Академический Документы
Профессиональный Документы
Культура Документы
Managementul Pacientilor Boala Arteriala Periferica
Загружено:
Irina NeamtuАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Managementul Pacientilor Boala Arteriala Periferica
Загружено:
Irina NeamtuАвторское право:
Доступные форматы
CRITICIAL LIMB ISCHEMIA: EPIDEMIOLOGY
Mark G. Davies, M.D., Ph.D., M.B.A.
Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
M.G. Davies, M.D.,
Ph.D., M.B.A.
Abstract
Critical limb ischemia is found in 12% of the U.S. adult population. Its clinical presentation varies from no symptoms to intermittent
claudication, atypical leg pain, rest pain, ischemic ulcers, or gangrene. Those with critical limb ischemia have a high incidence of
cardiovascular comorbidities that reflect a significant systemic atherosclerotic burden; they have increased functional impairment
and increased rates of functional decline compared with persons without critical limb ischemia. Interventions for critical limb
ischemia and the impact of major amputation have a significant social and economic impact. At 1 year, 25% of patients will
be dead, 30% will have undergone amputation, and only 45% will remain alive with both limbs. At 5 years, more than 60% of
patients with critical limb ischemia will be dead.
Introduction
Eight to ten million Americans suffer from arterial occlusive
disease, leading to approximately 500–1,000 new cases of chronic
limb ischemia per million people per year.1 The prevalence
of critical limb ischemia is 12% in the adult population, with
men affected slightly more than women. This prevalence is
age-dependent as well, with nearly 20% of adults age 70 and older
carrying a diagnosis of critical limb ischemia. As the population
ages, the impact of this disease on health care will be magnified.
The PARTNERS (PAD Awareness, Risk, and Treatment: New
Resources for Survival) study found critical limb ischemia present
in 29% of the study patients aged 70 years and older and aged 50
to 69 years with at least a 10-pack-per-year history of smoking or a
history of diabetes.2 Greater than 70% of primary care providers in
the PARTNERS study were unaware of the presence of critical limb
ischemia in their patients who had the disease. Coexistent coronary
Figure 1. 10-year survival in patients with asymptomatic and symptomatic
artery disease (CAD) and cerebrovascular disease (CVD) are highly peripheral arterial disease.
prevalent (63%) in patients with critical limb ischemia, particularly
in the elderly population. Patients over the age of 50 with critical alive with both limbs.1 More than 60% of patients with critical
limb ischemia in an academic, hospital-based geriatric practice limb ischemia will be dead at 5 years.6 Patients with critical limb
have a 68% and 42% incidence of coexistent CAD and stroke, ischemia are at an exceptionally high risk for cardiovascular events,
respectively.3 The Reduction of Atherothrombosis for Continued and the majority will eventually die of a cardiac or cerebrovascular
Health (REACH) registry showed that one of six patients with event. The more symptomatic and severe the critical limb ischemia
peripheral arterial disease (PAD), CVD, or CAD had involvement as objectively measured by the ankle-brachial index (ABI), the
of one or two other arterial beds.4, 5 The REACH registry also worse the overall patient prognosis (Figure 1). In the REACH
demonstrated a substantial gap between recommended clinical registry, the relative risk of dying among patients with large-vessel
guidelines and actual clinical practices in caring for patients with critical limb ischemia versus none was 3.1 (95% CI 1.9–4.9) for
or at risk for atherothrombosis. A pattern of underutilization of deaths from all causes and 5.9 (95% CI 3.0–11.4) for all deaths from
established medical therapies and lifestyle interventions was shown cardiovascular disease. Mortality due to cardiovascular disease
throughout all geographic regions studied and vascular disease was 15-fold higher among symptomatic subjects with severe large-
subtypes.4 vessel critical limb ischemia. Finally, critical limb ischemia has
Chronic limb ischemia reflects the local manifestations of been classified as a coronary heart disease (CHD) risk equivalent
a lethal systemic disease — atherosclerosis. If left untreated, (i.e., carrying >20% risk of a coronary event in 10 years).
chronic limb ischemia can result in major limb loss. Critical limb The Expert Panel on Detection, Evaluation, and Treatment
ischemia can be separated into four distinct cohorts: asymptomatic, of High Blood Cholesterol in Adults (2001)7 classified diabetes,
claudication, critical limb ischemia with rest pain, and critical multiple cardiac risk factors, and critical limb ischemia, including
limb ischemia with tissue loss. The natural history of critical carotid disease and abdominal aortic aneurysm, as a CHD risk
limb ischemia is well documented. At 1 year, 25% of patients will equivalent. The epidemic of diabetes and metabolic syndrome
be dead, 30% will have undergone amputation, and 45% will be has escalated the number of lower-extremity problems presenting
10 debakeyheartcenter.com/journal MDCVJ | VIII (4) 2012
for treatment. It has been estimated that 50% of diabetic patients
have evidence of chronic critical limb ischemia.8 Diabetics suffer
from both micro- and macro-vascular disease of complex etiology,
manifested often as ischemia but more frequently as motor or
sensory neuropathies.9 Globally, diabetes accounts for 1 amputation
every 30 seconds and 80,000 amputations annually in the United
States alone. Fifty percent of these patients will have an above- or
below-knee amputation, 50% will require a second amputation
within 5 years, and 50% will be dead in five years. Of those
patients presenting with critical limb ischemia, 67% undergo a
primary amputation, and 50% of these are performed without
imaging or noninvasive testing. Of these amputations, 85% are
considered preventable.7
Clinical Presentation and Diagnosis
The clinical presentation of critical limb ischemia may vary
Figure 2. The relative importance of key risk factors in the progression of
from no symptoms to intermittent claudication, atypical leg pain, peripheral arterial disease.
rest pain, ischemic ulcers, or gangrene. The ABI is a simple test
that can be conducted in the office and typically confirm the
presence of disease. It is calculated by dividing the ankle pressure patients. The all-cause mortality was 3.1 times greater and CVD
by the highest brachial pressure. An ABI <0.9 is abnormal and mortality was 5.9 times greater in patients with critical limb
indicates critical limb ischemia. An ABI between 0.7 and 0.9 is ischemia compared to patients without critical limb ischemia.
considered mild disease, between 0.3 and 0.69 is moderate disease, Studies have shown that the risk of cardiovascular events is
and less than 0.3 is severe disease. There are many classifications similar between critical limb ischemia patients with claudication
for claudication and limb ischemia, but the most utilized is the and those without symptoms. The extremely high morbidity
Rutherford-Becker classification. Rutherford Grade I indicates and mortality in the critical limb ischemia population is due to
essentially asymptomatic patients or symptoms during a very myocardial infarction and stroke. Both the Edinburgh Artery
high level of activity; Rutherford Grade II is symptoms during a Study12 and the ARIC (Atherosclerosis Risk in Communities)13
moderate level of activity; and Rutherford Grade III is symptoms study correlated an increased risk of stroke and transient ischemic
during a low level of activity. Claudicants are considered to fall attack with increased severity of critical limb ischemia. The
within Rutherford Grade I-III. Rutherford Grade IV is symptoms combination of known coronary or cerebrovascular disease and
during rest and is termed “Rest Pain.” Rutherford Grade V is critical limb ischemia has been shown to increase mortality risk.
forefoot ulceration, and Rutherford Grade VI is ulceration with The BARI (Bypass Angioplasty Revascularization Investigation)
tissue necrosis. Rutherford Grade V and VI are termed “Tissue trial demonstrated that patients with multivessel CAD and critical
Loss.” limb ischemia had a relative risk of death 4.9-times greater than
Claudication is the typical symptomatic expression of critical those without critical limb ischemia.14, 15 Additionally, in a pooled
limb ischemia. However, asymptomatic disease may occur in analysis of eight randomized prospective trials involving 19,867
up to 50% of these patients. Of the 460 patients with critical limb patients undergoing percutaneous coronary intervention, the
ischemia in the Walking and Leg Circulation Study,10 19.8% had no 1-year mortality was 5% in patients with critical limb ischemia and
exertional leg pain, 28.5% had atypical leg pain, 32.6% had classic coronary disease compared with 2.1% in patients with coronary
intermittent claudication, and 19.1% had pain at rest. The results disease alone (p <0.001).16
of these and other studies indicate that more patients with critical Chronic limb ischemia is strongly associated with
limb ischemia are asymptomatic or have atypical leg symptoms cardiovascular risk factors such as cigarette smoking, diabetes
than have classic intermittent claudication. mellitus, dyslipidemia, hypertension, and hyperhomocysteinemia
The presence of critical limb ischemia has two major (Figure 2).17-19 Cigarette smoking is associated with a marked
consequences. The first is a decrease in overall well-being and increased risk for peripheral atherosclerosis, and 70–90%
quality of life due to reduced blood flow and atypical leg pain. of patients with chronic limb ischemia are either current or
This often leads to patients becoming sedentary due to pain and ex-smokers.17, 20-22 Follow-up of smokers and ex-smokers at 7 years
discomfort. They may develop depression. The second consequence shows that critical limb ischemia had developed in 16% of smokers
is markedly increased cardiovascular morbidity (myocardial but not in ex-smokers.23 The 10-year incidence of myocardial
infarction and stroke) and mortality (cardiovascular and all-cause). infarction is five times greater in the smoking group compared
to ex-smokers (53% vs. 11%). At 10-year follow-up, cardiovascular-
Risk Factors related mortality in the smoking group is more than 50%, three
Critical limb ischemia is most often diagnosed by an ABI ≤ 0.9. times that of the nonsmoking group.
A low ABI is an independent predictor of increased mortality. In Elevated cholesterol has been shown in the Framingham
the Framingham Study, mortality in patients with intermittent study to be a weak but significant increased risk for chronic limb
claudication was 2–3 times higher than in age- and sex-matched ischemia.20 Lipid profile abnormalities, such as elevated serum
control patients, with 75% of critical limb ischemia patients dying triglyceride levels and reduced high-density lipoproteins, have
from cardiovascular events. In a 15-year review of patients with been found in the majority of studies of patients with chronic limb
claudication, over 66% of mortality was attributable to CVD. ischemia,24 and there is a strong inverse relationship between
In a 10-year prospective study by Criqui et al.,11 critical limb high-density lipoprotein levels and chronic limb ischemia
ischemia patients both with and without a history of CVD had severity.25 Lipoprotein (a) levels have been shown to correlate with
a significantly increased risk of dying from cardiovascular and LDL, cholesterol fibrinogen levels, and with the severity of critical
coronary heart disease compared with age-matched control limb ischemia.26 The Scandinavian Simvastatin Survival Study
MDCVJ | VIII (4) 2012 debakeyheartcenter.com/journal 11
(4S) demonstrated that subjects randomized to simvastatin had a at rest and after exercise. Thrombin formation is enhanced in
38% reduction in new or worsening claudication compared with these patients after submaximal treadmill exercise. Cumulatively,
subjects randomized to placebo.27 Another study has demonstrated these data suggest that the patients with critical limb ischemia
improved walking ability in patients treated with a statin are relatively hypercoagulable. Higher D-dimer levels are
compared to those not on a statin.28 associated with poorer functional activity measures,33 however, the
Markers of inflammation have been associated with the significance of such findings is unknown.57, 58
development of atherosclerosis and cardiovascular events.29,30 In
particular, C-reactive protein (CRP) is independently associated Socio-Economic Effects
with critical limb ischemia, even in patients with normal Patients with critical limb ischemia have increased functional
lipid levels.31, 32 Higher CRP levels are associated with poorer impairment and increased rates of functional decline compared to
functioning measures.33 In the Physicians Health Study, an those without critical limb ischemia;10 specifically, they have lower
elevated CRP level was a risk factor for developing symptomatic physical activity levels, slower walking speed, poorer balance,
critical limb ischemia as well as for peripheral revascularization.34 and poorer walking endurance.10, 59 This functional impairment
Elevated plasma homocysteine levels are an independent risk factor affects quality of life and may lead to an increased prevalence of
for critical limb ischemia.35-37 Although B-vitamin supplements can depressive symptoms that have been observed in patients with
lower homocysteine levels, there is minimal evidence that they can critical limb ischemia.60 Even patients with critical limb ischemia
help prevent cardiovascular events.38, 39 who are asymptomatic have significantly impaired lower extremity
Platelets and their products are known to play a key role in function compared with those who do not have PAD.59
atherosclerosis. Platelet activity has been shown to be 30% higher The economic burden of critical limb ischemia is considerable.
in patients with peripheral vascular disease even if they are Brahmanandam et al.61 recently reported that patients with critical
asymptomatic.40, 41 Not surprisingly, antiplatelet therapy has shown limb ischemia who underwent revascularization used more
significant reductions in fatal and non-fatal vascular events in health care services after hospital discharge than did patients
‘high-risk’ vascular patients, e.g., claudicants.42-44 The risk reduction with noncritical limb ischemia. These services included home
for antiplatelet therapy versus placebo in the claudicant population health care and transfers to rehabilitation facilities. Independent
was 46% for nonfatal stroke, 32% for nonfatal myocardial infarction, predictors for increased health care services utilization include
and 20% for death from a vascular cause. Even “low-risk” patients older age, female gender, care at a private hospital, longer length
on antiplatelet therapy have shown small but significant risk of hospitalization, African American race, highest income
reduction. Progression of peripheral atherosclerosis, as measured quartile, and undergoing amputation or debridement.61 The cost
by angiography, has also been shown to be inhibited in antiplatelet- of clinical care for patients with critical limb ischemia in 1990 was
treated patients.45 A randomized, blinded trial of clopidogrel estimated at $43,000/patient/year.62 The mean cost of inpatient
versus aspirin in patients at risk of ischemic events (CAPRIE) hospital treatment during the first 12 months of follow-up in
had a large subgroup of patients with atherosclerotic vascular patients undergoing surgical bypass for critical limb ischemia was
disease.46 Clopidogrel was shown to have a small but significantly estimated at £23,322 sterling, which was approximately one-third
greater reduction in vascular morbidity and mortality than aspirin, higher than patients undergoing angioplasty treatment.63 Others
and there were no major differences in safety profiles between have shown that although there is nearly a two-fold difference in
the two drugs. Despite clopidogrel therapy, patients undergoing initial cost, the cost-savings of endovascular therapy is not realized
percutaneous coronary intervention with stenting are at risk of over time secondary to subsequent reintervention, particularly
recurrent coronary events. This could be partly explained by a in critical limb ischemia patients.64 Finally, the median cost of
reduced efficacy of clopidogrel to inhibit platelet aggregation, an ex managing a patient after amputation is estimated at almost twice
vivo-defined phenomenon called clopidogrel nonresponsiveness that of successful limb salvage.65 Thus, critical limb ischemia
or resistance. Laboratory clopidogrel nonresponsiveness can be represents a challenging disease state that is associated with
found in approximately 1 in 5 patients. It is inversely correlated considerable morbidity and mortality and a large financial impact
with time between clopidogrel loading and determination of on society.
nonresponsiveness and loading dose used.47
Hemostatic abnormalities are found frequently in critical limb CONCLUSION
ischemia and may contribute to pathogenesis or be a marker of Chronic critical limb ischemia is a significant, often under-
disease progression.48-50 The presence of the lupus anticoagulant recognized facet of atherosclerotic disease that has significant
and elevated markers of platelet activation (beta thromboglobulin medical and functional consequences. A thorough understanding
levels) have been associated with peripheral atherosclerosis.51, 52 of the systemic risk factors associated with the disease followed by
In a study by Gosk-Bierska et al., hemostatic abnormalities were rapid intervention and interruption of the process is necessary to
present in diabetic subjects, with greater evidence of thrombin improve outcomes and prevent limb loss and death.
generation than in non-diabetics.53 Clinical studies on patients
undergoing peripheral bypass surgery have demonstrated the Conflict of Interest Disclosure: The author has completed and submitted
the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement
presence of a definite subset of patients with abnormal coagulation and none were reported.
profiles.54 After adjusting for age and sex, von Willebrand Factor Funding/Support: The author has no funding disclosures.
(vWF), fibrin, D-dimer and urinary fibrinopeptide A are elevated in Keywords: critical limb ischemia; cardiovascular disease; cardiovascular
patients with critical limb ischemia, and the risk for claudication is risk factors; claudication; peripheral arterial disease; amputation
significantly raised with unit changes in each factor.55, 56 Enhanced
levels of fibrinogen, alpha-1-antitrypsin, thrombin/antithrombin References
III complex, alpha-2 plasmin inhibitor/plasmin complex, and 1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA,
thrombomodulin were documented in claudicants.57 Compared Fowkes FGR, on behalf of the TASC II Working Group. Inter-
with healthy control subjects, patients with critical limb ischemia society consensus for the management of peripheral arterial
show higher t-PA antigen, PAI-1 antigen, and D-dimer levels both disease (TASC II). J Vasc Surg. 2007 Jan;45(1 Suppl):S5-S67.
12 debakeyheartcenter.com/journal MDCVJ | VIII (4) 2012
2. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, 17. Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on
Creager MA, Olin JW, et al. Peripheral arterial disease detection, the prevalence of peripheral arterial disease, The San Luis Valley
awareness, and treatment in primary care. JAMA. 2001 Sep diabetes study. Circulation. 1995 Mar 1;91(5):1472-9.
19;286(11):1317-24. 18. Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP,
3. Ness J, Aronow WS. Prevalence of coexistence of coronary Borhani NO, et al. Ankle arm index as a marker of atherosclerosis
artery disease, ischemic stroke, and peripheral arterial in Cardiovascular Health Study (CHS) Collaborative Research
disease in older persons, mean age 80 years, in an academic Group. Circulation. 1993 Sep;88(3):837-45.
hospital-based geriatrics practice. J Am Geriatr Soc. 1999 19. Graham IM, Daly LE, Refsum HM, Robinson K, Brattström
Oct;47(10):1255-6. LE, Ueland PM, et al. Plasma homocysteine as a risk factor
4. Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, for vascular disease. The European Concerted Action Project.
et al. International prevalence, recognition, and treatment of JAMA. 1997 Jun 11;277(22):1775-81.
cardiovascular risk factors in outpatients with atherothrombosis. 20. Kannel WB, McGee DL. Update on some epidemiological feature
JAMA. 2006 Jan 11;295(2):180-9. of intermittent claudication: the Framingham Study. J Am Ger
5. Cacoub PP, Abola MT, Baumgartner I, Bhatt DL, Creager Soc. 1985 Jan;33(1):13-8.
MA, Liau CS, et al. Cardiovascular risk factor control and 21. Kannel WB, McGee DL, Castelli WP. Latest perspectives on
outcomes in peripheral artery disease patients in the Reduction cigarette smoking and cardiovascular disease: the Framingham
of Atherothrombosis for Continued Health (REACH) Registry. study. J Card Rehabil. 1984;4:267-77.
Atherosclerosis. 2009 Jun;204(2):e86-92.
22. Vogt MT, Cauley JA, Kuller LH, Hulley SB. Prevalence and
6. Jämsén TS, Manninen HI, Tulla HE, Jaakkola PA, Matsi PJ. correlates of lower extremity arterial disease in elderly women.
Infrainguinal revascularization because of claudication: total long- Am J Epidemiol. 1993 Mar 1;137:559-68.
term outcome of endovascular and surgical treatment. J Vasc
Surg. 2003 Apr;37(4):808-15. 23. Jonason T, Bergastrom R. Cessation of smoking in patients with
intermittent claudication. Effects on the risk of peripheral vascular
7. Expert Panel on Detection, Evaluation, and Treatment of High complications, myocardial infarction and mortality. Acta Med
Blood Cholesterol in Adults. Executive Summary of The Third Scand. 1987;221(3):253-60.
Report ofThe National Cholesterol Education Program (NCEP)
Expert Panel on Detection, Evaluation, And Treatment of High 24. Belch J. Medical management of intermittent claudication. In:
Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. Greenhalgh RM, editor. Vascular and endovascular opportunities.
2001 May 16;285(19):2486-97. London: WB Saunders; 2000. p. 361-88.
8. Brandman O, Redisch W. Incidence of peripheral vascular 25. Fowkes FG, Housley E, Riemersma RA, Macintyre CC, Cawood
changes in diabetes mellitus. Diabetes. 1953 May-Jun;2:194-8. EH, Prescott RJ, et al. Smoking, lipids, glucose intolerance,
and blood pressure as risk factors for peripheral atherosclerosis
9. Adler AI, Stevens RJ, Neil A, Stratton IM, Boulton AJ, Holman compared with ischemic heart disease in the Edinburgh Arterial
RR. UKPDS 59: hyperglycemia and other potentially modifiable Study. Am J Epidemiol. 1992 Feb 15;135(4):331-40.
risk factors for peripheral vascular disease in type 2 diabetes.
Diabetes Care. 2002 May;25(5):894-9. 26. Cheng SWK, Ting AC, Wong J. Lipoprotein (a) and its
relationship to risk factors and severity of atherosclerotic
10. McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, peripheral vascular disease. Eur J Vasc Endovasc Surg. 1997
Chan C, et al. Functional decline in peripheral arterial disease: Jul;14(1):17-23.
associations with the ankle brachial index and leg symptoms.
JAMA. 2004 Jul 28;2929(4):453-61. 27. Pederson TR, Kjekshus J, Pyörälä K, Olsson AG, Cook TJ,
Musliner TA, et al. Effect of simvastatin on ischemic signs and
11. Criqui MH, Fronek A, Barrett-Conner E, Klauber MR, Gabriel S, symptoms in the Scandinavian simvastatin survival study (4S).
Goodman D. The prevalence of peripheral arterial disease in a Am J Cardiol. 1998 Feb 1;81:333-5.
defined population. Circulation. 1985 Mar;71(3):510-5.
28. McDermott MM, Guralnik JM, Greenland P, Pearce WH, Criqui
12. Fowkes FG, Housley E, Cawood EH, Macintyre CC, Ruckley CV, MH, Liu K, et al. Statin use and leg functioning in patients
Prescott RJ. Edinburgh Artery Study: prevalence of asymptomatic with and without lower-extremity peripheral arterial disease.
and symptomatic peripheral arterial disease in the general Circulation. 2003 Feb 11;107(5):757-61.
population. Int J Epidemiol. 1991 Jun;20(2):384-92.
29. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon
13. Zheng ZJ, Sharrett AR, Chambless LE, Rosamond WD, Nieto RO, Criqui M, et al. Markers of inflammation and cardiovascular
FJ, Sheps DS, et al. Associations of ankle-brachial index with disease: application to clinical and public health practice:
clinical coronary heart disease, stroke and preclinical carotid and A statement for healthcare professionals from the Centers
popliteal atherosclerosis: the Atherosclerosis Risk in Communities for Disease Control and Prevention and the American Heart
(ARIC) Study. Atherosclerosis. 1997 May;131(1):115-25. Association. Circulation. 2003 Jan 28;107(3):499-511.
14. Sutton-Tyrrell K, Rihal C, Sellers MA, Burek K, Trudel J, Roubin 30. Wang TJ, Nam BH, Wilson PW, Wolf PA, Levy D, Polak JK, et
G, et al. Long-term prognostic value of clinically evident al. Association of C-reactive protein with carotid atherosclerosis
noncoronary vascular disease in patients undergoing coronary in men and women: the Framingham Heart Study. Arterioscler
revascularization in the Bypass Angioplasty Revascularization Thromb Vasc Biol. 2002 Oct 1;22(10):1662-7.
Investigation (BARI). Am J Cardiol. 1998 Feb 15;81(4):375-81.
31. Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive
15. Burek KA, Sutton-Tyrrell K, Brooks MM, Naydeck B, Keller N, protein and other markers of inflammation in the prediction of
Sellers MA, et al. Prognostic importance of lower extremity cardiovascular disease in women. N Engl J Med. 2000 Mar
arterial disease in patients undergoing coronary revascularization 23;342(12):836-43.
in the Bypass Angioplasty Revascularization Investigation (BARI).
J Am Coll Cardiol. 1999 Sep;34(3):716-21. 32. Ridker PM, Stampfer MJ, Rifai N. Novel risk factors for systemic
atherosclerosis: a comparison of C-reactive protein fibrinogen
16. Saw J, Bhatt DL, Moliterno DJ, Brener SJ, Steinhubl SR, homocysteine lipoprotein(a) and standard cholesterol screening
Lincoff AM, et al. The influence of peripheral arterial disease as predictors of peripheral arterial disease. JAMA. 2001 May
on outcomes: a pooled analysis of mortality in eight large 16;285(19):2481-5.
randomized percutaneous coronary intervention trials. J Am Coll
Cardiol. 2006 Oct 17;48(8):1567–72.
MDCVJ | VIII (4) 2012 debakeyheartcenter.com/journal 13
33. McDermott MM, Greenland P, Green D, Guralnik JM, Criqui MH, 48. Ray SA, Rowley MR, Loh A, Talbot SA, Bevan DH, Taylor RS.
Liu K, et al. D-dimer, inflammatory markers and lower extremity Hypercoagulable states in patients with leg ischemia. Br J Surg.
functioning in patients with and without peripheral arterial disease. 1994 Jun;81(6):811-4.
Circulation. 2003 Jul 1;107(25):3191-8. 49. Donaldson MC, Weinberg DS, Belkin M, Whittemore AD, Mannick
34. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. JA. Screening for hypercoagulable states in vascular surgical
Plasma concentration of C-reactive protein and risk of developing practice: a preliminary study. J Vasc Surg. 1990 Jun;11(6):825-31.
peripheral vascular disease. Circulation. 1998 Feb 10;97(5):425-8. 50. Strano A, Hoppensteadt D, Walenga JM, Fareed J, Sabba
35. Valentine RJ, Kaplan HS, Green R, Jacobsen DW, Myers SI, C, Berardi E, et al. Plasma levels of the molecular markers of
Clagett GP. Lipoprotein(a), homocysteine and hypercoaguable coagulation and fibrinolysis in patients with peripheral arterial
states in young men with premature peripheral atherosclerosis: a disease. Semin Thromb Hemost. 1996;22 Suppl 1:35-40.
prospective, controlled analysis. J Vasc Surg. 1996 Jan;23(1): 51. Donaldson MC, Weinberg DS, Belkin M, Whittemore AD, Mannick
53-61. JA. Screening for hypercoaguable states in vascular surgical
36. Hoogeveen FK, Kostense PJ, Beks PJ, Mackaay AJ, Jakobs C, practice: a preliminary study. J Vasc Surg. 1990 Jun;11(6):825-31.
Bouter LM, et al. Hyperhomocysteinemia is associated with an 52. Catalano M, Russo U, Libretti A. Plasma beta-thromboglobulin
increased risk of cardiovascular disease, especially in non-insulin- levels and claudication states in vascular surgical practice: a
dependent diabetes mellitus: a population-based study. preliminary study. Angiology. 1986;37:339-42.
Arterioscler Thromb Vasc Biol. 1998 Jan;18(1):133-8.
53. Gosk-Bierska I, Adamiec R, Alexewicz P, Wyokinski WE.
37. Selhub J, Jacques PF, Bostom AG, D’agostino RB, Wilson PW, Coagulation in diabetic and non-diabetic claudicants. Int Angiol.
Belanger AJ, et al. Association between plasma homocysteine 2002 Jun;21(2):128-33.
concentrations and extracranial carotid artery stenosis. N Engl J
Med. 1995 Feb 2;332(5):286-91. 54. Ray SA, Rowley MR, Bevan DH, Taylor RS, Dormandy JA.
Hypercoagulable abnormalities and postoperative failure
38. Jacques PF, Selhub J, Bostom AG, Wilson PW, Rosenberg of arterial reconstruction. Eur J Vasc Endovasc Surg. 1997
IH. The effect of folic acid fortification on plasma folate and Apr;13(4):363-70.
total homocysteine concentrations. N Engl J Med. 1999 May
13;340(19):1449-54. 55. Lee AJ, Fowkes FG, Rattray A, Rumley A, Lowe GD. Hemostatic
and rheological factors in intermittent claudication: the influence
39. Selhub J, Jacques PF, Bostom AG, Wilson PW, Rosenberg IH. of smoking and extent of arterial disease. Br J Haematol. 1996
Relationship between plasma homocysteine and vitamin status in Jan;92(1):226-30.
the Framingham study population: Impact of folic acid fortification.
Public Health Rev. 2000;28(1-4):117-45. 56. Johansson J, Egberg N, Johnsson H, Carlson LA. Serum
lipoproteins and hemostatic function in intermittent claudication.
40. Smith FB, Lowe GD, Fowkes FG, Rumley A, Rumley AG, Donnan Arterioscler Thrombo. 1993 Oct;13(10):1441-8.
PT, et al. Smoking, hemostatic factors and lipid peroxides in a
population case controlled study of peripheral arterial disease. 57. Handa K, Takao M, Nomoto J, Oku K, Shirai K, Saku K, et al.
Atherosclerosis. 1993 Sep;102(2):155-62. Evaluation of the coagulation and fibrinolytic systems in men with
intermittent claudication. Angiology. 1996 Jun;47(6):543-8.
41. Komarov A, Panchenko E, Dobrovolsky A, Karpov Y, Deev A,
Titaeva E, et al. D-dimer and platelet aggregability are related to 58. Mustonen P, Lepäntalo M, Lassila R. Physical exertion induces
thrombotic events in patients with peripheral arterial occlusive thrombin formation and fibrin degradation in patients with
disease. Eur Heart J. 2002 Aug;23(16):1309-16. peripheral atherosclerosis. Arterioscler Thromb Vasc Biol. 1998
Feb;18(2):244-9.
42. Antiplatelet Trialists’ Collaboration. Collaborative overview of
randomized trials of antiplatelet therapy - I: Prevention of death, 59. McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH,
myocardial infarction, and stroke by prolonged antiplatelet therapy Dolan NC, et al. Leg symptoms in peripheral arterial disease:
in various categories of patients. BMJ. 1994 Jan 8;308(6943): associated clinical characteristics and functional impairment.
81-106. JAMA. 2001 Oct 3;286(13):1599-606.
43. Collaborative overview of randomized trials of antiplatelet 60. Arseven A, Guralnik JM, O’Brien E, Liu K, McDermott MM.
therapy — II: maintenance of vascular graft or arterial patency by Peripheral arterial disease and depressed mood in older men and
antiplatelet therapy. Antiplatelet Trialists’ Collaboration. BMJ. 1994 women. Vasc Med. 2001 Nov;6:229-34.
Jan 15;308(6922):159-68. 61. Brahmanandam SM, Messina LM, Belkin M, Conte MS, Nguyen
44. Antiplatelet Trialists’ Collaboration. Collaborative meta-analysis of LL, editors. Determinants of hospital disposition after lower
randomized trials of antiplatelet therapy for prevention of death, extremity bypass surgery. Paper presented at: Vascular Annual
myocardial infarction, and stroke in high risk patients. BMJ. 2002 Meeting, Scientific Program; 2009 Jun 11-14; Denver, CO.
Jan 12;324(7329):71-86. 62. Hunink MG, Wong JB, Donaldson MC, Meyerovitz ME, deVries
45. Hess H, Mietaschk A, Deichsel G. Drug-induced inhibition of J, Harrington DP. Revascularization for femoropopliteal disease:
platelet function delays progression of peripheral occlusive arterial a decision and cost-effectiveness analysis. JAMA. 1995 Jul
disease. A prospective double blind arteriographically controlled 12;274(2):165-71.
trial. Lancet. 1985 Feb 23;1(8426):415-9. 63. Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes
46. A randomized blinded trial of clopidogrel versus aspirin in patients JF, et al. Bypass versus angioplasty in severe ischaemia of the leg
at risk of ischemic events (CAPRIE). CAPRIE steering Committee. (BASIL): multicentre, randomised controlled trial. Lancet. 2005
Lancet. 1996 Nov 16;348(9038):1329-39. Dec 3;366(9501):1925-34.
47. Snoep JD, Hovens MM, Eikenboom JC, van der Bom JG, Jukema 64. Stoner MC, Defreitas DJ, Manwaring MM, Carter JJ, Parker FM,
JW, Huisman MV. Clopidogrel nonresponsiveness in patients Powell CS. Cost per day of patency: understanding the impact of
undergoing percutaneous coronary intervention with stenting: patency and reintervention in a sustainable model of healthcare.
a systematic review and meta-analysis. Am Heart J. 2007 J Vasc Surg. 2008 Dec;48(6):1489-96.
Aug;154(2):221-31. 65. Singh S, Evens L, Datta D, Gaines P, Beard JD. The costs of
managing lower limb-threatening ischaemia. Eur J Vasc Endovasc
Surg. 1996 Oct;12(3):359-62.
14 debakeyheartcenter.com/journal MDCVJ | VIII (4) 2012
Вам также может понравиться
- Designing and Drawing PropellerДокумент4 страницыDesigning and Drawing Propellercumpio425428100% (1)
- At The Origins of Music AnalysisДокумент228 страницAt The Origins of Music Analysismmmahod100% (1)
- HEMATOLOGY-LECTURE-NOTES FTP Lectures PDFДокумент50 страницHEMATOLOGY-LECTURE-NOTES FTP Lectures PDFkat100% (8)
- EX200Документ7 страницEX200shubbyОценок пока нет
- Music 9 Q3 Mod4 Musical Elements of Given Romantic Period PiecesДокумент19 страницMusic 9 Q3 Mod4 Musical Elements of Given Romantic Period PiecesFinn Daniel Omayao100% (1)
- Peripheral Vascular DiseaseДокумент47 страницPeripheral Vascular Diseaseusmle prepОценок пока нет
- Enrico Fermi Pioneer of The at Ted GottfriedДокумент156 страницEnrico Fermi Pioneer of The at Ted GottfriedRobert Pérez MartinezОценок пока нет
- Science and Technology in Ancient India by NeneДокумент274 страницыScience and Technology in Ancient India by NeneAshok Nene100% (1)
- Congestive Heart FailureДокумент15 страницCongestive Heart FailureChiraz Mwangi100% (1)
- A Teachers' Journey: Phenomenological Study On The Puritive Behavioral Standards of Students With Broken FamilyДокумент11 страницA Teachers' Journey: Phenomenological Study On The Puritive Behavioral Standards of Students With Broken FamilyNova Ariston100% (2)
- Beyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisДокумент21 страницаBeyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisEra B. LargisОценок пока нет
- C. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Документ168 страницC. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Nelson100% (3)
- Rotating Equipment & ServiceДокумент12 страницRotating Equipment & Servicenurkasih119Оценок пока нет
- Toshiba MotorsДокумент16 страницToshiba MotorsSergio Cabrera100% (1)
- 160kW SOFT STARTER - TAP HOLE 1Документ20 страниц160kW SOFT STARTER - TAP HOLE 1Ankit Uttam0% (1)
- Hypertrophic CardiomyopathyДокумент10 страницHypertrophic CardiomyopathySam SonОценок пока нет
- 24Документ485 страниц24Irina Neamtu100% (1)
- Contemporaryandoptimal Medicalmanagementof PeripheralarterialdiseaseДокумент18 страницContemporaryandoptimal Medicalmanagementof PeripheralarterialdiseaseAnonymous kdBDppigEОценок пока нет
- Peripheral Arterial Disease in People With Diabetes: Consensus StatementДокумент9 страницPeripheral Arterial Disease in People With Diabetes: Consensus StatementMoch Abdul RokimОценок пока нет
- Peripheral Arterial Disease in Patients With Diabetes: State-Of-The-Art PaperДокумент9 страницPeripheral Arterial Disease in Patients With Diabetes: State-Of-The-Art PaperdonkeyendutОценок пока нет
- Peripheral Arterial DiseaseДокумент8 страницPeripheral Arterial DiseaseSILVIA FERNANDA CASTILLO GOYENECHEОценок пока нет
- Peripheral Artery Disease: Clinical PracticeДокумент11 страницPeripheral Artery Disease: Clinical Practiceapi-311409998Оценок пока нет
- PAD Current InsightsДокумент15 страницPAD Current InsightsMaria PopОценок пока нет
- Bod CerebrovasculardiseasestrokeДокумент67 страницBod CerebrovasculardiseasestrokeErlin IrawatiОценок пока нет
- Bod - Cerebrovascular Disease Stroke BurdenДокумент67 страницBod - Cerebrovascular Disease Stroke BurdenderiОценок пока нет
- Bod Cerebrovasculardiseasestroke PDFДокумент67 страницBod Cerebrovasculardiseasestroke PDFMax Laban SeminarioОценок пока нет
- Biomarkers of Peripheral Arterial Disease: John P. Cooke, MD, P D, Andrew M. Wilson, MBBS, P DДокумент7 страницBiomarkers of Peripheral Arterial Disease: John P. Cooke, MD, P D, Andrew M. Wilson, MBBS, P DBernardo Nascentes BrunoОценок пока нет
- Chronic Heart Failure: Overview#a0101Документ2 страницыChronic Heart Failure: Overview#a0101Erickson OcialОценок пока нет
- Cardiovascular Disease PHD ThesisДокумент6 страницCardiovascular Disease PHD Thesisafknawjof100% (2)
- Journal Coronary Heart DiseaseДокумент9 страницJournal Coronary Heart DiseaseYuliyanti AhmadОценок пока нет
- Task Force On Sudden Cardiac Death, European Society of CardiologyДокумент16 страницTask Force On Sudden Cardiac Death, European Society of Cardiologyvasarhely imolaОценок пока нет
- Definition, Epidemiology, and Prognosis: Reproduced With Permission From The AHAДокумент10 страницDefinition, Epidemiology, and Prognosis: Reproduced With Permission From The AHAIboy ZulhamОценок пока нет
- Corazon EnvejecidoДокумент13 страницCorazon EnvejecidoAntonio AlonsoОценок пока нет
- Causes of Heart FailureДокумент4 страницыCauses of Heart Failurejana7-7Оценок пока нет
- Current and Emerging Drug Treatment Strategies For Peripheral Arterial DiseaseДокумент15 страницCurrent and Emerging Drug Treatment Strategies For Peripheral Arterial DiseasedettolittaОценок пока нет
- Clinical Features and Diagnosis of Lower Extremity Peripheral Artery DiseaseДокумент42 страницыClinical Features and Diagnosis of Lower Extremity Peripheral Artery DiseaseAdrianaIDCОценок пока нет
- Stroke 2011 Schäbitz 2385 6Документ3 страницыStroke 2011 Schäbitz 2385 6Amry Irsyada YusufОценок пока нет
- Epidemiology of Coronary Heart Disease and Acute Coronary SyndromeДокумент6 страницEpidemiology of Coronary Heart Disease and Acute Coronary SyndromeAnonymous GpgioaDAbОценок пока нет
- Contemporary PAD ManagementДокумент27 страницContemporary PAD ManagementMaria PopОценок пока нет
- Peripheral Vascular Disease and DiabetesДокумент8 страницPeripheral Vascular Disease and DiabetesChikezie OnwukweОценок пока нет
- Device Therapy in Heart Failure Patients With Chronic Kidney DiseaseДокумент8 страницDevice Therapy in Heart Failure Patients With Chronic Kidney DiseaseElizabeth SniderОценок пока нет
- Pr2 Chapter 1 3 Peta Icamina 2Документ21 страницаPr2 Chapter 1 3 Peta Icamina 2JOHN ICAMINAОценок пока нет
- Acute Decompensated Heart Failure: ReviewДокумент11 страницAcute Decompensated Heart Failure: ReviewFercee PrimulaОценок пока нет
- Enfermedad CV en El BoxeoДокумент12 страницEnfermedad CV en El BoxeoOmar Fernando Hijar FraustoОценок пока нет
- Seminar: John J V Mcmurray, Marc A PfefferДокумент13 страницSeminar: John J V Mcmurray, Marc A Pfefferjvasco_santos8178Оценок пока нет
- Ankle Fractures in Diabetics: Victor R. Prisk, MD, Dane K. Wukich, MDДокумент15 страницAnkle Fractures in Diabetics: Victor R. Prisk, MD, Dane K. Wukich, MDAnonymous kdBDppigEОценок пока нет
- Epidemiology, Risk Factors, and Natural History of Peripheral Artery DiseaseДокумент20 страницEpidemiology, Risk Factors, and Natural History of Peripheral Artery Diseasesnyder120792Оценок пока нет
- Clinical Features and Diagnosis of Lower Extremity Peripheral Artery DiseaseДокумент16 страницClinical Features and Diagnosis of Lower Extremity Peripheral Artery DiseasePetru GlavanОценок пока нет
- Peripheral Artery DiseaseДокумент6 страницPeripheral Artery DiseaseArunDevaОценок пока нет
- Overview of Lower Extremity Peripheral Artery DiseaseДокумент24 страницыOverview of Lower Extremity Peripheral Artery DiseasePetru GlavanОценок пока нет
- Congestive Heart Failure in The ElderlyДокумент13 страницCongestive Heart Failure in The ElderlyKezia MarsilinaОценок пока нет
- Association Between Coronary Dominance and Acute Inferior Myocardial Infarction: A Matched, Case-Control StudyДокумент7 страницAssociation Between Coronary Dominance and Acute Inferior Myocardial Infarction: A Matched, Case-Control StudyandreaОценок пока нет
- Potential Clinical Benefits of D-Ribose in Ischemic Cardiovascular DiseaseДокумент11 страницPotential Clinical Benefits of D-Ribose in Ischemic Cardiovascular DiseaseNabilaОценок пока нет
- Congestive Heart FailureДокумент16 страницCongestive Heart FailureRahmat Burhanudin RamdaniОценок пока нет
- Coronary Artery Disease: Special Feature: Primary Care Issues For NephrologistsДокумент6 страницCoronary Artery Disease: Special Feature: Primary Care Issues For NephrologistssyahidОценок пока нет
- JournalДокумент11 страницJournalewetОценок пока нет
- In Elderley WileyДокумент6 страницIn Elderley WileyNoel Saúl Argüello SánchezОценок пока нет
- Hypertension in ElderlyДокумент13 страницHypertension in ElderlybookwormMD100% (2)
- Hendro Susilo-Af and StrokeДокумент7 страницHendro Susilo-Af and StrokeyudisОценок пока нет
- Ischemic 39!Документ6 страницIschemic 39!Adina Alexandra CОценок пока нет
- Section 5. Atherosclerotic Peripheral Vascular Disease and Aortic AneurysmДокумент23 страницыSection 5. Atherosclerotic Peripheral Vascular Disease and Aortic AneurysmsidoniavidicanОценок пока нет
- Blood Is Thicker Than WaterДокумент4 страницыBlood Is Thicker Than WateraontreochОценок пока нет
- Definition of Peripheral Arterial Disease (PAD)Документ5 страницDefinition of Peripheral Arterial Disease (PAD)Tudor DumitrascuОценок пока нет
- Pathophysiology and Treatment of Stroke: Present Status and Future PerspectivesДокумент24 страницыPathophysiology and Treatment of Stroke: Present Status and Future Perspectivesdewinta fitriОценок пока нет
- Pi Is 1078588416300533Документ4 страницыPi Is 1078588416300533npr00Оценок пока нет
- Arrhythmic Risk Stratification Among Patients With Hypertrophic CardiomyopathyДокумент14 страницArrhythmic Risk Stratification Among Patients With Hypertrophic CardiomyopathySid RitcherОценок пока нет
- Optimal Management of Peripheral Arterial Disease For The Non-SpecialistДокумент18 страницOptimal Management of Peripheral Arterial Disease For The Non-SpecialistpupuliciouzОценок пока нет
- Peripheral Artery DiseaseДокумент12 страницPeripheral Artery DiseaseAliОценок пока нет
- Nativel2018 Article LowerExtremityArterialDiseaseIДокумент14 страницNativel2018 Article LowerExtremityArterialDiseaseIRaynier GuerreroОценок пока нет
- Myocardial InfarctionДокумент18 страницMyocardial InfarctionYanna Habib-MangotaraОценок пока нет
- Abnormal Ankle Brachial Index and The Presence of Significant Coronary Artery DiseaseДокумент4 страницыAbnormal Ankle Brachial Index and The Presence of Significant Coronary Artery DiseaseNoviLindriatiОценок пока нет
- Ecg in AtheletsДокумент32 страницыEcg in AtheletsOnon EssayedОценок пока нет
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesОт EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesОценок пока нет
- Mplsheartjournal D 17 00004Документ6 страницMplsheartjournal D 17 00004Irina NeamtuОценок пока нет
- 1218 Anexa 15 - 8724 - 6616Документ9 страниц1218 Anexa 15 - 8724 - 6616Irina NeamtuОценок пока нет
- Mplsheartjournal D 17 00004Документ6 страницMplsheartjournal D 17 00004Irina NeamtuОценок пока нет
- Managementul Pacientilor Boala Arteriala PerifericaДокумент2 страницыManagementul Pacientilor Boala Arteriala PerifericaIrina NeamtuОценок пока нет
- Epidemiology of Peripheral Artery DiseaseДокумент18 страницEpidemiology of Peripheral Artery DiseaseIrina NeamtuОценок пока нет
- ESC Guidelines Peripheral Arterial Diseases 2017Документ9 страницESC Guidelines Peripheral Arterial Diseases 2017Irina NeamtuОценок пока нет
- Incidence of Peripheral Vascular Changes in Diabetes MellitusДокумент5 страницIncidence of Peripheral Vascular Changes in Diabetes MellitusIrina NeamtuОценок пока нет
- Pi Is 0741521414007095Документ12 страницPi Is 0741521414007095Irina NeamtuОценок пока нет
- Population-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial EventsДокумент11 страницPopulation-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial EventsIrina NeamtuОценок пока нет
- Complications After Peripheral Vascular Interventions in OctogenariansДокумент7 страницComplications After Peripheral Vascular Interventions in OctogenariansIrina NeamtuОценок пока нет
- Profilax TBCДокумент2 страницыProfilax TBCIrina NeamtuОценок пока нет
- ESC Guidelines Peripheral Arterial Diseases 2017Документ9 страницESC Guidelines Peripheral Arterial Diseases 2017Irina NeamtuОценок пока нет
- CTG HaДокумент15 страницCTG HaNabila SaribanunОценок пока нет
- Pneumonia NosocomialaДокумент6 страницPneumonia NosocomialaAriana CordoșОценок пока нет
- Endocrine VARIANTA 2Документ2 страницыEndocrine VARIANTA 2Irina NeamtuОценок пока нет
- Cap 1 Introduce Re)Документ2 страницыCap 1 Introduce Re)vlad910Оценок пока нет
- Understanding Cardiotocography - "CTGS": Max Brinsmead MB Bs PHD May 2015Документ29 страницUnderstanding Cardiotocography - "CTGS": Max Brinsmead MB Bs PHD May 2015Irina NeamtuОценок пока нет
- Pneumologie Subiecte ExamenДокумент6 страницPneumologie Subiecte ExamenSanda BuruianăОценок пока нет
- Anatomy Orbit and Eyelid - WashedДокумент1 страницаAnatomy Orbit and Eyelid - WashedIrina NeamtuОценок пока нет
- Xtype Power Train DTC SummariesДокумент53 страницыXtype Power Train DTC Summariescardude45750Оценок пока нет
- Resistance & Resistivity: Question Paper 1Документ15 страницResistance & Resistivity: Question Paper 1leon19730% (1)
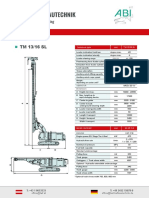
- ABI TM 13 16 SL - EngДокумент1 страницаABI TM 13 16 SL - EngJuan Carlos Benitez MartinezОценок пока нет
- Paul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146Документ27 страницPaul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146usman azharОценок пока нет
- Crisis of The World Split Apart: Solzhenitsyn On The WestДокумент52 страницыCrisis of The World Split Apart: Solzhenitsyn On The WestdodnkaОценок пока нет
- Sainik School Balachadi: Name-Class - Roll No - Subject - House - Assigned byДокумент10 страницSainik School Balachadi: Name-Class - Roll No - Subject - House - Assigned byPagalОценок пока нет
- EngHub How To Break HabitsДокумент13 страницEngHub How To Break HabitsViktoria NovikovaОценок пока нет
- Enrile v. SalazarДокумент26 страницEnrile v. SalazarMaria Aerial AbawagОценок пока нет
- RPH Week 31Документ8 страницRPH Week 31bbwowoОценок пока нет
- March For Our LivesДокумент22 страницыMarch For Our LivesLucy HanОценок пока нет
- Microwave EngineeringДокумент2 страницыMicrowave Engineeringசுந்தர் சின்னையா0% (9)
- Honda IzyДокумент16 страницHonda IzyTerry FordОценок пока нет
- DNA Vs RNA - Introduction and Differences Between DNA and RNAДокумент10 страницDNA Vs RNA - Introduction and Differences Between DNA and RNAKienlevyОценок пока нет
- Group 2 ITI Consensus Report: Prosthodontics and Implant DentistryДокумент9 страницGroup 2 ITI Consensus Report: Prosthodontics and Implant DentistryEsme ValenciaОценок пока нет
- Caradol sc48 08Документ2 страницыCaradol sc48 08GİZEM DEMİRОценок пока нет
- Term Paper Inorganic PolymersДокумент24 страницыTerm Paper Inorganic PolymersCasey Karua0% (1)
- Generalized Class of Sakaguchi Functions in Conic Region: Saritha. G. P, Fuad. S. Al Sarari, S. LathaДокумент5 страницGeneralized Class of Sakaguchi Functions in Conic Region: Saritha. G. P, Fuad. S. Al Sarari, S. LathaerpublicationОценок пока нет
- MS Lync - Exchange - IntegrationДокумент29 страницMS Lync - Exchange - IntegrationCristhian HaroОценок пока нет