MDA programs, where the majority of the population is
unaffected by the target condition. Ivermectin and albendazole can be safely coadministered,
and there is a growing body of safety evidence around the coadministration of these two drugs
with other NTD medications such as azithromycin [55], praziquantel [56], and DEC [49].
Additional coadministration studies will be important for planning of integrated control.
The potential for development of resistance in target or off-target organisms must also be
considered. Ivermectin resistance has been demonstrated in case reports for scabies [57],
although only in patients with severe, crusted scabies who had received >30 doses, and
therefore this risk may not translate to an MDA setting. Although clinically significant resistance
of Chlamydia trachomatis to azithromycin has not been demonstrated, potential selection for
resistance in other pathogenic bacteria, such as Streptococcus pneumoniae [58,59] and
Streptococcus pyogenes [60], is a cause for caution. This risk may depend in part on the
background frequency of macrolide resistance [61].
While MDA for conditions such as yaws and scabies offers promise, there are several NTDs
affecting the skin for which an MDA strategy will not be beneficial. These include diseases where
the treatment is complex or has significant side-effects (such as cutaneous leishmaniasis and
leprosy), where the risk of drug resistance is high, or where diseases occur at hypo-endemic
850 Trends in Parasitology, November 2016, Vol. 32, No. 11
levels. MDA may not provide effective community control for zoonotic conditions such as
leishmaniasis, myiasis, and tungiasis.
Beyond the Drugs: Integrated Prevention and Management of Disability
Following the successes of MDA programs in reducing infection transmission and disease
incidence, there is increasing attention on the management of morbidity and disability for the
millions of people already affected by symptomatic disease. There is an opportunity for the skin
NTDs to play a lead role in this movement. Morbidity management programs can sensibly be
integrated where commonalities exist. For example, treatment packages for podoconiosis,
including education, hygiene, emollients, elevation, and use of footwear, would likely also be
effective for LF, owing to the common need to prevent secondary infection and to control
lymphoedema and acute adenolymphangitis [62,63]. Home-based management strategies
require minimal resources and can be highly effective [64]. Ulceration is a complication of
several skin NTDs, including Buruli ulcer, tropical ulcer, yaws, and leprosy, and is also an issue
for many individuals with diabetes or vascular insufficiency. An integrated approach to wound
healing could be implemented, even in instances where the diagnosis is unclear or diagnostic
services are unavailable. Furthermore, a prototype toolkit has been developed for integrated
monitoring of disability and morbidity caused by NTDs, including Buruli ulcer, leishmaniasis,
leprosy, and podoconiosis [65].
Prevention of several conditions could also be integrated. Basic interventions such as the
provision of footwear and washing of the lower limbs would reduce the incidence of many
conditions, including podoconiosis, tungiasis, and tropical ulcer, but remain challenging to
resource and implement. Further integration between water, sanitation, and hygiene programs
will be necessary to achieve these goals [66].
Factors Underlying Successful Integration
While integration offers great potential for synergy and effective public health programs, it is far
from a simple process. In addition to the specific opportunities and challenges discussed above,
several crucial factors will be essential for successful integration.
Support of the WHO
WHO recommendations remain highly influential for country health programs. Many of the skin
NTDs discussed here are not part of the WHO list, and are therefore not included in the WHO
global NTD roadmap for implementation (Table 1). The finite resources of WHO understandably
necessitate some process of prioritization. However, there is a risk that opportunities for
synergistic integration may be missed. Sustained advocacy from country and regional dele-
gations may prompt change. For example, following submissions from Sudan, Nigeria, and
Egypt, the 69th World Health Assembly (May 2016) adopted a resolution to officially include
mycetoma among the diseases termed ‘neglected tropical diseases’ (www.who.int/
neglected_diseases/news/WHA_69_adopts_mycetoma_resolution/). The WHO Strategic and
Technical Advisory Group for NTDs has proposed a systematic, technically driven process for
evaluating and potentially adopting additional diseases as NTDs, recognizing that increased
attention can assist in advocacy, mobilization of resources, and the development of new tools
(www.who.int/neglected_diseases/diseases/Adoption_additional_NTDs.pdf).
Political Support and Partnerships
Integration is not possible without strong and sustained political support, but challenges to this
support may arise at any level. Initial optimism around concepts of integration may shift to
resistance as policy and logistic implications become clear. Clinicians, researchers, and non-
governmental development leaders may have spent entire careers focused on a specific
disease. Program managers, staff, and community workers would require considerable training
Trends in Parasitology, November 2016, Vol. 32, No. 11 851
and support to manage the diversity of skin conditions and the complexity of integrated control. Outstanding Questions
A new, integrated approach to NTD control will require a major shift in mind-set, driven by a Can strategies that have been suc-
willingness to share and to make concessions from highest standards for one disease for the cessful in the control of NTDs such
as lymphatic filariasis and onchocerci-
greatest overall impact on community wellbeing. Structures within national Ministries of Health asis be applied to other NTDs affecting
and governments, especially responsibilities of national and regional/district health services, may the skin?
be fragile, and restructuring of existing health program leadership and processes can be a
significant barrier [4]. Strong partnerships are required between governments, international Can MDA with oral ivermectin lead to a
sustainable reduction in scabies and
agencies, implementing partners, and donors. Relationships with complementary programs in
impetigo?
the water and sanitation [66–68], education, and health sectors are vital.
Can MDA of multiple drugs be given
Resources and Funding safely, efficiently, and effectively?
It is likely that integration of community treatment programs will deliver substantial cost-savings
compared to vertical funding models, particularly through reduced costs of community distri- How can groups working on diverse
NTDs collaborate toward the shared
bution, as seen with integration of MDA programs in Africa [69–71]. Current funding for many
goal of reducing morbidity in disadvan-
control programs exists in vertical, disease-specific streams that are inflexible to integration with taged populations?
other programs. Without additional funding and human resources, adding more diseases could
represent a risk. Several existing NTD control programs have built considerable momentum over How can the global health community
many years and are working toward ambitious targets. It is important that integration of new improve the control of skin conditions
affecting the most disadvantaged pop-
programs focusing on the skin does not undermine the success of the existing programs [72].
ulations without diverting required
Currently, NTD control is heavily reliant on drug donation programs, which are generally directed resources from current NTD
to specific diseases with defined public health targets and a clear ‘end-point’. For example, programs?
expansion of the Mectizan Donation Program to include ivermectin for the control of skin and/or
intestinal parasites would represent a major policy shift. External factors such as conflict and
natural disasters may also divert attention and resources from health programs.
Concluding Remarks and Future Perspectives
Neglected diseases of the skin disproportionately affect the world's most disadvantaged people,
cause significant morbidity, and exacerbate the cycle of poverty. The nations of the world have
pledged to end extreme poverty and address global inequality through the Sustainable Devel-
opment Goals initiative. However, efforts to achieve these goals will be hindered without
improving our understanding of the epidemiology of the most neglected conditions, and without
considerable investment in operational research for diagnosis, community control, and morbidity
management for the major skin NTDs. A sustainable strategy should work to strengthen existing
health systems [73], and could even lead efforts toward attainment of Universal Health Coverage
[74,75] by providing services to populations that hitherto have had little or no access. One step
may involve the formation of a collaborative network from diverse health backgrounds, including
those with expertise in specific diseases, integration, and political leadership, to further drive this
agenda. There are undoubtedly numerous challenges (see Outstanding Questions) but, given
careful consultation with, and support from, the wider health and development communities,
there are also numerous opportunities to improve the control of these truly neglected conditions.
Acknowledgments
This manuscript emerged from presentations made at, and discussions arising from, Symposium 57 (‘Neglected Tropical
Diseases and the Skin: Integration, Surveillance and Control’) of the 64th Annual Meeting of the American Society of Tropical
Medicine and Hygiene, held in October 2015 in Philadelphia, USA. D.E., J.S.M., and A.C.S. are supported by Australian
National Health and Medical Research Council research fellowships. D.E. and A.C.S. are additionally supported by the
National Heart Foundation of Australia. A.W.S. is an employee of the WHO. The views expressed in this article are the views
of the authors alone and do not necessarily reflect the decisions or the stated policy of the WHO.
References
1. World Health Organization (2010) Working to Overcome the 2. Hotez, P. et al. (2006) The neglected tropical diseases: the ancient
Global Impact of Neglected Tropical Diseases: First WHO Report afflictions of stigma and poverty and the prospects for their control
on Neglected Tropical Diseases, World Health Organization and elimination. Adv. Exp. Med. Biol. 582, 23–33
852 Trends in Parasitology, November 2016, Vol. 32, No. 11
3. Hofstraat, K. and van Brakel, W.H. (2016) Social stigma towards 29. Mofiz, E. et al. (2016) Genomic resources and draft assemblies of
neglected tropical diseases: a systematic review. Int. Health 8, the human and porcine varieties of scabies mites. Sarcoptes
i53–i70 scabiei var. hominis and var. suis. GigaScience 5, 23
4. Kabatereine, N.B. et al. (2010) How to (or not to) integrate vertical 30. Steer, A.C. et al. (2009) Validation of an Integrated Management of
programmes for the control of major neglected tropical diseases in Childhood Illness algorithm for managing common skin conditions
sub-Saharan Africa. PLoS Negl. Trop. Dis. 4, e755 in Fiji. Bull. World Health Organ. 87, 173–179
5. World Health Organization Western Pacific Region (2013) Regional 31. Faye, O. et al. (2007) A public health approach for leprosy detec-
Action Plan for Neglected Tropical Diseases in the Western Pacific tion based on a very short term-training of primary health care
(2012-2016), World Health Organization workers in basic dermatology. Lepr. Rev. 78, 11–16
6. Hotez, P. (2007) A new voice for the poor. PLoS Negl. Trop. Dis. 1, 32. Mahe, A. et al. (2005) Definition of an algorithm for the manage-
e77 ment of common skin diseases at primary health care level in sub-
7. Zijlstra, E.E. et al. (2016) Mycetoma: a long journey from neglect. Saharan Africa. Trans. R. Soc. Trop. Med. Hyg. 99, 39–47
PLoS Negl. Trop. Dis. 10, e0004244 33. Hay, R. et al. (2011) Managing skin disease in resource-poor
8. Hengge, U.R. et al. (2006) Scabies: a ubiquitous neglected skin environments – the role of community-oriented training and control
disease. Lancet Infect. Dis. 6, 769–779 programs. Int. J. Dermatol. 50, 558–563
9. Deribe, K. et al. (2015) The feasibility of eliminating podoconiosis. 34. Mahe, A. et al. (2005) Integration of basic dermatological care into
Bull. World Health Organ. 93, 712–718 primary health care services in Mali. Bull. World Health Organ. 83,
935–941
10. Davey, G. and Newport, M. (2007) Podoconiosis: the most
neglected tropical disease? Lancet 369, 888–889 35. Estrada, R. et al. (2012) Specialized dermatological care for mar-
ginalized populations and education at the primary care level: is
11. Hay, R.J. et al. (2014) The global burden of skin disease in 2010:
community dermatology a feasible proposal? Int. J. Dermatol. 51,
an analysis of the prevalence and impact of skin conditions. J.
1345–1350
Invest. Dermatol. 134, 1527–1534
36. Noormahomed, E.V. et al. (2016) Onchocerciasis, an undiagnosed
12. Clucas, D.B. et al. (2008) Disease burden and health-care clinic
disease in Mozambique: identifying research opportunities. Para-
attendances for young children in remote aboriginal communities
sit. Vectors 9, 180
of northern Australia. Bull. World Health Organ. 86, 275–281
37. Hotez, P.J. (2009) Mass drug administration and integrated con-
13. Figueroa, J.I. et al. (1998) Dermatology in southwestern Ethio-
trol for the world's high-prevalence neglected tropical diseases.
pia: rationale for a community approach. Int. J. Dermatol. 37,
Clin. Pharmacol. Ther. 85, 659–664
752–758
38. World Health Organization (2012) Eradication of yaws – the
14. Figueroa, J.I. et al. (1996) The prevalence of skin disease among
Morges strategy. Wkly. Epidemiol. Rec. 87, 189–194
school children in rural Ethiopia – a preliminary assessment of
dermatologic needs. Pediatr. Dermatol. 13, 378–381 39. Linehan, M. et al. (2011) Integrated implementation of programs
targeting neglected tropical diseases through preventive chemo-
15. Tasani, M. et al. (2016) The importance of scabies coinfection in
therapy: proving the feasibility at national scale. Am. J. Trop. Med.
the treatment considerations for impetigo. Pediatr. Infect. Dis. J.
Hyg. 84, 5–14
35, 374–378
40. Mengitsu, B. et al. (2016) Ethiopia and its steps to mobilize
16. Romani, L. et al. (2015) Prevalence of scabies and impetigo
resources to achieve 2020 elimination and control goals for
worldwide: a systematic review. Lancet Infect. Dis. 15, 960–967
neglected tropical diseases webs joined can tie a lion. Int. Health
17. Swe, P.M. et al. (2014) Parasitic scabies mites and associated 8 (Suppl 1), i34–i52
bacteria joining forces against host complement defence. Parasite
41. Hotez, P.J. et al. (2007) Control of neglected tropical diseases. N.
Immunol. 36, 585–593
Eng. J. Med. 357, 1018–1027
18. Engelman, D. et al. (2013) Toward the global control of human
42. Ottesen, E.A. et al. (2008) The global programme to eliminate
scabies: introducing the International Alliance for the Control of
lymphatic filariasis: health impact after 8 years. PLoS Negl. Trop.
Scabies. PLoS Negl. Trop. Dis. 7, e2167
Dis. 2, e317
19. Bonifaz, A. et al. (2004) Tinea imbricata or Tokelau. Int. J. Derma-
43. Molyneux, D.H. and Ward, S.A. (2015) Reflections on the Nobel
tol. 43, 506–510
Prize for Medicine 2015 – the public health legacy and impact of
20. Hay, R.J. et al. (2015) The global challenge for skin health. Br. J. avermectin and artemisinin. Trends Parasitol. 31, 605–607
Dermatol. 172, 1469–1472
44. Omura, S. and Crump, A. (2014) Ivermectin: panacea for
21. Solomon, A.W. et al. (2015) The Global Trachoma Mapping Proj- resource-poor communities? Trends Parasitol. 30, 445–455
ect: methodology of a 34-country population-based study. Oph-
45. Heukelbach, J. et al. (2004) Selective mass treatment with iver-
thalmic Epidemiol. 22, 214–225
mectin to control intestinal helminthiases and parasitic skin dis-
22. Marks, M. et al. (2015) Mapping the epidemiology of yaws in the eases in a severely affected population. Bull. World Health Organ.
Solomon Islands: a cluster randomized survey. Am. J. Trop. Med. 82, 563–571
Hyg. 92, 129–133
46. Krotneva, S.P. et al. (2015) African Program for Onchocerciasis
23. (2012) Transmission assessment surveys in the Global Pro- Control 1995-2010: impact of annual ivermectin mass treatment on
gramme to Eliminate Lymphatic Filariasis: WHO position state- off-target infectious diseases. PLoS Negl. Trop. Dis. 9, e0004051
ment. Wkly. Epidemiol. Rec. 87, 478–482
47. Mohammed, K.A. et al. (2012) Soil transmitted helminths and
24. Sime, H. et al. (2014) Integrated mapping of lymphatic filariasis scabies in Zanzibar, Tanzania following mass drug administration
and podoconiosis: lessons learnt from Ethiopia. Parasit. Vectors for lymphatic filariasis – a rapid assessment methodology to
7, 397 assess impact. Parasit. Vectors 5, 299
25. World Health Organization (2013) Sustaining the Drive To Over- 48. Ndyomugyenyi, R. et al. (2009) Perceptions on onchocerciasis
come the GLOBAL Impact of Neglected Tropical Diseases: Sec- and ivermectin treatment in rural communities in Uganda: impli-
ond WHO Report on Neglected Tropical Diseases, World Health cations for long-term compliance. Int. Health 1, 163–168
Organization
49. Thomsen, E.K. et al. (2016) Efficacy, safety, and pharmacokinetics
26. Cooley, G.M. et al. (2016) Evaluation of multiplex-based antibody of coadministered diethylcarbamazine, albendazole, and ivermectin
testing for use in large-scale surveillance for yaws: a comparative for treatment of bancroftian filariasis. Clin. Infect. Dis. 62, 334–341
study. J. Clin. Microbiol. 54, 1321–1325
50. Kastner, R.J. et al. (2015) What is needed to eradicate lymphatic
27. Priest, J.W. et al. (2016) Integration of multiplex bead assays for filariasis?. A model-based assessment on the impact of scaling up
parasitic diseases into a national, population-based serosurvey of mass drug administration programs. PLoS Negl. Trop. Dis. 9,
women 15-39 years of age in Cambodia. PLoS Negl. Trop. Dis. e0004147
10, e0004699
51. Hotez, P.J. et al. (2011) Integrating neglected tropical diseases
28. Notomi, T. et al. (2000) Loop-mediated isothermal amplification of into AIDS, tuberculosis, and malaria control. N. Eng. J. Med. 364,
DNA. Nucleic Acids Res. 28, E63 2086–2089
Trends in Parasitology, November 2016, Vol. 32, No. 11 853
52. WHO Malaria Policy Advisory Committee Secretariat (2016) 69. Leslie, J. et al. (2013) Neglected tropical diseases: comparison of
Malaria Policy Advisory Committee to the WHO: conclusions the costs of integrated and vertical preventive chemotherapy
and recommendations of eighth biannual meeting (September treatment in Niger. Int. Health 5, 78–84
2015). Malar. J. 15, 117 70. Evans, D. et al. (2011) Cost-effectiveness of triple drug adminis-
53. Solomon, A.W. et al. (2015) Trachoma and yaws: common tration (TDA) with praziquantel, ivermectin and albendazole for the
ground? PLoS Negl. Trop. Dis. 9, e0004071 prevention of neglected tropical diseases in Nigeria. Ann. Trop.
54. Marks, M. et al. (2015) Impact of community mass treatment with Med. Parasitol. 105, 537–547
azithromycin for trachoma elimination on the prevalence of yaws. 71. Brady, M.A. et al. (2006) Projected benefits from integrating NTD
PLoS Negl. Trop. Dis. 9, e0003988 programs in sub-Saharan Africa. Trends Parasitol. 22, 285–291
55. Coulibaly, Y.I. et al. (2013) A cluster randomized study of the safety 72. Lammie, P.J. et al. (2006) A blueprint for success: integration of
of integrated treatment of trachoma and lymphatic filariasis in chil- neglected tropical disease control programmes. Trends Parasitol.
dren and adults in Sikasso, Mali. PLoS Negl. Trop. Dis. 7, e2221 22, 313–321
56. Mohammed, K.A. et al. (2008) Triple co-administration of ivermec- 73. Smith, J. and Taylor, E.M. (2016) What is next for NTDs in the era of
tin, albendazole and praziquantel in Zanzibar: a safety study. PLoS the sustainable development goals? PLoS Negl. Trop. Dis. 10,
Negl. Trop. Dis. 2, e171 e0004719
57. Currie, B.J. et al. (2004) First documentation of in vivo and in vitro 74. Holmes, P. (2014) Neglected tropical diseases in the post-2015
ivermectin resistance in Sarcoptes scabiei. Clin. Infect. Dis. 39, e8– health agenda. Lancet 383, 1803
e12 75. World Health Organization (2015) Investing to Overcome the
58. Coles, C.L. et al. (2013) Mass distribution of azithromycin for Global Impact of Neglected Tropical Diseases: Third WHO Report
trachoma control is associated with increased risk of azithromy- on Neglected Tropical Diseases, World Health Organization
cin-resistant Streptococcus pneumoniae carriage in young chil- 76. Hay, R.J. et al. (2012) Scabies in the developing world – its
dren 6 months after treatment. Clin. Infect. Dis. 56, 1519–1526 prevalence, complications, and management. Clin. Microbiol.
59. Ho, D.K. et al. (2015) Antibiotic resistance in Streptococcus pneu- Infect. 18, 313–323
moniae after azithromycin distribution for trachoma. J. Trop. Med. 77. La Vincente, S. et al. (2009) Community management of endemic
2015, 917370 scabies in remote aboriginal communities of northern Australia:
60. Gagliotti, C. et al. (2006) Macrolide prescriptions and erythromycin low treatment uptake and high ongoing acquisition. PLoS Negl.
resistance of Streptococcus pyogenes. Clin. Infect. Dis. 42, 1153– Trop. Dis. 3, e444
1156 78. Romani, L. et al. (2015) Mass drug administration for scabies
61. Batt, S.L. et al. (2003) Impact of azithromycin administration for control in a population with endemic disease. N. Eng. J. Med.
trachoma control on the carriage of antibiotic-resistant Streptococ- 373, 2305–2313
cus pneumoniae. Antimicrob. Agents Chemother. 47, 2765–2769 79. Lawrence, G. et al. (2005) Control of scabies, skin sores and
62. Sikorski, C. et al. (2010) Effectiveness of a simple lymphoedema haematuria in children in the Solomon Islands: another role for
treatment regimen in podoconiosis management in southern ivermectin. Bull. World Health Organ. 83, 34–42
Ethiopia: one year follow-up. PLoS Negl. Trop. Dis. 4, e902 80. Kearns, T.M. et al. (2015) Impact of an ivermectin mass drug
63. Negussie, H. et al. (2015) Podoconiosis treatment in northern administration on scabies prevalence in a remote australian
Ethiopia (GoLBet): study protocol for a randomised controlled aboriginal community. PLoS Negl. Trop. Dis. 9, e0004151
trial. Trials 16, 307 81. Mason, D.S. et al. (2016) The prevalence of scabies and impetigo
64. Jullien, P. et al. (2011) Efficacy of home-based lymphoedema in the Solomon Islands: a population-based survey. PLoS Negl.
management in reducing acute attacks in subjects with lymphatic Trop. Dis. 10, e0004803
filariasis in Burkina Faso. Acta Trop. 120 (Suppl. 1), S55–S61 82. Mounsey, K.E. et al. (2016) Prospects for moxidectin as a new oral
65. van ‘t Noordende, A.T. et al. (2016) Towards a toolkit for cross- treatment for human scabies. PLoS Negl. Trop. Dis. 10, e0004389
neglected tropical disease morbidity and disability assessment. 83. Al-Awadi, A.R. et al. (2014) Guinea worm (Dracunculiasis) eradi-
Int. Health 8, i71–i81 cation: update on progress and endgame challenges. Trans. R.
66. Boisson, S. et al. (2016) Water, sanitation and hygiene for accel- Soc. Trop. Med. Hyg. 108, 249–251
erating and sustaining progress on neglected tropical diseases: a 84. Hotez, P.J. et al. (2014) The global burden of disease study 2010:
new global strategy 2015-20. Int. Health 8, i19–i21 interpretation and implications for the neglected tropical diseases.
67. Freeman, M.C. et al. (2013) Integration of water, sanitation, and PLoS Negl. Trop. Dis. 8, e2865
hygiene for the prevention and control of neglected tropical dis- 85. Molyneux, D.H. (2012) Tropical lymphedemas – control and pre-
eases: a rationale for inter-sectoral collaboration. PLoS Negl. Trop. vention. N. Engl. J. Med. 366, 1169–1171
Dis. 7, e2439
86. Bethony, J. et al. (2006) Soil-transmitted helminth infections:
68. Johnston, E.A. et al. (2015) Challenges and opportunities associated ascariasis, trichuriasis, and hookworm. Lancet 367, 1521–1532
with neglected tropical disease and water, sanitation and hygiene
intersectoral integration programs. BMC Public Health 15, 547
854 Trends in Parasitology, November 2016, Vol. 32, No. 11
Вам также может понравиться
- James W. Hardin, Joseph M. Hilbe - Generalized Linear Models and Extensions-Stata Press (2018)Документ789 страницJames W. Hardin, Joseph M. Hilbe - Generalized Linear Models and Extensions-Stata Press (2018)owusuessel100% (1)
- Academic Unit of General Practice: 2019 Newsletter - Semester 2, Christmas EditionДокумент8 страницAcademic Unit of General Practice: 2019 Newsletter - Semester 2, Christmas EditionowusuesselОценок пока нет
- Gender Inequality IndexДокумент16 страницGender Inequality IndexowusuesselОценок пока нет
- E94296 PDFДокумент54 страницыE94296 PDFowusuesselОценок пока нет
- Spatial Analysis of Skilled Birth Attendant Utilization in GhanaДокумент12 страницSpatial Analysis of Skilled Birth Attendant Utilization in GhanaowusuesselОценок пока нет
- CMSA General Guidelines Booklet - 4 May 2017 20-7-2018Документ92 страницыCMSA General Guidelines Booklet - 4 May 2017 20-7-2018owusuessel100% (1)
- Health Policy: Kristin Farrants, Clare Bambra, Lotta Nylen, Adetayo Kasim, Bo Burström, David HunterДокумент8 страницHealth Policy: Kristin Farrants, Clare Bambra, Lotta Nylen, Adetayo Kasim, Bo Burström, David HunterowusuesselОценок пока нет
- Diagnosis of Urethral Diverticulum Mimicking Pelvic Organ Prolapse With Translabial UltrasonographyДокумент1 страницаDiagnosis of Urethral Diverticulum Mimicking Pelvic Organ Prolapse With Translabial UltrasonographyowusuesselОценок пока нет
- Primary Papillary Serous Carcinoma of The Fallopian Tube Presenting As A Vaginal Mass: A Case Report and Review of The LiteratureДокумент6 страницPrimary Papillary Serous Carcinoma of The Fallopian Tube Presenting As A Vaginal Mass: A Case Report and Review of The LiteratureowusuesselОценок пока нет
- Environment International: SciencedirectДокумент8 страницEnvironment International: SciencedirectowusuesselОценок пока нет
- Cesarean Scar Pregnancy Associated With An Impending Uterine Rupture Diagnosed With 3-Dimensional UltrasonographyДокумент2 страницыCesarean Scar Pregnancy Associated With An Impending Uterine Rupture Diagnosed With 3-Dimensional UltrasonographyowusuesselОценок пока нет
- Health Policy: Sarah-Jo Sinnott, Helen Whelton, Jessica Myers Franklin, Jennifer Milan PolinskiДокумент8 страницHealth Policy: Sarah-Jo Sinnott, Helen Whelton, Jessica Myers Franklin, Jennifer Milan PolinskiowusuesselОценок пока нет
- 1 s2.0 S0002937816308225 MainДокумент1 страница1 s2.0 S0002937816308225 MainowusuesselОценок пока нет
- Critical Appraisal of The Paper TitledДокумент3 страницыCritical Appraisal of The Paper TitledowusuesselОценок пока нет
- Payment MethodsДокумент4 страницыPayment MethodsowusuesselОценок пока нет
- Wacs Accreditation StatusДокумент4 страницыWacs Accreditation StatusowusuesselОценок пока нет
- Wacp Primary Curriculum For Psychiatry PDFДокумент5 страницWacp Primary Curriculum For Psychiatry PDFowusuesselОценок пока нет
- Cervical Cancer: Presented at Bole Methodist Church, NRДокумент39 страницCervical Cancer: Presented at Bole Methodist Church, NRowusuesselОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Giovan Cosimo Bonomo (1663-1696) - Discoverer of The Etiology of ScabiesДокумент8 страницGiovan Cosimo Bonomo (1663-1696) - Discoverer of The Etiology of ScabiesPratik PatelОценок пока нет
- Insights From Veterinary MedicineДокумент290 страницInsights From Veterinary Medicinenorma paulina carcausto lipaОценок пока нет
- 2020 PBR CORRECTIONS AND CLARIFICATIONS GUIDE - 2021 ImagesДокумент80 страниц2020 PBR CORRECTIONS AND CLARIFICATIONS GUIDE - 2021 ImagespbradminОценок пока нет
- Grade 7 SchemesДокумент7 страницGrade 7 SchemesMalesi SiemaОценок пока нет
- Scabies Questions and AnswersДокумент15 страницScabies Questions and AnswersCandra Adie Wicahyono100% (1)
- ScabiesДокумент6 страницScabiesJayson ShieldsОценок пока нет
- Original Research Article - Controlling Scabies in Madrasahs (Islamic Religious Schools) in BangladeshДокумент9 страницOriginal Research Article - Controlling Scabies in Madrasahs (Islamic Religious Schools) in BangladeshMuhammad IkbarОценок пока нет
- Common Child and AdolescentДокумент23 страницыCommon Child and AdolescentValeria BeltranОценок пока нет
- My Cat Scratched Me and A Weird Welt Formed Around It - MildlyinterestingДокумент12 страницMy Cat Scratched Me and A Weird Welt Formed Around It - MildlyinterestingGoo GleОценок пока нет
- Np1 July2021 ActualДокумент15 страницNp1 July2021 ActualAnnizaОценок пока нет
- Nclex BulletsДокумент34 страницыNclex Bulletssaroberts2202100% (1)
- Permethrin Topical Cream RLD 019855 RC08-17Документ7 страницPermethrin Topical Cream RLD 019855 RC08-17Ritesh RastogiОценок пока нет
- Akwanwa Botanics Full Skincare EbookДокумент150 страницAkwanwa Botanics Full Skincare EbookChinaemerem83% (6)
- CASE 4 PharmaДокумент2 страницыCASE 4 PharmaJoana Mikee RasayОценок пока нет
- Nursing Management of Skin and Parasitic DiseasesДокумент14 страницNursing Management of Skin and Parasitic Diseasesyer tagalajОценок пока нет
- Rash Potpourri Didacticwith AnimationДокумент75 страницRash Potpourri Didacticwith AnimationFlavius AnghelОценок пока нет
- Jurnal Scabies 7Документ9 страницJurnal Scabies 7Eric FullerОценок пока нет
- Skin ConditionsДокумент43 страницыSkin ConditionspdladvaОценок пока нет
- Scabies.: Vanessa ChelimoДокумент19 страницScabies.: Vanessa ChelimoAlvin OmondiОценок пока нет
- Integumentary Disorders (New)Документ41 страницаIntegumentary Disorders (New)coosa liquorsОценок пока нет
- Daily Lesson Plan - NSTP1Документ3 страницыDaily Lesson Plan - NSTP1Charity Mae DoradoОценок пока нет
- Original Papers: The Efficacy of Oral Ivermectin vs. Sulfur 10% Ointment For The Treatment of ScabiesДокумент8 страницOriginal Papers: The Efficacy of Oral Ivermectin vs. Sulfur 10% Ointment For The Treatment of ScabieserwinОценок пока нет
- Medical EntomologyДокумент39 страницMedical EntomologyRIZIQ TSОценок пока нет
- Analisis Perilaku Pencegahan Skabies Pada Santri Pondok Pesantren Nurul Huda Pringsewu LampungДокумент8 страницAnalisis Perilaku Pencegahan Skabies Pada Santri Pondok Pesantren Nurul Huda Pringsewu LampungSilviaОценок пока нет
- Tea Tree Oil Benefits, Uses and Potential Side Effects - Dr. AxeДокумент8 страницTea Tree Oil Benefits, Uses and Potential Side Effects - Dr. AxeJoseph TupasОценок пока нет
- What Is ScabiesДокумент7 страницWhat Is ScabiesKenОценок пока нет
- Jurnal Skabies EBM 2Документ18 страницJurnal Skabies EBM 2Bianti Nur'ainiОценок пока нет
- Medicines in BreastfeedingДокумент4 страницыMedicines in BreastfeedingIshan ShahОценок пока нет
- Absence of Responsible Member and Financial ConstraintsДокумент2 страницыAbsence of Responsible Member and Financial ConstraintsFavor ColaОценок пока нет