Академический Документы
Профессиональный Документы
Культура Документы
POLSTForm 2017rv2
Загружено:
agelesswapИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
POLSTForm 2017rv2
Загружено:
agelesswapАвторское право:
Доступные форматы
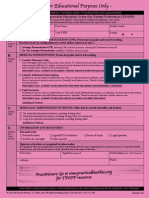
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTH CARE PROVIDERS AS NECESSARY
Physician Orders for Life-Sustaining Treatment (POLST)
First follow these orders, then contact Patient Last Name: Date Form Prepared:
Physician/NP/PA. A copy of the signed POLST
form is a legally valid physician order. Any section Patient First Name: Patient Date of Birth:
not completed implies full treatment for that section.
EMSA #111 B POLST complements an Advance Directive and Patient Middle Name: Medical Record #: (optional)
(Effective 4/1/2017)* is not intended to replace that document.
A CARDIOPULMONARY RESUSCITATION (CPR): If patient has no pulse and is not
breathing.
Chec
k
If patient is NOT in cardiopulmonary arrest, follow orders in Sections B and C.
One Attempt Resuscitation/CPR (Selecting CPR in Section A requires selecting Full Treatment in Section B)
Do Not Attempt Resuscitation/DNR (Allow Natural Death)
B MEDICAL INTERVENTIONS:
If patient is found with a pulse and/or is breathing.
Full Treatment – primary goal of prolonging life by all medically effective means.
Chec
k In addition to treatment described in Selective Treatment and Comfort-Focused Treatment, use intubation,
One advanced airway interventions, mechanical ventilation, and cardioversion as indicated.
Trial Period of Full Treatment.
Selective Treatment – goal of treating medical conditions while avoiding burdensome measures. In
addition to treatment described in Comfort-Focused Treatment, use medical treatment, IV antibiotics, and IV
fluids as indicated. Do not intubate. May use non-invasive positive airway pressure. Generally avoid intensive
care.
Request transfer to hospital only if comfort needs cannot be met in current location.
Comfort-Focused Treatment – primary goal of maximizing comfort.
Relieve pain and suffering with medication by any route as needed; use oxygen, suctioning, and manual treatment
of airway obstruction. Do not use treatments listed in Full and Selective Treatment unless consistent with comfort
goal. Request transfer to hospital only if comfort needs cannot be met in current location.
Additional Orders: ___________________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________________________________________
ARTIFICIALLY ADMINISTERED NUTRITION: Offer food by mouth if feasible and desired.
C Long-term artificial nutrition, including feeding tubes. Additional Orders: ________________________
Chec
k Trial period of artificial nutrition, including feeding tubes. __________________________________________
One
No artificial means of nutrition, including feeding tubes. __________________________________________
INFORMATION AND SIGNATURES:
D Discussed with: Patient (Patient Has Capacity) Legally Recognized Decisionmaker
Advance Directive dated _______, available and reviewed Health Care Agent if named in Advance Directive:
Advance Directive not available Name: ________________________________________
No Advance Directive Phone: _______________________________________
Signature of Physician / Nurse Practitioner / Physician Assistant (Physician/NP/PA)
My signature below indicates to the best of my knowledge that these orders are consistent with the patient’s medical condition and preferences.
Print Physician/NP/PA Name: Physician/NP/PA Phone #: Physician/PA License #, NP Cert. #:
Physician/NP/PA Signature: (required) Date:
Signature of Patient or Legally Recognized Decisionmaker
I am aware that this form is voluntary. By signing this form , the legally recognized decisionmaker acknowledges that this request regarding
resuscitative measures is consistent with the known desires of , and with the best interest of, the individual who is the subject of the form.
Print Name: Relationship: (write self if patient)
Signature: (required) Date: Your POLST may be added to a
secure electronic registry to be
Mailing Address (street/city/state/zip): Phone Number: accessible by health providers, as
permitted by HIPAA.
SEND FORM WITH PATIENT WHENEVER TRANSFERRED OR DISCHARGED
*
Form versions with effective dates of 1/1/2009, 4/1/2011,10/1/2014 or 01/01/2016 are also valid
HIPAA PERMITS DISCLOSURE OF POLST TO OTHER HEALTH CARE PROVIDERS AS NECESSARY
Patient Information
Name (last, first, middle): Date of Birth: Gender:
F
M
NP/PA’s Supervising Physician Preparer Name (if other than signing Physician/NP/PA)
Name: Name/Title: Phone #:
Additional Contact None
Name: Relationship to Patient: Phone #:
Directions for Health Care Provider
Completing POLST
• Completing a POLST form is voluntary. California law requires that a POLST form be followed by healthcare providers,
and provides immunity to those who comply in good faith. In the hospital setting, a patient will be assessed by a physician,
or a nurse practitioner (NP) or a physician assistant (PA) acting under the supervision of the physician, who will issue
appropriate orders that are consistent with the patient’s preferences.
• POLST does not replace the Advance Directive. When available, review the Advance Directive and POLST form to
ensure consistency, and update forms appropriately to resolve any conflicts.
• POLST must be completed by a health care provider based on patient preferences and medical indications.
• A legally recognized decisionmaker may include a court-appointed conservator or guardian, agent designated in an Advance
Directive, orally designated surrogate, spouse, registered domestic partner, parent of a minor, closest available relative, or
person whom the patient’s physician/NP/PA believes best knows what is in the patient’s best interest and will make decisions
in accordance with the patient’s expressed wishes and values to the extent known.
• A legally recognized decisionmaker may execute the POLST form only if the patient lacks capacity or has designated that the
decisionmaker’s authority is effective immediately.
• To be valid a POLST form must be signed by (1) a physician, or by a nurse practitioner or a physician assistant acting under
the supervision of a physician and within the scope of practice authorized by law and (2) the patient or decisionmaker. Verbal
orders are acceptable with follow-up signature by physician/NP/PA in accordance with facility/community policy.
• If a translated form is used with patient or decisionmaker, attach it to the signed English POLST form.
• Use of original form is strongly encouraged. Photocopies and FAXes of signed POLST forms are legal and valid. A copy
should be retained in patient’s medical record, on Ultra Pink paper when possible.
Using POLST
• Any incomplete section of POLST implies full treatment for that section.
Section A:
• If found pulseless and not breathing, no defibrillator (including automated external defibrillators) or chest
compressions should be used on a patient who has chosen “Do Not Attempt Resuscitation.”
Section B:
• When comfort cannot be achieved in the current setting, the patient, including someone with “Comfort-Focused Treatment,”
should be transferred to a setting able to provide comfort (e.g., treatment of a hip fracture).
• Non-invasive positive airway pressure includes continuous positive airway pressure (CPAP), bi-level positive airway
pressure (BiPAP), and bag valve mask (BVM) assisted respirations.
• IV antibiotics and hydration generally are not “Comfort-Focused Treatment.”
• Treatment of dehydration prolongs life. If a patient desires IV fluids, indicate “Selective Treatment” or “Full Treatment.”
• Depending on local EMS protocol, “Additional Orders” written in Section B may not be implemented by EMS personnel.
Reviewing POLST
It is recommended that POLST be reviewed periodically. Review is recommended when:
• The patient is transferred from one care setting or care level to another, or
• There is a substantial change in the patient’s health status, or
• The patient’s treatment preferences change.
Modifying and Voiding POLST
• A patient with capacity can, at any time, request alternative treatment or revoke a POLST by any means that indicates intent
to revoke. It is recommended that revocation be documented by drawing a line through Sections A through D, writing “VOID”
in large letters, and signing and dating this line.
• A legally recognized decisionmaker may request to modify the orders, in collaboration with the physician/NP/PA, based on
the known desires of the patient or, if unknown, the patient’s best interests.
This form is approved by the California Emergency Medical Services Authority in cooperation with the statewide POLST Task Force.
For more information or a copy of the form, visit www.caPOLST.org.
SEND FORM WITH PATIENT WHENEVER TRANSFERRED OR DISCHARGED
Вам также может понравиться
- Genesys NoSkills Fillable Character Sheet PDFДокумент3 страницыGenesys NoSkills Fillable Character Sheet PDFMasterWallwalkerОценок пока нет
- Policy On Generic Prescribing and RecordingДокумент2 страницыPolicy On Generic Prescribing and RecordingHugh Perry Tejamo50% (2)
- Manual Procedures AMS in Hospital 2016 PDFДокумент83 страницыManual Procedures AMS in Hospital 2016 PDFagelesswapОценок пока нет
- Project Report On e BikesДокумент57 страницProject Report On e Bikesrh21940% (5)
- Advanced Directive & Durable Power of Attorney For Health CareДокумент6 страницAdvanced Directive & Durable Power of Attorney For Health CareTexieraОценок пока нет
- Bom Sample NP AgreementДокумент7 страницBom Sample NP Agreementsfox8792Оценок пока нет
- Hospital Disaster Risk Reduction GuidelinesДокумент43 страницыHospital Disaster Risk Reduction GuidelinesEdjey Luis F. MatinongОценок пока нет
- MOA Red CrossДокумент4 страницыMOA Red Crossagelesswap100% (2)
- Family Law Outline RevisedДокумент11 страницFamily Law Outline RevisedAdriana CarinanОценок пока нет
- Rebrand and Relaunch Hydrox CookiesДокумент9 страницRebrand and Relaunch Hydrox CookiesAruba KhanОценок пока нет
- POLSTForm 2017rv2Документ2 страницыPOLSTForm 2017rv2Emyrose IceОценок пока нет
- 2020.05.11 National POLST Form With Instructions r2Документ3 страницы2020.05.11 National POLST Form With Instructions r2A PremierОценок пока нет
- Approved POLSTFormДокумент2 страницыApproved POLSTFormShawna BrechbillОценок пока нет
- Hawaii Polst FormДокумент2 страницыHawaii Polst FormJames OkamotoОценок пока нет
- Nys Molst FormДокумент4 страницыNys Molst FormDaniel_Taylor_4541Оценок пока нет
- Missouri Transportable Physician Orders For Patient Preferences Tpopp FormДокумент2 страницыMissouri Transportable Physician Orders For Patient Preferences Tpopp FormitargetingОценок пока нет
- Montana Do Not Resuscitate FormДокумент2 страницыMontana Do Not Resuscitate FormitargetingОценок пока нет
- 3.02.19 Verbal Orders and Critical Values2Документ2 страницы3.02.19 Verbal Orders and Critical Values2Robert TucayОценок пока нет
- Inform ConsentДокумент9 страницInform ConsentMeta Bachtiar100% (1)
- HMRM RECORD DoccДокумент13 страницHMRM RECORD DoccBharath BeeОценок пока нет
- DOH-4359 (2010) Physician'S Order For Personal Care/Consumer Directed Personal Assistance ServicesДокумент4 страницыDOH-4359 (2010) Physician'S Order For Personal Care/Consumer Directed Personal Assistance ServicesRebeca MartínezОценок пока нет
- Attending Physicians Statement Crisis Cover Major Organ Transplant - 041222Документ2 страницыAttending Physicians Statement Crisis Cover Major Organ Transplant - 041222max leeОценок пока нет
- 01-RCD General Consent Form For TreatmentДокумент2 страницы01-RCD General Consent Form For TreatmentSaad HussainОценок пока нет
- Template Registration Form and Consent Form V3 - Final For RPSДокумент7 страницTemplate Registration Form and Consent Form V3 - Final For RPSHamdi PutraОценок пока нет
- Appendix 4a - Patient Registration Form GuidanceДокумент4 страницыAppendix 4a - Patient Registration Form GuidanceYuwono AriyantoОценок пока нет
- QR-RCP-009 Authorization For Disclosure of Health InformationRecords - Rev07Документ1 страницаQR-RCP-009 Authorization For Disclosure of Health InformationRecords - Rev07Yel BОценок пока нет
- General Consent Form English 29-IV-09Документ3 страницыGeneral Consent Form English 29-IV-09rubenguzОценок пока нет
- Authorized Durable DNR FormДокумент5 страницAuthorized Durable DNR FormBenjamin RayОценок пока нет
- Patient Admission Hospital Admission ChecklistДокумент6 страницPatient Admission Hospital Admission ChecklistSweetly MamukoОценок пока нет
- GW Hospital MOU & Observer Health Information FormДокумент2 страницыGW Hospital MOU & Observer Health Information Formengel0321hotmail.comОценок пока нет
- ReimbursementДокумент2 страницыReimbursementFAZILОценок пока нет
- General Consent For Treatment Form Oct 2016Документ2 страницыGeneral Consent For Treatment Form Oct 2016Dewi Ratna SariОценок пока нет
- DNR - Do Not Resuscitate Law - 2017Документ8 страницDNR - Do Not Resuscitate Law - 2017Keelie SmithОценок пока нет
- REV - Inpatient Claim Form - AIAДокумент2 страницыREV - Inpatient Claim Form - AIAYen SylvaniОценок пока нет
- All FormsДокумент13 страницAll FormsSam EmekaОценок пока нет
- Informed Consent: Prof. Moch. Istiadjid E.S. Dr. Dr. Sps. Spbs. MhumДокумент68 страницInformed Consent: Prof. Moch. Istiadjid E.S. Dr. Dr. Sps. Spbs. MhumJames BudiantoОценок пока нет
- 03.03 Documentation and Confidentiality WorksheetДокумент3 страницы03.03 Documentation and Confidentiality Worksheetanshi christinaОценок пока нет
- PTCE Review NotesДокумент11 страницPTCE Review NotesSantos Wheeler100% (1)
- Patient Physician AgreementДокумент3 страницыPatient Physician Agreementmike johnОценок пока нет
- Attending Physicians Statement Crisis Cover Muscular Dystrophy - 041222Документ2 страницыAttending Physicians Statement Crisis Cover Muscular Dystrophy - 041222laraОценок пока нет
- POST and Advance Directives Study GuideДокумент8 страницPOST and Advance Directives Study GuideAubrey ManimtimОценок пока нет
- Informed Consent For Medical-Surfgical Procedure and Acknowledgment of Receipt of InformationДокумент2 страницыInformed Consent For Medical-Surfgical Procedure and Acknowledgment of Receipt of InformationSaad HussainОценок пока нет
- Claim Form (Out Patient + Hospitalisation)Документ2 страницыClaim Form (Out Patient + Hospitalisation)ahsan_hayat28660% (1)
- Hospital Treatment Form: Anumediclaim PoliciesДокумент1 страницаHospital Treatment Form: Anumediclaim PoliciesSubhadip MaityОценок пока нет
- 3-Do Not Resuscitate OrdersДокумент9 страниц3-Do Not Resuscitate Ordersmoon_teenОценок пока нет
- Nhs England Ifr FormДокумент10 страницNhs England Ifr FormdanielОценок пока нет
- Attending Physicians Statement Crisis Cover Renal Failure - 041222Документ2 страницыAttending Physicians Statement Crisis Cover Renal Failure - 041222max leeОценок пока нет
- EPass ApplicationДокумент2 страницыEPass ApplicationHardip BhatiaОценок пока нет
- Pcs Manual 2014 Revised4Документ311 страницPcs Manual 2014 Revised4safety jprizalОценок пока нет
- 4a - Patient Registration FormДокумент7 страниц4a - Patient Registration FormHygiena Kumala SuciОценок пока нет
- DNRДокумент3 страницыDNRAak CeyeОценок пока нет
- Department of State Academic Exchanges Participant Medical History and Examination FormДокумент8 страницDepartment of State Academic Exchanges Participant Medical History and Examination FormNurman HidayatОценок пока нет
- SB Toledo: (A) Policy StatementДокумент2 страницыSB Toledo: (A) Policy StatementSofie DyahОценок пока нет
- Complete Care Plan Form 508Документ5 страницComplete Care Plan Form 508RSUD SangkulirangОценок пока нет
- Medical CertificateДокумент2 страницыMedical CertificateBhem Fernandez RomeroОценок пока нет
- SLMC-English-TELEHEALTH CONSENT FORMДокумент3 страницыSLMC-English-TELEHEALTH CONSENT FORMyio16711Оценок пока нет
- Advance Directive For Medical / Surgical Treatment (Living Will) - ColoradoДокумент6 страницAdvance Directive For Medical / Surgical Treatment (Living Will) - ColoradocleincoloradoОценок пока нет
- Medical Terminology Term PaperДокумент14 страницMedical Terminology Term Paper27mickie0% (1)
- DNR OrderДокумент3 страницыDNR OrderStephanie Joy EscalaОценок пока нет
- l8 - End of Life Issues (Part 1)Документ57 страницl8 - End of Life Issues (Part 1)Zoya MoraniОценок пока нет
- Hcs120r2 Week 3 Terms WorksheetДокумент3 страницыHcs120r2 Week 3 Terms WorksheetCarsha RidleyОценок пока нет
- Others Claim FormДокумент5 страницOthers Claim FormArvind RayОценок пока нет
- Write A Consultation ReportДокумент9 страницWrite A Consultation ReportHari25885Оценок пока нет
- Legal Issues Emergency Medicine (Final)Документ97 страницLegal Issues Emergency Medicine (Final)GerardChanОценок пока нет
- Medical Records: Making and Retaining Them: What Is A Medical Record?Документ6 страницMedical Records: Making and Retaining Them: What Is A Medical Record?mfadly maulanaОценок пока нет
- SLMC Consent For Treatment and Procedure During Covid19 PandemicДокумент2 страницыSLMC Consent For Treatment and Procedure During Covid19 PandemicCatie Tan ChingОценок пока нет
- (Nursing English) DIYAH AHADYATUNNISAДокумент10 страниц(Nursing English) DIYAH AHADYATUNNISAdiyah hansuОценок пока нет
- 6 Chapter Six Templates Forms and Checklists V2Документ85 страниц6 Chapter Six Templates Forms and Checklists V2agelesswap100% (3)
- Antimicrobial Rational UseДокумент19 страницAntimicrobial Rational UseagelesswapОценок пока нет
- Policy On Generic Prescribing and RecordingДокумент19 страницPolicy On Generic Prescribing and RecordingagelesswapОценок пока нет
- Magna Carta of Women in The PhilippinesДокумент21 страницаMagna Carta of Women in The PhilippinesYrra LimchocОценок пока нет
- Evaluation Tool Certificate of Need For New General HospitalsДокумент5 страницEvaluation Tool Certificate of Need For New General HospitalsagelesswapОценок пока нет
- Administrative Order 2010 0028 HIV Counselling Testing PDFДокумент14 страницAdministrative Order 2010 0028 HIV Counselling Testing PDFagelesswapОценок пока нет
- Emergency Department Operational SOP v1.1 Mar2017Документ15 страницEmergency Department Operational SOP v1.1 Mar2017agelesswapОценок пока нет
- Newborn Screening Policy and Guidelines - August 2011 PDFДокумент15 страницNewborn Screening Policy and Guidelines - August 2011 PDFagelesswapОценок пока нет
- DNR FormДокумент13 страницDNR FormagelesswapОценок пока нет
- DNRFormДокумент4 страницыDNRFormAri KimОценок пока нет
- Resource Guide - Model Nbs PolicyДокумент7 страницResource Guide - Model Nbs PolicyagelesswapОценок пока нет
- Administrative Order 2010 0028 HIV Counselling TestingДокумент31 страницаAdministrative Order 2010 0028 HIV Counselling TestingagelesswapОценок пока нет
- Christmas Health PromoДокумент1 страницаChristmas Health PromoagelesswapОценок пока нет
- New Text DocumentДокумент4 страницыNew Text DocumentagelesswapОценок пока нет
- The Philippine NUrsing Act of 2002 Aka R.A. 9173Документ7 страницThe Philippine NUrsing Act of 2002 Aka R.A. 9173Rho Vince Caño MalagueñoОценок пока нет
- Adult Emergency Care ProtocolsДокумент2 страницыAdult Emergency Care ProtocolsagelesswapОценок пока нет
- Menu Standard PDFДокумент26 страницMenu Standard PDFagelesswapОценок пока нет
- Yify AlternativesДокумент1 страницаYify AlternativesagelesswapОценок пока нет
- Adult Emergency Care ProtocolsДокумент2 страницыAdult Emergency Care ProtocolsagelesswapОценок пока нет
- Trends and IssuesДокумент4 страницыTrends and IssuesagelesswapОценок пока нет
- FoundationДокумент1 страницаFoundationagelesswapОценок пока нет
- Adult Emergency Care ProtocolsДокумент2 страницыAdult Emergency Care ProtocolsagelesswapОценок пока нет
- CMDДокумент4 страницыCMDagelesswapОценок пока нет
- Chapter 3Документ9 страницChapter 3agelesswap100% (1)
- Staffing: Presentation TranscriptДокумент4 страницыStaffing: Presentation TranscriptagelesswapОценок пока нет
- Social Media As An Effective Tool To Promote BusinessДокумент5 страницSocial Media As An Effective Tool To Promote BusinessHannah Gwyneth BalaОценок пока нет
- Lesson 2 - Pure Substances and MixturesДокумент41 страницаLesson 2 - Pure Substances and Mixturescecil tayagОценок пока нет
- Hampers 2023 - Updted Back Cover - FAДокумент20 страницHampers 2023 - Updted Back Cover - FAHaris HaryadiОценок пока нет
- Rhinitis Allergic: Elma Wiliandini G4A020043Документ10 страницRhinitis Allergic: Elma Wiliandini G4A020043elma wiliandiniОценок пока нет
- Prepositioncombinations PDFДокумент14 страницPrepositioncombinations PDFMichalisBenedictusОценок пока нет
- Assessment of The Role of Radio in The Promotion of Community Health in Ogui Urban Area, EnuguДокумент21 страницаAssessment of The Role of Radio in The Promotion of Community Health in Ogui Urban Area, EnuguPst W C PetersОценок пока нет
- Success Criteria For Change InitiativesДокумент6 страницSuccess Criteria For Change Initiativesgimmeanearful100% (1)
- Nosocomial InfectionДокумент31 страницаNosocomial InfectionDr. Ashish Jawarkar0% (1)
- LMC - Boundary Dispute CasesДокумент12 страницLMC - Boundary Dispute CasesLR FОценок пока нет
- M.Vikram: Department of Electronics and Communication EngineeringДокумент26 страницM.Vikram: Department of Electronics and Communication EngineeringSyed AmaanОценок пока нет
- Nano Technology Oil RefiningДокумент19 страницNano Technology Oil RefiningNikunj Agrawal100% (1)
- Marketing Mix 4P's and SWOT Analysis of OLPERSДокумент3 страницыMarketing Mix 4P's and SWOT Analysis of OLPERSSaad AliОценок пока нет
- HR Awards PPT 2020 12.09.2020 FinalДокумент64 страницыHR Awards PPT 2020 12.09.2020 FinalLolo OhwОценок пока нет
- PMO Crossword 1Документ4 страницыPMO Crossword 1Waseem NosimohomedОценок пока нет
- What Is Thick Film Ceramic PCBДокумент13 страницWhat Is Thick Film Ceramic PCBjackОценок пока нет
- Very Important General Knowledge MCQs With DetailsДокумент13 страницVery Important General Knowledge MCQs With DetailsNiaz AsgharОценок пока нет
- Telangana Peasants Armed StruggleДокумент9 страницTelangana Peasants Armed StruggleSudheer KolachinaОценок пока нет
- Fritz Perls in Berlin 1893 1933 ExpressiДокумент11 страницFritz Perls in Berlin 1893 1933 ExpressiLeonardo Leite0% (1)
- Synonyms, Antonyms, Spelling CorrectionsДокумент10 страницSynonyms, Antonyms, Spelling CorrectionsVenkateswara RasupalliОценок пока нет
- Conflict of Laws by Sempio DiyДокумент81 страницаConflict of Laws by Sempio DiyAp Arc100% (10)
- Engineering Economics & Financial Accounting Two Mark Questions and AnswersДокумент15 страницEngineering Economics & Financial Accounting Two Mark Questions and AnswerspothigaiselvansОценок пока нет
- Coronavirus Disease (COVID-19) : Situation Report - 125Документ17 страницCoronavirus Disease (COVID-19) : Situation Report - 125CityNewsTorontoОценок пока нет
- Unit - 5 - Trial BalanceДокумент7 страницUnit - 5 - Trial BalanceHANY SALEMОценок пока нет
- Anatomy of A Resume 2Документ4 страницыAnatomy of A Resume 2Anna CruzОценок пока нет
- Wed 0945-Avionics Modernization For LegacyДокумент38 страницWed 0945-Avionics Modernization For LegacygasparferrerОценок пока нет
- Atlas of Pollen and Spores and Their Parent Taxa of MT Kilimanjaro and Tropical East AfricaДокумент86 страницAtlas of Pollen and Spores and Their Parent Taxa of MT Kilimanjaro and Tropical East AfricaEdilson Silva100% (1)