Академический Документы
Профессиональный Документы
Культура Документы
CURE Trial
Загружено:
Cristina PazmiñoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
CURE Trial
Загружено:
Cristina PazmiñoАвторское право:
Доступные форматы
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
EFFECTS OF CLOPIDOGREL IN ADDITION TO ASPIRIN IN PATIENTS WITH
ACUTE CORONARY SYNDROMES WITHOUT ST-SEGMENT ELEVATION
THE CLOPIDOGREL IN UNSTABLE ANGINA TO PREVENT RECURRENT EVENTS TRIAL INVESTIGATORS*
ABSTRACT who are treated according to an invasive strategy,4,5 but
Background Despite current treatments, patients long-term oral therapy with glycoprotein IIb/IIIa
who have acute coronary syndromes without ST-seg- receptor blockers is not beneficial and may even in-
ment elevation have high rates of major vascular crease mortality.6 Similarly, continuing treatment with
events. We evaluated the efficacy and safety of the low-molecular-weight heparin beyond one week has
antiplatelet agent clopidogrel when given with aspi- not been shown to be effective.7 Although the long-
rin in such patients. term use of oral anticoagulants may be useful, no
Methods We randomly assigned 12,562 patients convincing evidence of their benefit is yet available.8
who had presented within 24 hours after the onset of Therefore, there is a need to reduce further the risk
symptoms to receive clopidogrel (300 mg immediately,
followed by 75 mg once daily) (6259 patients) or pla-
of ischemic events in a broad spectrum of patients both
cebo (6303 patients) in addition to aspirin for 3 to 12 when they first present with acute coronary syndromes
months. and in the long term.
Results The first primary outcome — a composite The thienopyridine derivatives, ticlopidine and clo-
of death from cardiovascular causes, nonfatal myocar- pidogrel, are antiplatelet agents that inhibit the plate-
dial infarction, or stroke — occurred in 9.3 percent of let aggregation induced by adenosine diphosphate,
the patients in the clopidogrel group and 11.4 percent thereby reducing ischemic events.9 Combining one of
of the patients in the placebo group (relative risk with these drugs with aspirin, which blocks the thrombox-
clopidogrel as compared with placebo, 0.80; 95 per- ane-mediated pathway, may have an additive effect. In
cent confidence interval, 0.72 to 0.90; P<0.001). The patients who are undergoing percutaneous translumi-
second primary outcome — the first primary outcome
nal coronary angioplasty (PTCA) with stenting, short-
or refractory ischemia — occurred in 16.5 percent of
the patients in the clopidogrel group and 18.8 percent term aspirin treatment plus a thienopyridine derivative
of the patients in the placebo group (relative risk, 0.86, results in a substantially lower rate of myocardial in-
P<0.001). The percentages of patients with in-hospital farction than does either aspirin alone or warfarin.10
refractory or severe ischemia, heart failure, and revas- However, the role of long-term combined therapy with
cularization procedures were also significantly lower aspirin and an antiplatelet agent in a broader group of
with clopidogrel. There were significantly more pa- patients at high risk for cardiovascular events is un-
tients with major bleeding in the clopidogrel group known. We therefore designed the Clopidogrel in Un-
than in the placebo group (3.7 percent vs. 2.7 percent; stable Angina to Prevent Recurrent Events (CURE)
relative risk, 1.38; P=0.001), but there were not signif- trial to compare the efficacy and safety of the early and
icantly more patients with episodes of life-threatening
long-term use of clopidogrel plus aspirin with those
bleeding (2.1 percent vs. 1.8 percent, P=0.13) or hem-
orrhagic strokes. of aspirin alone in patients with acute coronary syn-
Conclusions The antiplatelet agent clopidogrel has dromes and no ST-segment elevation.
beneficial effects in patients with acute coronary syn- METHODS
dromes without ST-segment elevation. However, the
risk of major bleeding is increased among patients Study Design
treated with clopidogrel. (N Engl J Med 2001;345: We undertook a randomized, double-blind, placebo-controlled
494-502.) trial comparing clopidogrel with placebo in patients who presented
Copyright © 2001 Massachusetts Medical Society. with acute coronary syndromes without ST-segment elevation. The
design and rationale of the study have been reported previously.9
Study Patients
Patients were eligible for the study if they had been hospital-
ized within 24 hours after the onset of symptoms and did not
have ST-segment elevation. Initially, patients older than 60 years
T
HROMBOSIS caused by a ruptured or
eroded atherosclerotic plaque is the usual
underlying mechanism of acute coronary The Manuscript Writing Committee (Salim Yusuf, D.Phil., F.R.C.P.C.,
syndromes.1 Aspirin and heparin reduce the Feng Zhao, M.Sc., Shamir R. Mehta, M.D., F.R.C.P.C., Susan Chrolavicius,
B.Sc., Gianni Tognoni, M.D., and Keith K. Fox, M.D., F.R.C.P.) assumes
risk of death from cardiovascular causes, new myocar- responsibility for the overall content of the manuscript. Address reprint re-
dial infarction, and recurrent ischemia,2,3 but there is quests to Dr. Yusuf at the Canadian Cardiovascular Collaboration Project
still a substantial risk of such events in both the short Office, Population Health Research Institute, McMaster University, Hamil-
ton General Hospital, 237 Barton St. E., Hamilton, ON L8L 2X2, Canada,
term and the long term. Intravenous glycoprotein or at yusufs@mcmaster.ca.
IIb/IIIa receptor blockers have been shown to reduce *The Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE)
the incidence of early events, mainly among patients trial investigators are listed in the Appendix.
494 · N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
C L O P I D O G R E L IN ADDIT ION TO ASP IRIN F OR ACUTE C ORONA RY SYND ROMES WITH OUT ST-S EGMENT ELEVATION
of age with no new electrocardiographic changes but with a history ditional interventions (such as thrombolytic therapy, cardiac cath-
of coronary artery disease were included. However, after a review of eterization, the insertion of an intraaortic balloon pump, coronary
the overall rates of events among the first 3000 patients, the steering revascularization, or transfer to a referral hospital for an invasive pro-
committee recommended that we enroll only patients who had ei- cedure) by midnight of the next calendar day. Refractory ischemia
ther electrocardiographic changes or an elevation in the serum level after discharge was defined by rehospitalization lasting at least 24
of cardiac enzymes or markers at entry. We excluded patients with hours for unstable angina, with ischemic electrocardiographic
contraindications to antithrombotic or antiplatelet therapy, those changes. Severe ischemia (in the hospital) was defined as ischemia
who were at high risk for bleeding or severe heart failure, those who that was similar to in-hospital refractory ischemia but for which no
were taking oral anticoagulants, and those who had undergone cor- urgent intervention was performed. Recurrent angina (in the hos-
onary revascularization in the previous three months or had received pital) was defined similarly, but electrocardiographic changes were
intravenous glycoprotein IIb/IIIa receptor inhibitors in the previ- not required.
ous three days. Major bleeding episodes were defined as substantially disabling
After we had obtained written informed consent, patients were bleeding, intraocular bleeding leading to the loss of vision, or bleed-
randomly assigned to either the clopidogrel group or the placebo ing necessitating the transfusion of at least 2 units of blood. Major
group by a central, 24-hour, computerized randomization service. bleeding was classified as life-threatening if the bleeding episode
Permuted-block randomization, stratified according to clinical cen- was fatal or led to a reduction in the hemoglobin level of at least
ter, was used. A loading dose of clopidogrel (300 mg orally) or 5 g per deciliter or to substantial hypotension requiring the use of
matching placebo was administered immediately, followed by clo- intravenous inotropic agents, if it necessitated a surgical interven-
pidogrel (75 mg per day) or matching placebo for 3 to 12 months tion, if it was a symptomatic intracranial hemorrhage, or if it neces-
(mean duration of treatment, 9 months). Aspirin (recommended sitated the transfusion of 4 or more units of blood. Minor bleeding
dose, 75 to 325 mg daily) was started or continued simultaneously episodes included other hemorrhages that led to the interruption
with the study drug. Follow-up assessments occurred at discharge, of the study medication.
at one and three months, and then every three months until the
end of the study. Statistical Analysis
The study was initially designed to include 9000 patients, with
Study Organization an expected rate of events in the placebo group of 12 to 14 percent.
Patients were recruited between December 1998 and Septem- However, because the rate of events appeared to be lower than had
ber 2000 at 482 centers in 28 countries. The ethics review board originally been expected, the size of the study was increased. As-
at each institution approved the study. The study was organized and suming a rate of 10 percent in the placebo group for the first pri-
coordinated and all the data were managed and analyzed by the mary outcome and a two-sided alpha level of 0.045, a study with
Canadian Cardiovascular Collaboration Project Office, McMaster 12,500 patients would have 90 percent power to detect a 16.9 per-
University, Hamilton, Ontario. A steering committee consisting of cent reduction in risk. For the second primary outcome, assuming
national coordinators oversaw the study. The data were periodically a 14 percent rate of events in the placebo group and a two-sided
reviewed by an independent data and safety monitoring board. alpha level of 0.01, the study had 90 percent power to detect a
reduction of 16.4 percent in risk. Partitioning the alpha maintains
Outcomes an overall level of 0.05, after adjustment for the overlap between
The first primary outcome was the composite of death from the two sets of outcomes. All analyses were based on the inten-
cardiovascular causes, nonfatal myocardial infarction, or stroke, and tion-to-treat principle and used either the log-rank statistic or the
the second primary outcome was the composite of the first primary chi-square test. Subgroup analyses were conducted with the use
outcome or refractory ischemia. The secondary outcomes were se- of tests for interactions in the Cox regression model.
vere ischemia, heart failure, and the need for revascularization. The The data and safety monitoring board monitored the incidence
safety-related outcomes were bleeding complications, which were of the primary outcome to determine the benefit of clopidogrel,
categorized as life-threatening, major (requiring the transfusion of using a modified Haybittle–Peto boundary of 4 SD in the first
2 or more units of blood), or minor. All primary outcomes and half of the study and 3 SD in the second half of the study. The
life-threatening and major bleeding complications were adjudicated boundary had to be exceeded at two or more consecutive time
by persons who were unaware of the patients’ treatment-group points, at least three months apart, for the board to consider ter-
assignments. minating the study early. There were two formal interim assess-
ments performed at the times when approximately one third and
Definitions two thirds of the expected events had occurred. Despite the fact
that the preset boundary indicating efficacy had been crossed by
Death from cardiovascular causes was defined as any death for the time of the second interim analysis, the board recommended
which there was no clearly documented nonvascular cause. Myocar- that the trial continue until its planned end, in order to define
dial infarction was defined by the presence of at least two of the more clearly whether the risks of major bleeding episodes could
following: ischemic chest pain; the elevation of the serum levels offset the benefits of therapy.
of cardiac markers or enzymes (troponin, creatine kinase, creatine All unrefuted events that occurred up to the end of the sched-
kinase MB isoenzyme, or other cardiac enzymes) to at least twice uled follow-up period on December 6, 2000, are included in the
the upper limit of the normal reference range or three times the up- analyses. Vital status was ascertained for 12,549 of the 12,562 pa-
per limit of normal within 48 hours after percutaneous coronary tients who underwent randomization (99.9 percent), with 6 patients
intervention (or to a level 20 percent higher than the previous val- in the clopidogrel group and 7 in the placebo group lost to fol-
ue if the level had already been elevated because of an early myo- low-up.
cardial infarction); and electrocardiographic changes compatible
with infarction.9 Stroke was defined as a new focal neurologic def- RESULTS
icit of vascular origin lasting more than 24 hours. Stroke was fur-
ther classified as the result of intracranial hemorrhage, ischemia (if The base-line characteristics of the patients are
a computed tomographic or magnetic resonance imaging scan was shown in Table 1.
available), or uncertain cause.
Refractory ischemia in the hospital was defined as recurrent chest Primary Outcomes
pain lasting more than five minutes with new ischemic electrocar-
diographic changes while the patient was receiving optimal med-
The first primary outcome — death from cardiovas-
ical therapy (two antianginal agents, one of which was intravenous cular causes, nonfatal myocardial infarction, or stroke
nitrate unless such therapy was contraindicated) and leading to ad- — occurred in 582 of the 6259 patients in the clo-
N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org · 495
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
pidogrel group (9.3 percent) as compared with 719
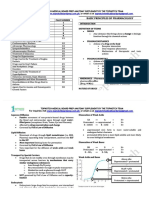
of the 6303 patients in the placebo group (11.4 per- TABLE 1. BASE-LINE DEMOGRAPHIC CHARACTERISTICS,
MEDICAL HISTORY, ELECTROCARDIOGRAPHIC CHANGES,
cent); relative risk, 0.80; 95 percent confidence inter- AND DRUG THERAPY.*
val, 0.72 to 0.90; P<0.001) (Fig. 1 and 2 and Table
2). The rate of the second primary outcome — death
from cardiovascular causes, nonfatal myocardial infarc- CLOPIDOGREL PLACEBO
GROUP GROUP
tion, stroke, or refractory ischemia — was also higher CHARACTERISTIC (N=6259) (N=6303)
in the placebo group (1187 patients [18.8 percent])
Age — yr 64.2±11.3 64.2±11.3
than in the clopidogrel group (1035 patients [16.5 Female sex — no. (%) 2420 (38.7) 2416 (38.3)
percent]; relative risk, 0.86; 95 percent confidence Time from onset of pain to ran- 14.2±7.2 14.1±7.1
interval, 0.79 to 0.94; P<0.001). The rate of each domization — hr
component of these composite outcomes also tended Heart rate — beats/min 73.2±14.8 73.0±14.6
to be lower in the clopidogrel group. However, the Systolic blood pressure — mm Hg 134.4±22.5 134.1±22.0
clearest difference was observed in the rates of myo- Diagnosis at study entry — no. (%)
Unstable angina 4690 (74.9) 4724 (74.9)
cardial infarction (Table 2). With respect to refractory Suspected myocardial infarction 1569 (25.1) 1579 (25.1)
ischemia, the difference was observed primarily in first Associated myocardial infarction 1624 (25.9) 1659 (26.3)
events that occurred during the initial hospitalization — no. (%)†
(85 in the clopidogrel group as compared with 126 Medical history — no. (%)
Myocardial infarction 2029 (32.4) 2015 (32.0)
in the placebo group; relative risk, 0.68; 95 percent CABG or PTCA 1107 (17.7) 1139 (18.1)
confidence interval, 0.52 to 0.90; P=0.007), with lit- Stroke 274 (4.4) 232 (3.7)
tle difference in the rate of rehospitalization for unsta- Heart failure 462 (7.4) 492 (7.8)
Hypertension 3750 (59.9) 3642 (57.8)
ble angina. Diabetes 1405 (22.4) 1435 (22.8)
Current or former smoker 3790 (60.6) 3841 (60.9)
Other In-Hospital Outcomes Electrocardiographic abnormality
— no. (%)‡
Significantly fewer patients in the clopidogrel group Any 5863 (93.7) 5921 (93.9)
than in the placebo group had severe ischemia (176 ST segment
patients [2.8 percent] vs. 237 patients [3.8 percent]; Depression »1 mm 2642 (42.2) 2646 (42.0)
Elevation «1 mm 203 (3.2) 199 (3.2)
relative risk, 0.74; 95 percent confidence interval, 0.61 Transient elevation >2 mm 38 (0.6) 37 (0.6)
to 0.90; P=0.003) or recurrent angina (1307 [20.9 T-wave inversion
Major (»2 mm) 1589 (25.4) 1635 (25.9)
percent] vs. 1442 [22.9 percent]; relative risk, 0.91; Other (<2 mm) 721 (11.5) 713 (11.3)
95 percent confidence interval, 0.85 to 0.98; P=0.01) Other 670 (10.7) 690 (10.9)
(Fig. 3). Slightly fewer patients in the clopidogrel Medications at time of randomiza-
group underwent coronary revascularization during tion — no. (%)
Aspirin 4168 (66.6) 4134 (65.6)
the study (36.0 percent vs. 36.9 percent), but the dif- Heparin or LMW heparin 4522 (72.3) 4605 (73.1)
ference was accounted for entirely by a difference in ACE inhibitor 2347 (37.5) 2309 (36.6)
Beta-blocker 3678 (58.8) 3690 (58.5)
the rate of revascularization during the initial period Calcium-channel blocker 1784 (28.5) 1771 (28.1)
of hospitalization (20.8 percent in the clopidogrel Lipid-lowering agent 1599 (25.6) 1586 (25.2)
group vs. 22.7 percent in the placebo group, P=0.03). Intravenous nitrate 2836 (45.3) 2906 (46.1)
Radiologic evidence of heart failure was found in few- *Plus–minus values are means ±SD. CABG denotes coronary-artery by-
er patients in the clopidogrel group (229 [3.7 per- pass grafting, PTCA percutaneous transluminal coronary angioplasty, LMW
cent], vs. 280 [4.4 percent] in the placebo group; rel- low molecular weight, and ACE angiotensin-converting enzyme.
ative risk, 0.82; 95 percent confidence interval, 0.69 †An associated myocardial infarction was defined as a myocardial infarc-
tion associated with the episode of pain that occurred before randomization.
to 0.98; P=0.03).
‡Data on the particular type of abnormality were missing for one patient
in the placebo group.
Temporal Trends
The rate of the first primary outcome was lower
in the clopidogrel group both within the first 30 days
after randomization (relative risk, 0.79; 95 percent
confidence interval, 0.67 to 0.92) and between 30 the placebo group; relative risk, 0.66; 95 percent con-
days and the end of the study (relative risk, 0.82; 95 fidence interval, 0.51 to 0.86).
percent confidence interval, 0.70 to 0.95) (Fig. 1 and
2). Further analysis indicated that the benefit of clo- Subgroup Analyses
pidogrel was apparent within a few hours after ran- The consistency of the results in a number of key
domization, with the rate of death from cardiovascular subgroups is documented in Figure 4. The benefits
causes, nonfatal myocardial infarction, stroke, or refrac- were also consistent among subgroups receiving dif-
tory or severe ischemia significantly lower in the clo- ferent doses of aspirin and among those receiving or
pidogrel group by 24 hours after randomization (1.4 not receiving lipid-lowering drugs, beta-blockers, hep-
percent in the clopidogrel group vs. 2.1 percent in arin, or angiotensin-converting–enzyme inhibitors at
496 · N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
C L O P I D O G R E L IN ADDIT ION TO ASP IRIN F OR ACUTE C ORONA RY SYND ROMES WITH OUT ST-S EGMENT ELEVATION
0.14
0.12
Placebo
Cumulative Hazard Rate
0.10
Clopidogrel
0.08
0.06
0.04 P<0.001
0.02
0.00
0 3 6 9 12
Months of Follow-up
NO. AT RISKF F F F F F
PlaceboF 6303F 5780F 4664F 3600F 2388F
Clopidogrel 6259 5866 4779 3644 2418
Figure 1. Cumulative Hazard Rates for the First Primary Outcome (Death from Cardiovascular Causes,
Nonfatal Myocardial Infarction, or Stroke) during the 12 Months of the Study.
The results demonstrate the sustained effect of clopidogrel.
the time of randomization. There was a tendency to- 0.06
Cumulative Hazard Rate
ward a greater benefit among patients who had pre-
0.05
viously undergone revascularization (relative risk of Placebo
the first primary outcome, 0.56; 95 percent confidence 0.04
interval, 0.43 to 0.72) than among those who had Clopidogrel
0.03
not (relative risk, 0.88; 95 percent confidence interval,
0.78 to 0.99; P for interaction=0.002). However, 0.02
these results should be interpreted cautiously, given P=0.003
the large numbers of subgroup analyses that were 0.01
performed. Furthermore, consistent benefits were ob- 0.00
served irrespective of whether patients underwent re- 0 10 20 30
vascularization procedures after randomization. Days of Follow-up
Safety NO. AT RISKF F F F F
Major bleeding was significantly more common in PlaceboF 6303F 6108F 5998F 5957F
the clopidogrel group (3.7 percent in the clopidogrel Clopidogrel 6259 6103 6035 5984
group as compared with 2.7 percent in the placebo Figure 2. Cumulative Hazard Rates for the First Primary Outcome
group; relative risk, 1.38; 95 percent confidence in- (Death from Cardiovascular Causes, Nonfatal Myocardial Infarc-
terval, 1.13 to 1.67; P=0.001) (Table 3). There were tion, or Stroke) during the First 30 Days after Randomization.
135 patients with life-threatening bleeding episodes The results demonstrate the early effect of clopidogrel.
in the clopidogrel group (2.2 percent) as compared
with 112 in the placebo group (1.8 percent; relative
risk, 1.21; 95 percent confidence interval, 0.95 to
1.56). There was no excess rate of fatal bleeding, bleed-
ing requiring surgical intervention, or hemorrhagic
stroke. The excess major bleeding episodes were gas-
trointestinal hemorrhages and bleeding at the sites of
N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org · 497
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
TABLE 2. INCIDENCE OF THE MAIN STUDY OUTCOMES.*
CLOPIDOGREL PLACEBO
GROUP GROUP RELATIVE RISK
OUTCOME (N=6259) (N=6303) (95% CI) P VALUE
no. (%)
First primary outcome: nonfatal myo- 582 (9.3) 719 (11.4) 0.80 (0.72–0.90) <0.001
cardial infarction, stroke, or
death from cardiovascular
causes
Second primary outcome: first 1035 (16.5) 1187 (18.8) 0.86 (0.79–0.94) <0.001
primary outcome or
refractory ischemia
Death from cardiovascular causes 318 (5.1) 345 (5.5) 0.93 (0.79–1.08)
Myocardial infarction† 324 (5.2) 419 (6.7) 0.77 (0.67–0.89)
Q-wave 116 (1.9) 193 (3.1) 0.60 (0.48–0.76)
Non–Q-wave 216 (3.5) 242 (3.8) 0.89 (0.74–1.07)
Stroke 75 (1.2) 87 (1.4) 0.86 (0.63–1.18)
Refractory ischemia‡ 544 (8.7) 587 (9.3) 0.93 (0.82–1.04)
During initial hospitalization 85 (1.4) 126 (2.0) 0.68 (0.52–0.90)
After discharge 459 (7.6) 461 (7.6) 0.99 (0.87–1.13)
Death from noncardiovascular causes 41 (0.7) 45 (0.7) 0.91 (0.60–1.39)
*The number of patients who died from cardiovascular causes or had a nonfatal myocardial infarc-
tion was 539 (8.6 percent) in the clopidogrel group and 660 (10.5 percent) in the placebo group
(P<0.001; relative risk, 0.81; 95 percent confidence interval, 0.72 to 0.91). The corresponding num-
bers at 30 days were 241 (3.9 percent) and 305 (4.8 percent) (relative risk, 0.79; 95 percent confi-
dence interval, 0.67 to 0.94; P=0.007). CI denotes confidence interval.
†Some patients had both a Q-wave and a non–Q-wave myocardial infarction.
‡Only the first ischemic event was counted for each patient.
arterial punctures. The number of patients who re- P=0.06). Overall, the risk of minor bleeding was
quired the transfusion of 2 or more units of blood was significantly higher in the clopidogrel group than in
higher in the clopidogrel group (177 [2.8 percent]) the placebo group (322 [5.1 percent] vs. 153 [2.4
than in the placebo group (137 [2.2 percent], P= percent]; P<0.001). The numbers of patients with
0.02). The rate of major bleeding episodes was higher thrombocytopenia (28 in the placebo group and 26
early (within 30 days after randomization: 2.0 percent in the clopidogrel group) or neutropenia (5 and 8,
vs. 1.5 percent; relative risk, 1.31; 95 percent confi- respectively) were similar.
dence interval, 1.01 to 1.70) and also late (more than
Adherence to Study Medication and Aspirin
30 days after randomization: 1.7 percent vs. 1.1 per-
cent; relative risk, 1.48; 95 percent confidence interval, A total of 46.2 percent of the patients in the clopid-
1.10 to 1.99). Overall, there was no significant excess ogrel group discontinued the study medication tem-
of major bleeding episodes after coronary-artery by- porarily (for more than five days), as compared with
pass grafting (CABG) (1.3 percent vs. 1.1 percent; rel- 45.4 percent in the placebo group. The most common
ative risk, 1.26; 95 percent confidence interval, 0.93 to reason for the temporary discontinuation of the study
1.71). However, in most patients scheduled for CABG medication was the need for revascularization or an-
surgery, the study medication was discontinued be- other surgical procedure; 84 percent of the patients
fore the procedure (median time before the procedure, with such a need discontinued the medication before
five days). In the 910 patients in whom the study med- the procedure. A total of 21.1 percent of the patients
ication was discontinued more than five days before in the clopidogrel group discontinued the study med-
the procedure (five days being the duration of the ef- ication permanently, as compared with 18.8 percent
fect of clopidogrel), there was no apparent excess of in the placebo group. A total of 99 percent of the pa-
major bleeding within seven days after surgery (4.4 tients in both groups were taking aspirin while they
percent of the patients in the clopidogrel group vs. were in the hospital, 96 percent were taking it at three
5.3 percent of those in the placebo group). In the 912 months, and 94 percent at the final visit. The use of
patients who stopped taking the medications within all other medications (other than thrombolytic ther-
five days before CABG surgery, the rate of major apy and glycoprotein IIb/IIIa receptor inhibitors)
bleeding was 9.6 percent in the clopidogrel group and was similar in the clopidogrel group and the placebo
6.3 percent in the placebo group (relative risk, 1.53; group.
498 · N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
C L O P I D O G R E L IN ADDIT ION TO ASP IRIN F OR ACUTE C ORONA RY SYND ROMES WITH OUT ST-S EGMENT ELEVATION
1442F 1307F 1431F 1302F
(22.9%) (20.9%) (22.7%) (20.8%)
25
RR=0.91F RR=0.92F
P=0.01 P=0.03
20
PlaceboF
Patients with Outcome (%)
Clopidogrel
15
10
280F 229F
237F 176F (4.4%) (3.7%)
(3.8%) (2.8%)
RR=0.82F
126F 85F RR=0.74F
5 P=0.026
(2.0%) (1.4%) P=0.003
RR=0.68F
P=0.007
0
RefractoryŁ Other severeŁ Other recurrentŁ RevascularizationŁ HeartŁ
ischemia ischemia angina procedure failure
Other In-Hospital Outcomes
Figure 3. Proportions of Patients Who Had Events Other Than Those Included in the First Primary Outcome while They
Were in the Hospital.
The numbers and percentages of patients in each group with the specified outcome are given above the bars. RR de-
notes relative risk.
Thrombolytic Therapy and Glycoprotein IIb/IIIa coprotein IIb/IIIa receptor inhibitor. The benefits we
Receptor Inhibitors observed were in addition to those of aspirin, which
A total of 71 patients in the clopidogrel group (1.1 was recommended for all patients, indicating that
percent) and 126 patients in the placebo group (2.0 blocking the adenosine diphosphate–receptor path-
percent) received thrombolytic therapy (relative risk, way with clopidogrel leads to further benefit.
0.57; 95 percent confidence interval, 0.43 to 0.76; Our study primarily included centers in which there
P<0.001); 369 patients in the clopidogrel group (5.9 was no routine policy of early use of invasive proce-
percent) and 454 in the placebo group (7.2 percent) dures, since such a policy would have led to a high rate
received a glycoprotein IIb/IIIa receptor inhibitor of immediate discontinuation of the study medication
(relative risk, 0.82; 95 percent confidence interval, and the use of an open-label thienopyridine derivative.
0.72 to 0.93; P=0.003). Once a patient had been randomly assigned to a treat-
ment group, there were no restrictions on the use of
DISCUSSION any therapy or intervention. In particular, if the clini-
Our study demonstrates the benefit of adding clo- cian believed that angiography and revascularization
pidogrel to the regimen of treatment for patients with were needed or that a thienopyridine derivative was
acute coronary syndromes without ST-segment eleva- indicated, the study medication could be stopped or
tion who are receiving aspirin and other medications. open-label clopidogrel or ticlopidine could be used.
Treatment with clopidogrel reduced the risk of myo- In fact, 5491 patients (43.7 percent) underwent an-
cardial infarction and recurrent ischemia, with a trend giography, 2072 patients (16.5 percent) underwent
toward lower rates of stroke and death from cardiovas- CABG, and 2658 patients (21.2 percent) underwent
cular causes. Fewer patients in the clopidogrel group PTCA. In 85.8 percent of the patients who under-
received a thrombolytic agent or an intravenous gly- went PTCA and 84.9 percent of those who underwent
N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org · 499
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
No. ofŁ Percentage ofŁ
Characteristic Patients Patients with Event
Placebo Clopidogrel
OverallF 125620F 11.4F 09.3F
F F F
Associated MIF 3283F 13.7F 11.3F
No associated MIF 9279F 10.6F 08.6F
F F F
Male sexF 7726F 11.9F 09.1F
Female sexF 4836F 10.7F 09.5F
F F F
«65 yr oldF 6354F 07.6F 05.4F
>65 yr oldF 6208F 15.3F 13.3F
F F F
ST-segment deviationF 6275F 14.3F 11.5F
No ST-segment deviationF 6287F 08.6F 07.0F
F F F
Enzymes elevated at entryF 3176F 13.0F 10.7F
Enzymes not elevated at entryF 9386F 10.9F 08.8F
F F F
DiabetesF 2840F 16.7F 14.2F
No diabetesF 9722F 09.9F 07.9F
F F F
Low riskF 4187F 06.7F 05.1F
Intermediate riskF 4185F 09.4F 06.5F
High riskF 4184F 18.0F 16.3F
F F F
History of revascularizationF 2246F 14.4F 08.4F
No history of revascularizationF 103160F 10.7F 09.5F
F F F
Revascularization after randomizationF 4577F 13.9F 11.5F
No revascularization after randomization 7985 10.0 08.1F
F
F
0.4 0.6 0.8 1.0 1.2
Clopidogrel better Placebo better
Relative Risk (95% CI)
Figure 4. The Rates and Relative Risks of the First Primary Outcome (Death from Cardiovascular Causes, Nonfatal Myocardial In-
farction, or Stroke) in Various Subgroups.
The data show the consistency of the benefit of clopidogrel. The dotted line represents the average treatment effect. The size of
each box is proportional to the number of patients in the individual analysis. An associated myocardial infarction (MI) was defined
as a myocardial infarction associated with the episode of pain that occurred before randomization. Because of missing data, six
patients could not be classified in a risk category. CI denotes confidence interval.
CABG, the use of the study medication was tempo- selective and short-term use among those undergoing
rarily interrupted for more than five days, and the implantation of a coronary stent.
vast majority of the patients who underwent PTCA Clopidogrel prevented a range of ischemic coronary
received a thienopyridine-type antiplatelet agent for events — among them, myocardial infarction and se-
about two to four weeks. In the patients who under- vere and refractory ischemia. Clopidogrel was associ-
went CABG, the study medication was restarted after ated with a trend toward fewer ischemic strokes, and
a median of 11 days. Although these interruptions of there was no increase in the rate of hemorrhagic stroke
therapy with the study medication would tend to re- that would offset these benefits. There was a significant
sult in an underestimate of the difference between the reduction in the incidence of heart failure with clo-
clopidogrel group and the placebo group, they also pidogrel that was of about the same magnitude as the
permit us to make useful estimates of the benefits and reduction in the incidence of ischemic events, suggest-
risks of clopidogrel when it is used routinely and over ing that the reduction of ischemia can prevent heart
the long term, as compared with a strategy of more failure. The benefits of clopidogrel were observed in
500 · N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
C L O P I D O G R E L IN ADDIT ION TO ASP IRIN F OR ACUTE C ORONA RY SYND ROMES WITH OUT ST-S EGMENT ELEVATION
TABLE 3. BLEEDING COMPLICATIONS.*
CLOPIDOGREL PLACEBO
GROUP GROUP RELATIVE RISK
VARIABLE (N=6259) (N=6303) (95% CI) P VALUE
no. (%)
Major bleeding 231 (3.7) 169 (2.7) 1.38 (1.13–1.67) 0.001
Necessitating transfusion of »2 units 177 (2.8) 137 (2.2) 1.30 (1.04–1.62) 0.02
of blood
Life-threatening 135 (2.2) 112 (1.8) 1.21 (0.95–1.56) 0.13
Fatal 11 (0.2) 15 (0.2)
Causing 5 g/dl drop in hemoglobin 58 (0.9) 57 (0.9)
level
Requiring surgical intervention 45 (0.7) 43 (0.7)
Causing hemorrhagic stroke 7 (0.1) 5 (0.1)
Requiring inotropic agents 34 (0.5) 34 (0.5)
Necessitating transfusion of »4 units 74 (1.2) 60 (1.0)
of blood
Non–life-threatening 96 (1.5) 57 (0.9) 1.70 (1.22–2.35) 0.002
Site of major bleeding
Gastrointestinal 83 (1.3) 47 (0.7)
Retroperitoneal 8 (0.1) 5 (0.1)
Urinary (hematuria) 4 (0.1) 5 (0.1)
Arterial puncture site 36 (0.6) 22 (0.3)
Surgical site 56 (0.9) 53 (0.8)
Minor bleeding 322 (5.1) 153 (2.4) 2.12 (1.75–2.56) <0.001
Total with bleeding complications 533 (8.5) 317 (5.0) 1.69 (1.48–1.94) <0.001
*The number of patients with bleeding that met the criteria for major bleeding established by the
Thrombolysis in Myocardial Infarction trial11 was 68 in the clopidogrel group and 73 in the placebo
group (relative risk, 0.94; 95 percent confidence interval, 0.68 to 1.30; P=0.70). The number with
bleeding that met the criteria for life-threatening or severe bleeding established by the Global Utilization
of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries trial12 was 78 in the
clopidogrel group and 70 in the placebo group (relative risk, 1.12; 95 percent confidence interval, 0.81
to 1.55; P=0.48). Some patients had more than one bleeding episode. CI denotes confidence interval.
a range of patients, including both patients who were pidogrel was not associated with an excess rate of any
undergoing revascularization procedures and those other type of adverse event that necessitated the dis-
who were not. The benefits were also observed in continuation of the study drug; this finding indicates
those at low, medium, and high risk of cardiovascular that the combination of clopidogrel and aspirin is as
events and those who were receiving various proven well tolerated as aspirin alone.
therapies such as aspirin, lipid-lowering drugs, an- In summary, clopidogrel significantly reduces the
giotensin-converting–enzyme inhibitors, and beta- risk of the composite outcome of death from cardio-
blockers.13-16 The benefits of clopidogrel were appar- vascular causes, nonfatal myocardial infarction, or
ent as early as the first 24 hours after randomization, stroke, as well as a range of related ischemic events.
indicating that the oral loading dose was rapidly ef- The use of the drug, in addition to aspirin, is asso-
fective. Thereafter, the differences between the two ciated with an increased risk of bleeding.
groups were maintained until the end of the study.
Clopidogrel increased the risk of minor and major Supported by Sanofi-Synthelabo and Bristol-Myers Squibb. Dr. Yusuf is
bleeding episodes. For every 1000 patients treated the recipient of a Senior Scientist award from the Canadian Institutes of
with clopidogrel, 6 will require a transfusion. However, Health Research and holds an endowed chair from the Heart and Stroke
Foundation of Ontario. Dr. Mehta is a research fellow of the Heart and
there was no excess in bleeding that caused strokes, Stroke Foundation of Canada.
required surgical intervention or inotropic agents, or Drs. Yusuf, Mehta, Tognoni, and Fox have received honorariums for ed-
caused permanent disability. Furthermore, the excess ucational activities or have served as consultants to Bristol-Myers Squibb
and Sanofi-Synthelabo.
risk of bleeding we observed is similar to that observed
with aspirin alone, as compared with a control, in pre- We are indebted to Judy Lindeman for secretarial assistance.
vious studies and lower than that observed in most
trials of the short-term intravenous use or the pro- APPENDIX
longed oral use of glycoprotein IIb/IIIa receptor in-
hibitors.4,16,17 The risk of bleeding may have been part- The following persons participated in the CURE trial: Steering Com-
mittee: S. Yusuf (chair and principal investigator), K.A.A. Fox (cochair),
ly mitigated by the temporary discontinuation of the G. Tognoni (cochair), S.R. Mehta (project officer), S. Chrolavicius (study
study medication before surgery. Treatment with clo- coordinator), S. Anand, A. Avezum, N. Awan, M. Bertrand, A. Budaj, L.
N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org · 501
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Ceremuzynski, J. Col, P.J. Commerford, R. Diaz, M. Flather, M.-G. Fran- no, R. Ferreira, M. Veloso Gomes; South Africa (308) — A. Aboo, L.
zosi, B. Gersh, W. Grossman, D.A. Halon, D. Hunt, C. Joyner (chair of Bobak, B. Brown, S. Cassim, S. Harripersadh, P. Manga, F. Maritz, J. Marx,
the Events Adjudication Committee), N. Karatzas, M. Keltai, S. Kopecky, D. Myburgh, H. Nell, A. Okreglicki, H. Theron; Spain (330) — N. Alonso
B.S. Lewis, A. Maggioni, K. Malmberg, T. Moccetti, J. Morais, M. Nat- Orcajo, F. Colomina, I. Echanove, J. Garcia Guerrero, E. Gomez-Martinez,
arajan, E. Paolasso, R. Peters, L. Piegas, A. Pipilis, J. Pogue, M. Ramos- I. Lekuona, L. Miralles, C. Pasaval, A. Rovira, J. San Jose, A. Rodriguez
Corrales, H.-J. Rupprecht, E. Sitkei, V. Valentin, J. Varigos, P. Widimsky, Llorian, V. Valentin; Sweden (260) — N. Abdon, B. Bartholdson, E. Basilier,
T. Wittlinger, M. Blumenthal, J. Bouthier, C. Gaudin, T. Hess, N. Khurmi, I. Johansson, B. Kristensson, K. Larsson, P. Lindell, B. Moller, G. Ras-
M. Sotty; Canadian Cardiovascular Collaboration (CCC) Project Of- manis, A. Stjerna, K. Tolhagen; Switzerland (225) — B. Caduff, G. Noseda,
fice: I. Copland, B. Cracknell, C. Demers, J. Eikelboom, B. Morris, J. Pas- A. Rossi, D. Schmidt, J. Zerega; United States (462) — K. Carr, R. Detrano,
quale, V. Yacyshyn, F. Zhao; Data Safety and Monitoring Board: G. R. Geer, G. Grewal, P. Hermany, N. Lakkis, W.R. Lewis, T.R. Pacheco, G.
Wyse (chair), J. Cairns, R. Hart, J. Hirsh, M. Gent, T. Ryan, J. Wittes; In- Papuchis, J. Puma, S. Runckey, U. Thadani, J. Whitaker; United Kingdom
vestigators who recruited more than 10 patients (the numbers of pa- (737) — Y.J.A. Adgey, D. Blackman, M. Brack, A. Bridges, A. Cohen, P.
tients appear in parentheses): Argentina (512) — R. Ahuad Guerrero, V. Currie, S. Duffy, I. Findlay, J. Goodfellow, K. Gray, D. Hogg, D. Holdright,
Arias, F.H. Bello, J.O. Bono, L. Bujan, A. Caccavo, A.A. Fernandez, J.J. D. Hughes, N. Irvine, K. Jennings, P. Keeling, P. Ludman, T. Mathew, P.
Fuselli, A.J. Gambarte, E.G. Hasbani, E. Marzetti, G. Mon, R. Nordaby, McIntyre, R. Oliver, N. Palmer, E. Rodrigues, L. Smyth, D. Sprigings, J.
G. Quijano, A. Salvati, E. San Martin, P. Schygiel, A. Sosa Liprandi, H. Stephens, A. Timmis, R. Vincent.
Torre, E. Tuero; Australia (742) — J. Amerena, J.H.N. Bett, J. Botha, A.
Buncle, D. Careless, A. Ewart, A. Fagan, D. Fitzpatrick, P. Garrahy, K. REFERENCES
Gunawardane, A. Hamer, A. Hill, N. Jepson, G. Lane, H. LeGood, G. Nel-
son, M. Sallaberger, G. Tulloch, D. Owensby, J. Padley, D. Rees, K. Rob- 1. Yeghiazarians Y, Braunstein JB, Askari A, Stone PH. Unstable angina
erts, D. Rosen, J. Sampson, B. Singh, C. Singh, R. Taylor, A. Thomson, pectoris. N Engl J Med 2000;342:101-14.
W. Walsh; Austria (5); Belgium (38) — H. De Raedt, J. Rankin; Brazil 2. Antiplatelet Trialists’ Collaboration. Collaborative overview of random-
(598) — J.A. Abrantes, D.C. de Albuquerque, C. Blacher, L.C. Bodanese, ised trials of antiplatelet therapy. I. Prevention of death, myocardial infarc-
A.C. Carvalho, M. Coutinho, O. Dutra, J.P. Esteves, P. Leães, N.S. Lima, tion, and stroke by prolonged antiplatelet therapy in various categories of
N. Lobo, J.A. Marin Neto, R.L. Marino, J.C. Nicolau, R.C. Pedrosa, I. patients. BMJ 1994;308:81-106. [Erratum, BMJ 1994;308:1540.]
Pereira Filho, W. Rabelo, A. Rabelo Jr., R.F. Ramos, R.M. Rocha, E.C. 3. Low-molecular-weight heparin during instability in coronary artery dis-
Schramm, C.V. Serrano, Jr., V.P. Souza, A. Timerman, R. Vaz, S.S. Xavier; ease. Lancet 1996;347:561-8.
Canada (1761) — P. Auger, K. Barbin, I. Bata, L. Bergeron, R.K. Bharga- 4. The Platelet Receptor Inhibition in Ischemic Syndrome Management in
va, P. Bogaty, P. Bolduc, T. Boyne, L. Boyer, B. Bozek, T. Calmusky, Y.K. Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) Inves-
Chan, D. Cole, M. D’Astous, M. David, T. Davies, L. Desjardins, F.C. tigators. Inhibition of the platelet glycoprotein IIb/IIIa receptor with ti-
Dohaney, M. Doody, F. Dumont, C. Fortin, A. Fung, G. Galdreault, P.B. rofiban in unstable angina and non–Q-wave acute myocardial infarction.
Gervais, J.P. Giannoccaro, G. Gosselin, D. Grandmont, A. Grover, M. N Engl J Med 1998;338:1488-97.
Gupta, H. Hink, J.G. Hiscock, D. Hutton, J.W.H. Hynd, A. Iless, C. Kent, 5. The GUSTO IV-ACS Investigators. Effect of glycoprotein IIb/IIIa re-
A. Kitching, S. Kouz, K. Kwok, M. LaForest, H. Lee, C. Lefkowitz, B. ceptor blocker abciximab on outcome in patients with acute coronary syn-
Lubelsky, P. Ma, J.-F. Marquis, A. McCallum, R. Major, B. May, M. Mer- dromes without early coronary revascularization: the GUSTO IV-ACS ran-
cier, M. Montigny, A. Morris, S. Nawaz, J. Norris, S. Pallie, A. Panju, P. domized trial. Lancet 2001;357:1915-24.
Parekh, C. Patterson, Y. Pesant, C. Pilon, A.R.J. Rajakumar, T. Rebane, J. 6. Chew DP, Bhatt D, Sapp S, Topol EJ. Increased mortality with oral
Ricci, M. Ruel, R. Schuld, R. Starra, M. Thornley, A.S. Weeks, L.H. Wink- platelet glycoprotein IIb/IIIa antagonists: a meta-analysis of phase III mul-
ler, G. Wisenberg, I. Witt, K. Woo, E. Yu, R. Zadra, D. Zaniol; Czech ticenter randomized trials. Circulation 2001;103:201-6.
Republic (165) — P. Bocek, M. Branny, V. Cepelak, P. Gregor, L. Groch, 7. FRagmin and Fast Revascularisation during InStability in Coronary artery
P. Jansky, P. Svitil, A. Vaclavicek; Denmark (40) — S. Husted, B. Ziegler; disease (FRISC II) Investigators. Long-term low-molecular-mass heparin in
Finland (161) — A. Karhu, J. Mustonen, M. Nieminen, K. Nissinen, K. unstable coronary-artery disease: FRISC II prospective randomised multi-
Peuhkurinen, P. Tuomainen, A. Ylitalo; France (360) — M. Adam, G. Amat, centre study. Lancet 1999;354:701-7. [Erratum, Lancet 1999;354:1478.]
K. Asward, G. Bessede, P. Dambrine, E. Decoulx, B. D’Hautefeuille, J. 8. The Organization to Assess Strategies for Ischemic Syndromes (OASIS)
Dujardin, R. Fouche, P. Fournier, Y. Haftel, J.Y. Ketelers, R. Lallemant, M. Investigators. Effects of long-term, moderate-intensity oral anticoagulation
Lang, F. Leroy, M. Richard; Germany (778) — W. Dippold, J. Gronholz, in addition to aspirin in unstable angina. J Am Coll Cardiol 2001;37:475-84.
J. Harenberg, C. Hilpert, T. Horacek, A. Moritz, H. Neuss, K. Nitsche, 9. CAPRIE Steering Committee. A randomised, blinded, trial of clopido-
H.R. Ochs, M. Plumer-Schmidt, B. Pollock, G. Post, M. Sauer, A. grel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet
Schmidt, H. Schmitt, H.-O. Schulze, P. Schuster, E.-R. von Leitner; Greece 1996;348:1329-39.
(144) — S. Christakos, K. Karidis, K. Kifnidis, K. Papadopoulos, D. Sym- 10. CURE Study Investigators. The Clopidogrel in Unstable angina to
conidis, A. Tirologos; Hungary (599) — B. Garai, T. Gesztesi, K. Heltai, prevent Recurrent Events (CURE) trial programme: rationale, design and
B. Herczeg, A. Janosi, A. Kadar, E. Kalo, P. Karpati, B. Kiss, A. Nagy, M. baseline characteristics including a meta-analysis of the effects of thieno-
Okros, F. Poor, L. Regos, J. Sebo, E. Sitkei, P. Soltesz, J. Stefan, F. Szaboki, pyridines in vascular disease. Eur Heart J 2000;21:2033-41.
S. Timar, Z. Varallyay, K. Veres; Ireland (37) — K. Daly; Israel (694) — 11. Rao AK, Pratt C, Berke A, et al. Thrombolysis in Myocardial Infarc-
G. Cotter, A. Marmor, D. Nazzal, M. Omary, L. Reisin, T. Rosenfeld, M. tion (TIMI) Trial — phase I: hemorrhagic manifestations and changes in
Shargorodsky, S. Shasha, A. Smulovitz, Z. Vered, R. Zimlichman; Italy plasma fibrinogen and the fibrinolytic system in patients treated with re-
(538) — G. Beria, D. Bernardi, E. Bonfanti, V. Ceci, R. De Caterina, S. combinant tissue plasminogen activator and streptokinase. J Am Coll Car-
De Servi, M. DelPinto, A. Di Chiara, G. Di Pasquale, L. Filippucci, M. diol 1988;11:1-11.
Galli, E. Gardinale, M.T. Landoni, A. Martoni, F. Mauri, N. Maurea, P. 12. The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein
Meneghetti, M. Mennuni, A. Murrone, A. Pani, E. Paolini, P. Passarelli, G. IIb/IIIa with eptifibatide in patients with acute coronary syndromes.
Pettinati, B. Pontillo, L. Rossi, R. Rossi, M. Santini, G. Sabino, P. Tricoci, N Engl J Med 1998;339:436-43.
F.M. Turazza; Mexico (240) — A. Cruz Diaz, A. Garcia-Sosa, I. Hernandez 13. The Heart Outcomes Prevention Evaluation Study Investigators. Ef-
Santamaria, J. Leiva Pons, J.N. Medecigo, F.J. Rangez Rojo, C. Jorges- fects of an angiotensin-converting–enzyme inhibitor, ramipril, on cardio-
Sanchez Diaz, J. Trujillo Castro, E. Villegas Morales; the Netherlands (499) vascular events in high-risk patients. N Engl J Med 2000;342:145-53.
— S. Baldew, D.C.G. Basart, N. Bijsterfeld, P. Bronzwaer, A. Chardon, M. [Erratum, N Engl J Med 2000;342:748.]
den Hartoog, H. Heijmen, J. Heijmeriks, G. Jochemsen, H. Klomps, P. 14. Yusuf S, Wittes J, Friedman L. Overview of results of randomized clin-
Landsaat, H. Michels, A. Moons, M. Pieterse, A. Sadée, G. van Beek, M. ical trials in heart disease. II. Unstable angina, heart failure, primary preven-
Van Hessen, J. Verheul, E. Viergever; New Zealand (89) — M. Audeau, M. tion with aspirin, and risk factor modification. JAMA 1988;260:2259-63.
Hills, H. Ikram, M. Johnstone, A. Smart; Norway (61) — J. Erikssen, T. 15. Tonkin AM, Colquhoun D, Emberson J, et al. Effects of pravastatin
Morstel, J. Winther Haerem; Poland (2050) — P. Achremczyk, A. Bara- in 3260 patients with unstable angina: results from the LIPID study. Lan-
nowska, P. Burduk, D. Cichon, A. Czepiel, H. Danielewicz, P. Danielewicz, cet 2000;356:1871-5.
W. Dworzanski, J. Gessek, A. Gorecki, J. Gorny, K. Janik, A. Jedrzejowski, 16. Anti-thrombotic Trialists Collaboration. Prevention of death, myocar-
G. Kania, T. Kawka-Urbanek, J. Klaudel, D. Kopcik, A. Kozlowski, W. Kra- dial infarction and stroke by antiplatelet therapy: collaborative meta-analysis
sowski, A. Ladach, M. Laniec, J. Maciejewicz, P. Maciejewski, Z. Majcher, of 266 trials involving 200,000 patients at high risk of occlusive vascular
S. Malinowski, T. Marczyk, P. Miekus, T. Myczka, M. Ogorek, M. Piepior- disease. BMJ (in press).
ka, K. Religa, Z. Reszka, M. Rozwodowska, W. Smielak-Korombel, D. 17. The SYMPHONY Investigators. Comparison of sibrafiban with aspirin
Smiglak, J. Spyra, S. Stec, D. Susol, M. Szpajer, P. Szymanski, G. Szumczyk- for prevention of cardiovascular events after acute coronary syndromes:
Muszytowska, M. Tomzynski, M. Ujda, W. Wasek, T. Waszyrowski, P. a randomised trial. Lancet 2000;355:337-45.
Wojewoda, A. Wnorowska, P. Wrobel, J. Zadrozny, A. Zebrowski, Z. Zie-
linski; Portugal (129) — J.M. Bastos, P. Cardoso, M. Carrageta, C. Catari- Copyright © 2001 Massachusetts Medical Society.
502 · N Engl J Med, Vol. 345, No. 7 · August 16, 2001 · www.nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 26, 2019. For personal use only. No other uses without permission.
Copyright © 2001 Massachusetts Medical Society. All rights reserved.
Вам также может понравиться
- Nejmoa 010746Документ9 страницNejmoa 010746Mmle BlaséОценок пока нет
- Prasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesДокумент15 страницPrasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDito LopezОценок пока нет
- COMMIT ClopidogrelДокумент15 страницCOMMIT ClopidogrelCristina PazmiñoОценок пока нет
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Документ11 страницEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazОценок пока нет
- Editorial 2Документ4 страницыEditorial 2david1086Оценок пока нет
- Duration of Dual Antiplatelet Therapy in Acute Coronary SyndromeДокумент8 страницDuration of Dual Antiplatelet Therapy in Acute Coronary SyndromeCaro GasparОценок пока нет
- Jamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFДокумент10 страницJamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFFernando DominguezОценок пока нет
- Myocard InfarctionДокумент10 страницMyocard InfarctionFelicia HoseaОценок пока нет
- White 2012 Champion PooledДокумент13 страницWhite 2012 Champion PooledRadu CiprianОценок пока нет
- Prologhed TherapyДокумент5 страницProloghed TherapyNagatzulОценок пока нет
- Neuro - Jurding - TIA Minor StrokeДокумент23 страницыNeuro - Jurding - TIA Minor StrokesalfarinaОценок пока нет
- High-Dose Clopidogrel, Prasugrel or Ticagrelor: Trying To Unravel A Skein Into A Ball. Alessandro Aprile, Raffaella Marzullo, Giuseppe Biondi Zoccai, Maria Grazia ModenaДокумент8 страницHigh-Dose Clopidogrel, Prasugrel or Ticagrelor: Trying To Unravel A Skein Into A Ball. Alessandro Aprile, Raffaella Marzullo, Giuseppe Biondi Zoccai, Maria Grazia ModenaDrugs & Therapy StudiesОценок пока нет
- Anticoagulation and Antiplatelet Therapy in Acute Coronary Syndromes (CCJM 2014)Документ12 страницAnticoagulation and Antiplatelet Therapy in Acute Coronary Syndromes (CCJM 2014)Luis Gerardo Alcalá GonzálezОценок пока нет
- Ticagrelor in Patients With Stable Coronary Disease and DiabetesДокумент11 страницTicagrelor in Patients With Stable Coronary Disease and DiabetesPaulo VictorОценок пока нет
- heart failure articleДокумент7 страницheart failure articlefaraz.mirza1Оценок пока нет
- MatcH 2004Документ7 страницMatcH 2004Pedro Garcia CervantesОценок пока нет
- CYP450 System and Not BeingДокумент5 страницCYP450 System and Not BeingArfa'i LaksamanaОценок пока нет
- New England Journal Medicine: The ofДокумент11 страницNew England Journal Medicine: The ofChanakarn PanОценок пока нет
- cilostazol timingДокумент11 страницcilostazol timingesdras pramuditaОценок пока нет
- Isar React 5Документ11 страницIsar React 5Pedro JalladОценок пока нет
- 3745 PDFДокумент6 страниц3745 PDFJanuar RezkyОценок пока нет
- JCN 10 189 PDFДокумент8 страницJCN 10 189 PDFMeilinda SihiteОценок пока нет
- PLATO糖尿病Документ11 страницPLATO糖尿病陈诗哲Оценок пока нет
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionДокумент9 страницPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyОценок пока нет
- Nikolsky2007 PDFДокумент7 страницNikolsky2007 PDFPicha PichiОценок пока нет
- 2009.-Prasugrel in Clinical PracticeДокумент3 страницы2009.-Prasugrel in Clinical Practicetristan9454Оценок пока нет
- 1 s2.0 S0735109719300956 MainДокумент9 страниц1 s2.0 S0735109719300956 MainAlberto PolimeniОценок пока нет
- Colchicine in Coronary Artery Disease (NEJM, 2020) PDFДокумент10 страницColchicine in Coronary Artery Disease (NEJM, 2020) PDFthe_leoОценок пока нет
- Nejmoa2021372 PDFДокумент10 страницNejmoa2021372 PDFNiki MawraОценок пока нет
- Jurnal ACS 2001Документ6 страницJurnal ACS 2001Artha CimutОценок пока нет
- On-Treatment Function Testing of Platelets and Long-Term Outcome of Patients With Peripheral Arterial Disease Undergoing Transluminal AngioplastyДокумент8 страницOn-Treatment Function Testing of Platelets and Long-Term Outcome of Patients With Peripheral Arterial Disease Undergoing Transluminal AngioplastyGono GenieОценок пока нет
- Johnston 2018Документ23 страницыJohnston 2018cru1s3rОценок пока нет
- Su 2015Документ7 страницSu 2015carolin enjelin rumaikewiОценок пока нет
- Prasugrel Vs ClopidogrelДокумент13 страницPrasugrel Vs ClopidogrelCLARA NATALIA LARA MORENOОценок пока нет
- New England Journal Medicine: The ofДокумент9 страницNew England Journal Medicine: The ofHila AmaliaОценок пока нет
- Initial Invasive or Conservative Strategy For Stable Coronary DiseaseДокумент12 страницInitial Invasive or Conservative Strategy For Stable Coronary DiseaseDrMarcus KeyboardОценок пока нет
- Stroke 1998 Gorelick 1737Документ9 страницStroke 1998 Gorelick 1737mochamad rizaОценок пока нет
- TIM StudyДокумент9 страницTIM StudypsoluopostimОценок пока нет
- Clopi Vs Tica Prasu Mayor 70 AnosДокумент6 страницClopi Vs Tica Prasu Mayor 70 AnosGustavo Reyes QuezadaОценок пока нет
- Trial Updates: ClinicalДокумент10 страницTrial Updates: ClinicalIndahОценок пока нет
- 02art8090web PDFДокумент9 страниц02art8090web PDFSyilla PriscilliaОценок пока нет
- MinaДокумент6 страницMinaminamoharebОценок пока нет
- ASD2Документ6 страницASD2Aqla Sabrianti MaulidaОценок пока нет
- Nejmc 0909586Документ4 страницыNejmc 0909586theboy14juneОценок пока нет
- Joc120067 882 889Документ8 страницJoc120067 882 889www.manvith8Оценок пока нет
- CapricornДокумент6 страницCapricornMarkanthony256Оценок пока нет
- Cocot TrialДокумент9 страницCocot TrialAngelEduardoVillarrealGiraldoОценок пока нет
- Treatment Effect of Early Dual Antiplatelet Therapy in Minor StrokeДокумент14 страницTreatment Effect of Early Dual Antiplatelet Therapy in Minor Strokelemonia krakerОценок пока нет
- 3ยา ต้องให้PPIДокумент7 страниц3ยา ต้องให้PPIChayagon MongkonsawatОценок пока нет
- Cortez-Neuroradiology 2020Документ10 страницCortez-Neuroradiology 2020Pedro VillamorОценок пока нет
- TilemahДокумент7 страницTilemahAndreea TudurachiОценок пока нет
- Safety and Efficacy of Intensive Vs Guideline Antiplatelet Thera 2015Документ7 страницSafety and Efficacy of Intensive Vs Guideline Antiplatelet Thera 2015AnDreARОценок пока нет
- Jama You 2020 Oi 200094 1603319690.60891Документ11 страницJama You 2020 Oi 200094 1603319690.60891edo adimastaОценок пока нет
- Clopidogrel Withdrawal: Is There A "Rebound" Phenomenon?: Thrombosis and Haemostasis February 2011Документ11 страницClopidogrel Withdrawal: Is There A "Rebound" Phenomenon?: Thrombosis and Haemostasis February 2011Jhonatan Efrain Lopez CarbajalОценок пока нет
- Ticagrelor With or Without Aspirin in High-Risk Patients After PCIДокумент11 страницTicagrelor With or Without Aspirin in High-Risk Patients After PCIAdane PetrosОценок пока нет
- EFNS Congress Vienna Semax AbstractДокумент60 страницEFNS Congress Vienna Semax AbstractnontjeОценок пока нет
- COMMIT Trial PDFДокумент11 страницCOMMIT Trial PDFachyutsharmaОценок пока нет
- CPG3 Secondary Stroke PreventionДокумент10 страницCPG3 Secondary Stroke Preventionmochamad rizaОценок пока нет
- MainДокумент1 страницаMainDarimotu MankogulsОценок пока нет
- Qdoc - Tips Topnotch Supplement Pharmacology HandoutДокумент57 страницQdoc - Tips Topnotch Supplement Pharmacology HandoutShehana MusahariОценок пока нет
- Prep U Exam #1 Adult 1Документ14 страницPrep U Exam #1 Adult 1Adriana RemedioОценок пока нет
- PANRE and PANCE Review Emergency MedicineДокумент15 страницPANRE and PANCE Review Emergency MedicineThe Physician Assistant Life100% (2)
- Anembryonic Pregnancy/ Gestation (O02.0)Документ137 страницAnembryonic Pregnancy/ Gestation (O02.0)Marvin Mark AbamongaОценок пока нет
- Pre-Operative AssessmentДокумент33 страницыPre-Operative AssessmentKartika FitriОценок пока нет
- Finals Trans (Hema)Документ16 страницFinals Trans (Hema)Ayesha CaragОценок пока нет
- Hpia & Specific Indicators Tech Spec 2022Документ65 страницHpia & Specific Indicators Tech Spec 2022Aslam AssandakaniОценок пока нет
- Drug Study RifampicinДокумент1 страницаDrug Study RifampicinEphraim MaravillaОценок пока нет
- Initial Evaluation Reveals Moderate ComplexityДокумент3 страницыInitial Evaluation Reveals Moderate ComplexitykhushmitОценок пока нет
- 2018 IspadДокумент28 страниц2018 IspadJohana JuarezОценок пока нет
- Complete Breathing and Exchange of GasesДокумент20 страницComplete Breathing and Exchange of GasesAОценок пока нет
- Chapter 16-Urinary SystemДокумент24 страницыChapter 16-Urinary SystemSekar ArumОценок пока нет
- ECG Rhythm Interpretation Module VДокумент27 страницECG Rhythm Interpretation Module Vtri ditaОценок пока нет
- Hypertrophic CardiomyopathyДокумент37 страницHypertrophic CardiomyopathyMarko Vukovic100% (1)
- Hypertension ThesisДокумент31 страницаHypertension ThesisNavin AdhikariОценок пока нет
- Pharma Notes Frcem ResourcesДокумент5 страницPharma Notes Frcem ResourcesKim Nicole VillafloresОценок пока нет
- Chronic SinusitisДокумент7 страницChronic SinusitisMEDS easyОценок пока нет
- Titans AnatomyДокумент355 страницTitans AnatomyAron Anthony RomeyОценок пока нет
- Quiz - Red Blood Cell and Bleeding Disorder - Attempt ReviewДокумент83 страницыQuiz - Red Blood Cell and Bleeding Disorder - Attempt ReviewAdrian CaballesОценок пока нет
- NBME 26 Questions Version PDFДокумент203 страницыNBME 26 Questions Version PDFRakulОценок пока нет
- Kmedical Definition of Respiratory RateДокумент65 страницKmedical Definition of Respiratory RateKebede KassuОценок пока нет
- Drug Prefixes&Suffixes Copyright BNДокумент3 страницыDrug Prefixes&Suffixes Copyright BNJeshan Yanong BeltranОценок пока нет
- Adherence Tradeoff To Multiple Preventive Therapies and All-Cause Mortality After Acute Myocardial InfarctionДокумент12 страницAdherence Tradeoff To Multiple Preventive Therapies and All-Cause Mortality After Acute Myocardial InfarctionRoberto López MataОценок пока нет
- Muscular System Notes Part 1: Muscle AnatomyДокумент3 страницыMuscular System Notes Part 1: Muscle AnatomyMaddie BulauОценок пока нет
- STEMIДокумент34 страницыSTEMIefendiОценок пока нет
- Medicine Lecture 17,18Документ51 страницаMedicine Lecture 17,18Nayela AkramОценок пока нет
- Unit Iii R2019Документ57 страницUnit Iii R2019Gayathri RadhaОценок пока нет
- Ministry of Health of Ukraine Vinnitsa National Medical University of N.I.PirogovaДокумент7 страницMinistry of Health of Ukraine Vinnitsa National Medical University of N.I.PirogovaRitu ChoudharyОценок пока нет
- Facility Risk Assessment Form v.2Документ1 страницаFacility Risk Assessment Form v.2Errol Llanes100% (1)
- Presentant: Dr. Arli Suryawinata Fasilitator: Dr. M.Iqbal Rivai, SP.-KBDДокумент44 страницыPresentant: Dr. Arli Suryawinata Fasilitator: Dr. M.Iqbal Rivai, SP.-KBDArli SuryaОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesОт EverandThe Ultimate Guide To Memory Improvement TechniquesРейтинг: 5 из 5 звезд5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementОт EverandTechniques Exercises And Tricks For Memory ImprovementРейтинг: 4.5 из 5 звезд4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОценок пока нет
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОценок пока нет
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 5 из 5 звезд5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingОт EverandThe Happiness Trap: How to Stop Struggling and Start LivingРейтинг: 4 из 5 звезд4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 5 из 5 звезд5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 3.5 из 5 звезд3.5/5 (32)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОт EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОценок пока нет
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossОт EverandThe Tennis Partner: A Doctor's Story of Friendship and LossРейтинг: 4.5 из 5 звезд4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisОт EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisРейтинг: 5 из 5 звезд5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)