Академический Документы
Профессиональный Документы
Культура Документы
Safety and Efficacy of Phenylephrine Nasal Drops in Bronchiolitis
Загружено:
AriАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Safety and Efficacy of Phenylephrine Nasal Drops in Bronchiolitis
Загружено:
AriАвторское право:
Доступные форматы
Iran J Pediatr
Original Article Oct 2014; Vol 24 (No 5), Pp: 593-597
Safety and Efficacy of Phenylephrine Nasal Drops in Bronchiolitis
Gholamreza Soleimani*1, MD; Marzieh Akbarpour, MD; Mehdi Mohammadi2, PhD
1Research Center for Children and Adolescents, 2Department of Pediatrics, 3Department of Epidemiology and Biostatistics, Zahedan
University of Medical Sciences , Zahedan , Iran
Received: Nov 14, 2013; Accepted: Jun 25, 2013; First Online Available: Oct 05, 2014
Abstract
Objective: Bronchiolitis is a common lower respiratory tract infection in the first year of life. In this disease
upper respiratory tract infection is associated with nasal congestion, respiratory distress and hypoxia. We
studied the effect of phenylephrine drops as a decongestant in treatment of light and moderately severe cases
of acute bronchiolitis.
Methods: This is a double blind randomized trial involving 100 children aged 4 weeks to 12 months. The
patients were divided into two groups, the first group received 0.1 ml phenylephrine 0.5% and the second
group 0.1 ml sodium chloride (NaCl) 0.9% as placebo in both nostrils. Respiratory rate, heart rate, O2
saturation, dyspnea, retractions and wheezing were assessed before and 30 minutes after medication.
Findings: After medication, O2 saturation and respiratory muscles retractions in the phenylephrine group
were significantly better than those of the placebo group (P=0.004 and P=0.002, respectively). In the
phenylephrine group, O2 saturation, retractions and wheezing were also significantly better before than those
after medication (P=0.003 and P<0.0001 respectively). In the placebo group no significant difference before
and after intervention was observed.
Conclusion: Phenylephrine as a topical decongestant is an inexpensive, easily available and suitable means in
the treatment of mild to moderately severe bronchiolitis.
Iranian Journal of Pediatrics, Volume 24 (Number 5), October 2014, Pages: 593-597
Key Words: Respiratory Tract; Bronchiolitis; Alpha Agonist; Phenylephrine
Introduction signs and symptoms related to upper airway
obstruction. Phenylephrine as an alpha-agonist is
Acute bronchiolitis is the most common lower supposed to reduce nasal edema[4].
respiratory tract infection in the first year of life The effect of epinephrine[5-7], inhaled
and also the most common reason for the infants’ furosemide[1], inhaled hypertonic saline[8-10], xylo-
hospitalization during winter season[1,2], res- methazoline[2], phenylephrine[4], dexamethasone
piratory syncytial virus being the most common [11] and zinc sulfate[12] has been investigated in
cause. Unfortunately no remarkable progress in its treatment of bronchiolitis. Nevertheless, the only
treatment is achieved in recent years[3]. non-controversial treatment remains supportive
Involvement of upper airways in bronchiolitis therapy[3].
leads to nasal congestion, inadequate oral intake, The results of studies on the effect of α-
dehydration, respiratory distress and hypoxemia blockers as decongestant are controversial.
[2]. Therefore, nasal decongestants may relieve the Therefore, we tried to compare the effect of
* Corresponding Author;
Address: Research Center for Children and Adolescents Health, Zahedan University of Medical Sciences Ali- Ebne Abitaleb Hospital, Zahedan , Iran
E-mail: soleimanimd@yahoo.com
© 2014 by Pediatrics Center of Excellence, Children’s Medical Center, Tehran University of Medical Sciences, All rights reserved.
Iran J Pediatr; Vol 24 (No 5), Oct 2014
Published by: Tehran University of Medical Sciences (http://ijp.tums.ac.ir)
594 Safety and Efficacy of Phenylephrine Nasal Drops in Bronchiolitis
intranasal phenylephrine (as a decongestant) with To determine the sample size, mean respiratory
sodium chloride (NaCl) 0.9% (as placebo). rate was taken to be 43 in treatment and 42 in
control group with 1.6 as standard deviation[4], 5%
and 20% type I and II error respectively.
Therefore sample size was calculated to be 50
patients in each group.
Subjects and Methods Analyses of data were done by the SPSS
(version 16) using chi-square, Wilcoxon, Kruskal-
This double blind randomized clinical study was Wallis and independent sample t-test. The level of
conducted in Ali-Ebne-Abitaleb hospital, Zahedan, significance was considered according to 95%
Southeast Iran. All patients aged 4 weeks to 12 confidence interval.
months with clinical diagnosis of viral
bronchiolitis were eligible for the study. Clinical
diagnosis of viral bronchiolitis was based on the
first episodes of wheezing in infants with a viral Findings
upper respiratory tract infection[13]. Wheezing was
evaluated with a stethoscope and defined as end- One hundred and seven patients (38% boys)
expiratory or expiratory according to the between 4 weeks and 1 year old (mean age
physician’s hearing. Oxygen therapy was defined 6.02±3.2 months) were eligible to participate in
as oxygen supply via head box to increase blood O2 the study. Seven patients were excluded because
saturation to more than 90 percent. of prematurity (2 cases), unstable vital signs (2
Patients with following criteria were excluded: cases), severe bronchiolitis (2 cases), or congenital
gestational age less than 34 weeks; heart rate heart disease (1 case).
more than 200 beats/min; respiratory rate >70 In the initial examination there was no
breaths/min; use of α- or β-agonists during 24 significant difference between the two groups in
hours before admission; hypotension; chronic demographic data including heart rate, respiratory
disease, history of atopia in first degree relatives, rate, O2 saturation, retrac-tions, wheezing, and
known cases of cystic fibrosis and any signs and dyspnea (Table 1).
symptoms of severe bronchiolitis. Thirty minutes after administration of
The medical staff involved in the study was phenylephrine drops, O2 saturation significantly
blinded. Both drops were smell- and colorless and increased in group A (P=0.004) whereas the
just labeled A and B. Based on permuted-block severity of retractions significantly decreased
randomization, patients were allocated to receive (Table 2).
phenylephrine 0.5% drop (A) or NaCl 0.9% drop Comparison of data showed that O2 saturation
(B) in both nostrils while in supine position and significantly increased in the case group after
remained in this position for one minute. phenylephrine drops (P=0.003) and the severity of
Case and control group both received routine retractions and wheezing significantly decreased
treatment for bronchiolitis (O2 therapy, (P<0.0001 and P=0.006 respectively) (Table 3).
salbutamol spray, nasal suction and neubulizer). There were no statistical differences in any of
Case group received in addition phenylephrine the outcome measures in group B before and after
0.5%, one drop in each nostril, which was replaced medication (Table 4). No adverse effect was seen
by NaCl 0.9% in the control group. after application of the decongestant.
O2 saturation, respiratory rate, heart rate,
retractions, dyspenea and wheezing were
evaluated by the same investigator thirty minutes
after administration of the drug and placebo.
Dyspenea was defined as one or more of the Discussion
following items: difficulty in feeding; decreased
vocalization, and/or agitation. Retractions were This study demonstrated that phenylephrine (as a
noted as no retractions, intercostal retractions or nasal decongestant) is more effective than normal
subcostal+inter-costal retractions. saline solution (as a placebo) to treat acute
Iran J Pediatr; Vol 24 (No 5), Oct 2014
Published by: Tehran University of Medical Sciences (http://ijp.tums.ac.ir)
Soleimani Gh, et al 595
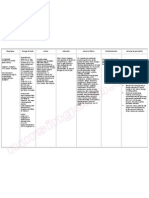
Table 1: Demographic characteristics and pre-treatment data
Parameter Phenylephrine (n=50) NaCl (n=50) P. value
Age 6.6 (3.4)α 5.4 (3.04)α 0.08
Male 21 (42%) 17 (34%) 0.4
Sex
Female 29 (58%) 33 (66%)
No retractions 5 (10%) 1 (2%)
Retraction Intercostal 19 (38%) 23 (46%) 0.7
Subcostal + intercostal 26 (52%) 26 (52%)
NL feeding, vocalization and activity 5 (10%) 7 (14%)
One of the following: difficulty in feeding;
Dyspnea decreased vocalization; or agitation 25 (50%) 14 (28%) 0.2
Two of the following: difficulty in feeding,
decreased vocalization, and/or agitation 20 (40%) 29 (58%)
End-expiratory 14 (28%) 17 (34%)
Wheeze 0.5
Expiratory 36 (72%) 33 (66%)
O2 saturation 93.1 (4.2)α 92.1 (4.03)α 0.2
Respiratory rate 44.7 (9.3)α 47.5 (9.5)α 0.1
Heart rate 115.3 (9.9)α 118.2 (8.7)α 0.1
α: Mean (Standard Deviation); NaCl: Sodium Chloride
bronchiolitis and reduce clinical severity of the decongestants in the treatment of pediatric
symptoms. Alpha-adrenergics produce vasocons- bronchiolitis[2,4]. According to American Academy
triction and decrease blood flow through of Pediatrics a consistent benefit from α-
microvesseles, leading to decreased resistance to adrenergic or β-adrenergic agents for bronchiolitis
airflow by reducing hyperemia, mucosa swelling, treatment is controversial. So, α-adrenergic or β-
plasma exudation and nasal secretions[13]. In adrenergic medication is an option to be more
allergic rhinitis, oral and topical decongestants investigated[17]. In a study, nasal decongestant
cause vasoconstriction and oppose vasodilation in (xylometazoline) was as effective as epinephrine
the nasal mucosa, thus decreasing inflammation in the treatment of acute bronchiolitis, so it was
and reducing nasal airway resistance so that the concluded that upper respiratory tract diseases
nasal congestion is diminished and nose breathing have an important effect on clinical presentation
faci-litated[14,15]. and pathogenesis of bronchiolitis[2]. Another study
There is a wide-range of practice in the assessed the effect of nasal phenyephrine in
management of bronchiolitis[16] but there are infants hospitalized for bronchiolitis and
limited studies available on the effect of nasal concluded that respiratory status does not change
Table 2: Comparison of data between phenylephrine and placebo 30 minutes after application
Parameter Phenylephrine (n=16) NaCl (n=16) P. value
No retractions 8 (16%) 0 (0%)
Retraction Intercostal 29 (58%) 25 (50%) 0.002
Subcostal + intercostal 13 (26%) 25 (50%)
NL feeding, vocalization and activity
4 (8%)
One of the following: difficulty in feeding; 8 (16%)
30 (60%)
Dyspnea decreased vocalization; or agitation 13 (26%) 0.2
Two of the following; difficulty in feeding; 29 (58%)
16 (32%)
decreased vocalization; and/or agitation
No wheeze 3 (6%) 0 (0%)
Wheeze End-expiratory 18 (36%) 19 (38%) 0.5
Expiratory 29 (58%) 31 (62%)
O2 saturation 94.1 (3.7)α 91.9 (3.5)α 0.004
Respiratory rate 43.9 (9.1)α 47.2 (9.5)α 0.1
Heart rate 114.3 (9.7)α 118.1 (10.7)α 0.06
α: Mean (Standard Deviation); NaCl: Sodium Chloride
Iran J Pediatr; Vol 24 (No 5), Oct 2014
Published by: Tehran University of Medical Sciences (http://ijp.tums.ac.ir)
596 Safety and Efficacy of Phenylephrine Nasal Drops in Bronchiolitis
Table 3: Comparison of data before and 30 minutes after phenylephrine application
Parameter Before (n=50) After (n=50) P. value
No retraction 5 (10%) 8 (16%)
Retraction Intercostal 19 (83%) 29 (58%) <0.0001
Subcostal+intercostal 26 (52%) 13 (26%)
NL feeding, vocalization and activity 5 (10%) 4 (8%)
One of the following: difficulty in feeding; 25 (50%) 30 (60%)
Dyspnea decreased vocalization; or agitation 0.3
Two of the following: difficulty in feeding; 20 (40%) 16 (32%)
decreased vocalization; and/or agitation
No wheeze 0 (0%) 3 (6%)
Wheeze End-expiratory 4 (28%) 18 (36%) 0.006
Expiratory 36 (72%) 29 (58%)
O2 saturation 93.1 (4.2)α 94.1 (3.7)α 0.003
Respiratory rate 44.7 (9.3)α 43.9 (9.09)α 0.07
Heart rate 115.3 (9.9)α 114.3 (9.7)α 0.2
α: Mean (Standard Deviation); NaCl: Sodium Chloride
after short term use of topical nasal of therapy, and long term follow up to validate
phenylephrine. This seemed to be attributed to systemic and topical effect and eventual side
strict inclusion and exclusion criteria, parental effects (such as rebound) of the lhenylephrine
refusal and lack of study personnel on weekends nasal drops more exactly.
and nights[4]. Diagnostic tests such as radiography
and viral antigen test can be applied to confirm
diagnosis, although clinical diagnosis is
decisive[18,19]. Therefore our patients were
diagnosed clinically. In accordance with previous Conclusion
studies[2,4], we observed no adverse effects of
phenylephrine as a topical nasal decongestant and Intranasal phenylephrine as an alpha-adrenergic
found it safe in short course usage. Rebound nasal decongestant, in combi-nation with supportive
congestion does not appear after a single dose but therapy in bronchiolitis, is a safe, not expensive
it might be seen after recurrent doses[4]. and effective treatment for mild to moderate viral
Short time assessment of decongestant effect bronchiolitis for both inpatient and outpatient
can be seen as a limitation of our study. More treatment. Further studies are needed to
studies with frequent usage of the decongestant determine the optimal dosing and time interval to
are needed to determine suitable dosage, duration identify the maximum effect.
Table 4: Comparison of data before and 30 minutes after normal NaCl application
Parameter Before (n=50) After (n=50) P-value
No retractions 1 (2%) 0 (0%)
Retraction Intercostal 23 (46%) 25 (50%) 1
Subcostal & intercostal 26 (52%) 25 (50%)
NL feeding, vocalization and activity 7 (14%) 8 (16%)
One of the following: difficulty in feeding; 14 (28%) 13 (26%)
Dyspnea decreased vocalization, or agitation 0. 65
Two of the following: difficulty in feeding, 29 (58%) 29 (58%)
decreased vocalization, and/or agitation
No wheeze 0 (0%) 0 (0%)
Wheeze End-expiratory 17 (34%) 19 (38%) 0.15
Expiratory 33 (66%) 31 (62%)
O2 saturation 92.1 (4.03)α 91.9 (3.5)α 0.57
Respiratory rate 47.5 (9.5)α 47.2 (9.5)α 0.17
Heart rate 118.2 (8.7)α 118.1 (10.7)α 0.95
α: Mean (Standard Deviation); NaCl: Sodium Chloride
Iran J Pediatr; Vol 24 (No 5), Oct 2014
Published by: Tehran University of Medical Sciences (http://ijp.tums.ac.ir)
Soleimani Gh, et al 597
Acknowledgment and gas exchange in bronchiolitis. Am J Respir Crit
Care Med 2001;164(1):86–91.
This study was approved by the Ethics Committee of
7. Modaressi M, Asadian A, Faghihinia J. Comparison of
Zahedan University of Medical Sciences (Registry code:
epinephrine to salbutamol in acute bronchiolitis.
89-2564).
Iran J Pediatr 2012;22(2):241-4.
Authors’ Contribution 8. Chaudhry K, Sinert R. Is nebulized hypertonic saline
solution an effective treatment for bronchiolitis in
G. Soleimani: Concept and Design, Critical Revision of the infants? Ann Emerg Med 2010;55(1):120-2.
Manuscript
9. Kuzik BA, Al Qadhi SA, Kent S, et al. Nebulized
M. Akbarpour: Acquisition of Data, Manuscript Preparation
M. Mohammadi: Data Analysis and Interpretation, hypertonic saline in the treatment of viral
All authors Approved final version of the paper. bronchiolitis in infants. J Pediatr 2007;151(3):266-
70.
Conflict of Interest: None 10. Kuzik BA, Flavin MP, Kent S, et al. Effect of inhaled
hypertonic saline on hospital admission rate in
children with viral bronchiolitis: a randomized trial.
CJEM 2010;12(6):477-84.
11. Corneli HM, Zorc JJ, Mahajan P, et al. A multicenter,
randomized, controlled trial of dexamethasone for
References bronchiolitis. N Engl J Med 2007;357(26):331-9.
12. Heydarian F, Behmanesh F, Daluee M, et al. The role
1. Bar A, Srugo I, Amirav I, et al. Inhaled furosemide in of zinc sulfate in acute bronchiolitis in patients aged
hospitalized infants with viral bronchiolitis: a 2 to 23 months. Iran J Pediatr 2012;22(1):231-4.
randomized, double-blind placebo-controlled pilot
study. Pediatr Pulmonol 2008;43(3):261–7. 13. Mathew JL. What works in bronchiolitis? Indian
Pediatrics 2009;46(2):154-8.
2. Livni G, Rachmel A, Marom D, et al. A randomized,
double-blind study examining the comparative 14. Corboz MR, Rivelli MA, Mingo GG, et al. Mechanism
efficacies and safety of inhaled epinephrine and of decongestant activity of alpha2-adrenoceptor
nasal decongestant in hospitalized infants with agonists. Pulm Pharmacol Therap 2008;21(3):449–
acute bronchiolitis. Pediatr Infect Dis J 2010;29(1): 54.
71-3. 15. Sur DK, Scandale S. Treatment of allergic rhinitis. SA
3. Sethi GR, Nagar G. Evidence based treatment of Fam Pract 2010;52(5):398-403.
bronchiolitis. Indian J Pediatr 2004;71(8):733-7. 16. Clover RD. Clinical Practice Guideline for
4. Ralston Sh, Roohi M. A randomized, controlled trial Bronchiolitis: Key Recommendations. Am Fam
of nasal phenylephrine in infants hospitalized for Physician 2007;75(2):171.
bronchiolitis. J Pediatr 2008;153(6):795-8. 17. American Academy of Pediatrics Subcommittee on
5. Wainwright C, Altamirano L, Cirujuno M. A Diagnosis and Management of Bronchiolitis:
multicenter, randomized, double-blind, controlled Diagnosis and management of bronchiolitis.
trial of nebulized epinephrine in infant with acute Pediatrics 2006;118(4):1774–93.
bronchiolitis. N Engl J Med 2003;349:27-35. 18. Zorc JJ, Hall CB. Bronchiolitis: recent evidence on
6. Numa HA, Williams GD, Dakin CJ. The effect of diagnosis and management. Pediatrics 2010;125(2):
nebulized epinephrine on respiratory mechanics 342-50.
19. Quinn T. Bronchiolitis. Innov Ai T 2011;4(7):379-84.
Iran J Pediatr; Vol 24 (No 5), Oct 2014
Published by: Tehran University of Medical Sciences (http://ijp.tums.ac.ir)
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Castration in The Horse: by Christina Cable, DVM, Dipl. ACVSДокумент5 страницCastration in The Horse: by Christina Cable, DVM, Dipl. ACVSRavi KangОценок пока нет
- Absorption and Fluoresence Spectra of Methyl Salicylate in The Vapor PhaseДокумент7 страницAbsorption and Fluoresence Spectra of Methyl Salicylate in The Vapor PhaseAriОценок пока нет
- Essential Oils in The Treatment of Respiratory Tract Diseases Highlighting Their Role in Bacterial Infections and Their Anti-Inflammatory Action: A ReviewДокумент11 страницEssential Oils in The Treatment of Respiratory Tract Diseases Highlighting Their Role in Bacterial Infections and Their Anti-Inflammatory Action: A ReviewAri100% (2)
- Clonidine HydrochlorideДокумент1 страницаClonidine HydrochlorideLovelyn Joy Abubo CortezОценок пока нет
- Incivility and Bullying PDFДокумент10 страницIncivility and Bullying PDFAndre GunawanОценок пока нет
- Density of The Alveolar and Basal Bones of TheДокумент8 страницDensity of The Alveolar and Basal Bones of Theucsurortodoncia100% (1)
- Mitral Stenosis PresentationДокумент84 страницыMitral Stenosis PresentationStawan Chougule100% (2)
- Annotated Bibliography FormatДокумент2 страницыAnnotated Bibliography FormatJohn TerryОценок пока нет
- Internal MedicineДокумент190 страницInternal MedicineNisreen Al-shareОценок пока нет
- PROCTOSIGMOIDOSДокумент5 страницPROCTOSIGMOIDOSJopet Llanita0% (1)
- The Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in OrthodonticsДокумент53 страницыThe Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in Orthodonticsdruzair007Оценок пока нет
- Club FootДокумент47 страницClub FootSujanaОценок пока нет
- Additional Motivation Letter v2Документ3 страницыAdditional Motivation Letter v2Laila Aceh100% (1)
- DodompemperidoneДокумент8 страницDodompemperidonetiwОценок пока нет
- Depression in Amyotrophic Lateral SclerosisДокумент8 страницDepression in Amyotrophic Lateral SclerosisAriОценок пока нет
- Inhaled Salbutamol Plus Ipratropium in Moderate and Severe AsthmaДокумент6 страницInhaled Salbutamol Plus Ipratropium in Moderate and Severe AsthmaAriОценок пока нет
- Sensitization Predicts Asthma Development Among Wheezing Toddlers in Secondary HealthcareДокумент8 страницSensitization Predicts Asthma Development Among Wheezing Toddlers in Secondary HealthcareAriОценок пока нет
- Daftar Isi PulmoДокумент5 страницDaftar Isi PulmoAriОценок пока нет
- Chronic Diarrhea Diagnosis and ManagementДокумент15 страницChronic Diarrhea Diagnosis and ManagementNicolas BustamanteОценок пока нет
- JpedsДокумент7 страницJpedsAriОценок пока нет
- Clinical Effectiveness and Safety of Montelukast in AsthmaДокумент12 страницClinical Effectiveness and Safety of Montelukast in AsthmaAriОценок пока нет
- Anemia: Dr. Saranya VinothДокумент45 страницAnemia: Dr. Saranya Vinothareeb khanОценок пока нет
- Intermittent Montelukast in Children Aged 10 Months To 5 Years With WheezeДокумент8 страницIntermittent Montelukast in Children Aged 10 Months To 5 Years With WheezeAriОценок пока нет
- Montelukast For Toddler AsthmaДокумент8 страницMontelukast For Toddler AsthmaAriОценок пока нет
- Meta-Analysis of The Efficacy of A Single Dose of Phenylephrine 10mg Compared With Placebo in Adults With Acute Nasal Congestion Due To The Common ColdДокумент14 страницMeta-Analysis of The Efficacy of A Single Dose of Phenylephrine 10mg Compared With Placebo in Adults With Acute Nasal Congestion Due To The Common ColdAriОценок пока нет
- Anemia Anak 2: Dr. BerthaДокумент35 страницAnemia Anak 2: Dr. BerthaAriОценок пока нет
- Evaluation of Step-Down Therapy From An Inhaled Steroid To Montelukast in Childhood AsthmaДокумент7 страницEvaluation of Step-Down Therapy From An Inhaled Steroid To Montelukast in Childhood AsthmaAriОценок пока нет
- Design Development and Evaluation of Oral Thin Films of Montelukast SodiumДокумент14 страницDesign Development and Evaluation of Oral Thin Films of Montelukast SodiumAriОценок пока нет
- New Efficacy of LTRAs (Montelukast Sodium)Документ3 страницыNew Efficacy of LTRAs (Montelukast Sodium)AriОценок пока нет
- 1 s2.0 S2221169115001033 Main PDFДокумент11 страниц1 s2.0 S2221169115001033 Main PDFxiuhtlaltzinОценок пока нет
- Bmri2014 606021Документ11 страницBmri2014 606021AriОценок пока нет
- AromaSciCh07 2Документ18 страницAromaSciCh07 2Ánh Nguyễn ThịОценок пока нет
- Are One or Two Dangerous? Methyl Salicylate ExposureДокумент7 страницAre One or Two Dangerous? Methyl Salicylate ExposureAriОценок пока нет
- Cold and Flu: Conventional Vs Botanical & Nutritional Therapy PDFДокумент14 страницCold and Flu: Conventional Vs Botanical & Nutritional Therapy PDFAriОценок пока нет
- Camphor: Risks and Benefits of A Widely Used Natural ProductДокумент6 страницCamphor: Risks and Benefits of A Widely Used Natural ProductAriОценок пока нет
- Use of Oral Gentamicin, Metronidazole, and Cholestyramine in The Treatment of Severe Persistent Diarrhea in InfantsДокумент7 страницUse of Oral Gentamicin, Metronidazole, and Cholestyramine in The Treatment of Severe Persistent Diarrhea in InfantsAriОценок пока нет
- A Comparative Trial of Cholestyramine and Loperamide For Acute Diarrhoea in Infants Treated As OutpatientsДокумент114 страницA Comparative Trial of Cholestyramine and Loperamide For Acute Diarrhoea in Infants Treated As OutpatientsAriОценок пока нет
- Pharmacologic Agents For Chronic DiarrheaДокумент7 страницPharmacologic Agents For Chronic DiarrheaAriОценок пока нет
- Cholestyramine Therapy For Intractable DiarrheaДокумент6 страницCholestyramine Therapy For Intractable DiarrheaAriОценок пока нет
- 12 Little Known Facts About CoffeeДокумент3 страницы12 Little Known Facts About CoffeeBulgare de SoareОценок пока нет
- DAFTAR KODE ICD 9 CM Untuk Unit Rehabilitasi Medis: By: Medical Record RS. Amanda 2015Документ5 страницDAFTAR KODE ICD 9 CM Untuk Unit Rehabilitasi Medis: By: Medical Record RS. Amanda 2015alsava shahiaОценок пока нет
- Global Idiopathic Pulmonary Fibrosis Treatment MarketДокумент3 страницыGlobal Idiopathic Pulmonary Fibrosis Treatment MarketiHealthcareAnalyst, Inc.Оценок пока нет
- Phonetic and Artic ApproachesДокумент4 страницыPhonetic and Artic ApproachesNoel VanNewkirkОценок пока нет
- Case KatarakДокумент8 страницCase KatarakLatoya ShopОценок пока нет
- Blood Clot in The BrainДокумент3 страницыBlood Clot in The BrainHarsh KananiОценок пока нет
- Carcinosinum 1Документ6 страницCarcinosinum 1Hilion FLAVIOОценок пока нет
- Dysphagya Screening PDFДокумент67 страницDysphagya Screening PDFMagaly DonosoОценок пока нет
- Understanding Virtues and Vices of The Healthcare ProviderДокумент3 страницыUnderstanding Virtues and Vices of The Healthcare ProviderChariss OdlosОценок пока нет
- Oral Station Scenario PDFДокумент3 страницыOral Station Scenario PDFlotuss45Оценок пока нет
- San Ma&no,: John Frush, and Roland FisherДокумент11 страницSan Ma&no,: John Frush, and Roland FisherAbhishek SharmaОценок пока нет
- DinamapCarescapeV100 OpsManualДокумент190 страницDinamapCarescapeV100 OpsManualbullmikeyОценок пока нет
- 01 - Activity 01Документ2 страницы01 - Activity 01Denice VicenteОценок пока нет
- RiteMED MetoprololДокумент7 страницRiteMED MetoprololAngie MandeoyaОценок пока нет
- Truncus ArteriosusДокумент4 страницыTruncus ArteriosuskemalahmadОценок пока нет
- Unicef ZincДокумент18 страницUnicef ZincTegar GemilangОценок пока нет
- LiverДокумент6 страницLiverMiguel Cuevas DolotОценок пока нет
- Angiographic ProjectionsДокумент16 страницAngiographic ProjectionsKarren_M888Оценок пока нет
- Endocrine Pathology LectureДокумент31 страницаEndocrine Pathology Lectureninja2007Оценок пока нет