Академический Документы
Профессиональный Документы
Культура Документы
Mohan Et Al
Загружено:
Dwi WicaksonoОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Mohan Et Al
Загружено:
Dwi WicaksonoАвторское право:
Доступные форматы
Reminder of important clinical lesson
CASE REPORT
Treacher Collins syndrome: a case report
Ravi Prakash Sasankoti Mohan, Sankalp Verma, Neha Agarwal, Udita Singh
Department of Oral Medicine & SUMMARY
Radiology, Kothiwal Dental Treacher Collins syndrome is a rare autosomal dominant
College & Research Center,
Moradabad, Uttar Pradesh,
disorder of craniofacial development. The fully expressed
India phenotype exhibits characteristic dysmorphic features
involving the face, eyes, mandible and ears. We report a
Correspondence to case of a 17-year-old woman presenting with the typical
Dr Ravi Prakash Sasankoti
orofacial implications of this syndrome.
Mohan,
sasan_ravi@rediffmail.com
BACKGROUND
Mandibulofacial dysostosis (MFD), or Treacher
Collins syndrome (TCS), is an autosomal domin-
antly inherited disorder that arises from aberrations
in the development of facial structures derived
from the first and second branchial arches during
histodifferentiation morphogenesis between
approximately the 20th day and the 12th week of
intrauterine life.1 This syndrome was described by
Thomson (1846), Berrry (1889), Treacher Collins
(1900) and Franceschetti and Klein (1949).2
Downward slanting palpebral fissures and hypo-
plasia of the zygomatic arch have been defined as
the minimum diagnostic criteria by Teber et al. The
present case report illustrates the orofacial features
of this syndrome.
Figure 1 Profile photograph of the patient
CASE PRESENTATION demonstrated mandibular and zygomatic hypoplasia and
A 17-year-old woman reported to our department antimongoloid slant of eyes.
with t a sensitivity to hot and cold in her left lower
back tooth. An extraoral examination revealed a
narrow face with mandibular and zygomatic Overall, clinical and radiographic features were
hypoplasia along with antimongoloid slant of eyes suggestive of TCS.
(figure 1). Mandibular hypoplasia caused the upper
dentition to appear protruded. Malar hypoplasia INVESTIGATIONS
resulted in a ‘sunk-in’ appearance temporally, causing Radiographs:
the nose to appear very prominent. The patient’s ▸ Extraoral PA skull view demonstrated malar and
eyes were remarkable and there was partial absence mandibular hypoplasia along with hypertrophy
of lower eyelashes and coloboma of lower lateral of both maxillary sinus walls (figure 4).
eyelid (figure 2). External ear malformation in the ▸ Lateral skull revealed prominent antigonial
form of a rudimentary pinna was present bilaterally. notch and anterior open bite (figure 5).
In addition, the external ear canals were atresic with
absence of opening from the external to the internal
ear. Conduction deafness with 50% reduction in
hearing was also present. Another interesting feature
was the presence of a tongue-shaped process of hair
on the lateral side of the face (figure 3). Intraoral
examination revealed an anterior open bite and
carious left lower first and second molars. This
patient was the youngest of the four children born to
parents with no history of consanguineous marriage.
Her mother was 36 years and her father was
To cite: Mohan RPS,
Verma S, Agarwal N, et al.
44-year-old at the time of her birth. None of the sib-
BMJ Case Rep Published lings showed these facial features. The radiographic
online: [ please include Day investigations (posterioanterior (PA) skull view and
Month Year] doi:10.1136/ lateral skull view) revealed mandibular hypoplasia Figure 2 Partial absence of lower eyelashes and
bcr-2013-009341 along with prominent antigonial notch. coloboma of the lower lateral eyelid.
Mohan RPS, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-009341 1
Reminder of important clinical lesson
Figure 5 Lateral skull revealed prominent antigonial notch and
anterior open bite.
Figure 3 External ear abnormality and tongue-shaped process of hair
on lateral aspect of face.
DIFFERENTIAL DIAGNOSIS
▸ Nager’s acrofacial dysostosis
▸ Milleracrofacial dysostosis
▸ Oculoauriculovertebral spectrum
▸ Goldenhar syndrome
TREATMENT
The patient was treated for her chief complaint and was moti-
vated for orthodontic treatment and prosthetic reconstruction
of the ears.
OUTCOME AND FOLLOW-UP
The prognosis for the current case was fair.
DISCUSSION
TCS, alternatively called MFD, is an autosomal craniofacial
development disorder related to the chromosomal region 5q32–
q33.1, presenting peculiar facial aspect and clinical and genetic
heterogeneity.3 A total of 51 mutations in the TCOF1 gene had
been identified to date, all of which result in introduction of
premature termination codons into the reading frame, suggest-
ing haploinsufficiency as the molecular mechanism underlying
the disorder.4 The incidence is estimated at 1 in 50 000 live
births; nearly 40% of cases present familial history, whereas the
remaining 60% are considered new mutations. Its occurrence is
influenced by the increase in paternal age.3 The adult patient
with fully expressed TCS has a convex facial profile with a
prominent dorsum of the nose above a retrusive lower jaw and
chin. The eyes are characterised by an antimongoloid slant of
the palpebral fissure resulting from coloboma and hypoplasia
of the lower eyelids and lateral canthi, including partial absence
Figure 4 Posterioanterior skull showing mandibular and malar of eyelid cilia.3 5 ‘Tongue-shaped’ processes of hair frequently
hypoplasia with hypertrophy of both maxillary sinus walls. extending into the pre-auricular region. The external ears are
2 Mohan RPS, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-009341
Reminder of important clinical lesson
absent, malformed or malposed, and hearing was impaired as a the defect to 50% of offsprings in accordance with Mendelian
result of variable degrees of hypoplasia of the external auditory laws of genetics. This emphasises the importance of genetic
canals and ossicles of the middle ears.5 All the above-mentioned counselling to affected individuals. It is our responsibility as oral
features were present in our case. Macrostomia or alternatively physicians to recognise this disorder, to be aware of its manifes-
microstomia with a narrow and high palatal vault, and a cleft tations and to provide close follow-up, appropriate therapy and
palate in about 35% of cases is also seen.6 Palate deformities counselling.9 Also, early diagnosis of TCS allows prompt and
were not present in our patient; however, intraorally, anterior appropriate treatment of aesthetic and functional deficiencies in
open bite was present. Dental misalignments with anterior open these patients. In fact, ameliorating the outward signs gives
bite are frequent in this syndrome.6 Other dental anomalies these patients the opportunity to have an improved social life.8
include supernumerary teeth, T-shaped teeth, enamel opacity,
enamel hypoplasia, tooth agenesis, microdontia, tooth rotations
and ectopic tooth positioning.3 The characteristic facies in TCS Learning points
occur as a result of the destruction of the neural crest cells
before they migrate to form the facial processes. Normally
derived structures of the first and second branchial arches ▸ Early diagnosis of Treacher Collin syndrome allows prompt
exhibit malformation.1 A diagnosis was made based upon a and appropriate treatment of aesthetic and functional
thorough clinical evaluation, detailed patient history and identi- deficiencies in these patients. If this can be performed early,
fication of characteristic findings. Specialised imaging techniques it is possible to take advantage of anticipated growth during
such as x-ray or CT may be performed to assess the extent of normal skeletal maturation and to obtain better therapeutic
certain craniofacial abnormalities such as middle and inner ear results.
structures.7 Molecular genetic testing to confirm a diagnosis is ▸ In severe cases the airway must be evaluated and secured
available through commercial and academic research laborator- from birth. Either positioning alone or tracheostomy is
ies to detect mutations in the TCOF1, POLR1C and POLR1D required to manage the airway, and a gastrostomy required
genes. Approximately 90–95% of individuals have an identifi- for feeding.
able mutation of the TCOF1 gene. Prenatal screening via ultra- ▸ Genetic counselling can help families understand the
sound during mid-to-late gestation may detect cases with severe condition and how to care for the patients.
craniofacial abnormalities. Relatives, especially parents and sib-
lings, of an individual diagnosed with TCS should be carefully
examined because mild cases often go unnoticed and undiag-
Competing interests None.
nosed.7 Treatment of MFD (TCS) is lengthy and requires a
Patient consent Obtained.
multidisciplinary approach focused on treatment of symptoms.
In newborns with MFD, immediate attention to airway and Provenance and peer review Not commissioned; externally peer reviewed.
swallowing inadequacies is critical. A tracheostomy (a hole into
the trachea through the front of the neck) may be needed REFERENCES
to help breathing, while reconstructive surgery may be necessary 1 Magalhaes MHCG, Da Silveria CB, Moreira CR, et al. Clinical and imaging
correlations of Treacher Collins syndrome: report of two cases. Oral Surg Oral Med
to correct a cleft palate. A notch, or coloboma, in the lower
Oral Pathol Oral Radiol Endod 2007;103:836–42.
eyelid may cause the eyes to dry out easily, increasing the risk of 2 Cannistra C, Barbet JP, Houtte A, et al. Mandibulo-facial dysostosis: comparison
infection. This may require surgery. Reconstructive surgery may study of a neonate with mandibulo-facial dyostosis and a normal neonate.
also be offered to build up the cheekbones, correct the nose or J Craniomaxillofac Surg 1998;26:92–7.
an underdeveloped jaw (which may help to improve breathing) 3 Dalben GD, Costa B, Gomide MR. Prevalence of dental anomalies, ectopic eruption
and associated malformations in subjects with Treacher Collins syndrome. Oral Surg
or reconstruct the outer ear.7 –9 Other treatment includes dis- Oral Med Oral Pathol Oral Radiol Endod 2006;101:588–92.
traction osteogenesis associated with preoperative and post- 4 Marszalek B, Wojcicki P, Kobus K, et al. Clinical features, treatment and genetic
operative orthodontic treatment leading to a better quality of background of Treacher Collins syndrome. J Appl Genet 2002;43:223–33.
life.8 Surgical reconstruction of the auricle can be satisfactorily 5 Posnick JC. Treacher Collins syndrome: perspectives in evaluation and treatment .
J Oral Maxillofac Surg 1997;55:1120–33.
achieved through a staged approach in the hands of a few
6 Opitz C, Ring P, Stoll C. Orthodontic and surgical treatment of patients with
experts. The successful grafting of a well-sculpted cartilage congenital unilateral and bilateral mandibulofacial dysostosis. J Orofac Orthop
framework is the foundation for a sound auricle repair. Other 2004;65:150–63.
stages of the auricular construction include lobule transposition, 7 National Organization for Rare Disorders. The physician’s guide to Treacher Collins
detaching the auricle with a skin graft, managing the hairline syndrome. Danbury, Connecticut: National Organization for Rare Disorders, 2012.
8 Martelli-Junior H, Coletta RD, Miranda RT, et al. Orofacial features of Treacher Collins
and reconstructing the tragus.5 TCS is an example of an auto- syndrome. Med Oral Patol Oral Cir Buccal 2009;14:E344–8.
somal dominant syndrome with incomplete penetrance and vari- 9 Mittman DL, Rodman OG. Mandibulofacial dysostosis (Treacher Collins syndrome):
able expressivity. An affected parent of either sex will transmit a case report. J Natl Med Assoc 1992;84:1051–4.
Mohan RPS, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-009341 3
Reminder of important clinical lesson
Copyright 2013 BMJ Publishing Group. All rights reserved. For permission to reuse any of this content visit
http://group.bmj.com/group/rights-licensing/permissions.
BMJ Case Report Fellows may re-use this article for personal use and teaching without any further permission.
Become a Fellow of BMJ Case Reports today and you can:
▸ Submit as many cases as you like
▸ Enjoy fast sympathetic peer review and rapid publication of accepted articles
▸ Access all the published articles
▸ Re-use any of the published material for personal use and teaching without further permission
For information on Institutional Fellowships contact consortiasales@bmjgroup.com
Visit casereports.bmj.com for more articles like this and to become a Fellow
4 Mohan RPS, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-009341
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Alabama Board of Medical Examiners Statement On Federal Pill Mill TakedownДокумент103 страницыAlabama Board of Medical Examiners Statement On Federal Pill Mill TakedownAshley RemkusОценок пока нет
- ENTEROBACTERIACEAEДокумент13 страницENTEROBACTERIACEAEStephen Jao Ayala Ujano100% (1)
- 2014 Body Code Client Information PDFДокумент7 страниц2014 Body Code Client Information PDFkrug100% (1)
- A Mindfulness Intervention For Children With Autism Spectrum DisorderДокумент155 страницA Mindfulness Intervention For Children With Autism Spectrum Disorderclaughlinsr4721Оценок пока нет
- Reiki 1 ManualДокумент11 страницReiki 1 Manualbelgarath2013100% (1)
- The Chemical ImbalanceДокумент70 страницThe Chemical ImbalancebredabredaОценок пока нет
- IntroductiontoEpidemiologyandPublicHealth AnswersДокумент17 страницIntroductiontoEpidemiologyandPublicHealth AnswersDiamond_136100% (2)
- Anatomy and Physiology of the Lactating BreastДокумент3 страницыAnatomy and Physiology of the Lactating BreastDwi WicaksonoОценок пока нет
- Treatment of Diabetic Neuropathy - UpToDateДокумент20 страницTreatment of Diabetic Neuropathy - UpToDateKarina MilaréОценок пока нет
- Principles of The Vascular ExamДокумент63 страницыPrinciples of The Vascular ExamDwi WicaksonoОценок пока нет
- Analytical Method Validation of Clopidogrel Tablets BR HPLCДокумент48 страницAnalytical Method Validation of Clopidogrel Tablets BR HPLCAman ThakurОценок пока нет
- S6 Upper Cervical Spine TraumaДокумент82 страницыS6 Upper Cervical Spine TraumaDwi WicaksonoОценок пока нет
- Treacher Collins Syndrome: A Case Report and Review of LiteratureДокумент10 страницTreacher Collins Syndrome: A Case Report and Review of LiteratureDwi WicaksonoОценок пока нет
- Sci-Hub - The Microvascular Anatomy of Superior and Inferior Gluteal Artery Perforator (SGAP and IGAДокумент1 страницаSci-Hub - The Microvascular Anatomy of Superior and Inferior Gluteal Artery Perforator (SGAP and IGADwi WicaksonoОценок пока нет
- Lirik 1Документ2 страницыLirik 1Dwi WicaksonoОценок пока нет
- KothariДокумент7 страницKothariDwi WicaksonoОценок пока нет
- Treacher Collins Syndrome-A Case Report and Review of LiteratureДокумент5 страницTreacher Collins Syndrome-A Case Report and Review of LiteratureDwi WicaksonoОценок пока нет
- Nash Head1Документ1 страницаNash Head1Dwi WicaksonoОценок пока нет
- v3Документ29 страницv3Dwi WicaksonoОценок пока нет
- An Alternative To Hysterectomy: Manchester RepairДокумент0 страницAn Alternative To Hysterectomy: Manchester RepairDwi WicaksonoОценок пока нет
- Hippokratia 11 99Документ6 страницHippokratia 11 99Dwi WicaksonoОценок пока нет
- Kord All of MeДокумент2 страницыKord All of MeMuhammad Nuh IzzuddinОценок пока нет
- Journal 2 - T3 and PTU On RatsДокумент8 страницJournal 2 - T3 and PTU On RatsDwi WicaksonoОценок пока нет
- FF 8Документ14 страницFF 8Dwi WicaksonoОценок пока нет
- Alida Harahap Dept. Clinical Pathology FmuiДокумент24 страницыAlida Harahap Dept. Clinical Pathology FmuiDwi WicaksonoОценок пока нет
- Misoprostole in ObstetricsДокумент11 страницMisoprostole in ObstetricsDr-Saja O. DmourОценок пока нет
- Aa 1 MasterRQsДокумент93 страницыAa 1 MasterRQsSadhana SabhandasaniОценок пока нет
- Sound Transduction EarДокумент7 страницSound Transduction Earhsc5013100% (1)
- Kerala PДокумент106 страницKerala PJeshiОценок пока нет
- Chapter 8 ErgonomicsДокумент18 страницChapter 8 ErgonomicsAsif Rahman RaktimОценок пока нет
- Spherocytosis & Increased Risk of Thrombosis. Kam Newman, Mojtaba Akhtari, Salim Shakour, Shahriar DadkhahДокумент1 страницаSpherocytosis & Increased Risk of Thrombosis. Kam Newman, Mojtaba Akhtari, Salim Shakour, Shahriar DadkhahjingerbrunoОценок пока нет
- Elgabri v. Lekas, M.D., 1st Cir. (1992)Документ21 страницаElgabri v. Lekas, M.D., 1st Cir. (1992)Scribd Government DocsОценок пока нет
- OrthodonticsДокумент9 страницOrthodonticsReda IsmaeelОценок пока нет
- Monnal t75 Air Liquide Ventilator PDFДокумент10 страницMonnal t75 Air Liquide Ventilator PDFFederico DonfrancescoОценок пока нет
- ReviewerДокумент20 страницReviewerYang MolosОценок пока нет
- Philips Respironics Bipap ST Niv Noninvasive VentilatorДокумент2 страницыPhilips Respironics Bipap ST Niv Noninvasive Ventilatorsonia87Оценок пока нет
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Документ81 страницаHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadОценок пока нет
- Occupational Therapy Rehabilitation Paraplegic PatientДокумент7 страницOccupational Therapy Rehabilitation Paraplegic PatientAlina PasăreОценок пока нет
- Essential and Non-Essential Fatty Acids PDFДокумент4 страницыEssential and Non-Essential Fatty Acids PDFBj Delacruz100% (2)
- Nursing Comps Study GuideДокумент15 страницNursing Comps Study GuideforminskoОценок пока нет
- Pulmonary EmbolismДокумент93 страницыPulmonary EmbolismRakesh PanchalОценок пока нет
- CasestudynervoussystemДокумент2 страницыCasestudynervoussystemapi-265854240Оценок пока нет
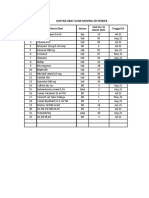
- Daftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Документ8 страницDaftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Vima LadipaОценок пока нет
- BSN 4A Group 5 Nigerian AmericanДокумент39 страницBSN 4A Group 5 Nigerian AmericanAngelie PantajoОценок пока нет
- Akupuntur 7Документ9 страницAkupuntur 7Ratrika SariОценок пока нет
- How To Avoid Medication ErrorsДокумент2 страницыHow To Avoid Medication ErrorsLorenn AdarnaОценок пока нет