Академический Документы
Профессиональный Документы
Культура Документы
STEMI Pathway Flowchart
Загружено:
Olga Jadha CasmiraОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
STEMI Pathway Flowchart
Загружено:
Olga Jadha CasmiraАвторское право:
Доступные форматы
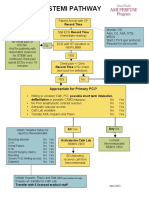
STEMI PATHWAY
Patient Arrival with CP
ECG shows ST Record Time
depression, nonspecific
Monitor V/S
changes uninterpretible Stat ECG Record Time Adm. O2, ASA, NTG,
or is normal - follow (Immediate reading) MSO4
local practice guideline
Start 2 PIVs (per protocol)
for chest pain or
ECG with ST elevation or Request for old records
R/O MI. No
And for patients with NEW LBBB
reasonable suspicion
for STEMI and YES
continued chest pain
repeat ECGs every 10 Chest pain < 12hrs
minutes Record Time of Sx onset
(see back for definition) Consult
Interventionalist
YES No REMIS 2950
Appropriate for Primary PCI?
Willing to consider Cath, PCI, possible short term intubation,
defibrillation or possible CABG (5%chance) No Yes
No Prior anaphylactic contrast reaction No Yes
Adequate vascular access No Yes
Cath Lab available No Yes
Tolerate ASA, Heparin and Plavix No Yes
Obtain Targeted history for All Yes Any No
report to Interventionalist
Bleeding disorder No Yes Activate the Cath Lab Consult
CVA No Yes REMIS 2950 Interventionalist
Renal Failure No Yes REMIS 2950
HTN No Yes
Recent Surgery (2wks) No Yes
Bleeding No Yes ED Attending
Severe PVD limiting access No Yes receives call from
Diabetes No Yes Interventionalist
Initiate Heparin, Plavix and Stat labs (per protocol on back)
Prepare pt. transfer to Cath Lab
Transfer with 2 licensed medical staff April 2012
Patients Emergently Reperfused by Facilities United for STEMI Excellence
Symptom Onset Definition
• For patients reporting symptoms initially intermittent and subsequently constant, the onset time is
defined as the time of change from intermittent to constant symptoms.
• Patients reporting symptoms that were initially mild and subsequently changed to severe, the
onset time is defined as the time of change in symptom severity.
• For patients with both, the change in symptom severity is given preeminence in determining
symptom onset time.
~AHA/ACC definition
PHYSICIAN ORDER GUIDELINES FOR THE STEMI PATIENT
Ancillary
● ECG 12 Lead STAT every 10 min with continuing CP
● RN pulse oximetry, adjust oxygen flow to obtain saturation above 95%
Laboratory
● CBC STAT ● CK/CKMB STAT
● Troponin T STAT ● PTT STAT
● CMP STAT ● PRO Time STAT
IV Fluids
□ Periph Line #1. Start 0.9% N/S 1000 ml @100 ml/hr until D/C. Use 32” extension set
□ Periph Line #1 Start Nitroglycerin concentration B, (400 mcg/ml D5W)(100mg/250ml)
Titrate to SBP 90 and pain, Cont. until D/C
Medications
□ Aspirin 325mg STAT
□ Heparin Inj 60 u/kg IV push Now (maximum dose 4000u)
□ Metoprolol 5mg IV push every 5 minutes Times 3 as tolerated**
□ Plavix 600 mg P.O. now
Physician to Nurse
□ Record estimated height, weight, and allergies
Time permitting
□ Have patient void before leaving for Cath Lab
□ Foley catheter at patient request PRN
□ Mark peripheral pulses
□ Prepare patient for cath Lab, no clothing, plastic snap gown, portable 02 and monitor
**Consider BB for hypertensive patients
Important occurrences to document and time benchmarks
1. ED Arrival
2. Mode Patient arrived in ED ( PV, EMS w/ECG, EMS w/o ECG)
3. 1st ECG time, subsequent ECG times, 1st ECG time when STEMI is diagnosed
4. Any delays that occur in ED – Pt refusal, cardiac arrest, intubation, etc.
5. Time patient departs the ED
Time goals – Time is Muscle!
ED arrival to ECG within 10 minutes
Вам также может понравиться
- ME10!03!003 MMC Pathway2Документ2 страницыME10!03!003 MMC Pathway2Indra WijayaОценок пока нет
- Algorithm-ACLS ACS 200806 1Документ1 страницаAlgorithm-ACLS ACS 200806 1Kavya Shree100% (1)
- EM Basic Chest Pain: Pet Mac P E T M A CДокумент7 страницEM Basic Chest Pain: Pet Mac P E T M A CAkanksha VermaОценок пока нет
- 49-Year-Old Male Admitted with Decreased SensoriumДокумент8 страниц49-Year-Old Male Admitted with Decreased SensoriumJan Crizza Dale R. FrancoОценок пока нет
- Post PCI Care When To ReferДокумент25 страницPost PCI Care When To ReferRahmat HidayatullahОценок пока нет
- EHC ED Critical Care Induced Hypothermia ProtocolДокумент4 страницыEHC ED Critical Care Induced Hypothermia ProtocolmaddythedocОценок пока нет
- 12 - Lead ECG Interpretation Case StudiesДокумент19 страниц12 - Lead ECG Interpretation Case StudiessharenОценок пока нет
- The PatientДокумент9 страницThe PatientJan Crizza Dale R. FrancoОценок пока нет
- Rhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Документ10 страницRhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Luis PadillaОценок пока нет
- Management of Acute Coronary Syndrome / NSTEMI: Purpose of The GuidelineДокумент7 страницManagement of Acute Coronary Syndrome / NSTEMI: Purpose of The GuidelineSahera Nurhidayah NasutionОценок пока нет
- Cerebrovascular Accident Case StudyДокумент5 страницCerebrovascular Accident Case StudyShainae meriolesОценок пока нет
- Cardiovascular Emergencies ReviewДокумент78 страницCardiovascular Emergencies Reviewtiff-toffОценок пока нет
- Expanding The Therapeutic Window For Acute Ischemic Stroke:: New Agents, New ApproachesДокумент29 страницExpanding The Therapeutic Window For Acute Ischemic Stroke:: New Agents, New ApproachesDr. RajibОценок пока нет
- Causes and Treatment of Cardiac ArrhythmiasДокумент64 страницыCauses and Treatment of Cardiac ArrhythmiasBonitavanyОценок пока нет
- Advanced Cardiac Life SupportДокумент37 страницAdvanced Cardiac Life SupportRoy Acosta GumbanОценок пока нет
- Case Study Ws I Perki 2019Документ70 страницCase Study Ws I Perki 2019Luh Leni AriniОценок пока нет
- Myocardial Infarct Checklist: TIMELINE // DateДокумент2 страницыMyocardial Infarct Checklist: TIMELINE // DateMohd Syamirulah RahimОценок пока нет
- Remon CovidДокумент13 страницRemon CovidJuli2022 Semnol-SemsaОценок пока нет
- Cardiac Emergency AMI GuideДокумент34 страницыCardiac Emergency AMI GuideAdmin neuro-usu.idОценок пока нет
- The Intern Pocket Card Surviving GraysДокумент2 страницыThe Intern Pocket Card Surviving GraysKathleen Grace ManiagoОценок пока нет
- The Finesse Trial: (Facilitated Intervention With Enhanced Reperfusion Speed To Stop Events)Документ18 страницThe Finesse Trial: (Facilitated Intervention With Enhanced Reperfusion Speed To Stop Events)NagatzulОценок пока нет
- Clinical Pathway StrokeДокумент8 страницClinical Pathway StrokedjizhieeОценок пока нет
- 15 Walters LLSA ArticlesДокумент33 страницы15 Walters LLSA ArticlesericОценок пока нет
- Symptom Onset Arrival: Circle Yes, No or Not Known As AppropriateДокумент2 страницыSymptom Onset Arrival: Circle Yes, No or Not Known As AppropriateB-win IrawanОценок пока нет
- ACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesДокумент2 страницыACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesFebrialitaFatoniОценок пока нет
- Clinical 2Документ21 страницаClinical 2api-487423840Оценок пока нет
- Pediatric ECG Final YearДокумент80 страницPediatric ECG Final Yeargrim reaperОценок пока нет
- Cpap and Bipap: "A CPAP A Day Helps Keep The ET Tube Away!"Документ15 страницCpap and Bipap: "A CPAP A Day Helps Keep The ET Tube Away!"Muhammad Tayyab MadniОценок пока нет
- Enls v4 0 Sah Slides FinalДокумент40 страницEnls v4 0 Sah Slides FinalTariku GelesheОценок пока нет
- Vascular Surgery Survival GuideДокумент8 страницVascular Surgery Survival GuideJames OyeniyiОценок пока нет
- Management of Common Cases in Emergency MedicineДокумент55 страницManagement of Common Cases in Emergency MedicinemonpyitharОценок пока нет
- Course in The Ward Intracerebral HemorrhageДокумент14 страницCourse in The Ward Intracerebral HemorrhageJeffrey Dela CruzОценок пока нет
- 26) Approach To Pediatric ArrhythmiasДокумент44 страницы26) Approach To Pediatric ArrhythmiasJude AlyousefОценок пока нет
- Medical Scenario 1Документ42 страницыMedical Scenario 1murphy 1087Оценок пока нет
- Topic: Cardiac Arrest Megacode: MD Khairulamin AS Nursing Lecturer PAPRSB Institute of Health Sciences UBDДокумент38 страницTopic: Cardiac Arrest Megacode: MD Khairulamin AS Nursing Lecturer PAPRSB Institute of Health Sciences UBDulipah100% (2)
- Acute Coronary SyndromeДокумент7 страницAcute Coronary SyndromePuskesmas Pinang JayaОценок пока нет
- Preop Conference AnesthesiaДокумент33 страницыPreop Conference AnesthesiaBhi-An BatobalonosОценок пока нет
- Bradycardia and TachycardiaДокумент66 страницBradycardia and TachycardiaKarissaОценок пока нет
- ACLS Study GuideДокумент28 страницACLS Study GuideNicole Berry100% (1)
- Joe Carcillo - Hemodynamic Managemnet in Peidtric SepsisДокумент92 страницыJoe Carcillo - Hemodynamic Managemnet in Peidtric SepsisMega SeptianaОценок пока нет
- Laporan Jaga 11 Sep (English) KoreksiДокумент30 страницLaporan Jaga 11 Sep (English) KoreksiArick Frendi AndriyanОценок пока нет
- Pre Cath DutiesДокумент2 страницыPre Cath Dutieskavvis98Оценок пока нет
- CARDIOLOGY Notes by MeДокумент33 страницыCARDIOLOGY Notes by MeJanie-Vi GorospeОценок пока нет
- Arritmias VentricularesДокумент36 страницArritmias VentricularesjshiordiaОценок пока нет
- Last Minute Notes For USMLE Step 2CKДокумент16 страницLast Minute Notes For USMLE Step 2CKJonathan B. Michaels100% (1)
- MATERI EWS PerbaikanДокумент24 страницыMATERI EWS PerbaikanagusОценок пока нет
- "Rara Sanguis": An Interesting Case PresentationДокумент83 страницы"Rara Sanguis": An Interesting Case PresentationErwin TalentoОценок пока нет
- CCU Clinical GuidelinesДокумент63 страницыCCU Clinical GuidelinesHAMMYER ALROKHAMIОценок пока нет
- An Introduction To Obstetrical Emergencies: Charles D Giordano CRNA, MSNДокумент49 страницAn Introduction To Obstetrical Emergencies: Charles D Giordano CRNA, MSNEffendi ZakriОценок пока нет
- Understanding Shock Types and TreatmentsДокумент75 страницUnderstanding Shock Types and TreatmentsaulianmediansyahОценок пока нет
- Acute Coronary SyndromeДокумент24 страницыAcute Coronary SyndromeMuhammad Alauddin Sarwar100% (8)
- Morning Report: Dr. Satya Leads Hospital TeamsДокумент42 страницыMorning Report: Dr. Satya Leads Hospital TeamsPramudia DeniОценок пока нет
- Approach To Tachyarrhythmia: SVT - VT - VF - Torsa de PointesДокумент17 страницApproach To Tachyarrhythmia: SVT - VT - VF - Torsa de PointesAmir Izzuddin SuibОценок пока нет
- Kawasaki DiseaseДокумент33 страницыKawasaki Diseasejoshianandk100% (2)
- Hydrocephalus Clinical PathwayДокумент6 страницHydrocephalus Clinical PathwayJayson OlileОценок пока нет
- Case Presentation On Supraventricular TachycardiaДокумент64 страницыCase Presentation On Supraventricular TachycardiaHazel AsperaОценок пока нет
- REV POMR KIPI SatyaДокумент20 страницREV POMR KIPI SatyaDoctoRides 46Оценок пока нет
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingОт EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingОценок пока нет
- Medicine MCQS JULY 2023 SOLVEDДокумент15 страницMedicine MCQS JULY 2023 SOLVEDLijo JoОценок пока нет
- Pott DiseaseДокумент36 страницPott DiseaseGiovanna Algu100% (1)
- Grand Rounds: Jinghua Chen, MD, PHD July 15Th, 2016Документ23 страницыGrand Rounds: Jinghua Chen, MD, PHD July 15Th, 2016miraОценок пока нет
- Kayexalate Drug StudyДокумент3 страницыKayexalate Drug StudyAngelou Joefred Congreso100% (1)
- Post-Hypoxic Myoclonus - Current Concepts, Neurophysiology, and TreatmentДокумент18 страницPost-Hypoxic Myoclonus - Current Concepts, Neurophysiology, and TreatmentkkkljlkjОценок пока нет
- Gliomas Linea Media 1Документ9 страницGliomas Linea Media 1JOHN LOPERAОценок пока нет
- Pediatrics IIДокумент22 страницыPediatrics IICertificate SurrenderОценок пока нет
- Clinical Approach To The Dysmorphic Child-R-1Документ108 страницClinical Approach To The Dysmorphic Child-R-1Drbhupeshwari Gour100% (1)
- Last Minute Notes For USMLE Step 2CKДокумент16 страницLast Minute Notes For USMLE Step 2CKJonathan B. Michaels100% (1)
- Kali CarbДокумент12 страницKali CarbRaveendra Mungara100% (1)
- PE and HealthДокумент3 страницыPE and HealthRia Ellaine Cornelio LachicaОценок пока нет
- Anaesthesia and CopdДокумент7 страницAnaesthesia and CopdAshish PandeyОценок пока нет
- Ice Berg Phenomenon of DiseaseДокумент50 страницIce Berg Phenomenon of DiseaseMan BoruahОценок пока нет
- Maternal Obstetric EWS SystemДокумент59 страницMaternal Obstetric EWS SystemIndrati TRОценок пока нет
- How Physiotherapy Helps - Patient StoriesДокумент2 страницыHow Physiotherapy Helps - Patient StoriesDobreanu Bianca100% (1)
- Tog 12685Документ3 страницыTog 12685saeed hasan saeedОценок пока нет
- Teaching Plan 2023Документ4 страницыTeaching Plan 2023Mark Victor CortezanoОценок пока нет
- Female Genital TuberculosisДокумент6 страницFemale Genital TuberculosisallauddinbarackzaiОценок пока нет
- TSO Medical GuidelinesДокумент42 страницыTSO Medical GuidelinesEmilio SantiagoОценок пока нет
- United Home Whitfield's OintmentДокумент5 страницUnited Home Whitfield's OintmentWalidur Rahman MridulОценок пока нет
- Renal EmergenciesДокумент11 страницRenal EmergenciesDemuel Dee L. BertoОценок пока нет
- Abg Tic Tac Toe Part 1 and 2Документ6 страницAbg Tic Tac Toe Part 1 and 2Elizabeth McKeeОценок пока нет
- Final NCP PediaДокумент2 страницыFinal NCP PediaKuro HanabusaОценок пока нет
- NCP Ineffective Tissue PerfusionДокумент1 страницаNCP Ineffective Tissue PerfusionLEONELLGABRIEL RAGUINDINОценок пока нет
- ESR Test ExplainedДокумент3 страницыESR Test ExplainedbibahОценок пока нет
- Endo Test Bank 1Документ6 страницEndo Test Bank 1mildred alidon100% (1)
- PracticeExam 3 QsДокумент17 страницPracticeExam 3 QsBehrouz YariОценок пока нет
- Oa Case ReportДокумент26 страницOa Case Reportaliffikri52100% (1)
- Nursing Lab 3 Skill Performance Checklist Administering A Blood Transfusion S U NP CommentsДокумент2 страницыNursing Lab 3 Skill Performance Checklist Administering A Blood Transfusion S U NP CommentsCandice Cheng88% (8)
- Form application for registration of AlbiglutideДокумент6 страницForm application for registration of AlbiglutideMd. Abdur RahmanОценок пока нет