Академический Документы
Профессиональный Документы
Культура Документы
Iv Fluids Insulin Potassium: 5,3 Meq/L
Загружено:
fatqur280 оценок0% нашли этот документ полезным (0 голосов)
17 просмотров1 страницаinsulin intravena
Оригинальное название
IV Reguler Insulin
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документinsulin intravena
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
17 просмотров1 страницаIv Fluids Insulin Potassium: 5,3 Meq/L
Загружено:
fatqur28insulin intravena
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 1
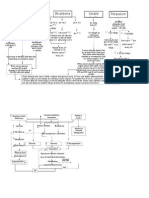
IV fluids insulin potassium
IV reguler insulin
Determine hydration status estabilise adequate
Insulin: 0,1 U/kg renal function (urine cutput 50 ml/hr)
Severe mild cardiogenic body weigh as
Hipovolemia Dehydration shock IV bolus
Administer 0,9% hemodynamic K+ <3,3 mEq/L K+ >5,3 mEq/L
(NaCl 1,0 L/hr) monitoring/
Pressors 0,1 U/kg/hr IV
continuous Hold insulin and give Do not give K1
Evaluats connected insulin infusion 20-30 mEqK1/hr until but check serum
Serum Na= K7 >3,5 mEq/L K1 every 2 hrs
Serum Na= Serum Na= Serum Na=
If serum glucosa does not
Hight normal low
full by 50-70 mg/dl in first K+ = <3,3 mmEq/L
0,45% NaCl 0,45% NaCl hour, double onsulin dose
(250-500 ml/hr) (250-500 ml/hr)
depanding on deppanding on Give 20 – 30 mEq K1 in each liter
Hydration state Hydration state When serum glucosa reaches 300 of IV fluid to keep serum K+
mg/dl, reduce reguler insulin infusion between 4-5 mEq/L
to 0,05-0,1 U/kg/hr IV. Keep serum
When serum glucosa
glucose between 250 and 300 mg/dl
reaches 200-250
mg/dl change to 5% until plasma osmolarity is <315
dextrose with 0,45% mOsm/kg and patient is mentally alert
NaCl at 150-250 ml/hr
Check electrolytas,BUN, creatinine and glucose every 2-4 hrs until stable. After resolution
of HHS and when patient is able to eat, inittiate SC multidose insulin regimen. Continue IV
insulin infusion for 1 – 2 hr after SC insulin begin to ensure adequate plasma insulin levels.
In insulin paive patients, start at 0,5 – 0,8 U/kg per day and adjust insulin as needed. Look
for precepitating cause(s).
Вам также может понравиться
- Principles of Management of DKAДокумент4 страницыPrinciples of Management of DKAHassen Kavi IsseОценок пока нет
- DKA Management Protocol - Docx PaulosДокумент3 страницыDKA Management Protocol - Docx PaulosMiraf MesfinОценок пока нет
- Guidelines For Management of Diabetes MellitusДокумент1 страницаGuidelines For Management of Diabetes MellitusthapanОценок пока нет
- Dka-Hhs Topic DiscussionДокумент2 страницыDka-Hhs Topic Discussionapi-648401824Оценок пока нет
- Dka 1Документ34 страницыDka 1Anne Lorraine BringasОценок пока нет
- Diabetes Mellitus in Pediatric: Dr. Wasnaa Hadi AbdullahДокумент30 страницDiabetes Mellitus in Pediatric: Dr. Wasnaa Hadi AbdullahLily AddamsОценок пока нет
- DM Diabetic Ketoacidosis DKA Management Algorithm Adult Patients 2019Документ1 страницаDM Diabetic Ketoacidosis DKA Management Algorithm Adult Patients 2019Hendra AfrilaОценок пока нет
- Guideline For The Management of Adults Patients With DKA or HHSДокумент3 страницыGuideline For The Management of Adults Patients With DKA or HHSJonard GiloОценок пока нет
- Diabetic Ketoacidosis (Dka) & Hyperosmolar Hyperglycemic Syndrome (HHS)Документ54 страницыDiabetic Ketoacidosis (Dka) & Hyperosmolar Hyperglycemic Syndrome (HHS)Beyene FelekeОценок пока нет
- Insulin Infustion OrdersДокумент1 страницаInsulin Infustion Orderserma wanda mundariОценок пока нет
- Type 1 Diabetes Mellitus and Diabetic Ketoacidosis (Pediatrics)Документ26 страницType 1 Diabetes Mellitus and Diabetic Ketoacidosis (Pediatrics)Sheharyar AjmalОценок пока нет
- Early Symptoms: Insidious Increase in Polydipsia and PolyuriaДокумент3 страницыEarly Symptoms: Insidious Increase in Polydipsia and Polyuriabes3rkerОценок пока нет
- IV Fluids Bicarbona Te Potassium: Soluble InsulinДокумент2 страницыIV Fluids Bicarbona Te Potassium: Soluble InsulinReza M. PrabowoОценок пока нет
- DKA Protocol TGДокумент11 страницDKA Protocol TGabelОценок пока нет
- Dka Dan HHS: Oleh: Tri Adiatmoko Hervi LaksariДокумент20 страницDka Dan HHS: Oleh: Tri Adiatmoko Hervi Laksarisunaryo lОценок пока нет
- Potassium Chloride GuidelinesДокумент25 страницPotassium Chloride GuidelinesYasser Gebril86% (7)
- Dka FueДокумент21 страницаDka Fuetrp45qm27dОценок пока нет
- Diabetic Ketoacidosis: Presented by The Students From Roll Numbers 31 - 40Документ20 страницDiabetic Ketoacidosis: Presented by The Students From Roll Numbers 31 - 40HUSSAIN NAZEESHAОценок пока нет
- Diabetic KetoacidosisДокумент22 страницыDiabetic KetoacidosispoktaviantiОценок пока нет
- Dka Topic Discussion ReviewДокумент5 страницDka Topic Discussion Reviewapi-648714317Оценок пока нет
- Diabetic Ketoacidosis (DKA)Документ12 страницDiabetic Ketoacidosis (DKA)Chinju Cyril50% (2)
- Diabetic Ketoacidosis IntanДокумент60 страницDiabetic Ketoacidosis Intandesi susantiОценок пока нет
- DKA AlgorismДокумент2 страницыDKA AlgorismYohannes hailuОценок пока нет
- Diabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiДокумент23 страницыDiabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiSreekrishnan Trikkur100% (2)
- Revised DKA 2015 PDFДокумент6 страницRevised DKA 2015 PDFDr AhmedОценок пока нет
- Diabetic Ketoacidosis (DKA) : Clinical ManifestationsДокумент3 страницыDiabetic Ketoacidosis (DKA) : Clinical ManifestationsJoyce Minerva Montero SamsonОценок пока нет
- Dka ProtocolДокумент3 страницыDka ProtocolRed DevilОценок пока нет
- Dijabetička KetoacidozaДокумент19 страницDijabetička KetoacidozaToNijeToniОценок пока нет
- Hyperglycemia in Critically Ill Management (: From ICU To The Ward)Документ20 страницHyperglycemia in Critically Ill Management (: From ICU To The Ward)destiana samputriОценок пока нет
- Hyperkalemia TreatДокумент5 страницHyperkalemia Treatpraveen kumarОценок пока нет
- DKA and HHS The Washington Manual of Critical CareДокумент6 страницDKA and HHS The Washington Manual of Critical Careمحمد عقيلي100% (1)
- Pediatric Diabetic Ketoacidosis (DKA) Algorithm (Page 1-ED) : DKA Diagnosed DKA Not DiagnosedДокумент2 страницыPediatric Diabetic Ketoacidosis (DKA) Algorithm (Page 1-ED) : DKA Diagnosed DKA Not Diagnosedrolland_arrizaОценок пока нет
- Diabetic KetoacidosisДокумент13 страницDiabetic KetoacidosisMabelle Blancada ConsultaОценок пока нет
- Acute Complication of Diabetes Mellitus: Laksmi SasiariniДокумент43 страницыAcute Complication of Diabetes Mellitus: Laksmi SasiariniClararida RiawanОценок пока нет
- Diabetic Ketoacidosis (DKA) : BackgroundДокумент7 страницDiabetic Ketoacidosis (DKA) : BackgroundLeoОценок пока нет
- Kad HHS 2019Документ35 страницKad HHS 2019Friska RamadayantiОценок пока нет
- Diabetic Ketoacidosis Hypoglycemia: DR MD Mamunul Abedin ShimulДокумент18 страницDiabetic Ketoacidosis Hypoglycemia: DR MD Mamunul Abedin ShimulDr. Mamunul AbedinОценок пока нет
- Seminar Presentation On Management of Diabetic Ketoacidosis BY:Kelil Kedir (CII)Документ34 страницыSeminar Presentation On Management of Diabetic Ketoacidosis BY:Kelil Kedir (CII)Meraol HusseinОценок пока нет
- DKA ModifiedДокумент25 страницDKA ModifiedSujit KoiralaОценок пока нет
- Acute Diabetic Ketoacidosis (DKA)Документ21 страницаAcute Diabetic Ketoacidosis (DKA)Madhu Sudhan Pandeya0% (1)
- Diabetic Ketoacidosis in Pregnancy: Diagnosis of DKAДокумент7 страницDiabetic Ketoacidosis in Pregnancy: Diagnosis of DKA123someone123Оценок пока нет
- DKA/HHS Pathway Phase 1 (Adult)Документ6 страницDKA/HHS Pathway Phase 1 (Adult)marshaОценок пока нет
- Diabetes KetoacidosisДокумент35 страницDiabetes KetoacidosisdaniejayanandОценок пока нет
- BIMC Adult DKA Protocol 2012Документ5 страницBIMC Adult DKA Protocol 2012djizhieeОценок пока нет
- Diabetic KetoacidosisДокумент41 страницаDiabetic Ketoacidosisdeneke100% (1)
- Kuwait PICU Taskforce DKA V1 5 June 2022Документ2 страницыKuwait PICU Taskforce DKA V1 5 June 2022Emad MashaalОценок пока нет
- Diabetic Ketoacidosis: Clinical Features and Management: - DR Sanjay Kalra, D.M. (Aiims)Документ26 страницDiabetic Ketoacidosis: Clinical Features and Management: - DR Sanjay Kalra, D.M. (Aiims)Siti RahmahОценок пока нет
- Management Protocol of DkaДокумент2 страницыManagement Protocol of Dkasky nutsОценок пока нет
- Iabetic ETO Cidosis: AnagementДокумент44 страницыIabetic ETO Cidosis: AnagementVenkata KrishnaОценок пока нет
- Diabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyДокумент24 страницыDiabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyGwEn LimОценок пока нет
- Dka 1Документ45 страницDka 1jomanabuhaniyehОценок пока нет
- Diabetic Ketoacidosis Treatment Protocol PDFДокумент3 страницыDiabetic Ketoacidosis Treatment Protocol PDFMoses MalungaОценок пока нет
- Hyperglycaemic Emergencies Inpatient Draft-1-3Документ13 страницHyperglycaemic Emergencies Inpatient Draft-1-3Cik JaaОценок пока нет
- Dr. Ashraf Hussein Ismail E.R Consultant, PSHДокумент17 страницDr. Ashraf Hussein Ismail E.R Consultant, PSHAshraf HusseinОценок пока нет
- Map DkaДокумент1 страницаMap DkaSH PrageethОценок пока нет
- High CBS in Medical EmergencyДокумент37 страницHigh CBS in Medical EmergencyHansika GunasekaraОценок пока нет
- TWU Anesthesia Cheat SheetДокумент2 страницыTWU Anesthesia Cheat Sheetinvading_jam7582100% (5)
- Guidelines and Protocols Of: Diabetes EmergenciesДокумент36 страницGuidelines and Protocols Of: Diabetes Emergenciesyassen hassanОценок пока нет
- DKA Management-2Документ7 страницDKA Management-2NisaОценок пока нет
- Pelvic Inflammatory Disease - 5Документ5 страницPelvic Inflammatory Disease - 5fatqur28Оценок пока нет
- Pelvic Inflammatory Disease - 2Документ2 страницыPelvic Inflammatory Disease - 2fatqur28Оценок пока нет
- Pelvic Inflammatory Disease - 1Документ8 страницPelvic Inflammatory Disease - 1fatqur28Оценок пока нет
- Jurnal Plasenta Akreta PDFДокумент5 страницJurnal Plasenta Akreta PDFfatqur28Оценок пока нет
- Herpes Zoster: Nurul Iska Ulmarika Idrisc111 10 831 Ruth Faustine J. Rayo C 1 1 1 1 0 1 8 0Документ26 страницHerpes Zoster: Nurul Iska Ulmarika Idrisc111 10 831 Ruth Faustine J. Rayo C 1 1 1 1 0 1 8 0fatqur280% (1)
- Case Report Herpes Zoster Regio Th11 - L5Документ37 страницCase Report Herpes Zoster Regio Th11 - L5fatqur28Оценок пока нет
- Antibiotik GangrenДокумент10 страницAntibiotik GangrenMutiara Khaerun NisaОценок пока нет
- Therapeutic Good Administration: Australia (TGA)Документ46 страницTherapeutic Good Administration: Australia (TGA)sanjivОценок пока нет
- Practice Test # 01 (Past Year PPSC Paper) : JOIN IS at WHATSAPP +92 333 2243031Документ19 страницPractice Test # 01 (Past Year PPSC Paper) : JOIN IS at WHATSAPP +92 333 2243031Saima ShehzadОценок пока нет
- Prioritization of Mabs During Resource Shortages 20211229Документ3 страницыPrioritization of Mabs During Resource Shortages 20211229News10NBCОценок пока нет
- API Supplier, Distributor & Manufacturers - 1000+ Lists - ChemjoinДокумент388 страницAPI Supplier, Distributor & Manufacturers - 1000+ Lists - Chemjoinমোঃ এমদাদুল হকОценок пока нет
- Passage 2Документ2 страницыPassage 2Minh ThanhОценок пока нет
- Request Letter For Pre-InD MeetingДокумент7 страницRequest Letter For Pre-InD MeetingharshitОценок пока нет
- Madhuri AbstractДокумент8 страницMadhuri AbstractRoll Number 115Оценок пока нет
- Training On Pfizer Vaccine ManagementДокумент132 страницыTraining On Pfizer Vaccine ManagementClaudia YuniarОценок пока нет
- 17.3 Note Taking GuideДокумент4 страницы17.3 Note Taking GuideGabriel ParksОценок пока нет
- Method For IV Heparin CalculationДокумент3 страницыMethod For IV Heparin CalculationDerricka CrosbyОценок пока нет
- Metabical AnalysisДокумент2 страницыMetabical AnalysisPriyanka NОценок пока нет
- KAPS Exam Guide and Sample Papers - Australian Pharmacy Council PDFДокумент10 страницKAPS Exam Guide and Sample Papers - Australian Pharmacy Council PDFShoaib BiradarОценок пока нет
- Abediterol (LAS100977), A Novel Long-Acting B - Agonist: Efficacy, Safety and Tolerability in Persistent AsthmaДокумент6 страницAbediterol (LAS100977), A Novel Long-Acting B - Agonist: Efficacy, Safety and Tolerability in Persistent AsthmaFi NoОценок пока нет
- Stockverfication NewДокумент184 страницыStockverfication NewbhadushaОценок пока нет
- MDR - Oral Boomer PDFДокумент15 страницMDR - Oral Boomer PDFBandameedi RamuОценок пока нет
- Pricardio Paracentesis/ Pericardiocentesis: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduДокумент17 страницPricardio Paracentesis/ Pericardiocentesis: Prepared By: Rashmita Byanju Shrestha Nursing Incharge Sicu and HduArchana MaharjanОценок пока нет
- Fake Dummy Data ClaimsДокумент616 страницFake Dummy Data ClaimsAnonymous ErWdFOTFОценок пока нет
- About The Baycol RecallДокумент4 страницыAbout The Baycol RecallZainab WowoussОценок пока нет
- C - II - 3 - Critical AppraisalДокумент10 страницC - II - 3 - Critical AppraisalWahyu NandaОценок пока нет
- Walmart 4 Dollar Drug ListДокумент6 страницWalmart 4 Dollar Drug ListCucho0% (2)
- B Pharm - 2019 - 3 - Pharmacology PDFДокумент1 страницаB Pharm - 2019 - 3 - Pharmacology PDFTripti PadaliaОценок пока нет
- Brand and Generic Medication Reference ListДокумент6 страницBrand and Generic Medication Reference ListAndi Dewi Pratiwi50% (2)
- SPC Septobar Effervescent GranulesДокумент3 страницыSPC Septobar Effervescent GranulesAia Hassan100% (1)
- 14 - Therapies PharmacyДокумент5 страниц14 - Therapies Pharmacymansourmona087Оценок пока нет
- ChemotherapyДокумент1 страницаChemotherapyGerardLum100% (2)
- S2k Guidelines For The Treatment ofДокумент12 страницS2k Guidelines For The Treatment ofVinh ThếОценок пока нет
- Antibiotics in Endodontics-Lecture 9Документ49 страницAntibiotics in Endodontics-Lecture 9mirfanulhaqОценок пока нет
- WHO Drug InformationДокумент99 страницWHO Drug Informationchromicutting100% (1)
- Chemotherapy For Gynecologic CancerДокумент69 страницChemotherapy For Gynecologic CancerBEREKET100% (1)